Highlights
-
•
We report a case of non-functional retroperitoneal paraganglioma.
-
•
Non-functioning retroperitoneal paragangliomas are rare and difficult to diagnose.
-
•
Surgical excision is recommended given potential malignant transformation.
-
•
Lifelong follow up is recommended as recurrence and metastasis are common.
Abbreviations: CT, computed tomography; NSE, neuron-specific enolase; MIBG, metaiodobenzylguanidine
Keywords: Paraganglioma, Organ of Zuckerkandl, Neuroendocrine tumour
Abstract
Paragangliomas are rare neoplasms arising from cells of the primitive neural crest. These tumours are often difficult to diagnose and treat. We report a case of a 42 year old female presenting with abdominal pain who had a retroperitoneal tumour situated at the aortic bifurcation. Serum catecholamine levels were normal. Complete resection of the tumour was performed. The histological examination and immunohistochemical analyses concluded the diagnosis of an organ of Zuckerkandl paraganglioma.
1. Introduction
Paragangliomas are rare neuroendocrine tumours arising from a widely dispersed collection of specialised neural crest cells [1]. The adrenal medullae represent the largest collection of paraganglionic tissue; tumours derived from them occur much more frequently than in extra-adrenal locations. It has been estimated that 10% of paragangliomas arise outside the adrenal glands [2]. The most common site of extra-adrenal occurrence is intra-abdominal, usually within the para-aortic and peri-nephric spaces [3]. Other rarer sites include the thorax, skull base and neck. Paragangliomas may be functional and result in symptoms of excess catecholamine production. Approximately 10–15% of such tumours is non-functional, and in another 10% hormone activity is not manifest clinically. They are often locally invasive and associated with a high incidence of local recurrence [4].
Non-functional paragangliomas pose a significant diagnostic challenge. In the absence of typical symptoms of catecholamine excess, the diagnosis of such tumours is often delayed [5]. In this report, the authors describe a new case of non-functional retroperitoneal paraganglioma discovered during investigation of abdominal pain.
2. Presentation of case
A 42 year old female was referred with vague abdominal pain of several years duration. She had a history of hypertension and her blood pressure was 135/95 mmHg at the time of admission, however she denied symptoms of catecholamine excess. She was taking no regular medications. There was no family history of illness. The physical examination was unremarkable with no palpable abdominal mass present. Abdominal ultrasonography showed an abnormal soft tissue mass anterior to the aortic bifurcation, initially thought to represent lymphadenopathy. Abdominal computed tomography (CT) showed a solitary well-defined heterogeneous mass centred level with the L5 vertebral body slightly to the left of midline, immediately anterior to the two common iliac arteries (Fig. 1) which was more consistent with paraganglioma. CT chest showed no intra-thoracic malignancy. Serum chromogranin A level was elevated at 276 ug/L (normal range 27–94 ug/L). The lesion was completely resected through a midline laparotomy incision. On macroscopic examination the mass measured 5.5 × 4.0 × 2.5 cm and was encapsulated with a lobulated, variegated orange/brown cut surface and central areas of hemorrhage (Fig. 2).
Fig. 1.

CT Scan: organ of Zuckerkandl paraganglioma.
Fig. 2.

Operative photo: organ of Zuckerkandl paraganglioma.
Histological examination identified a highly cellular, multinodular encapsulated tumour with a vascular framework containing many dilated and congested blood vessels (Fig. 3). The tumour was composed of compact nests of varying size in alveolar pattern. Two cell populations were noted within the tumour: larger epithelioid type cells with ill-defined granular cytoplasm and cells with small ovoid to polygonal monomorphic nuclei with granular chromatic pattern. The other cells were smaller, somewhat similar with scant cytoplasm. In places, zellballen pattern of paraganglioma was apparent. Diffuse sheets of tumour cells were also present. In one area, larger cells of epithelioid type, with eosinophilic granular cytoplasm, arranged in strands showed variation in nuclear size and shape with hyperchromasia. Occasional multinucleate giant cells were also seen. The tumour infiltrated the capsule and fibro-collagenous bands. Probable lymphovascular permeation was present. Immunohistochemical staining of the tumour showed that it strongly expressed chromogranin (Fig. 4), neuron-specific enolase (NSE) and synaptophysin. These findings led to a histological diagnosis of retroperitoneal paraganglioma.
Fig. 3.
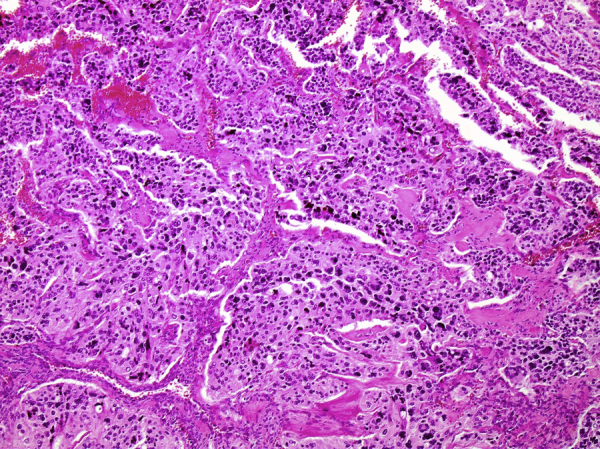
Haematoxylin and eosin stain: paraganglioma.
Fig. 4.
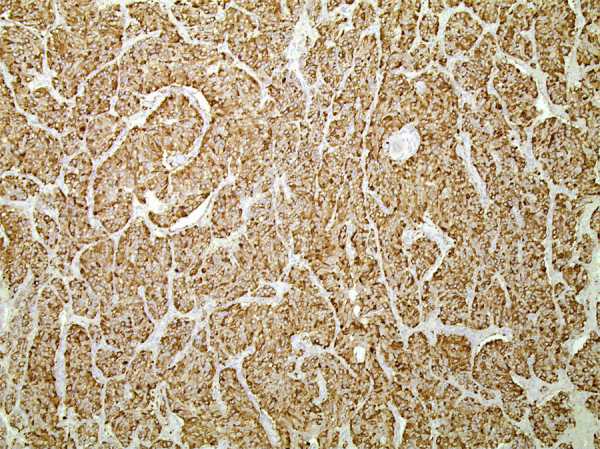
Immunohistochemistry: cells expressing chromogranin.
Post-operative 24-hour urine catecholamine studies and plasma metanephrines were negative. Scintigraphy with 123-I labeled metaiodobenzylguanidine (MIBG) was also negative. There were no complications over 6 months of follow up.
3. Discussion
Paragangliomas are rare tumours arising from sympathetic and parasympathetic paraganglia, which are derived from the neural crest cells. Those arising from the adrenal medulla are named phaeochromocytoma and comprise approximately 80% of these tumours. Extra-adrenal paragangliomas are found arising from chromaffin tissue along the autonomic nervous system and can thus be found in the head, neck, thorax, abdomen and pelvis. The most common site of sympathetic paragangliomas is in the abdomen, usually located in the organ of Zuckerkandl at the aortic bifurcation, consistent with the distribution of paraganglia first characterized in the human fetus by Zuckerkandl in 1901 [6], [7].
The median age of diagnosis for retroperitoneal paragangliomas is 37–43 years and the incidence is similar between men and women [1], [8], [9]. A large proportion of paragangliomas are related to disease-causing mutations or hereditary syndromes such as Von Hippel–Lindau (VHL) gene mutations, multiple endocrine neoplasia type 2 (MEN2), neurofibromatosis type 1 (NF1), the Carney triad and gene mutations of the subunits of succinate dehydrogenase (SDH) [10], [11].
Patients with functional paragangliomas that produce catecholamines may experience hypertension, flushing, tachycardia, palpitations, anxiety, headache and/or profuse diaphoresis [4], [5], [12]. Those with non-functioning retroperitoneal paragangliomas may be diagnosed incidentally or present with compressive symptoms such as abdominal pain that may be associated with nausea, vomiting, abdominal distension and weight loss [4], [13]. Non-functional retroperitoneal paragangliomas have also been reported to present atypically with chest pain or paralytic ileus [14], [15]. The diverse range of presentations often makes the clinical diagnosis of these tumours difficult.
Serum levels of chromogranin A, NSE or vimentin are elevated with most of the neuroendocrine tumours and are helpful to differentiate them from non-neuroendocrine tumours. On the basis of endocrine symptoms, neuroendocrine tumours can be differentiated by using hormonal assay in blood or urine. Ultrasound may be used as a first-line investigation however CT and MRI have higher sensitivity. Paragangliomas may show central necrosis or haemorrhage, calcification and enhancement. Functional imaging with MIBG scintigraphy may be used for better localisation of extra-adrenal disease or metastatic sites. Angiography may be useful in revealing vascular invasion or in demonstrating small metastases [16]. Ultimately although imaging techniques are helpful, the diagnosis of paragangliomas can only be confirmed with careful histological and immunohistochemical evaluation [17], [18].
Due to the malignant potential of paragangliomas, surgical excision is the preferred management. Resection is often challenging as these highly vascular tumours are frequently located near multiple vital blood vessels. If a tumour is felt to be unresectable, attempts to reduce its size using chemotherapy, radiation therapy or embolisation may be indicated because resection offers the only chance of cure [19]. Radiotherapy may also be used for inoperable tumours or for palliation. Radionucleotides may be the indicated therapy for tumours exhibiting uptake on diagnostic scan. Inoperable paragangliomas can be treated with octreotide [20].
Histologically paragangliomas are diagnosed by their highly vascular appearance, with chief cells and sustenacular cells arranged in clusters called zellballen. Chief cells are often positive for neuroendocrine markers (synaptophysin, NSE, chromogranin) on immunohistochemistry, while sustenacular cells are positive for S-100 protein [5]. Malignancy cannot be reliably diagnosed histologically and is often diagnosed based on presence of metastases. Approximately 20–42% of extra-adrenal sympathetic paragangliomas metastasise, compared to only 2–10% of phaeochromocytomas. Sites of metastasis include lymph nodes, bone, liver and lung. Metastatic lesions have a poor prognosis, with a reported 5-year survival rate of 36% [4].
4. Conclusion
Paragangliomas of the retroperitoneum are a rare group of tumours with malignant potential that cause considerable difficulty both in diagnosis and treatment. Our case highlights the importance of including the extra-adrenal paraganglioma in the differential diagnosis of retroperitoneal tumours. Advances in genetic testing and discovery of new molecular markers are contributing to increased understanding of paragangliomas, however at present there is no way to definitively predict metastatic risk. As recurrence and metastasis are common, lifelong follow-up is required.
Consent
Written consent was obtained from the patient to publish this case report.
Conflict of interest
The authors report no conflict of interest.
Funding
None.
Ethical approval
None.
Author contribution
Emma Gannan: writing.
Penelope van Veenendaal: review and editing.
Adam Scarlett: pathological analysis.
Michael Ng: review.
All authors approved the final version of the manuscript to be submitted.
Guarantor
Mr Michael Ng.
References
- 1.Feng N., Zhang W.Y., Wu X.T. Clinicopathological analysis of paraganglioma with literature review. World J. Gastroenterol. 2009;15(June (24)):3003–3009. doi: 10.3748/wjg.15.3003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wen J., Li H.Z., Ji Z.G., Mao Q.Z., Shi B.B., Yan W.G. A case of large silent extra-adrenal retroperitoneal paraganglioma resected laparoscopically. Chin. Med. Sci. J. 2010;25:61–64. doi: 10.1016/s1001-9294(10)60023-5. [DOI] [PubMed] [Google Scholar]
- 3.Whalen R.K., Althausen A.F., Daniels G.H. Extra-adrenal pheochromocytoma. J. Urol. 1992;147:1–10. doi: 10.1016/s0022-5347(17)37119-7. [DOI] [PubMed] [Google Scholar]
- 4.Sclafani L.M., Woodruff J.M., Brennan M.F. Extraadrenal retroperitoneal paragangliomas: natural history and response to treatment. Surgery. 1990;108:1124–1130. [PubMed] [Google Scholar]
- 5.Lack E.E., Cubilla A.L., Woodruff J.M., Lieberman P.H. Extra-adrenal paragangliomas of the retroperitoneum: a clinicopathologic study of 12 tumours. Am. J. Surg. Pathol. 1980;4:109–120. doi: 10.1097/00000478-198004000-00002. [DOI] [PubMed] [Google Scholar]
- 6.DeLellis R.A., Lloyd R.V., Heitz P.U., Eng C. World Health Organization Classification of Tumours. IARC Press; Lyon, France: 2004. Pathology and genetics of tumours of endocrine organs. [Google Scholar]
- 7.Zuckerkandl E. Ueber nebenorgane des sympathicus in retroperitonaealraum des menschen. Anat. Anz. 1901;15:91. [Google Scholar]
- 8.Somasundar P., Krouse R., Hostetter R., Vaughan R., Covey T. Paragangliomas –decade of clinical experience. J. Surg. Onc. 2000;74:286–290. doi: 10.1002/1096-9098(200008)74:4<286::aid-jso9>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 9.Hayes W.S., Davidson A.J., Grimley P.M., Hartman D.S. Extraadrenal retroperitoneal paraganglioma: clinical, pathologic and ct findings. AJR. 1990;155:1247–1250. doi: 10.2214/ajr.155.6.2173385. [DOI] [PubMed] [Google Scholar]
- 10.Jafri M., Maher E.R. The genetics of phaeochromocytoma: using clinical features to guide genetic testing. Eur. J. Endocrinol. 2012;166:151–158. doi: 10.1530/EJE-11-0497. [DOI] [PubMed] [Google Scholar]
- 11.Van Hulsteijn L.T., Dekkers O.M., Hes F.J., Smit J.W., Corssmit E.P. Risk of malignant paraganglioma in SDHB-mutation and SDHD-mutation carriers: a systematic review and meta-analysis. J. Med. Gen. 2012;49(12):768–776. doi: 10.1136/jmedgenet-2012-101192. [DOI] [PubMed] [Google Scholar]
- 12.Erickson D., Kudva Y.C., Ebersold M.J., Thompson G.B., Grant C.S., Van Heerden J.A., Young W.F., Jr. Benign paragangliomas: clinical presentation and treatment outcomes in 236 patients. J. Clin. Endocrinol. Metab. 2001;86:5210–5216. doi: 10.1210/jcem.86.11.8034. [DOI] [PubMed] [Google Scholar]
- 13.Kaltsas G.A., Besser G.M., Grossman A.B. The diagnosis and medical management of advanced neuroendocrine tumors. Endocr. Rev. 2004;25:458–511. doi: 10.1210/er.2003-0014. [DOI] [PubMed] [Google Scholar]
- 14.Brahmbhatt P., Patel P., Saleem A., Narayan R., Young M. Retroperitoneal paraganglioma presenting as a chest pain: a case report. Case Rep. Oncol. Med. 2013:1–4. doi: 10.1155/2013/329472. Art ID 329472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lin W.C., Wang H.Y., Chang C.W., Lin J.L., Tsai C.H. Retroperitoneal paraganglioma manifesting as paralytic ileus: a case report. J. Med. Case Rep. 2012;6(158):1–5. doi: 10.1186/1752-1947-6-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patel Y.D., Morehouse I.I.T. Malignant paragangliomas of the retroperitoneum: value of computed tomography and angiography. Clin. Radiol. 1984;35:185–188. doi: 10.1016/s0009-9260(84)80131-2. [DOI] [PubMed] [Google Scholar]
- 17.Van Gils A.P., Falke T.H., van Erkel A.R., Arndt J.W., Sandler M.P., van der Mey A.G. MR imaging and MIBG scintigraphy of pheochromocytomas and extraadrenal functioning paragangliomas. Radiographics. 1991;11:37–57. doi: 10.1148/radiographics.11.1.1671719. [DOI] [PubMed] [Google Scholar]
- 18.Sahdec A., Sohaib A., Monson J.P., Grossman A.B., Chew S.L., Reznek R.H. CT and MR imaging of unusual locations of extra-adrenal paragangliomas (pheochromocytomas) Eur. Radiol. 2005;15:85–92. doi: 10.1007/s00330-004-2412-3. [DOI] [PubMed] [Google Scholar]
- 19.Bryant R.L., Stevenson D.R., Hunton D.W. Primary malignant retroperitoneal tumors. Am. J. Surg. 1982;144:646–649. doi: 10.1016/0002-9610(82)90543-8. [DOI] [PubMed] [Google Scholar]
- 20.Mikhail R.A., Moore J.B., Reed D.N., Jr. Malignant retroperitoneal paragangliomas. J. Surg. Oncol. 1986;32:32–36. doi: 10.1002/jso.2930320110. [DOI] [PubMed] [Google Scholar]


