Highlights
-
•
80 year old presenting with abdominal pain, raised lactate, hyperglycaemia.
-
•
Radiological diagnosis of mesenteric panniculitis from CT.
-
•
No clear cause for raised lactate.
-
•
Patient simultaneously found to be type 2 diabetic—further research warranted.
Keywords: Mesenteric panniculitis, Abdominal pain, Hyperglycaemia, Raised lactate, Steroids, Fat necrosis
Abstract
Introduction
Mesenteric panniculitis is a rare condition which presents as abdominal pain. It involves benign inflammatory or fibrotic changes affecting the mesentery of the bowel.
Presentation of case
An 80 year old man presented with severe abdominal pain of acute onset. He was found to have a high lactate and high blood glucose. He was not a known diabetic. A computed tomography (CT) scan revealed a diagnosis of mesenteric panniculitis, and the patient rapidly responded to steroid treatment.
Discussion
Mesenteric panniculitis has been known to present as an acute abdomen. However, an associated high lactate and hyperglycaemia is hitherto unreported in the literature. With no obvious precipitant for an increased lactate, we propose it is potentially caused by the subsequent fat necrosis and regional ischaemia associated with mesenteric panniculitis.
Conclusion
This case report underlines the importance of further research into the relationship between mesenteric panniculitis, a high lactate, and diabetes. In addition, short term steroid treatment (one month) seemed to confer the same benefit as long term steroid treatment.
1. Introduction
An unusual presentation of an unusual condition; this case report of a patient with a diagnosis of mesenteric panniculitis serves to contribute to the sparse amount of literature on a rare and poorly-understood condition. First described in 1924, it has been theorized to be part of a spectrum of sclerosing panniculitis; which has been further sub-classified according to the predominance of three processes affecting the mesentery of the small bowel; all present but to varying degrees. These are: inflammation (in which case it is termed mesenteric panniculitis), fat necrosis (described as mesenteric lipodystrophy) and fibrosis (known as retractile mesenteritis) [1].
2. Presentation of case
An 80 year old man presented with severe abdominal and back pain, associated with vomiting and bowels not opening for five days.
His past medical history included vascular dementia, a mitral valve replacement, a coronary artery bypass graft, cerebrovascular attacks, atrial fibrillation, hypertension, hyperlipidaemia and epilepsy. The patient’s regular medications included warfarin, furosemide, nicorandil, bisoprolol, atorvastatin and Epilim Chrono.
The patient was haemodynamically stable. On physical examination the abdomen was grossly distended with generalized tenderness, tympanic and had normal bowel sounds. Rectal examination was unremarkable. Urine dipstick was positive for blood and glucose, but negative for leucocytes and ketones.
Arterial blood gases showed a pH of 7.39, pCO2 of 4.40 kPa, pO2 of 10.3 kPa, HCO3− of 21.0 mmol/L. The lactate was raised at 8.1 mmol/L. Otherwise, laboratory results showed mild leucocytosis (13.0 × 109/L), mild neutrophilia (10.3 × 109/L) and normocytic anaemia (Hb: 124 g/L). C reactive protein (CRP) was mildly elevated (21 mg/L). Liver function tests, urea, creatinine and electrolytes were all normal. The patient was hyperglycaemic, with a blood glucose of 21.7 mmol/L. An abdominal X-ray was unremarkable.
The initial impression was ischaemic bowel.
The patient remained stable with a good urine output. He was transferred to an intensive care unit for optimisation and fluid resuscitation. The patient’s lactate dropped to 6.3 mmol/L, whilst his blood glucose was 12.1 mmol/L and blood ketones were 0.1 mmol/L.
An urgent CT abdomen and pelvis scan showed no evidence of bowel ischaemia or obstruction. However, the CT scan did show “an ill-defined increase in the density of the peritoneal fat at the base of the mesentery with a few small associated lymph nodes. The appearance is that of a panniculitis” (Fig.1, Fig. 2, Fig. 3 ).
Fig.1.
CT scan depicting hyperattenuated fatty mass.
Fig. 2.

Saggital view with a hyperdense strip visible.
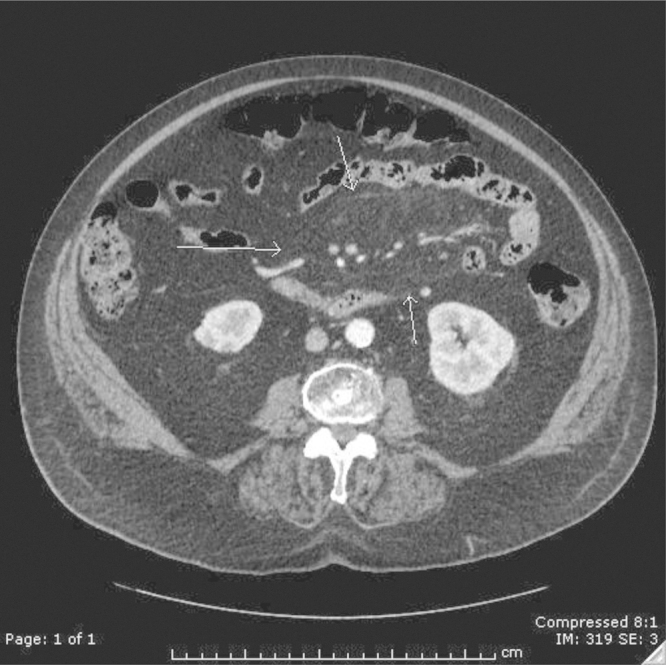
Fig. 3.

Transverse view.
On the second day of admission the patient was started on intravenous hydrocortisone 50 mg (four-times daily) and antibiotics were stopped.
Within 24 h of commencing steroid treatment there was a clinical improvement in the patient’s condition; the patient no longer had abdominal pain, nausea or vomiting and was passing flatus and stool. His inflammatory markers quickly normalised, a HbA1c result was 76 mmol/mol, and an ESR was found to be 33 mm/h seven days post-admission.
After five days of intravenous steroids, the patient was switched to a reducing regime of oral steroids. He was also started on insulin for his newly-diagnosed type II diabetes.
A second abdominal CT scan, twenty days after admission, revealed no additional findings or changes, with the patient remaining clinically asymptomatic.
3. Discussion
The presentation of mesenteric panniculitis with an acute abdomen has previously been reported in the literature, but we were unable to find any precedent for a significantly high lactate. Furthermore, there was no obvious cause; we found no evidence for shock, cardiac arrest, trauma, seizure, excessive muscle activity, burns and smoke inhalation, diabetic ketoacidosis, thiamine deficiency, malignancy, liver dysfunction, inborn errors of metabolism, pharmacologic agents or toxins or alcohol [2]. Interestingly, Delgado Plasencia et al. documented histopathological evidence of fat necrosis and chronic inflammation in all eight cases of mesenteric panniculitis they investigated [3]. In the presence of such processes, the resulting regional ischaemia will lead to anaerobic conditions, and thereby could have potentially caused the elevated levels of lactate seen in this patient. Significantly, mesenteric panniculitis has been postulated as being severely under-diagnosed; affecting as much as 1% of the population. In this case report, we ask, could lactate be used as an additional tool alongside clinical, radiological and operative findings in the challenging diagnosis of mesenteric panniculitis?
A multitude of chemotherapeutic interventions have been proposed including steroids, colchicine, and antibiotics [4], [5]. This patient was started on IV hydrocortisone followed by oral prednisolone. Miyake et al. have documented a case of a 65 year old man showing a good response to steroid treatment both clinically and radiologically [6]. This was also the case here as the patient showed a good response to steroid therapy clinically with a significant improvement in symptoms (including pain, nausea and vomiting) within 24 h of commencement and was discontinued on steroids after one month with no adverse features on follow up. This case report adds further weight to the efficacy of steroid treatment in the management of mesenteric panniculitis, although a randomized controlled trial is required to establish solid evidence.
The patient was also concurrently hyperglycaemic on admission, although was neither acidotic nor ketotic. He had been investigated for diabetes prior to admission when he was found to have a normal HbA1c. He has now been initiated on insulin treatment, and his HbA1c remains elevated. Whilst we recognise mesenteric panniculitis and diabetes could present simultaneously, we do wonder whether this could represent more than a coincidence. Considering the precise aetiology of mesenteric panniculitis has never been fully established, we suggest an area for future research; a possible link between mesenteric fat, glycaemic regulation and mesenteric panniculitis.
4. Conclusion
This case report of a patient with a confirmed radiological diagnosis of mesenteric panniculitis serves as a valuable contribution to the existing literature of a condition with an unknown aetiology, a vague presentation, and no consensus on classification nor first-line treatment. Further research on lactate as a diagnostic tool, as well as glycaemic regulation in its pathophysiology, could help to enable greater clarity and understanding on this condition, whilst increasing much-needed awareness.
Conflict of interests
None.
Sources of funding
There were no sponsors involved.
Ethical approval
Case report only requiring no ethics committee involvement.
Consent
Consent has been obtained from the patient.
Authors contribution
Moaize Chechi largely responsible for the abstract, introduction, case presentation and the conclusion.
Zeyad Sallami overseeing the whole case report and providing his expertise, knowledge and direction, as well as significantly editing the paper.
Luke Armstrong largely responsible for the literature review and the writing up of the discussion.
All authors have approved the final submission of the paper.
Guarantor
Dr. Moaize Chechi MBBS B.Sc., 132 Addison Road, Reading, Berkshire RG1 8EG.
Acknowledgements
We hereby acknowledge the assistance Dr. Liaquat Khan (consultant radiologist at Bronglais General Hospital) in interpreting the radiological findings used in this paper.
Contributor Information
Moaize Chechi, Email: moaizechechi@gmail.com.
Zeyad Alsallami, Email: zeyad.sallami@wales.nhs.uk.
Luke Armstrong, Email: lukearmstrong1088@gmail.com.
References
- 1.Mata J.M., Inaraja L., Martin J., Olazabal A., Castilla M.T. CT features of mesenteric panniculitis. J. Comput. Assist. Tomogr. 1987;11:1021–1023. doi: 10.1097/00004728-198711000-00018. [DOI] [PubMed] [Google Scholar]
- 2.Andersen L.W., Mackenhauer J., Roberts J.C., Berg K.M., Cocchi M.N., Donnino M.W. Etiology and therapeutic approach to elevated lactate levels. Mayo Clin. Proc. 2013;88(October (10)):1127–1140. doi: 10.1016/j.mayocp.2013.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Delgado Plasencia L., Rodruez Ballester L., Lez-Tomassetti Ferndez E.M., Herndez Morales A., Carrillo Pallar A., Herndez Siverio N. Mesenteric panniculitis: experience in our center. Rev. Esp. Enferm. Dig. 2007;99:291–297. doi: 10.4321/s1130-01082007000500010. [DOI] [PubMed] [Google Scholar]
- 4.Grieser C., Denecke T., Langrehr J., Hamm B., Hanninen E.L. Sclerosing mesenteritis as a rare cause of upper abdominal pain and digestive disorders. Acta Radiol. 2008:1–3. doi: 10.1080/02841850802093887. [DOI] [PubMed] [Google Scholar]
- 5.Issa Iyad, Baydoun Hassan. Mesenteric panniculitis: various presentations and treatment regimens. World J. Gastroenterol. 2009;15(August (30)):3827–3830. doi: 10.3748/wjg.15.3827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miyake H., Sano T., Kamiya J., Nagino M., Uesaka K., Yuasa N., Oda K., Nimura Y. Successful steroid therapy for postoperative mesenteric panniculitis. Surgery. 2003;133:118–119. doi: 10.1067/msy.2003.54. [DOI] [PubMed] [Google Scholar]


