Abstract
BACKGROUND AND OBJECTIVE:
Applying topical fluoride varnish (FV) to young children’s teeth is an effective therapeutic strategy for preventing early childhood caries (ECC). In 2008, the pediatricians at Contra Costa Regional Medical Center and Health Centers became concerned that our low-income pediatric patients had high rates of ECC and very limited access to dental care. We formed an interdisciplinary safety net-academic partnership with the University of California San Francisco to implement routine FV applications, along with oral health education, screening, and referral during well-child exams for children aged 1 to 5 years.
METHODS:
Over 3 years, the team developed clinical policies, educational materials, billing, and support systems to facilitate implementation in the primary care setting. A pilot study was performed in 2 health centers; improvements to the implementation plan were made. A team of local providers and academic partners performed system-wide didactic and hands-on trainings and spread this intervention to the remaining 6 health centers. Continued improvement strategies and provider feedback were pursued with each measurement cycle.
RESULTS:
In August 2012, 95% of all children aged 1 to 5 years who were seen for well-child checkups received a FV application and oral health education during their primary care well visit. Repeat measurement in April 2014 showed a sustained rate of 97% application of FV for children in this age group seen for well-child visits.
CONCLUSIONS:
With institutional commitment and an academic partnership, a safety net institution can integrate routine FV applications and oral health interventions into well-child visits to reduce ECC.
Early childhood caries (ECC) is the most common chronic disease of childhood.1 Children from low-income families suffer from high rates of caries, particularly those from Latino and Asian backgrounds. The NHANES from 1999 to 2004 reported that 42% of poor US children experienced ECC by age 5.2–5 Caries in primary dentition predicts future decay and misalignment of permanent teeth.6 Despite the high prevalence of this disease, dental care remains the largest unmet health need of US children. This unmet need is particularly true for toddlers, who infrequently visit dentists; in 2014 only 17% of Medicaid-enrolled toddlers aged 12 to 23 months had any preventive dental services.7,8
Primary care physicians frequently observe children with pain from decayed teeth, as well as increased school absences, trouble eating, sleep loss, and risk of serious infection.9,10 In recent position statements, the American Academy of Pediatrics (AAP) has recommended that primary care health care professionals conduct oral health risk assessments starting when children are 6 months old, and refer patients to a dentist at 12 months of age.11,12 In 2014, the US Preventive Services Task Force recommended “primary care clinicians apply fluoride varnish (FV) to the primary teeth of all infants and children starting at the age of primary tooth eruption.”13 The AAP Section on Oral Health subsequently endorsed universal early childhood FV application and clarified that FV should be applied “to the teeth of all infants and children at least once every 6 months and preferably every 3 months, starting when the first tooth erupts and until establishment of a dental home.”14
FV is a safe, well-tolerated, low-cost caries preventive agent that can quickly be painted onto young children’s teeth. Medicaid reimburses FV application in 49 states and the District of Columbia.15 When accompanied by educational counseling, a single FV application has been shown to reduce ECC for high-risk children by 33% to 50%.16,17 In the North Carolina “Into the Mouths of Babes” program, young children with ≥4 primary care oral health visits with FV applications were shown to have significantly lower likelihood of future caries-related treatments and hospital episodes than children with no primary care oral health visits.18,19
Despite the proven efficacy of FV, many barriers have been identified that have, to date, prevented widespread adoption of oral health practices in primary care.20,21 Close et al surveyed primary care providers participating in a North Carolina Medicaid demonstration program and identified provider barriers, including resistance to implementation by colleagues, difficulties integrating these procedures into the practice routine, and difficulties with referrals for dental problems.22 Similarly, in a series of national surveys performed since 2008, Lewis et al and Quinonez et al have reported that although surveyed pediatricians consistently view performing oral-health-related screening and preventive tasks as within their purview, lack of oral health training, inadequate time during health supervision visits, and inadequate reimbursement remain as barriers to actually integrating these tasks into their practices.23,24
In 2007, our pediatric department at Contra Costa Regional Medical Center (CCRMC), a safety-net hospital and clinic system in California, decided to launch a quality improvement (QI) initiative to address high ECC rates and inadequate access to dental care for young children from CCRMC low-income families. A 2007 oral health report regarding Contra Costa County low-income children documented that only 3 pediatric dentists in Contra Costa County were accepting new patients, and few dentists in the County saw children younger than 5 years old. Although California’s MediCal program covers dental care for children, only 17% of MediCal-insured low-income children aged 0 to 5 years in the County visited a dentist annually and local hospitals reported a 6-month wait for ECC treatment under general anesthesia.25
In response to this crisis, we organized an interdisciplinary oral health work group. Department members also participated in 2 ECC trainings sponsored by California’s First Smiles program, an education and training initiative that sought to increase primary care providers’ role in ECC prevention.26 Although there was widespread support for FV applications in our department, enhanced Medicaid reimbursement of $18 for the procedure every 6 months for children through age 5 years, and evidence of significant effectiveness, translating the research-based FV application guidelines into clinical practice initially proved to be a challenge for our safety-net health system. After 6 months, the workgroup reached the conclusion that the effort could not succeed without dedicated staff and technical assistance. A year later, the University of California San Francisco (UCSF) Center to Address Disparities in Children’s Oral Health was recruiting practice sites through the San Francisco Bay Area Collaborative Research Network to participate in a National Institute of Dental and Craniofacial Research (NIDCR)-funded study on ECC prevention. This article describes the process of improvement that took place after CCRMC partnered with the UCSF researchers to integrate oral health prevention into routine primary care practice.
Methods
Setting
Located in the San Francisco Bay Area, CCRMC hospital and regional clinics in 2011 served a population of ∼100 000 low-income individuals and provided 11 947 well-child visits for children aged 1 to 5 years annually. Ninety-five percent of children seen for well-child care were insured by either our local Medicaid managed care health plan or fee-for-service Medicaid. One hundred twenty salaried primary care family physicians, pediatricians, nurse practitioners, and family medicine residents staffed our 8 federally qualified health clinics.
Planning
In 2010, CCRMC and UCSF convened a multiagency, multidisciplinary team to develop interventions and measure outcomes for both the departmental QI initiative and the NIDCR-funded study. The NIDCR-funded pilot study was reviewed and approved by the UCSF Committee on Human Research. Neither the UCSF nor the CCRMC committees felt it was necessary to review the CCRMC QI project according to UCSF policy that “sharing or generalizing the results of a QI activity does not imply that the original activity was in fact research.”
The expanded intervention team was composed of a pediatrician, an ambulatory nurse, a quality nurse, a dentist, a dental hygienist from UCSF, and a registered dental hygienist in alternative practice (RDHAP) hired by CCRMC as the project manager. Over the 4-year project time span, the team met regularly every 2 to 4 weeks. Team members identified 3 elements essential to expanded oral health primary care practice: enhanced oral health education, routine FV application and provider examination, and facilitated referrals for ongoing dental health care (Fig 1).
FIGURE 1.
Components of enhanced oral health intervention in primary care.
To facilitate routine FV application, providers were prompted to perform enhanced oral health education throughout well-child visits by using questions and documentation integrated initially into paper forms, and finally into the EPIC (Epic Systems, Verona, WI) electronic health record (EHR) system. We added parental questions regarding tooth-brushing habits, bottle use, and sweetened beverage consumption to our intake questionnaires. Nurses began asking parents about the most recent dental visit when welcoming caregivers at scheduled well-child visits. Upon discharge from the clinic, nurses provided families with additional health education, a toothbrush, and information on local dental resources.
The multidisciplinary team decided to implement FV application with every well-child visit from ages 1 through 5 years. This schedule created 3 opportunities for FV in the second year of life, 2 in the third year, and 1 application at ages 3, 4, and 5 years, for a total of 8 opportunities during early-childhood primary care visits.
Providers were prompted to complete orders for the discharging nurse to apply FV at the end of the visit while administering vaccines, performing blood tests, or giving discharge instructions to the family. We also developed a FV nursing ambulatory policy that added standing orders for FV at each toddler well-child visit. If providers forgot to order FV or if the family came in for immunizations only, treatment nurses were given authority to inform the family that FV was due and apply it to the child’s teeth. Families who had seen a dentist in the past month or who did not desire the varnish were not given an application.
To ensure follow-up of patients in need of dental evaluation and treatment, the pediatric oral health team collaborated with the CCRMC dental department and developed referral appointments in our colocated dental clinics. Initially, we attempted to refer all children to our dental clinics if they did not already have a local dentist; however, we found that our dental clinics did not have capacity for these referrals and ultimately gave patients contact information for local dentists and only referred children with suspected caries for an appointment in our system.
Pilot Study and Project Dissemination
In partnership with UCSF, the team piloted the oral health intervention at 2 of the CCRMC regional health centers from May to July 2010. The research protocol initiated by UCSF had stipulated that primary care staff at 1 health center would apply the FV during well-child visits while staff at the second health center would refer children to a local dentist for the FV application. The pilot study showed that FV application rates were significantly higher when applied during well-child visits than when the child was referred to the dentist (results to be reported separately). Anecdotally, parents and staff reported ECC prevention was consistent with the mission of well-child visits; the procedure proved to be quick and was relatively easy to incorporate into the visit workflow.
After completing the pilot study, the QI team began a series of Plan-Do-Study-Act cycles to address barriers to integrated oral health activities and support dissemination throughout all 8 regional health centers (Table 1).27 Dissemination occurred in a stepwise process to all primary care sites between January and March 2011.
TABLE 1.
Barriers and Solutions Essential to FV Implementation
| Barrier | Example | Solution |
|---|---|---|
| Lack of primary care expertise in oral health interventions | Primary care team uncertain regarding periodicity, safety, and contraindications to FV application; ambulatory providers and nurses lacked skills in FV application | Hired a RDHAP and partnered with UCSF to develop policies and training curriculum. Hands-on and didactic trainings provided by dental/primary care teams. |
| Time | Providers and nurses reluctant to add additional time demands to primary care visits | FV application is quick; providers and nurses educated regarding the efficacy of FV. FV application linked to immunizations and discharge procedures. |
| Patient acceptance | Patients unfamiliar with FV and oral health recommendations regarding brushing, foods, and referral to a dental home | Providers and nurses educated and prompted to discuss recommendations with families during visit. Educational brochure and posters developed. |
| Uniform adoption throughout clinic system | Previous projects had faltered with incomplete adoption throughout the system | Policies adopted and age-specific forms developed to prompt education and FV application. Feedback provided to health centers regarding comparative rates by site. |
| Reimbursement | Costs of FV | Billing form developed to charge for procedure. Expenses recouped through federally qualified health center billing, Medicaid managed-care payment. |
| Inadequate monitoring and provider feedback | Previous initiatives had been incompletely implemented because of lack of monitoring and provider feedback | Partnership with UCSF provided stipend to hire project manager. Pediatric department adopted FV as a QI project providing staffing of quality nurse. Charts reviewed regularly and feedback given to providers, nurses, and administration. |
The project team developed training curriculum and organized lunch trainings for all primary care providers and nurses with information on the pathophysiology and prevalence of ECC, the efficacy of FV for ECC prevention, the oral health examination, health education principles, and referrals to local dental resources. Every treatment nurse also received a skills-based “hands-on” training. At each clinic site, the RDHAP demonstrated FV application on a child between the ages of 1 and 5 years and gave each treatment nurse the opportunity to apply FV, ask questions, and receive feedback during the training. To ensure fidelity, the project manager completed a skills acquisition checklist and verified proficiency for each nurse upon completing the training.
After providers and nurses were trained, the team introduced educational materials, FV supplies, and revised well-child forms to each site. Before and after implementation, the RDHAP project manager visited clinic sites regularly to address concerns; project leaders also sent reminder e-mails to staff, and a clinic newsletter featured the project.
After each implementation step, the project team identified further revisions to processes to improve FV rates at all sites and made changes to the periodicity, training, policies, and billing protocols for the initiative
Whenever outcome data were collected, we shared results with the ambulatory medical and nursing staff and the hospital and health centers’ quality committees. To build consistent rates throughout all sites, we gave comparative feedback to the clinics; one of the authors (NMM) explored system attitudes with nursing staff focus groups and one-on-one key informant interviews with clinic administrators.
Measures and Analysis
Our outcome measure for the project was the percentage of children aged 1 through 5 years who received a FV application during, or in association with, a well-child visit. During the project period, we had 4 measurement cycles and reviewed 1977 charts or patient health records. As a QI project, we chose the data collection dates to study the impact of each phase of the initiative’s implementation. Each measurement cycle cohort represented all children seen for a well-child examination during a 2-week period. For each cycle, we generated a list of all well-child visits and all FV applications billed for children aged 1 through 5, regardless of payer. For the 2011–2012 cycles, secondary chart review was performed if FV was not billed with the visit. After our system adopted EPIC as our EHR in July 2012, we developed a report identifying the FV application rates for well-child visits aged 1 through 5 during the designated time period.
Results
The target population for the QI project was the children aged 1 through 5 years seen for well-child examinations by a primary care provider in the CCRMC regional health centers. Table 2 shows the demographic characteristics for the young children seen for well-child visits in our system in July 2012 and April 2014, time periods corresponding to the completion of the intervention, and the follow-up FV measurement. The demographics for the populations were similar; however, younger children and more children on Medicaid managed care were seen in 2012, before California’s expansion of Medicaid eligibility in 2013 (Table 2).
TABLE 2.
Characteristics of Young Children Seen for Well-Child Visits 2012, 2014
| Characteristics | July 2012 (n = 198) | April 2014 (n = 471) |
|---|---|---|
| Age, mo | ||
| 12–23 | 75 (37.9) | 177 (37.6) |
| 24–35 | 34 (17.2) | 86 (18.3) |
| 36–47 | 27 (13.6) | 63 (13.4) |
| 48–59 | 42 (21.2) | 83 (17.6) |
| 60–71 | 20 (10.1) | 62 (13.2) |
| Race/ethnicity | ||
| Asian | 10 (5.1) | 31 (6.6) |
| Black/African American | 30 (15.2) | 63 (13.4) |
| Hispanic or Latina/Latino | 126 (63.6) | 291 (61.8) |
| White/Caucasian | 26 (13.1) | 61 (13.0) |
| Other | 6 (3.0) | 25 (5.3) |
| Spoken language | ||
| English | 102 (51.5) | 249 (52.9) |
| Spanish | 90 (45.5) | 206 (43.7) |
| Other | 6 (3.0) | 16 (3.4) |
| Insurance status | ||
| Medicaid | 21 (10.6) | 160 (34.0) |
| Medicaid managed care | 170 (85.9) | 302 (64.1) |
| Other | 7 (3.5) | 9 (1.9) |
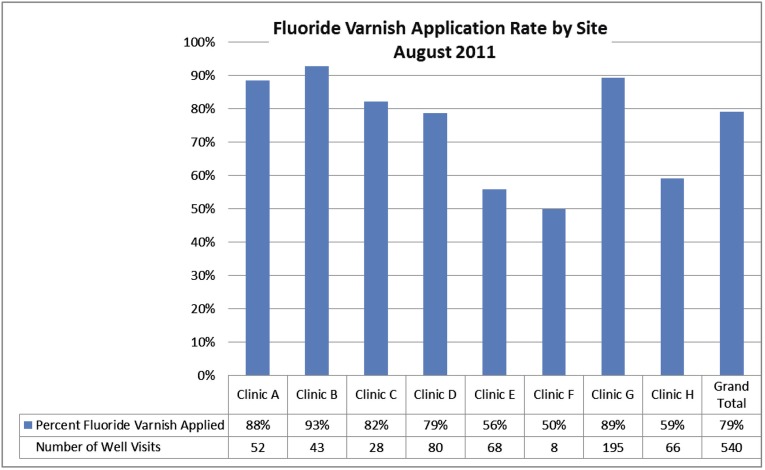
Before 2011, there were no children receiving FV during primary care visits. After implementation, our initial measurement in April 2011 showed a FV application rate of 77%. Follow-up in August 2011 showed little improvement with wide variations among the clinic sites (Fig 2).
FIGURE 2.
FV application rate by clinic site, August 2011.
With changes in processes to decrease variation in care, we saw rates rise to 95% and less variation among sites in April 2012. This rate was sustained when measured 2 years later after implementing the EHR. Figure 3 shows FV application rates during the evaluation period 2010–2014.
FIGURE 3.
FV application rates 2010–2014.
Discussion
This project demonstrates that oral health interventions in primary care, including routine topical FV applications, can successfully be integrated into early childhood well-child visits in safety net primary care health centers. Our multidisciplinary project team was able to develop care processes that blended well into the everyday flow of well-child care, resulting in a sustained FV rate of 95% to 97% in the targeted age group. More than 11 000 applications of FV occur in our system annually. The impact of this intervention is the potential for a significant reduction in ECC within a high-risk, diverse, safety-net population of young children.
Primary care QI projects are notoriously difficult to pursue to this level of adoption and maintenance. We believe that the project’s success resulted in part because our multidisciplinary team framed this intervention to fit into the primary care staff’s perspectives, both in the necessity of the preventive intervention and in the flow in the clinic setting. After education about ECC and the impact of multiple FV applications in reducing caries-related treatments, medical providers and nurses saw caries prevention as part of their mission, similar to preventing childhood infectious diseases. We aligned the FV applications periodicity with the AAP-recommended schedule for well-child visits, which recommends that toddlers have 1 to 3 well-child visits annually.28 Providers and parents became accustomed to discussing oral health and FV at all early childhood visits. By linking the FV, dental referral, and oral health education to the vaccines and other discharge procedures, we took advantage of nursing staff skills in administering treatments to young children and educating families.
We also believe that the development of an interdisciplinary team, use of consistent Plan-Do-Study-Act improvement cycles, and our medical-dental-academic partnership created momentum and success for our project. Consistent with the Model of Improvement, we continually strategized on how to improve our rates, measured the results, and analyzed patterns and opportunities for further improvement.27 Our partnerships with UCSF and our dental staff allowed us to address implementation barriers. The adoption of standardized practice in the health centers and prompts in the EHR assisted in reducing variation in practice within our geographically dispersed ambulatory staff. UCSF and the San Francisco Bay Area Collaborative Research Network also provided us with the $45 000 necessary to hire a RDHAP project manager, whose experience in oral disease prevention was a major contributor to this project’s success.
Staff training and our medical-dental partnership were essential components of our success; however, health systems choosing to implement oral health interventions into primary care would not need to have an academic partner. Successful oral health integration into the primary care setting has been studied by the Pediatric Oral Health Research & Policy Center of the American Academy of Pediatric Dentistry; they found that model programs had partnered with AAP Chapter Oral health advocates, Cavity Free at Three, and/or local dental hygienists. After visiting 12 successful practices in a variety of settings with oral health integration, the American Academy of Pediatric Dentistry study team concluded that common elements of successful integration were as follows: an oral health champion who “had strong feelings about the importance of oral health and its relationship to systemic health,” delegation of oral health activities throughout the health care team, formal integration of activities into the workflow, and prompts and questions included in the EHR.29
Limitations
Although our team implemented oral health education and provider examinations, we did not measure system-wide compliance with these components of our program. We also could not reliably determine which children were seeing a dentist and/or receiving FV applications in other community sites.
Next Steps
We limited our intervention to children in the targeted age range coming into clinic for a well-child examination. The recent US Preventive Services Task Force statement recommends all children receive this preventive treatment starting at the age of primary teeth eruption to 5 years. Similar to immunizations, full implementation of FV in our system would include an integrated medical-dental periodicity and tracking of all primary care visits, dental visits, and FV applications.
Conclusions
FV application in primary care settings is an effective ECC preventive intervention that has been sustainably implemented by our health care system. Primary care staff members are well positioned to provide caries-prevention interventions. This preventive approach is particularly effective for early childhood, in which patients and families are seen frequently, and in which the key to prevention is counseling, oral health interventions, and referral. FV application in the primary care setting also addresses the significant disparities in ECC rates by income and race/ethnicity. Enhanced provider knowledge regarding ECC as well as administration of FV may serve to address some of the present inequities in access to dental care and high rates of dental decay for low-income children.
Acknowledgments
Donna Kaufman, RN, Kelley Taylor, RN, Matthew C. White, Domenic Cavallaro, DDS, Anthony M. Longoria, FNP, and Nathan G. Kaufman, DDS, all contributed to the development, implementation of, and/or data collection for the FV project. We are indebted to the Dental Health Action Group for clearly outlining our access problems in 2007. We also benefited from the support of our local health plan, Contra Costa Health Plan. Finally, we also thank the administrative, nursing, and medical staff, as well as the patients at CCRMC, for their support of this project.
Glossary
- AAP
American Academy of Pediatrics
- CCRMC
Contra Costa Regional Medical Center
- ECC
early childhood caries
- EHR
electronic health record
- FV
fluoride varnish
- NIDCR
National Institute of Dental and Craniofacial Research
- QI
quality improvement
- RDHAP
registered dental hygienist in alternative practice
- UCSF
University of California San Francisco
Footnotes
Dr Dooley carried out the implementation of the quality improvement project, coordinated data collection, and drafted the initial manuscript; Ms Moultrie carried out the implementation of the quality improvement project, coordinated and performed data collection, and critically reviewed the manuscript; Ms Heckman conceptualized and designed the study, carried out the implementation of the quality improvement project, and critically reviewed the manuscript; Drs Gansky, Potter, and Walsh conceptualized and designed the study and critically reviewed the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: This work was made possible by grant U54 DE 019285 from the National Institute of Dental and Craniofacial Research, a component of the National Institutes of Health (NIH). This publication was also supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF-CTSI grant UL1 RR024131. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.US Department of Health and Human Services Oral Health in America: A Report of the Surgeon General. Rockville, MD: National Institute of Dental and Craniofacial Research, National Institutes of Health, US Dept of Health and Human Services; 2000 [Google Scholar]
- 2.Dye BA, Tan S, Smith V, et al. Trends in oral health status: United States, 1988–1994 and 1999–2004. Vital Health Stat 11 2007;(248):1–92 [PubMed]
- 3.Dye BA, Arevalo O, Vargas CM. Trends in paediatric dental caries by poverty status in the United States, 1988–1994 and 1999–2004. Int J Paediatr Dent. 2010;20(2):132–143 [DOI] [PubMed] [Google Scholar]
- 4.Edelstein BL, Chinn CH. Update on disparities in oral health and access to dental care for America’s children. Acad Pediatr. 2009;9(6):415–419 [DOI] [PubMed] [Google Scholar]
- 5.Iida H, Auinger P, Billings RJ, Weitzman M. Association between infant breastfeeding and early childhood caries in the United States. Pediatrics. 2007;120(4). Available at: www.pediatrics.org/cgi/content/full/120/4/e944 [DOI] [PubMed] [Google Scholar]
- 6.Lynch RJ. The primary and mixed dentition, post-eruptive enamel maturation and dental caries: a review. Int Dent J. 2013;63(suppl 2):3–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Newacheck PW, Hughes DC, Hung YY, Wong S, Stoddard JJ. The unmet health needs of America’s children. Pediatrics. 2000;105(4 pt 2):989–997 [PubMed] [Google Scholar]
- 8.US Department of Health & Human Services; Centers for Medicare and Medicaid Services Early and periodic screening, diagnostic, and treatment. 2014. National Data. Available at: http://www.medicaid.gov. Accessed October 30, 2015
- 9.Braun PA, Lind KE, Henderson WG, Brega AG, Quissell DO, Albino J. Validation of a pediatric oral health-related quality of life scale in Navajo children. Qual Life Res. 2015;24(1):231–239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huntington NL, Spetter D, Jones JA, Rich SE, Garcia RI, Spiro A III. Development and validation of a measure of pediatric oral health-related quality of life: the POQL. J Public Health Dent. 2011;71(3):185–193 [PMC free article] [PubMed] [Google Scholar]
- 11.Hale KJ; American Academy of Pediatrics Section on Pediatric Dentistry . Oral health risk assessment timing and establishment of the dental home. Pediatrics. 2003;111(5 pt 1):1113–1116 [DOI] [PubMed] [Google Scholar]
- 12.Section on Pediatric Dentistry and Oral Health . Preventive oral health intervention for pediatricians. Pediatrics. 2008;122(6):1387–1394 [DOI] [PubMed] [Google Scholar]
- 13.Moyer VA; US Preventive Services Task Force . Prevention of dental caries in children from birth through age 5 years: US Preventive Services Task Force recommendation statement. Pediatrics. 2014;133(6):1102–1111 [DOI] [PubMed] [Google Scholar]
- 14.Clark MB, Slayton RL; Section on Oral Health . Fluoride use in caries prevention in the primary care setting. Pediatrics. 2014;134(3):626–633 [DOI] [PubMed] [Google Scholar]
- 15.Trusts PC. Reimbursing physicians for fluoride varnish. Updated October2015. Available at: http://www.pewstates.org/research/analysis/reimbursing-physicians-for-fluoride-varnish-85899377335. Accessed October 30, 2015
- 16.Marinho VC, Worthington HV, Walsh T, Clarkson JE. Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2013;7:CD002279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chou R, Cantor A, Zakher B, Mitchell JP, Pappas M. Preventing dental caries in children <5 years: systematic review updating USPSTF recommendation. Pediatrics. 2013;132(2):332–350 [DOI] [PubMed] [Google Scholar]
- 18.Pahel BT, Rozier RG, Stearns SC, Quiñonez RB. Effectiveness of preventive dental treatments by physicians for young Medicaid enrollees. Pediatrics. 2011;127(3). Available at: www.pediatrics.org/cgi/content/full/127/3/e682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stearns SC, Rozier RG, Kranz AM, Pahel BT, Quiñonez RB. Cost-effectiveness of preventive oral health care in medical offices for young Medicaid enrollees. Arch Pediatr Adolesc Med. 2012;166(10):945–951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lewis C, Lynch H, Richardson L. Fluoride varnish use in primary care: what do providers think? Pediatrics. 2005;115(1). Available at: www.pediatrics.org/cgi/content/full/115/1/e69 [DOI] [PubMed] [Google Scholar]
- 21.O’Callaghan AM, Douglass JM. The experience of medical clinicians implementing fluoride varnish in Connecticut. Pediatr Dent. 2013;35(5):435–439 [PubMed] [Google Scholar]
- 22.Close K, Rozier RG, Zeldin LP, Gilbert AR. Barriers to the adoption and implementation of preventive dental services in primary medical care. Pediatrics. 2010;125(3):509–517 [DOI] [PubMed] [Google Scholar]
- 23.Lewis CW, Boulter S, Keels MA, et al. Oral health and pediatricians: results of a national survey. Acad Pediatr. 2009;9(6):457–461 [DOI] [PubMed] [Google Scholar]
- 24.Quinonez RB, Kranz AM, Lewis CW, et al. Oral health opinions and practices of pediatricians: updated results from a national survey. Acad Pediatr. 2014;14(6):616–623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dental Health Action Group Children’s oral health program. Healthy teeth for life: the oral health of children in Contra Costa County. Martinez, CA: Contra Costa County Health Services; 2007. Available at: http://cchealth.org/dental/pdf/healthy_teeth_for_life_2007.pdf. Accessed October 30,2015
- 26.Barbara Aved Associates First 5 Oral Health Education and Training Program. Final evaluation report. March 2008. Available at: http://www.cdafoundation.org/Portals/0/pdfs/first5_finalevalrpt.pdf. Accessed October 30,2015
- 27.Langley GJ, Moen R, Nolan KM, et al. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. 2nd ed. San Francisco, CA: Jossey-Bass; 2009 [Google Scholar]
- 28.Cynthia Baker, Graham A Barden III, Brown OW, et al. ; Geoffrey R Simon; Committee on Practice and Ambulatory Medicine; Bright Futures Periodicity Schedule Workgroup . 2014 recommendations for pediatric preventive health care. Pediatrics. 2014;133(3):568–570 [DOI] [PubMed] [Google Scholar]
- 29.Mitchell-Royston L, Nowak A, Silverman J American Academy of Pediatric Dentistry. Interprofessional study of oral health in primary care. May 2014. Available at: http://www.aapd.org/assets/1/7/Dentaquest_Year_1_Final_Report.pdf. Accessed October 30,2015