Abstract
Background:
Concussion guidelines recommend physical and cognitive rest until all postconcussion symptoms resolve, in part because of potential health risks, including catastrophic injury related to a second impact. However, when postconcussion symptoms persist for weeks or months, these risks are poorly characterized.
Hypothesis:
Physicians’ perceived health risks and management strategies for patients with persistent postconcussion symptoms will vary.
Study Design:
Cross-sectional study.
Level of Evidence:
Level 3.
Methods:
A survey of the physician members of the American College of Sports Medicine assessed the perceived health risks related to advancing activity, the indications for neuroimaging, and the referral patterns for patients with persistent postconcussion symptoms.
Results:
A total of 572 physicians completed the survey (response rate, 27.2%). The majority of physicians recommended physical rest (97.4%) and cognitive rest (93.8%) within the first week of injury. Perceived health risks related to advancing activity in the symptomatic patient differed at 2 weeks versus 3 months after injury (P < 0.001 for all comparisons). Respondents from the United States were more likely to list second impact syndrome as a potential health risk at 2 weeks compared with respondents from other countries (P = 0.04). The majority (56%) responded that the risk of second impact syndrome remains until all symptoms resolve. When postconcussion symptoms persist beyond 1 month, 61.9% of physicians responded that neuroimaging is indicated. Approximately 60% of respondents had access to a multidisciplinary concussion clinic within 60 miles of their practice.
Conclusion:
When postconcussion symptoms persist, the perceived health risks, management practices, and access to multidisciplinary care vary among physicians.
Keywords: concussion, postconcussion syndrome, mild traumatic brain injury, management, survey
It is estimated that 1.6 to 3.8 million sport-related traumatic brain injuries (TBIs) occur in the United States each year, the majority of which are concussions.11 All current concussion management guidelines from the American Academy of Neurology,5 American Academy of Pediatrics,8 American Medical Society for Sports Medicine,9 National Athletic Trainers’ Association,1 and 4th International Conference on Concussion in Sport15 recommend physical and cognitive rest as the cornerstone for acute management of the symptomatic patient after concussion.
Some degree of physical and cognitive rest postinjury may hasten recovery,2 but the management recommendation originates from the potential health risks related to prematurely advancing physical activity.9 Patients who return to sports while symptomatic from acute concussion may have a lowered concussion threshold with subsequent impact,6 while poor balance and slowed reaction times may increase collision risk, further increasing risk of injury.7,9 Among high school and collegiate football players, 79% to 92% of same-season repeat concussions occur within 10 days of the initial concussion.6,13 Advancing activity in the symptomatic patient may exacerbate concussion symptoms and delay overall recovery. The most concerning health risk related to the premature advance of activity in the symptomatic concussion patient is catastrophic injury, specifically second impact syndrome (SIS).16 While the patient is still symptomatic from an acute concussion, the brain is prone to autoregulatory dysfunction.18 With a second impact, malignant cerebral edema and herniation can develop, resulting in a nearly 100% mortality rate.16,21
While consensus exists about general concussion management acutely after injury, very little is known about the potential health risks when postconcussion symptoms persist beyond the typical recovery time of 7 to 10 days. Rather than continuing physical and cognitive rest, the gradual resumption of preinjury activities may be beneficial.19,20 Since the potential health risks are not well characterized after this early postconcussion period, management practices may vary. The aim of the current study was to determine physicians’ perceived health risks and management strategies for the patient with postconcussion symptoms that persist beyond the typical 7- to 10-day recovery period.
Methods
This study was approved by the institutional review board at Nationwide Children’s Hospital. We conducted a cross-sectional survey of the American College of Sports Medicine (ACSM) physician members. From September to October 2013, email invitations containing a unique survey link were sent, with up to 2 subsequent email reminders sent at 2- to 4-week intervals.
The survey (see Appendix, available at http://sph.sagepub.com/content/by/supplemental-data) queried respondents about their management practices and the perceived health risks when patients have persistent postconcussion symptoms. Specific survey questions addressed physician demographics and medical practice characteristics, the roles for physical and cognitive rest after acute concussion, the perceived health risks associated with advancing activity in the patient with persistent symptoms at 2 weeks and at 3 months, the perceived time frame for SIS risk, the indications for neuroimaging when symptoms persist for more than 1 month, referral patterns when symptoms persist, and access to multidisciplinary concussion clinics. The survey was face-validated by 10 study-ineligible physicians (not members of the ACSM) at our institution. Consent was indicated by survey completion.
Data Analysis
Data were analyzed using SPSS version 21 (SPSS Inc). Descriptive statistics were calculated. Categorical variables were compared using the Pearson chi-square test or the Fisher exact test. Predictor variables were modeled using binary logistic regression. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. Significance was set at 5%.
Results
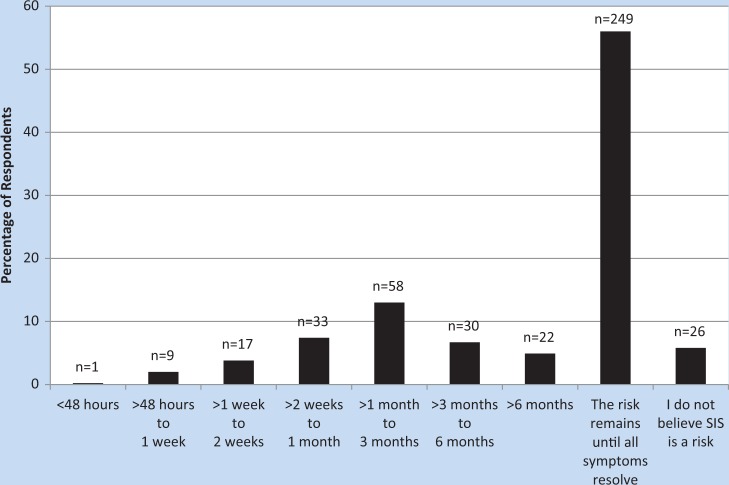
Among the 2191 physicians eligible for survey, 85 emails returned as “undeliverable.” Of the 2106 remaining participants, 572 (27.2%) responded to the survey (Table 1). Survey questions and results are shown in Figure 1 and Tables 2 through 7.
Table 1.
Respondent demographics
| n (%) | |
|---|---|
| Country | |
| USA | 500 (87.4) |
| Other | 72 (12.6) |
| Medical specialtya | |
| Sports medicine | 443 (77.4) |
| Family practice | 239 (41.8) |
| Physical medicine | 61 (10.7) |
| Pediatrics | 59 (10.3) |
| Internal medicine | 44 (7.7) |
| Orthopaedics | 37 (6.5) |
| Emergency medicine | 21 (3.7) |
| Neurology | 4 (0.7) |
| Neurosurgery | 2 (0.3) |
| Other | 42 (7.3) |
| Years in practice | |
| <10 | 178 (31.1) |
| 10-20 | 150 (26.2) |
| >20 | 228 (39.9) |
| Other (in training or not practicing) | 16 (2.8) |
| Practice settinga | |
| Solo | 70 (12.2) |
| Group | 200 (35) |
| Hospital-based | 136 (23.8) |
| Government | 18 (3.2) |
| Academic, clinical | 206 (36) |
| Academic, research only | 9 (1.6) |
| Other | 32 (5.6) |
| Do not practice | 12 (2.1) |
| Percentage of concussion patients in practiceb | |
| 10 | 312 (56.8) |
| 10-50 | 182 (33.2) |
| >50 | 22 (4.0) |
| Other (retired or do not practice) | 33 (6.0) |
| Percentage of concussion patients that are pediatric (<18 years old)b | |
| <50 | 184 (35.6) |
| >50 | 306 (59.2) |
| Do not manage pediatric concussion | 27 (5.2) |
More than 1 answer could be selected.
Automatically skipped by some respondents based on prior answers.
Figure 1.
Visual representation of responses to the question: In the adolescent patient who continues to experience postconcussion symptoms, what is the earliest time period after injury where second impact syndrome (SIS) is no longer a risk? Excludes respondents who were not familiar with SIS (n = 16) and those who did not have an opinion (n = 111).
Table 2.
In the patient with postconcussion symptoms, do you typically recommend physical rest and cognitive rest (also referred to as “brain rest”) within the first week after injury?
| n (%)a | |
|---|---|
| Yes, I typically recommend both | 497 (92.9) |
| No, I rarely recommend either | 9 (1.7) |
| I typically recommend physical rest but rarely recommend cognitive rest | 24 (4.5) |
| I typically recommend cognitive rest but rarely recommend physical rest | 5 (0.9) |
Excludes respondents who do not see patients within 1 week of injury (n = 10) and those who do not provide these sorts of treatment recommendations (n = 27).
Table 7.
Do you have a multidisciplinary concussion clinic within 60 miles of your medical practice?
| n (%) | |
|---|---|
| Yes | 341 (59.6) |
| No | 158 (27.6) |
| I do not know | 67 (11.7) |
| I do not have a medical practice | 5 (0.9) |
Table 3.
Two weeks/3 months after injury, what are the health risks associated with the gradual advancement of physical and cognitive activities in the patient who continues to experience postconcussion symptoms?
| 2 Weeks After Injury, n (%)a | 3 Months After Injury, n (%)a | P Valueb | |
|---|---|---|---|
| Lowered threshold for repeat concussion | 349 (61) | 263 (46) | <0.001 |
| Worsening of current symptoms | 459 (80.2) | 320 (55.9) | <0.001 |
| Delayed recovery from current concussion | 443 (77.4) | 273 (47.7) | <0.001 |
| Second impact syndrome | 268 (46.9) | 138 (24.1) | <0.001 |
| There are no potential health risks related to activity and postconcussion symptoms | 17 (3) | 84 (14.7) | <0.001 |
Excludes respondents who reported that they did not know (n = 22 at 2 weeks, n = 55 at 3 months) and those who marked “other” (n = 32 at 2 weeks, n = 48 at 3 months).
Boldfaced P values indicate statistical significance.
Table 5.
Is the persistence of postconcussion symptoms beyond 1 month an indication for brain scan (CT or MRI)?
| n (%) | |
|---|---|
| Yes | 354 (61.9) |
| No | 162 (28.3) |
| I do not know | 30 (5.2) |
| I do not have an opinion | 25 (4.4) |
CT, computed tomography; MRI, magnetic resonance imaging.
Table 6.
When you refer patients with complex or persistent postconcussion symptoms to other medical specialists, to which medical specialist(s) do you refer?
| n (%) | |
|---|---|
| Neurology | 332 (58) |
| Neuropsychology | 294 (51.4) |
| Vestibular rehabilitation | 208 (36.4) |
| Multidisciplinary concussion clinic | 186 (32.5) |
| Headache specialist | 96 (16.8) |
| Psychology | 78 (13.6) |
| Sports medicine | 56 (9.8) |
| Psychiatry | 48 (8.2) |
| Neurosurgery | 43 (7.5) |
| Other | 36 (6.3) |
| I do not refer | 28 (4.9) |
Logistic Regression
Several physician characteristics were predictive of a perceived SIS risk at 2 weeks and 3 months postconcussion (Table 4). Respondents from the United States were more likely than respondents from other countries to list SIS as a risk at 2 weeks; sports medicine physicians were less likely to list SIS as a risk at 2 weeks and at 3 months; and physicians with greater than 10 years of experience were also less likely to consider SIS to be a risk at 2 weeks and at 3 months.
Table 4.
Predictors of second impact syndrome as a perceived health risk at 2 weeks versus 3 months
| 2 Weeks | 3 Months | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P Valuea | OR | 95% CI | P Valuea | |
| Constant | 1.78 | 0.02 | 1.5 | 0.34 | ||
| US vs non-US | 1.9 | 1.02-3.55 | 0.04 | 0.68 | 0.35-1.3 | 0.24 |
| Sports medicine vs other | 0.43 | 0.28-0.65 | <0.001 | 0.37 | 0.23-0.58 | <0.001 |
| Academic vs other | 0.97 | 0.66-1.4 | 0.86 | 1.19 | 0.76-1.85 | 0.45 |
| >10% concussion patients vs <10% | 0.75 | 0.52-1.09 | 0.14 | 0.81 | 0.52-1.26 | 0.35 |
| >50% pediatric concussion vs <50% | 0.95 | 0.65-1.4 | 0.8 | 0.7 | 0.45-1.1 | 0.12 |
| >10 years’ experience vs <10 years | 0.66 | 0.44-0.97 | 0.04 | 0.57 | 0.36-0.9 | 0.02 |
OR, odds ratio.
Boldfaced P values indicate statistical significance.
Discussion
Current guidelines endorse physical and cognitive rest as the cornerstone of acute concussion treatment, but evidence-based guidelines do not exist when postconcussion symptoms persist beyond the typical 7- to 10-day period. More than 90% of the physicians in our survey report adherence to the guideline recommendations of rest within the first week of injury, an improvement compared with a 2012 survey of family practice physicians where 75.5% recommended physical rest but only 28.4% recommended cognitive rest during the acute recovery period.12 In contrast, there was less uniformity among our survey respondents regarding management practices and perceived health risks when concussion symptoms persist beyond the typical recovery period.
After an acute concussion, the symptomatic patient may have a lower concussion threshold, slower reaction times, and impaired balance, all of which could increase the risk of further injury if activities are advanced too quickly.7,9 In our survey, physicians acknowledged several potential health risks related to the premature advance of activity. The most commonly identified risks included worsening of the current concussion symptoms and delayed concussion recovery. Few experimental data exist about the direct effects of physical and cognitive activity on acute concussion recovery. Complete physical and cognitive rest may not be practical (or beneficial).19,20 Among 335 patients aged 8 to 23 years, Brown et al2 found that those patients with the highest self-reported levels of cognitive activity after concussion had the longest recovery times. There were no differences among patients with complete cognitive rest and those with mild or moderate cognitive activity.
In our survey, physicians’ perceptions of health risks differed at 2 weeks compared with 3 months after concussion. These health risks included worsening of current symptoms, delayed concussion recovery, lowered threshold for repeat concussion, and catastrophic risks such as SIS. Both the 2-week and 3-month durations represent degrees of abnormal postconcussion symptom persistence, yet fewer physicians acknowledged health risks when symptoms lasted longer. For example, more respondents considered SIS to be a potential health risk at 2 weeks than at 3 months, suggesting that the physicians perceive that the risk decreases over time, even as symptoms persist. In a subsequent survey question (intentionally worded differently), the majority responded that the SIS risk remains until all symptoms resolve, regardless of symptom duration. We cannot readily explain the apparent dissonance between responses. Perhaps the former question led fewer physicians to identify health risks at 3 months because they perceived a lower relative risk compared with 2 weeks, while the latter question lacked the 2-week comparison, causing more physicians to align their responses with the published consensus recommendations.1,5,8,9
Considering that the risk of catastrophic injury such as SIS plays an important role in concussion management, little is known about this risk when concussion symptoms persist. In a critical review of published SIS cases, the 5 patients with the most convincing evidence of SIS each sustained their second impact within 1 week of the first injury.16 In our survey, certain physician characteristics predicted SIS as a perceived health risk at 2 weeks and at 3 months after concussion. Respondents from the United States may have been more likely to list SIS as a risk because of the predominance of SIS cases published from the United States and the absence of SIS cases reported in the European or Australian literature.14 Sports medicine physicians and physicians with more than 10 years of experience were less likely to regard SIS as a potential health risk, which could reflect the ongoing debate about the mere existence of SIS in the sports medicine literature.3,14,16,17
In the acute concussion setting, neuroimaging is not recommended except in certain situations to rule out more severe brain injury, but no recommendations exist about neuroimaging when postconcussion symptoms persist.1,5,8,9,15 The majority of physicians in our survey responded that neuroimaging is indicated when symptoms persist beyond 1 month. The utility of conventional neuroimaging for persistent symptoms is unclear; however, advanced neuroimaging techniques used in concussion research have shown some inconsistent abnormalities in patients with prolonged postconcussion symptoms.4 To aid in the management of complex or persistent postconcussion symptoms, referral to medical specialists and dedicated concussion clinics can be beneficial. We found a high referral rate to neurology and a small percentage of physicians who do not refer patients with complex or persistent postconcussion symptoms. These findings are consistent with a survey of general pediatricians where 95% acknowledged referring patients with persistent postconcussion symptoms to other medical specialists, with neurology being the specialty of choice.10 Approximately one-third of the physicians in our survey refer to a multidisciplinary concussion clinic, whereas almost twice as many respondents have such a clinic within 60 miles of their practice.
We acknowledge several potential study limitations. Our response rate was relatively low, which can bias results. We limited our survey questions to 2 specific time points: 2 weeks and 3 months. These time points were arbitrarily chosen to represent early persistent and late persistent symptoms. ACSM physicians with an interest in concussion may be more likely to respond to a concussion survey and may have different opinions and practices than nonresponders, limiting our ability to generalize results. Survey questions were multiple choice and provided few opportunities for respondents to write in comments or to qualify responses, which could limit accurate assessment of opinion. Finally, survey self-report may not reflect actual clinical practice.
Conclusion
Whereas physical and cognitive rest are generally accepted in the management of acute concussion, physicians’ perceived health risks and management practices vary when concussion symptoms persist.
Supplementary Material
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Broglio SP, Cantu RC, Gioia GA, et al. National Athletic Trainers’ Association position statement: management of sport concussion. J Athl Train. 2014;49:245-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Brown NJ, Mannix RC, O’Brien MJ, Gostine D, Collins MW, Meehan WP., 3rd Effect of cognitive activity level on duration of post-concussion symptoms. Pediatrics. 2014;133:E299-E304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cantu RC, Gean AD. Second-impact syndrome and a small subdural hematoma: an uncommon catastrophic result of repetitive head injury with a characteristic imaging appearance. J Neurotrauma. 2010;27:1557-1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Eierud C, Craddock RC, Fletcher S, et al. Neuroimaging after mild traumatic brain injury: review and meta-analysis. Neuroimage Clin. 2014;4:283-294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Giza CC, Kutcher JS, Ashwal S, et al. Summary of evidence-based guideline update: evaluation and management of concussion in sports: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2013;80:2250-2257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Guskiewicz KM, McCrea M, Marshall SW, et al. Cumulative effects associated with recurrent concussion in collegiate football players: the NCAA Concussion Study. JAMA. 2003;290:2549-2555. [DOI] [PubMed] [Google Scholar]
- 7. Guskiewicz KM, Perrin DH, Gansneder BM. Effect of mild head injury on postural stability in athletes. J Athl Train. 1996;31:300-306. [PMC free article] [PubMed] [Google Scholar]
- 8. Halstead ME, Walter KD. American Academy of Pediatrics. Clinical report—sport-related concussion in children and adolescents. Pediatrics. 2010;126:597-615. [DOI] [PubMed] [Google Scholar]
- 9. Harmon KG, Drezner J, Gammons M, et al. American Medical Society for Sports Medicine position statement: concussion in sport. Clin J Sport Med. 2013;23:1-18. [DOI] [PubMed] [Google Scholar]
- 10. Kaye AJ, Gallagher R, Callahan JM, Nance ML. Mild traumatic brain injury in the pediatric population: the role of the pediatrician in routine follow-up. J Trauma. 2010;68:1396-1400. [DOI] [PubMed] [Google Scholar]
- 11. Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21:375-378. [DOI] [PubMed] [Google Scholar]
- 12. Lebrun CM, Mrazik M, Prasad AS, et al. Sport concussion knowledge base, clinical practises and needs for continuing medical education: a survey of family physicians and cross-border comparison. Br J Sports Med. 2013;47:54-59. [DOI] [PubMed] [Google Scholar]
- 13. McCrea M, Guskiewicz K, Randolph C, et al. Effects of a symptom-free waiting period on clinical outcome and risk of reinjury after sport-related concussion. Neurosurgery. 2009;65:876-882. [DOI] [PubMed] [Google Scholar]
- 14. McCrory P, Davis G, Makdissi M. Second impact syndrome or cerebral swelling after sporting head injury. Curr Sports Med Rep. 2012;11:21-23. [DOI] [PubMed] [Google Scholar]
- 15. McCrory P, Meeuwisse WH, Aubry M, et al. Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport Held in Zurich, November 2012. Br J Sports Med. 2013;47:250-258. [DOI] [PubMed] [Google Scholar]
- 16. McCrory PR, Berkovic SF. Second impact syndrome. Neurology. 1998;50:677-683. [DOI] [PubMed] [Google Scholar]
- 17. Mori T, Katayama Y, Kawamata T. Acute hemispheric swelling associated with thin subdural hematomas: pathophysiology of repetitive head injury in sports. Acta Neurochir Suppl. 2006;96:40-43. [DOI] [PubMed] [Google Scholar]
- 18. Reilly PL. Brain injury: the pathophysiology of the first hours. “Talk and die revisited”. J Clin Neurosci. 2001;8:398-403. [DOI] [PubMed] [Google Scholar]
- 19. Schneider KJ, Iverson GL, Emery CA, McCrory P, Herring SA, Meeuwisse WH. The effects of rest and treatment following sport-related concussion: a systematic review of the literature. Br J Sports Med. 2013;47:304-307. [DOI] [PubMed] [Google Scholar]
- 20. Silverberg ND, Iverson GL. Is rest after concussion “the best medicine?”: recommendations for activity resumption following concussion in athletes, civilians, and military service members. J Head Trauma Rehabil. 2013;28:250-259. [DOI] [PubMed] [Google Scholar]
- 21. Wetjen NM, Pichelmann MA, Atkinson JL. Second impact syndrome: concussion and second injury brain complications. J Am Coll Surg. 2010;211:553-557. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.