Abstract
No regulatory mandate exists in the United States (U.S.) for comprehensive obstructive sleep apnea (OSA) risk assessment and stratification for commercial motor vehicle (CMV) drivers. Current Federal Motor Carrier Safety Administration (FMCSA) requirements are outdated and depend largely on subjective report, a less reliable strategy in an occupational setting. Without FMCSA standards, sleep specialists, occupational medical examiners and employers rely on a collection of medical consensus recommendations to establish standards of care. These recommendations advise OSA risk assessment through a combination of focused medical history, physical examination, questionnaires, and accident history, which increase OSA detection compared to current FMCSA standards. For those diagnosed with OSA, consensus-based risk stratification helps identify CMV drivers who may benefit from OSA treatment and establish minimum standards for assessing treatment efficacy and adherence. Unfortunately no consolidated recommendation exists; rather, publications span medical and governmental literature in a patchwork fashion that no longer fully reflect current practice due to subsequent advances in OSA diagnosis, treatment, and technology. Based on searches of medical literature, internet materials, and reference lists from existing publications, an overview and discussion of key published recommendations regarding OSA assessment and treatment in CMV operators is provided. Suggestions for incorporating these recommendations into clinical sleep medicine practice in the U.S. are presented. The challenge for sleep specialists is maintaining the delicate balance between recommendations impacting standard of care and associated medico-legal impact with stakeholder interests from medical, regulatory, industry and public perspectives while providing high quality and efficient care.
Citation:
Colvin LJ, Collop NA. Commercial motor vehicle driver obstructive sleep apnea screening and treatment in the United States: an update and recommendation overview. J Clin Sleep Med 2016;12(1):113–125.
Keywords: obstructive sleep apnea, commercial motor vehicle, driver, federal motor carrier safety administration, screening, sleep apnea, occupation, department of transportation, CMV
OBSTRUCTIVE SLEEP APNEA AND THE COMMERCIAL MOTOR VEHICLE DRIVER
When untreated, obstructive sleep apnea (OSA) in adults is associated with sleepiness, fatigue, sleep disturbance, snoring, apneas during sleep, systemic hypertension, type 2 diabetes mellitus, coronary artery disease, congestive heart failure, cardiac arrhythmias including atrial fibrillation, and premature death.1 The prevalence of OSA is conservatively estimated around 5% in the general adult population, with higher prevalence associated with male gender, increased weight, and advanced age.2,3 It is estimated that 13% of men and 6% of women between age 30 and 70 years have moderate to severe OSA.3 For body mass index (BMI) measurements of 40 kg/m2 or greater between age 50 and 70, it is estimated that over half of men (56.0%) and approximately one-third of women (33.5%) have moderate-to-severe OSA.3 Compared to general populations, OSA prevalence estimates for CMV drivers are increased, which may be affected by unique population characteristics such as higher proportion of males, obesity rates, and age distribution.4–6
There is concern about the interplay between OSA and motor vehicle crash (MVC) risk in the CMV driver. In general driving populations, OSA is associated with an increase in MVC risk and a comparable reduction associated with continuous positive airway pressure (CPAP) therapy; however, applicability to the CMV driver population is limited.7–13 Because of the increased risk of negative consequences in a crash involving a CMV driver due to complicating factors of operating a heavier vehicle, transporting passengers, or carrying hazardous materials, any potential safety risk is alarming.13,14 In the U.S., it is estimated that 12.0% of fatal crashes and 6.6% of non-fatal crashes involved at least one large truck or bus.15 Transportation and warehousing occupations have the second highest number and rate of fatal work injuries, with truck and passenger transport comprising 76% of these fatalities.16 Additionally, MVCs associated with commercial vehicles are much more likely to cause injury or death to the non-CMV drivers.17
Although the focus of this article is the CMV driver within the U.S., these concerns are of international concern as well. For North America, road transport of goods and passengers across the Canadian and Mexican borders is best addressed through international cooperation to standardize practices. A joint position paper by the Canadian Thoracic Society and the Canadian Sleep Society, for example, states a general agreement with a U.S. consensus recommendation.18 This same principle applies to all continents and nations involved in international commerce. The issue is complex and varies by country or region due to the unique intersections of governmental regulation, private industry, international trade, and healthcare resources.
OBSTRUCTIVE SLEEP APNEA ASSESSMENT, DIAGNOSIS, AND TREATMENT
In clinical settings, OSA assessment includes comprehensive evaluation of questionnaires, symptom report, medical history, and physical examination.19 When OSA is suspected, sleep testing provides objective diagnosis confirmation, severity assessment, and risk stratification. Within the clinical environment, assessment and treatment decisions include a combined assessment of OSA severity, subjective symptoms, and significant medical history findings.1,19 In occupational environments, self-report appears less reliable, which may be attributed to factors such as reduced symptom awareness and disincentives to pursing OSA evaluation due to concerns about missed work or financial burdens.8,20
Two clinical OSA questionnaires, the Epworth Sleepiness Scale (ESS) and the Berlin questionnaire (BQ) have been included in CMV driver OSA recommendations as part of a comprehensive risk assessment.14,21–23 Each has been studied in clinical and driving populations, but they have not been well studied in the CMV driver population.24 Because each questionnaire relies wholly or in part on patient reported symptoms, their role in an occupational setting may be limited to assessment of positive findings without drawing any further conclusions based on negative responses. Despite this limitation, there are advantages to using validated and standardized symptom assessment tools as part of a comprehensive evaluation.
The ESS assesses sleepiness via a patient-completed written questionnaire in which the patient rates their likelihood of dozing in eight situations rated on a Likert scale from zero to three, with a score greater than 10 considered significant.14,22 Despite its widespread use in clinical settings, it is unclear if the ESS reliably predicts crash or OSA risk in the CMV driver given limitations in occupational settings.6–8,20,25,26 In an occupational clinic setting, Talmage et al. report an inverse relationship between Epworth scores and OSA severity in contrast to patterns normally seen within clinical settings.14,25,27 Additionally, the ESS is neither sensitive nor specific for the diagnosis of OSA.27
The BQ also uses a written questionnaire, assessing a broader array of symptoms. Through responses to questions regarding snoring, tiredness, fatigue, falling asleep while driving, and hypertension, a weighted scoring algorithm assigns low- and high-risk OSA categories.23 The BQ has been validated in clinical populations and is recommended as a potential OSA screening tool but also relies on subjective patient report, and the scoring algorithm may be less practical in an occupational health environment.7,21,28,29
The STOP-Bang questionnaire has not specifically been studied in CMV driver populations,24 despite its close resemblance to published OSA screening recommendations and validation in clinical populations, specifically preoperative clinics.30–33 This may be partly an issue of timing, as the primary CMV driver OSA recommendations are from 2006 to 2012, during a time when studies assessing the STOP-Bang were emerging in publication.14,21,30,31,33 The mnemonic STOP-Bang assesses snoring, tiredness, observed apneas, blood pressure, body mass index, age, neck circumference, and gender, assigning one point for each positive finding up to a maximum score of eight with three or more indicating significant OSA risk. Although this tool also relies on symptom report, four criteria (B-a-n-g) can be obtained objectively through physical examination, and one (blood pressure or hypertension) through history and potentially physical examination when uncontrolled.30 The STOP-Bang has also been compared to the ESS and BQ in sleep clinic populations, showing higher sensitivity, odds ratio, and a greater area under the receiver operating characteristics curve, but low specificity.27,34
Recommendations for utilization of the physical examination for CMV drivers emphasize findings associated with increased OSA risk.14,21,33 This includes measurement of height, weight, neck circumference, and blood pressure with visualization of facial and airway anthropomorphic features offering an opportunity to assess objective risk factors for OSA without relying on the patient subjective report. Measurement of height, weight, and blood pressure are already included in FMCSA standards for medical assessment.35 Not required by the FMCSA, but included in expert recommendations, is an additional assessment for micrognathia, retrognathia, or narrowed posterior oropharynx.14,21,33 One method to assess the posterior oropharynx is through use of the Mallampati classification.33 With this method, the uvula and soft palate are visualized with the tongue extended without phonation. The structures visible are compared to a scale from 1 to 4 (or I to IV), with 1 representing a normal finding and 4 indicating the soft palate and uvula cannot be visualized.19,33 Mallampati class 2–4 have been associated with OSA; however, this relationship is best predicted when combined with BMI, gender, and age.36 The Friedman tongue position classification, a similar assessment to the Mallampati with the tongue in natural position using slightly modified numerical classes, is also associated with OSA risk.37
Historically, OSA has been diagnosed by the polysomno-gram (PSG), which remains the “gold standard” diagnostic tool; however, new diagnostic technologies have gained acceptance. The PSG is commonly performed in a sleep testing facility with a sleep technologist monitoring a minimum of 11 parameters including respiratory airflow, respiratory effort, oxygen saturation, electrocardiography, electroencephalography (EEG), body position, and muscle movements of the eyes, chin, and limbs from various recording sensors.14,20,21,38 Alternative diagnostic strategies, “home sleep apnea testing (HSAT),” enable OSA testing away from the sleep center without attendance and use fewer and simple sensors, hence offering the advantage of decreased test cost and increased testing access in appropriate patients.14,20,21,39–41 HSAT has become more common and accepted after approval by the Centers for Medicare and Medicaid Services (CMS) and subsequent commercial insurer emphasis as an alternative diagnostic tool for OSA.42–44 Clinical guidelines recommend HSAT can be considered for those deemed to be at high risk of having OSA without significant cardiac, pulmonary, or neurologic comorbidities.39,44 However, when using HSAT for OSA diagnosis, consideration must be given to the pretest and posttest probability of detecting OSA considering the individual circumstances of the patient undergoing evaluation.40 Because HSATs are performed without a technologist present, a mechanism for maintaining chain of custody is recommended for occupational assessment when identification verification of the individual undergoing testing is preferred.33,40,41 When HSATs are performed without electroencephalography (EEG), objective assessment of time slept is not available, potentially affecting diagnostic accuracy.20,39–41 Given the potential limitations of HSAT impacting CMV driver testing,41 individualized clinical assessment of OSA pretest and posttest probability is particularly important in this population and may necessitate further diagnostic confirmation with PSG, particularly in the setting of a “negative” HSAT result.
The severity of OSA is commonly assessed using a calculation of the number of respiratory events per hour.1 A common calculation is the apnea hypopnea index (AHI), which is the sum of apneas and hypopneas divided by the time slept. Sleep time is determined by EEG which is a standard recording on PSG.1,14,38 When sleep time cannot be derived from EEG recordings, the respiratory event index (REI) is reported utilizing device recording time in the denominator as a surrogate for estimating amount of sleep per the diagnostic criteria established by the American Academy of Sleep Medicine (AASM).1,40 Historically, the respiratory disturbance index (RDI) has been utilized for severity assessment, but can represent more than one calculation.44 Per AASM standards, RDI calculation requires EEG derived sleep time as the denominator.1,38 In 2008 CMS adopted an alternative definition in which RDI represents the same calculation as REI on HSAT when recording time is used in lieu of EEG derived sleep time.38,42 Increased AHI is associated with increased crash risk and recommended for use in risk stratification of the driver diagnosed with OSA.7,8 Additionally, nadir oxygen saturation is associated with increased crash risk, however recommendations do not currently provide specific thresholds to identify significant oxygen levels for CMV driver OSA risk assessment.7,8
Positive airway pressure (PAP) therapy including CPAP, bi-level PAP, and auto-titrating PAP (aPAP) is a common treatment for OSA, particularly for moderate-to-severe disease.44 CPAP has been shown to reduce abnormal sleepiness levels in as little as one week with symptom improvements correlating to amount of CPAP usage in a dose-dependent fashion.10,45,46 Titration in the home using an aPAP machine is becoming common in appropriate populations, reducing the utilization of PSG with technologist titration of CPAP.14,21,33,39–41 Studies suggest similar outcomes when comparing aPAP to CPAP for adherence to therapy and improvement in sleepiness as measured by the ESS in select clinical populations.47,48 PAP usage for 4 or more hours for at least 70% of nights is a commonly used cut-point for assessing adherence, initially established in research settings and later adopted by CMS as a criterion for continuation of therapy coverage.49,50 The use of 4 hours as a defining threshold may be problematic when applied to the CMV driver population without strong evidence to support this particular amount of use versus another threshold. However, practicality must also be considered as commercially produced software for data analysis and reporting are typically used to generate printed objective reports of PAP usage. Currently, there is no standardized data capture, analysis, and reporting system commonly in use outside of these proprietary programs, requiring significant cooperation between competing companies and investment of resources to standardize reporting specific to the CMV driver population. With these considerations in mind, this threshold has also been recommended as a minimum standard for assessing adherence in the CMV driver when determining fitness for duty, although longer usage during any sleep periods should be advised to the CMV driver to optimize benefit.14,21,33
OSA treatments in addition to PAP therapy are available to the CMV driver including weight loss or airway modification surgery. An objective assessment of treatment efficacy after these interventions is recommended. The delay this imposes limits their utilization in CMV drivers who are required to have treated OSA to maintain their medical certification.14,21,33 PAP therapy is often the more practical first-line therapy for maintaining a CMV driver in-service or shortening their time out of service. For the purposes of treatment in CMV drivers deemed to be in higher risk categories, use of dental appliances are problematic due to limited data on crash risk assessment and limitations in treatment adherence verification, and therefore are not a currently recommended treatment option.14,21,33 Newer technologies exist to enable objective adherence monitoring of dental appliances and further study of their role in CMV drivers is recommended.21,51 However, with a current paucity of literature specifically on CMV drivers and use of oral appliances, their role remains unclear as monitoring technology continues to evolve.52
REGULATION OF COMMERCIAL MOTOR VEHICLE DRIVERS
Within the United States Department of Transportation (DOT) the FMCSA develops and regulates CMV drivers.53 The mission of the FMCSA is to “reduce crashes, injuries, and fatalities involving large trucks and buses” through activities ranging from promoting safety awareness and equipment or technology enhancement to safety regulation development and enforcement.53,54 The Medical Program Division is responsible for medical regulations, guidelines, and policies, which set standards for determining if a driver is physically qualified to operate a CMV and establishing standards for those performing the examinations commonly known as a “DOT physical.”55 Medical certification is required for drivers operating motor vehicles meeting certain criteria defined by vehicle weight, hazardous materials, or number of passengers and distance transported.56 Employers who choose to develop their own policies and procedures for safety-sensitive positions, even when not specifically regulated by the FMCSA, (ex: rail transport) may choose to use FMCSA regulations and recommendations as guidance, requiring their employees to undergo medical assessment similar to the FMCSA process.
In the U.S. Code of Federal Regulations (CFR), CMV driver physical examination standards are found within title 49 (transportation), part 391 (FMCSA) subpart E (physical qualifications and examinations).57 Per 49 CFR 391.41 (b) (5) a driver is qualified to drive a commercial motor vehicle (CMV) if the driver “has no established medical history or clinical diagnosis of a respiratory dysfunction likely to interfere with his/her ability to control and drive a commercial motor vehicle safely.”57 There is not specific reference to OSA, however there are specific standards for other medical disorders which can increase the risk of sudden driver incapacitation such as diabetes, hypertension, epilepsy, and cardiovascular disorders. Section 49 CFR 391.43 provides standards for the medical examination certification process using the provided medical examination report form and standards for the medical examiner including training, licensure, and registration requirements.35,57 On the medical examination report form, the health history section asks the driver to indicate “yes” or “no” to a series of medical history and symptom questions and provide their signature at the bottom certifying that the information is “complete and true.”35 In 2000 this section was modified to include “sleep disorders, pauses in breathing while asleep, daytime sleepiness, loud snoring” in an effort to identify those with sleep disorders.58
The FMCSA Medical Program Division develops and implements policies utilizing a number of resources. To establish the scientific knowledge base, comprehensive literature searches and analysis reports are contracted by the FMCSA.59,60 For expertise in a specific body system or disease, a Medical Expert Panel (MEP) may be convened periodically to advise the FMCSA within their particular area of expertise.60 Routinely, the panel of physicians who comprise the Medical Review Board (MRB) meets to evaluate and recommend standards on CMV driver medical qualification to the FMCSA.59,61 Additionally, the FMCSA receives recommendations from the Motor Carrier Safety Advisory Committee (MCSAC) comprised of members representing industry, labor, safety enforcement and safety advocacy sectors.61
DEVELOPING RECOMMENDATIONS FOR COMMERCIAL MOTOR VEHICLE DRIVERS
In 1988, the DOT convened a conference of experts to revise recommendations for “neurologic disorders” followed by recommendations for “pulmonary disorders” in 1991; each also addressed sleep disorders.63,64 Over time, these recommendations for OSA and CMV operators became outdated compared to advances within sleep science and clinical practice. In response, an independent joint task force (JTF) composed of experts in sleep and occupational medicine was formed by three interested societies. In 2006, the panel published their findings based on review of the scientific literature which included recommendations regarding OSA screening, diagnosis, and treatment.14 Unlike standards and recommendations up to this point, which relied primarily on the CMV driver to affirm or deny significant symptoms and medical history, the JTF added objective findings obtained largely through physical examination. These included medical examiner assessment of blood pressure, body mass index (BMI), neck circumference, and posterior oropharynx examination.14
In 2007, a report commissioned by the FMCSA on OSA and CMV driver safety was completed.8,59 Based on review of this evidence summary, the MEP of sleep experts presented medical consensus recommendations to the FMCSA for OSA screening, diagnosis, and treatment in 2008.21 In 2011, the evidence review was updated, responding to additional questions pertaining to OSA screening and diagnosis.20 Then, in 2012, detailed recommendations on OSA screening, diagnosis and treatment were submitted to the FMCSA jointly by the MCSAC and MRB.33
After 5 years of gathering scientific evidence and expert opinion, the FMCSA published proposed OSA recommendations in the Federal Register seeking public comment.65 These proposed recommendations were promptly withdrawn without explanation within the public record, a mere one week after publication, but remain accessible for reference.66 In 2013, Congress passed H.R.3095 and S 7213 which became Public Law 113-45. This legislation requires the Secretary of Transportation to only implement or enforce a requirement pertaining to obstructive sleep apnea pursuant to formal rulemaking proceedings.67 Formal rulemaking is a defined mechanism within the federal regulatory process that appears to have significantly slowed the momentum for OSA-related action as no further public action has been taken since 2013. Perhaps with recent efforts on the part of the National Transportation Safety Board, which identified sleep disorders screening as a specific area of concern on their 2015 “top 10 most wanted transportation safety improvements list,”69 there will be more action in the future, but the momentum for this remains uncertain.
PUBLISHED OBSTRUCTIVE SLEEP APNEA RECOMMENDATIONS FOR COMMERCIAL MOTOR VEHICLE DRIVERS
The recommendations of the JTF, MEP, and MCSAC-MRB provide guidance on OSA, screening, risk assessment, and treatment in absence of updated federal standards.14,21,33 Although officially withdrawn from the federal register, the FMCSA recommendations proposed remain accessible and provide insight into the standards under consideration by the FMCSA in 2012; therefore, they are included for reference.65,66 In general, these recommendations agree in the comprehensive assessment of objective findings, detailed symptoms, medical history, and crash history; however, the specifics of their recommendations vary. A comparison of key elements of OSA screening recommendations is presented in Table 1.14,21,33,65
Table 1.
Published recommendations for obstructive sleep apnea risk assessment and screening.
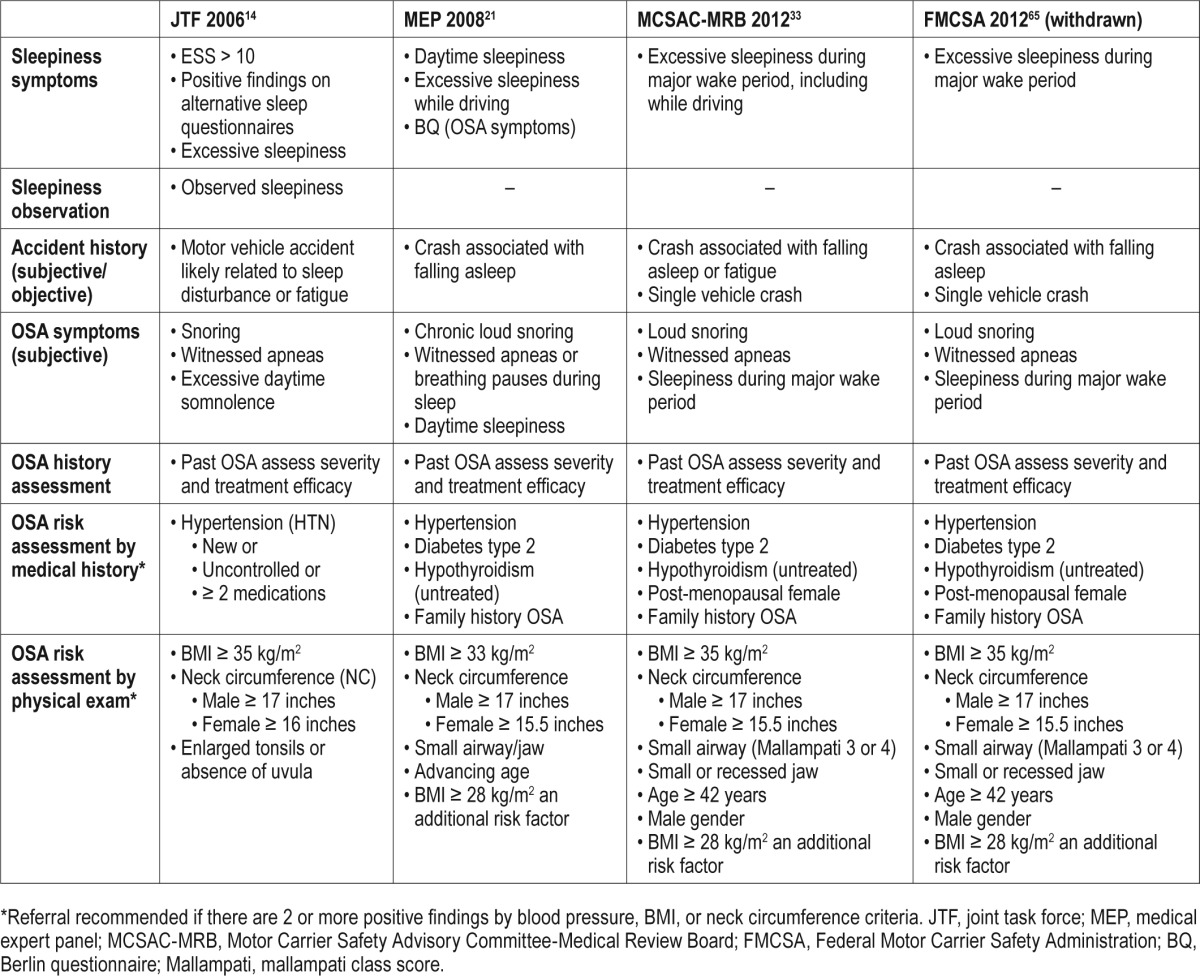
For OSA risk evaluation, the JTF added further assessment of sleepiness (including the ESS), crash history, neck circumference, oropharyngeal anatomy, and hypertension. For any positive findings in OSA associated symptoms, sleepiness, crash history, or previously diagnosed OSA, referral for detailed evaluation was advised. If at least two positive findings were noted when assessing hypertension, neck circumference, or obesity detailed in Table 1, referral was also advised.14 When the MEP published their recommendations for OSA screening, the BMI and neck circumference thresholds were lowered.21 They provided additional recommendations for patient history and physical examination evaluation, including the use of the BQ as a standardized OSA screening tool. The MCSAC-MRB recommendations showed many similarities to the past recommendations using the JTF recommendation for BMI and the MEP recommendation for neck circumference thresholds. Symptom assessment was similar, including crash history, sleepiness, and OSA-associated symptoms; however, they did not provide a recommendation for a specific OSA screening questionnaire.33 The FMCSA proposed recommendations essentially mirrored the MCSAC-MRB recommendations as detailed in Table 1.65
Of note, there appears to be inconsistency in the use of the symbols in early publications representing greater than or equal to (≥) versus greater than (>). Within the JTF recommendations,14 this is found with neck circumference recommendations when comparing the JTF article text to table 4 within the article. For purposes of our summary, we chose the recommendations listed in the text (Barbara Phillips, personal communication, 2015, Jan 19). Within the MEP recommendations,21 a similar discrepancy is found with BMI thresholds, we choose to include what was listed under guideline 4 within their publication.
Once testing is completed, the recommendations rely on a combination of medical history, symptoms, and crash history combined with OSA severity to assess OSA risk and advise treatment as detailed in Table 2.14,21,33,65 Over time, HSAT and aPAP have become more common, which is reflected in later recommendations.
Table 2.
Published recommendations for obstructive sleep apnea diagnosis and treatment.
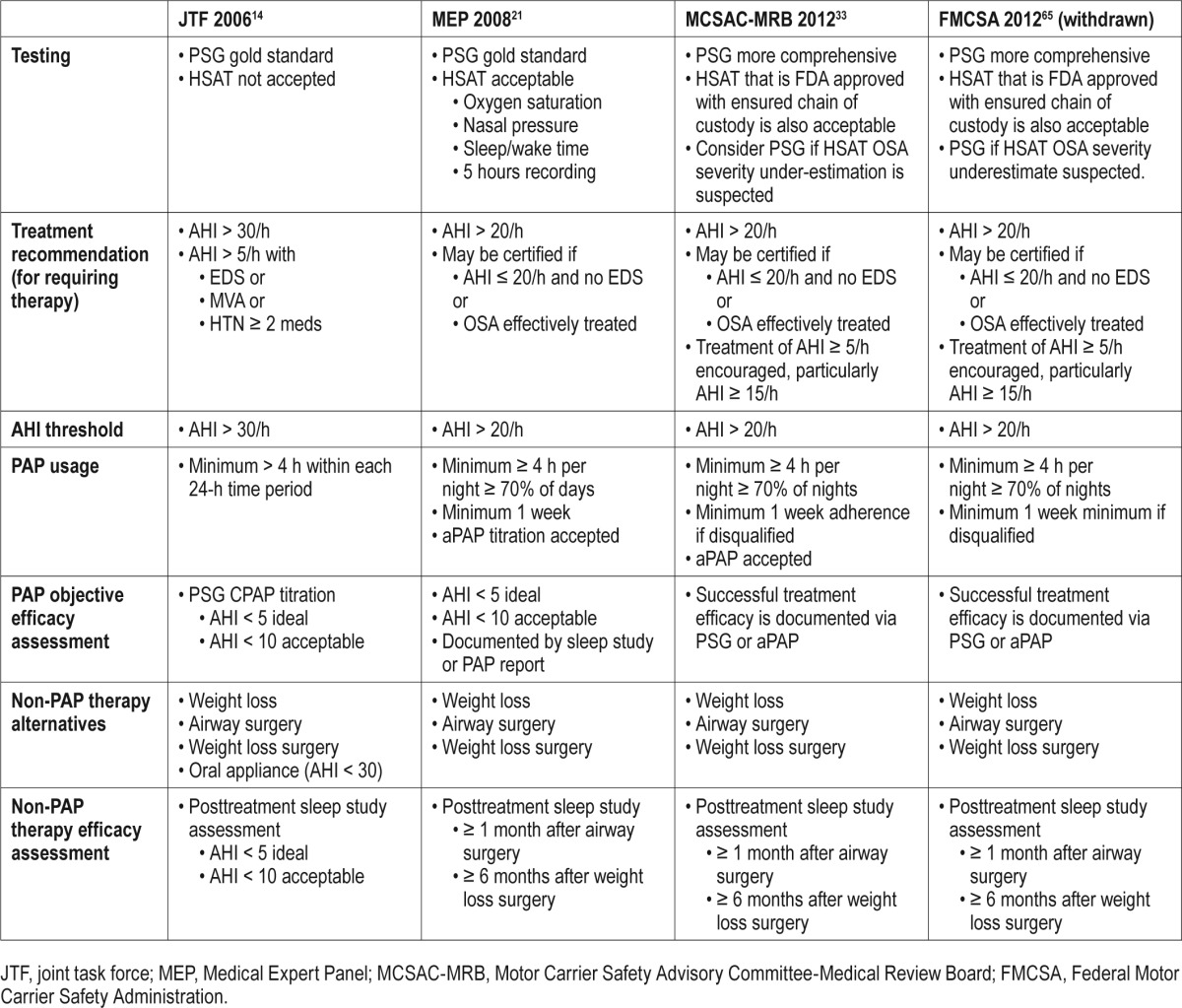
For OSA testing, the earliest publication (JTF) does not consider HSAT as acceptable; however, the MEP, MSCAC-MRB, and FMCSA do provide allowances for HSAT while recognizing potential limitations in this diagnostic tool. The MEP provides recommendations for the channels monitored during HSAT, while the later recommendations include a requirement to utilize U.S. Food and Drug Administration (FDA)-cleared devices with a chain of custody mechanism and again note potential underestimation of OSA severity with HSAT.
In each recommendation, minimum AHI thresholds are provided for both OSA risk stratification to define when treatment should be required and to determine efficacy of treatment. No separate guidance for HSAT thresholds are provided in these recommendations. In all cases, decisions about therapy were ultimately left to the treating clinician to consider cases in which a driver may benefit from PAP therapy at lower AHI values, particularly based on medical comorbidities or concern for sleepiness or any history of a significant crash. When establishing a threshold in which a requirement for treatment is recommended, the JTF used a threshold of AHI greater than 30, which was lowered to AHI greater than 20 events per hour in newer recommendations. The criteria for assessing efficacy of treatment changes over time as well, with lower numeric thresholds in earlier publications. Additional guidance was given (excluding the JTF publication) for timing of post-surgical assessment. Within the JTF publication, there is inconsistency in the use of symbols representing less than or equal to (≤) versus less than (<) for thresholds to determine PAP efficacy, we chose to use less than (<) 5 and 10 as thresholds within Table 2.
Assessment of PAP therapy includes a minimum amount of time when treatment is used, using data objectively recorded and reported from the machine. Usage more than 4 hours per each 24 hour time period was recommended by the JTF while this was changed to 4 hours or more for at least 70% of days in the other recommendations. While the JTF did not define a minimum time period to measure adherence to therapy, the MEP, MCSAC-MRB, and FMCSA specified a minimum of one week. In the MEP column, we have listed 4 hours or more as the threshold as this is what is reported via the most common PAP machine adherence reports rather than greater than 4 hours as listed in their publication.
ASSESSMENT OF CURRENT RECOMMENDATIONS
Three studies have been published assessing the implementation of more comprehensive OSA risk assessment in CMV drivers in an occupational clinic setting in the U.S.25,26,70 An additional study has been published assessing efficacy of driver self-reported symptoms, medical history, and anthropomorphic measures in an employer-based OSA assessment program.6 Each of these studies report impressive findings with positive predictive values (PPV) ranging from 79% to 100% utilizing combined objective and subjective OSA risk assessment criteria, despite limitations in study designs. This has been the experience of one of our authors assessing CMV drivers after referral by their DOT medical examiner to a sleep clinic with PPV of approximately 80%.71 These findings are particularly remarkable when compared to the diagnosed OSA, which missed detection using the current FMCSA medical examination report form. Talmage and colleagues found that none of their drivers provided a “yes” response to the question about “sleep disorders, pauses in breathing while asleep, daytime sleepiness, loud snoring” in the 127 newly diagnosed with OSA.25 For those drivers already on PAP, they reported that not all drivers responded yes to this question despite a known diagnosis of OSA.25 Parks et al. reported they also detected unreported OSA diagnosis until the driver was advised of the need for a sleep study, which has also been our clinical experience.26
SUMMARY AND CONCLUSIONS
Adopting comprehensive screening assessment appears effective in increasing detection of OSA. In our clinical experience, we are seeing increased implementation of these recommendations in occupational health clinics and employer-initiated programs and consequently more referrals to the sleep center. Implementing consensus-based recommendations into practice prior to establishing a regulatory mandate can provide valuable feedback to federal regulators. But, it also brings uncertainty for the CMV driver as they navigate employer, medical examiner, and clinician practices that may not align with each other.
In clinical practice, the challenge remains integrating recommendations into practice as OSA diagnosis and treatment technologies evolve, perhaps more rapidly than regulatory agencies can respond. HSAT and aPAP therapy have become options to potentially reduce diagnostic testing and treatment costs for CMV drivers and their medical insurers, but have limited scientific study in the CMV driver population. Additionally, when a CMV driver denies OSA symptoms, navigating insurance pre-authorization for sleep testing can be challenging, despite the high likelihood of a driver having OSA based on objective risk factors.43 With the recent publication of the International Classification of Sleep Disorders, Third Edition, the modified criteria defining OSA can impact diagnostic criteria within the CMV driver population.1 When there are less than 15 obstructive breathing events per hour, the diagnosis is established with an OSA associated comorbidity or related symptom.1 In a population that may under-report symptoms, meeting this diagnostic criterion may be a challenge. Also, if HSAT technology underestimates the disordered breathing event rates, this affects the ability to meet diagnostic criteria.40,41 When the purpose of OSA screening is early identification of OSA and potential risk mitigation, falling below diagnostic criteria on symptom assessment can be limiting, as a CMV operator may continue with an unrestricted 2-year medical certification, rather than being limited to 1 year once OSA is diagnosed.
Much work has been done to provide a foundation of knowledge for clinicians, but some questions remain. For OSA screening, the frequency for reassessment with a sleep study has not been proposed, when CMV drivers will return in subsequent years with similar OSA risk factors, advancing age, and potential progression of sleep-disordered breathing.72 When using a sleep study to stratify OSA risk for those with an AHI of 20 or less, there is no defined standard for incorporating nadir oxygen saturation, despite reports of the association between oxygen saturation and crash risk,8 as well as oxygen desaturation index and progression of sleep disordered breathing.72 PAP therapy is encouraged when the AHI is lower if there may be a benefit to the driver; however, it is not clear if this driver is then held to the same minimum adherence standard as those falling into the category of requiring OSA treatment. Additionally, there have been no detailed recommendations regarding objective assessment of weight loss and weight gain in CMV drivers already diagnosed with OSA when considering OSA risk assessment.
Beyond the scope of this article are the potential legal implications of OSA screening, evaluation, and treatment of CMV drivers. Federal regulations can standardize expectations and help level the playing field for CMV drivers, employers, and medical evaluators. However, the current lack of comprehensive regulatory guidance does not lessen the medical and legal standards of care to which the sleep specialist or certified medical examiner is responsible in a medico-legal environment. Knowledge and understanding of medical consensus recommendations and regulatory requirements provides a foundation for medical-decision making and counseling by the sleep specialist to the individual patient.
The challenge going forward for sleep researchers and clinicians is to better understand the relationship between OSA and driving impairment specifically in the CMV driver population. Although it is clear that OSA has historically been under-diagnosed in this group, the diagnosis of OSA alone does not reliably predict functional outcomes such as impaired driving performance; rather it casts a wide net for disease detection to potentially impact a smaller number of CMV drivers who pose a higher safety risk. Research is ongoing in this area; however, broad implementation of driving performance evaluation technology across the U.S. would be a large undertaking.
It is the hope of many sleep professionals that the FMCSA will continue to develop regulatory guidance for OSA evaluation in CMV operators, navigating the rule-making process efficiently. Until this occurs, we rely on consensus-based recommendations to guide our practice. Continued research and understanding of the impact these recommendations have in clinical practice is crucial to help balance safety concerns with the potential effects of regulatory change on the various stake-holders involved.
RECOMMENDATIONS
Significant time has passed since the Joint Task Force published the first consensus recommendations regarding CMV drivers in 2006.12 The DOT, FMCSA, and NTSB have dedicated significant resources to scientific investigation, analysis, and recommendations regarding OSA screening, risk stratification and treatment of CMV drivers but currently appear to be stuck in a holding pattern without significant public action for over a year.8,20,21,33,59,65–67 Additionally, sleep research and the clinical practice of sleep medicine has changed significantly since 2006, including increased utilization of home-based diagnostic testing (HSAT) and PAP therapy (aPAP). Furthermore, sleep science continues to evolve and broaden our understanding of issues specific to the CMV driver population.
However, the sleep specialist is faced with the reality of clinical practice in which CMV drivers are presenting as patients today and will continue to present for clinical evaluation and treatment in the future. These patients come from various referral sources including the certified medical examiner, employer, primary care provider or self-referral. In our opinion, it is our responsibility as sleep professionals to identify professional drivers within the clinical setting and counsel them on screening recommendations whether they are referred specifically for this purpose or not. They present with needs ranging from OSA screening, comprehensive sleep disorders assessment, post-accident evaluation, and risk assessment with subsequent treatment discussion, initiation, and monitoring. With this in mind, we offer proposed recommendations to the sleep specialist for clinical screening for OSA and screening for associated sleepiness in CMV drivers based on our individual analysis of key published consensus recommendations and subsequent relevant studies in publication; our analysis is provided in context of our own clinical experience, current health-care practice, and structures. They are intended to provide a practical guide to the sleep specialist in clinical practice and supplement those recommendations already published regarding OSA screening, assessment and treatment without acting necessarily as a replacement for these recommendations. Of particular note, these recommendations focus primarily on OSA screening, assessment, and treatment considerations; we do not offer recommendations for comprehensive sleep disorders screening or driving performance evaluation nor do we offer comprehensive opinions on OSA treatment beyond what is included in previously published recommendations. When there is not already consensus in the recommendations, we take the approach of considering the more strict threshold for screening in the sleep clinic environment, recognizing that the certified medical examiner or employer may choose a different approach as they weigh other factors in their policy development and medical decision-making. Ultimately, it is the clinical judgment of the sleep specialist that determines exact OSA screening and evaluation practices applied individually to a patient, considering OSA screening principles, consensus-based recommendations, and the specific patient presentation, history, and clinical evaluation findings.
In Table 3, we have provided an overview of the initial clinical assessment focused on OSA risk assessment and subjective assessment of associated sleepiness based largely on recommendations detailed in Table 1. This is intended to serve as a guide in considering paperwork that might be utilized to gather data prior to face-to-face evaluation of the patient who is a CMV driver. The sections are separated into those obtained through subjective report versus those which can be obtained with more objective techniques.
Table 3.
Author recommendations for sleep specialist obstructive sleep apnea (OSA) clinical assessment.
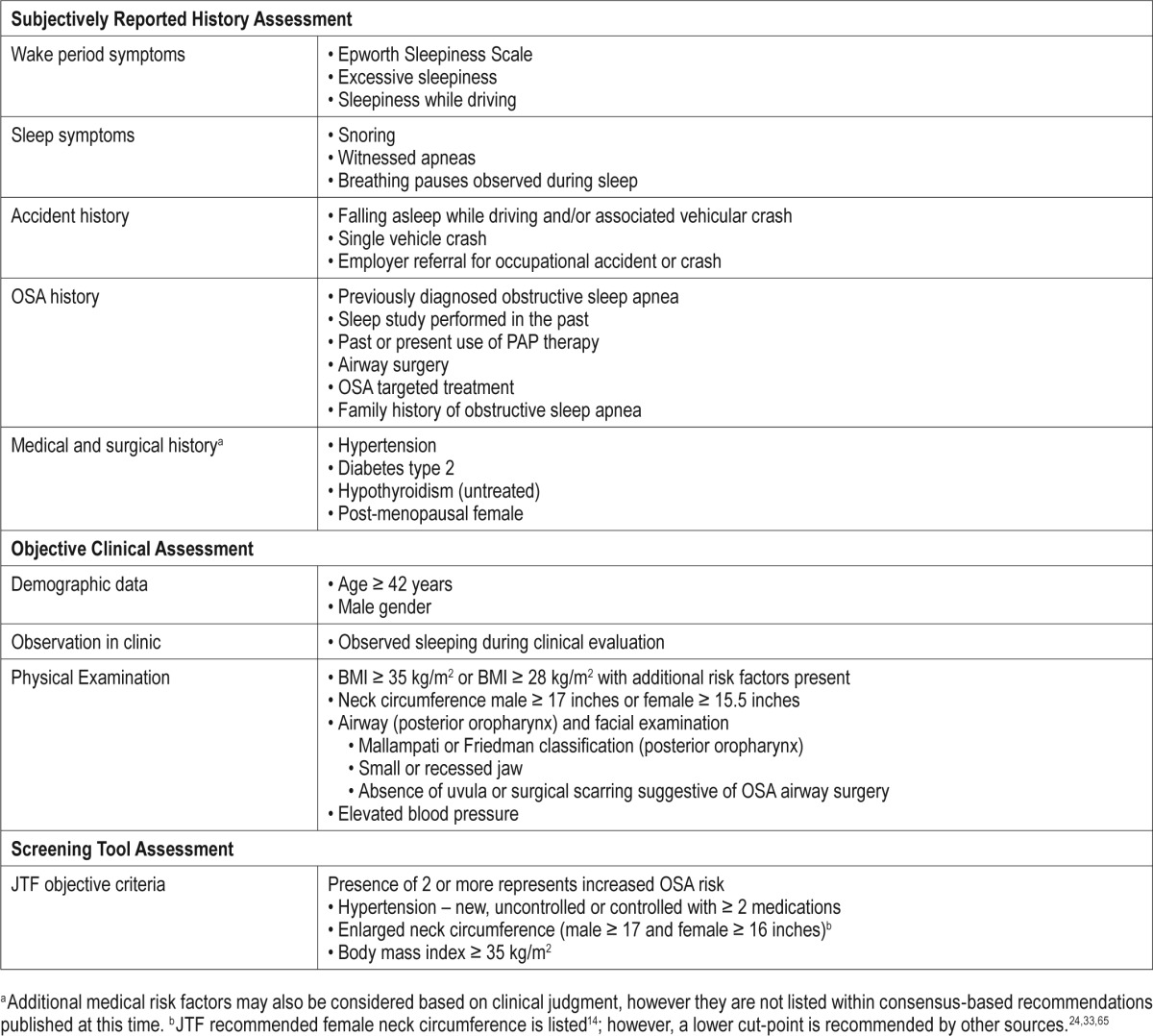
We recommend a standardized assessment of sleepiness and potential driving risk. While it is clear from published studies, that this may be under-reported in the CMV population, documentation of this assessment remains a critical piece of a comprehensive evaluation in all CMV drivers. We recommend including a standardized assessment of sleepiness such as the Epworth Sleepiness Scale. We do note the inherent limitations of this subjective screening tool, but there are benefits to using a standardized assessment of sleepiness in the small number of CMV drivers who may self-report these symptoms. In assessing potential risk, at a minimum the driver should be queried regarding any history of falling asleep while driving or any prior accident that could be reasonably attributed to falling asleep or an unexplained lapse in attention such as a single motor vehicle collision.
For OSA specific assessment, we suggest further investigation into both wake period and sleep associated symptoms suggestive of OSA as listed in Table 3. We recognize that the sleep specialist will likely include a more thorough sleep disorder associated symptom assessment; therefore, our recommendations serve merely as a guide for minimum baseline assessment. The CMV driver should also be questioned regarding any known history of OSA; however, our own clinical experience leads us to recommend additional questions which can be helpful in this assessment, such as inquiring about any past sleep studies performed, past recommendations and/or prescription of PAP therapy or prescription of other OSA targeted therapies.
When considering clinical assessment of OSA risk based on criteria that do not rely primarily on the CMV driver report, we focus on the physical examination and measurements obtained as part of this assessment. These recommendations are consolidated from those listed in Table 1 with the addition of airway assessment for evidence of past airway surgery. We also list both the Friedman classification as an alternative to the Mallampati classification, leaving this decision to the discretion of the sleep specialist.
At the end of Table 3, we also summarize the key objective assessment findings recommended by the JTF consensus statement.14 Based on the 3 studies in CMV drivers in occupational health clinic settings, these criteria appear to have a high positive predictive value for OSA diagnosis.25,26,70 Our clinical experience echoes the findings of these studies, and we find the overwhelming majority of drivers qualify for OSA screening based on the objective criteria recommended by the JTF, rather than subjective report such as the questions currently in use on the FMCSA required medical examination report form.35 We therefore highlight the JTF criteria as a potential simple screening criteria for a quick first-line assessment of OSA risk in conjunction with additional comprehensive assessment by the sleep specialist. Furthermore, these three studies are helpful in communicating potential OSA risk to the CMV driver who meets JTF screening criteria; they can be advised that based on these criteria alone, it is reasonable to anticipate approximately 80% or more of those undergoing evaluation will be diagnosed with OSA.25,26,70 For example, a patient seeking employment as a CMV operator may be required by their potential employer to qualify for an unrestricted medical certification, meaning they cannot have diagnosed OSA. If this patient has very limited financial resources, knowledge of the significant chance that they will be diagnosed with OSA provides them with useful information in deciding whether they wish to financially invest in sleep apnea testing. The role of other assessment techniques and technology for OSA screening and diagnosis remains an area of interest and further study.24 Clinical tools such as the STOP-Bang or the Berlin Questionnaire may have relevance, but need studies within the CMV driver population. At this time, we chose to not include these tools in our suggestions based on the limitations in evidence or consensus to support their inclusion. Given the high degree of overlap between the STOP-Bang questionnaire and JTF consensus criteria, research investigation of this tool specifically within a CMV population would be beneficial.
When the CMV driver is found to have sufficient OSA risk or history of significant OSA by the sleep specialist, further evaluation should be recommended and documented within the medical record. Table 4 provides basic recommendations for continued evaluation beyond initial clinical screening and assessment. It is important to note that the certified medical examiner is ultimately responsible for determining if an evaluation continues while the driver remains in service or if there is reason to not renew their medical certification awaiting further evaluation. However, given the thorough history and examination subsequently performed by the sleep specialist, it is possible for additional data to be obtained which may influence the current service status of the CMV driver medical certification, and communication between the sleep specialist and certified medical examiner should be considered. Sleep specialists must also be mindful of any state laws that may apply to commercial drivers who appear to have risk for driving impairment and their individual duty to counsel the driver if their assessment indicates the driver should abstain from driving, both for commercial and non-commercial purposes.
Table 4.
Obstructive sleep apnea (OSA) evaluation, testing, and treatment considerations for the sleep specialist.
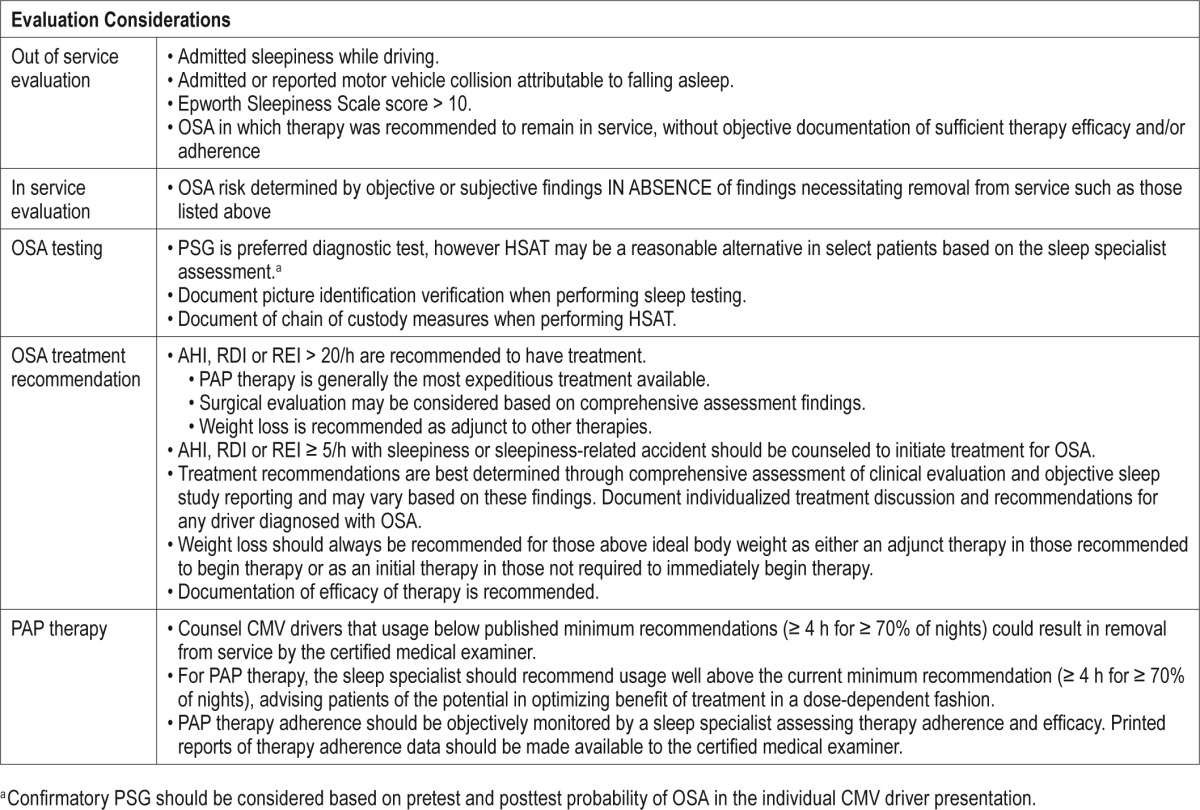
The utilization of PSG versus HSAT in the CMV driver population is a topic that is beyond the focus of this paper, as we recognize the potential limitations of HSAT that deserve further study in occupational settings.41 Therefore, in our suggestions, we rely on consensus-based recommendations but acknowledge that diagnostic decisions are not made in a vacuum and require a balance of the potentially conflicting viewpoints of sleep specialists with healthcare insurance policies and other financial constraints that influence clinical practice and patient preference.
Lastly, regarding treatment, we must consider the paucity of evidence in many areas surrounding OSA treatment in the CMV driver that require further investigation. Some OSA treatment recommendations rely on extrapolation from clinical populations without dedicated study to CMV drivers such as surgical intervention or oral appliances. Additionally, we need further clarification in what defines sufficient PAP therapy adherence. In practicality, however, patients are initiating treatment today and require counseling from sleep specialists regarding the role of treatment, potential benefits, and anticipated requirements from the certified medical examiner.
While the screening methods recommended may not capture all CMV drivers with OSA,73 they are important initial steps in addressing concerns about under-diagnosed OSA in this population. Compared to current requirements, they significantly increase detection of OSA, therefore providing an opportunity to discuss and offer treatment to the individual patient. However, there is much work still to be done to understand the impact of these efforts to both diagnose and treat OSA on public safety, CMV driver health and the commercial driving industry.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. Collop receives royalties from UpToDate. Dr. Colvin has indicated no financial conflicts of interest.
ABBREVIATIONS
- AHI
apnea-hypopnea index
- aPAP
auto-titrating positive airway pressure
- BMI
body mass index
- BQ
Berlin Questionnaire
- CFR
Code of Federal Regulations
- CMS
Centers for Medicare and Medicaid Servies
- CMV
commercial motor vehicle
- CPAP
continuous positive airway description
- DOT
Department of Transportation
- EEG
electroencephalography
- ESS
Epworth Sleepiness Scale
- FDA
Food and Drug Administration
- FMCSA
Federal Motor Carrier Safety Administration
- h
hour(s)
- HSAT
home sleep apnea test
- JTF
Joint Task Force
- Mallampati
mallampati class score
- MCSAC
Motor Carrier Safety Advisory Committee
- MEP
Medical Expert Panel
- MRB
Medical Review Board
- MVC
motor vehicle crash
- OSA
obstructive sleep apnea
- PAP
positive airway pressure
- PPV
positive predictive values
- PSG
polysomnogram
- RDI
respiratory distrurbance index
- REI
respiratory event index
REFERENCES
- 1.American Academy of Sleep Medicine. 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014. International classification of sleep disorders. [Google Scholar]
- 2.Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165:1217–39. doi: 10.1164/rccm.2109080. [DOI] [PubMed] [Google Scholar]
- 3.Peppard PE, Young T, Barnet J, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177:1006–14. doi: 10.1093/aje/kws342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pack AI, Maislin G, Staley B, et al. Impaired performance in commercial drivers. Am J Respir Crit Care Med. 2006;174:446–54. doi: 10.1164/rccm.200408-1146OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Howard ME, Desai AV, Grunstein RR, et al. Sleepiness, sleep-disordered breathing, and accident risk factors in commercial vehicle drivers. Am J Respir Crit Care Med. 2004;170:1014–21. doi: 10.1164/rccm.200312-1782OC. [DOI] [PubMed] [Google Scholar]
- 6.Berger M, Varvarigou V, Rielly A, Czeisler CA, Malhotra A, Kales SN. Employer-mandated sleep apnea screening and diagnosis in commercial drivers. J Occup Environ Med. 2012;54:1017–25. doi: 10.1097/JOM.0b013e3182572e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tregear S, Reston J, Schoelles K, Phillips B. Obstructive sleep apnea and risk of motor vehicle crash: systematic review and meta-analysis. J Clin Sleep Med. 2009;5:573–81. [PMC free article] [PubMed] [Google Scholar]
- 8.Tregear SJ, Tiller M, Fontarrosa J, Price N, Akafomo C. McLean, VA: Manila Consulting Group; 2007. Executive summary obstructive sleep apnea and commercial vehicle driver safety [Internet] [cited 2015 Feb 11]. Available from: http://ntl.bts.gov/lib/30000/30100/30187/Final_Sleep_Disorders_Evid_Report_Vol._1.pdf. [Google Scholar]
- 9.Ellen RB, Marshall SC, Palayew M, Molnar FJ, Wilson KG, Man-Son-Hing M. Systematic review of motor vehicle crash risk in persons with sleep apnea. J Clin Sleep Med. 2006;2:193–200. [PubMed] [Google Scholar]
- 10.Tregear S, Reston J, Schoelles K, Phillips B. Continuous positive airway pressure reduces risk of motor vehicle crash among drivers with obstructive sleep apnea: systematic review and meta-analysis. Sleep. 2010;33:1373–80. doi: 10.1093/sleep/33.10.1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hiestand D, Phillips B. Obstructive sleep apnea syndrome: assessing and managing risk in the motor vehicle operator. Curr Opin Pulm Med. 2011;17:412–18. doi: 10.1097/MCP.0b013e32834b96a4. [DOI] [PubMed] [Google Scholar]
- 12.Meuleners L, Fraser ML, Govorko MH, Stevenson MR. Obstructive sleep apnea, health-related factors, and long distance heavy vehicle crashes in Western Australia: a case control study. J Clin Sleep Med. 2015;11:413–18. doi: 10.5664/jcsm.4594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karimi M, Hedner J, Häbel H, Nerman O, Grote L. Sleep apnea related risk of motor vehicle accidents is reduced by continuous positive airway pressure: Swedish traffic accident registry data. Sleep. 2015;38:341–9. doi: 10.5665/sleep.4486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hartenbaum N, Collop N, Rosen IM, et al. Sleep apnea and commercial motor vehicle operators. J Occup Environ Med. 2006;48:S4–37. doi: 10.1097/01.jom.0000236404.96857.a2. [DOI] [PubMed] [Google Scholar]
- 15.U.S. Federal Motor Carrier Administration. Washington DC: U.S. Federal Motor Carrier Safety Administration [Internet]; 2014. Pocket guide to large truck and bus statistics. [cited 2015 Feb 12]. Available from: http://www.fmcsa.dot.gov/sites/fmcsa.dot.gov/files/docs/FMCSA Pocket Guide to Large Truck and Bus Statistics - June 2014 Version.pdf. [Google Scholar]
- 16.U.S. Bureau of Labor Statistics. Washington DC: U.S. Department of Labor, Bureau of Labor Statistics; 2014. Census of fatal work injuries (preliminary data 2013)[Internet] [cited 2015 Feb 12]. Available from: http://www.bls.gov/iif/oshwc/cfoi/cfch0012.pdf. [Google Scholar]
- 17.Bjornstig U, Bjornstig J, Eriksson A. Passenger car collision fatalities—with special emphasis on collisions with heavy vehicles. Accid Anal Prev. 2008;40:158–66. doi: 10.1016/j.aap.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 18.Ayas N, Skomro R, Blackman A, et al. Obstructive sleep apnea and driving: a Canadian Thoracic Society and Canadian Sleep Society position paper. Can Respir J. 2014;21:114–23. doi: 10.1155/2014/357327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cao M, Guilleminault C, Kushida C. Clinical features and evaluation of obstructive sleep apnea and upper airway resistance syndrome. In: Kryger MH, Roth T, Dement WC, editors. Principles and practice of sleep medicine. 5th ed. St. Louis, MO: Elsevier; 2011. [Google Scholar]
- 20.Williams JR, Amana A, Tregear SJ. McLean, VA: Manila Consulting Group; 2011. Obstructive sleep apnea and commercial motor vehicle driver safety: updated review[Internet] [cited 2015 Feb 11]. Available from: http://ntl.bts.gov/lib/44000/44600/44638/OSA_Update_11302011-p.pdf. [Google Scholar]
- 21.Ancoli-Israel S, Czeisler CA, George CFP, Guilleminault C, Pack AI. Washington DC: 2008. Obstructive sleep apnea and commercial driver safety[Internet] [cited 2015 Feb 11]. Available from: http://www.fmcsa.dot.gov/sites/fmcsa.dot.gov/files/docs/Sleep-MEP-Panel-Recommendations-508.pdf. [Google Scholar]
- 22.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 23.Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the berlin questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;5:485–91. doi: 10.7326/0003-4819-131-7-199910050-00002. [DOI] [PubMed] [Google Scholar]
- 24.Burns N. An integrative review of screening for obstructive sleep apnea in commercial vehicle drivers. Workplace Health Saf. 2014;62:114–20. doi: 10.1177/216507991406200305. [DOI] [PubMed] [Google Scholar]
- 25.Talmage JB, Hudson TB, Hegmann KT, Thiese MS. Consensus criteria for screening commercial drivers for obstructive sleep apnea: evidence of efficacy. J Occup Environ Med. 2008;50:324–29. doi: 10.1097/JOM.0b013e3181617ab8. [DOI] [PubMed] [Google Scholar]
- 26.Parks PD, Durand G, Tsismenakis AJ, Vela-Bueno A, Kales S. Screening for obstructive sleep apnea during commercial driver medical examinations. J Occup Environ Med. 2009;51:275–82. doi: 10.1097/jom.0b013e31819eaaa4. [DOI] [PubMed] [Google Scholar]
- 27.Silva GE, Vana KD, Goodwin JL, Sherrill DL, Quan SF. Identification of patients with sleep disordered breathing: comparing the four-variable screening tool, STOP, STOP-Bang, and Epworth Sleepiness Scales. J Clin Sleep Med. 2011;7:467–72. doi: 10.5664/JCSM.1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dabrh AMA, Firwana B, Cowl CT, Steinkraus LW, Prokop LJ, Murad MH. Health assessment of commercial drivers: a meta-narrative systematic review. BMJ Open. 2014;4:1–12. doi: 10.1136/bmjopen-2013-003434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Netzer NC, Hoegel JJ, Loube D, et al. Prevalence of symptoms and risk of sleep apnea in primary care. Chest. 2003;124:1406–14. doi: 10.1378/chest.124.4.1406. [DOI] [PubMed] [Google Scholar]
- 30.Chung F, Yegneswaran B, Liao P, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108:812–21. doi: 10.1097/ALN.0b013e31816d83e4. [DOI] [PubMed] [Google Scholar]
- 31.Chung F, Subramanyam R, Liao P, Sasaki E, Shapiro C, Sun Y. High STOP-Bang score indicates a high probability of obstructive sleep apnoea. Br J Anaesth. 2012;108:768–75. doi: 10.1093/bja/aes022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chung F, Yang Y, Brown R, Liao P. Alternative scoring models of STOP-Bang questionnaire improve specificity to detect undiagnosed obstructive sleep apnea. J Clin Sleep Med. 2014;10:951–58. doi: 10.5664/jcsm.4022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Parker DR, Hoffman BH. Washington DC: Federal Motor Carrier Safety Administration; 2012. Motor carrier safety advisory committee and medical review board task 11-05 report[Internet] [cited 2015 Feb 11]. Available from: http://mcsac.fmcsa.dot.gov/Reports.htm. [Google Scholar]
- 34.Pataka A, Daskalopoulou E, Kalamaras G, Fekete Passa K, Argyropoulou P. Evaluation of five different questionnaires for assessing sleep apnea syndrome in the sleep clinic. Sleep Med. 2014;15:776–81. doi: 10.1016/j.sleep.2014.03.012. [DOI] [PubMed] [Google Scholar]
- 35.U.S. Federal Motor Carrier Safety Administration. Washington DC: U.S. Department of Transportation; Medical examination report for commercial driver fitness determination [Internet] [updated 2014, Mar 19; cited 2015 Feb 11]. Available from: http://www.fmcsa.dot.gov/sites/fmcsa.dot.gov/files/docs/Medical_Examination_Report_for_Commercial_Driver_Fitness_Determination_649-F%286045%29.pdf. [Google Scholar]
- 36.Hukins C. Mallampati class is not useful in clinical assessment of sleep clinic patients. J Clin Sleep Med. 2010;6:545–49. [PMC free article] [PubMed] [Google Scholar]
- 37.Friedman M, Hamilton C, Samuelson CG, Lundgren ME, Pott T. Diagnostic value of the Friedman tongue position and Mallampati classification for obstructive sleep apnea: a meta-analysis. Otolaryngol Head Neck Surg. 2013;148:540–7. doi: 10.1177/0194599812473413. [DOI] [PubMed] [Google Scholar]
- 38.Berry RB, Brooks R, Gamaldo CE, et al. Darien IL: American Academy of Sleep Medicine; 2014. AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications, version 2.1. www.aasmnet.org. [Google Scholar]
- 39.Collop NA, Anderson AM, Boehlecke B, et al. Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. J Clin Sleep Med. 2007;3:737–47. [PMC free article] [PubMed] [Google Scholar]
- 40.Collop NA, Tracy SL, Kapur V, et al. Obstructive sleep apnea devices for out-of-center (OOC) testing: technology evaluation. J Clin Sleep Med. 2011;7:531–48. doi: 10.5664/JCSM.1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang C, Berger M, Malhotra A, Kales SN. Portable diagnostic devices for identifying obstructive sleep apnea among commercial motor vehicle drivers: considerations and unanswered questions. Sleep. 2012;35:1481–9. doi: 10.5665/sleep.2194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Centers for Medicare and Medicaid Services. Washington DC: Centers for Medicare and Medicaid Services; National coverage determination (NCD) for continuous positive airway pressure (CPAP) therapy for obstructive sleep apnea (OSA) (240.4) [Internet] [effective 2008 March 13; cited 2015 Feb 11]. Available from: http://www.cms.gov/medicare-coverage-database/details/ncd-details.aspx?NCDId=226&ncdver=3&NCAId=204&NcaName=Continuous+Positive+Airway+Pressure+%28CPAP%29+Therapy+for+Obstructive+Sleep+Apnea+%28OSA%29&IsPopup=y&bc=AAAAAAAAIAAA&. [Google Scholar]
- 43.Cigna. Cigna medical coverage policy (policy number 0158) [Internet] Cigna [updated 2013 Oct 15; cited 2015 Feb 11]. Available from: http://www.carecentrix.com/ProviderResources/Cigna Medical Coverage Policy.pdf.
- 44.Epstein LJ, Kristo D, Strollo PJ, et al. Clinical guide for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5:263–76. [PMC free article] [PubMed] [Google Scholar]
- 45.Weaver TD, Maislin G, Dinges DF, et al. Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning. Sleep. 2007;30:711–9. doi: 10.1093/sleep/30.6.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Antic NA, Catcheside P, Buchan C, et al. The effect of CPAP in normalizing daytime sleepiness, quality of life, and neurocognitive function in patients with moderate to severe OSA. Sleep. 2011;34:111–9. doi: 10.1093/sleep/34.1.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Berry RB, Sriram P. Auto-adjusting positive airway pressure treatment for sleep apnea diagnosed by home sleep testing. J Clin Sleep Med. 2014;10:1269–75. doi: 10.5664/jcsm.4272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rosen CL, Auckley D, Benca R, et al. A multisite randomized trial of portable sleep studies and positive airway pressure autotitration versus laboratory-based polysomnography for the diagnosis and treatment of obstructive sleep apnea: the HomePAP study. Sleep. 2012;35:757–67. doi: 10.5665/sleep.1870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kribbs NB, Pack AI, Kline LR, et al. Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep apnea. Am Rev Respir Dis. 1993;147:887–95. doi: 10.1164/ajrccm/147.4.887. [DOI] [PubMed] [Google Scholar]
- 50.Centers for Medicare and Medicaid Services. Washington DC: Centers for Medicare and Medicaid Services [cited 2015 Feb 11]; Local coverage determination (LCD): positive airway pressure (PAP) devices for the treatment of obstructive sleep apnea (L171) [Internet] Available from: http://www.cms.gov/medicare-coverage-database/indexes/national-and-local-indexes.aspx (individual state policies listed by state or local contractor) [Google Scholar]
- 51.Vanderveken OM, Dieltjens M, Wouters K, De Backer WA, Van de Heyning PH, Braem MJ. Objective measurement of compliance during oral appliance therapy for sleep-disordered breathing. Thorax. 2013;68:91–6. doi: 10.1136/thoraxjnl-2012-201900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Guimarães M, Hermont AP. Sleep apnea and occupational accidents: are oral appliances the solution? J Occup Environ Med. 2014;18:39–47. doi: 10.4103/0019-5278.146887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.U.S. Federal Motor Carrier Safety Administration [Internet] Washington DC: U.S. Department of Transportation; About us – history. [updated 2014 Mar 31; cited 2015 Feb 11]. Available from: http://www.fmcsa.dot.gov/mission/about-us. [Google Scholar]
- 54.U.S. Federal Motor Carrier Safety Administration [Internet] Washington DC: U.S. Department of Transportation; Our mission. [updated 2014 Jan 14; cited 2015 Feb 11]. Available from: http://www.fmcsa.dot.gov/mission. [Google Scholar]
- 55.U.S. Federal Motor Carrier Safety Administration [Internet] Washington DC: U.S. Department of Transportation; DOT medical exam and commercial motor vehicle certification. [updated 2015 Jan 28; cited 2015 Feb 11]. Available from: http://www.fmcsa.dot.gov/medical/driver-medical-requirements/dot-medical-exam-and-commercial-motor-vehicle-certification. [Google Scholar]
- 56.Washington DC: U.S. Department of Transportation; Federal Motor Carrier Safety Administration, Department of Transportation, 49 C.F.R., Sect. 390.5, Definitions [Internet] [n.d.; cited 2015 Feb 11]. Available from: http://www.fmcsa.dot.gov/regulations/title49/section/390.5. [Google Scholar]
- 57.Washington DC: U.S. Department of Transportation; U.S. Federal Motor Carrier Safety Administration, Department of Transportation, 49 C.F.R., Sect. 391.41 Physical qualifications and examinations [Internet] [n.d. cited 2015 Feb 11]. Available from: http://www.fmcsa.dot.gov/regulations/title49/section/391.41. [Google Scholar]
- 58.U.S. Federal Register. Washington DC: U.S: Department of Transportation, Federal Motor Carrier Safety Administration; Docket 98-3542, Physical qualification of drivers; medical examination; certificate [Internet] [published 2000 Oct 5; cited 2015 Feb 11]. Available at: http://www.gpo.gov/fdsys/pkg/FR-2000-10-05/html/00-25337.htm. [PubMed] [Google Scholar]
- 59.Hegmann KT, Anderson GBJ, Greenberg MI, Phillips B, Rizzo M. FMCSA's medical review board, five years of progress in commercial driver medical examinations. J Occup Environ Med. 2012;54:424–30. doi: 10.1097/JOM.0b013e3182480535. [DOI] [PubMed] [Google Scholar]
- 60.U.S. Federal Motor Carrier Safety Administration. Washington DC: U.S. Department of Transportation, Federal Motor Carrier Safety Administration; Medical Expert Panels [Internet] [updated 2014 Jul 8; cited 2015 Feb 11]. Available at: http://www.fmcsa.dot.gov/regulations/medical/medical-expert-panels. [Google Scholar]
- 61.U.S. Federal Motor Carrier Safety Administration. Washington DC: U.S. Department of Transportation, Federal Motor Carrier Safety Administration; Medical review board (home) [Internet] [n.d.; cited 2015 Feb 11]. Available at: http://www.mrb.fmcsa.dot.gov. [Google Scholar]
- 62.U.S. Federal Motor Carrier Safety Administration. Washington DC: U.S. Department of Transportation, Federal Motor Carrier Safety Administration; Welcome to the FMCSA MCSAC [Internet] [n.d.; cited 2015 Feb 11]. Available at: http://mcsac.fmcsa.dot.gov. [Google Scholar]
- 63.Washington DC; U.S: Department of Transportation, Office of Motor Carriers; Conference on Neurologic Disorders and Commercial Drivers [Internet] [published 1988 Jul; cited 2015 Feb 11]. Available at: http://www.fmcsa.dot.gov/sites/fmcsa.dot.gov/files/docs/neuro.pdf. [Google Scholar]
- 64.Washington DC: U.S. Department of Transportation, Office of Motor Carriers; Conference on Pulmonary/Respiratory Disorders and Commercial Drivers [Internet] [published 1991 Mar; cited 2015 Feb 11]. Available at: http://www.fmcsa.dot.gov/sites/fmcsa.dot.gov/files/docs/pulmonary1.pdf. [Google Scholar]
- 65.U.S. Federal Register 77 FR 23794. Proposed recommendations on obstructive sleep apnea [Internet]. U.S. Department of Transportation, Federal Motor Carriers Safety Administration [released 2012 Apr 20; cited 2015 Feb 11] Available from: https://www.federalregister.gov/articles/2012/04/20/2012-9555/proposed-recommendations-on-obstructive-sleep-apnea.
- 66.U.S. Federal Register 77 FR 25227. Washington DC: U.S. Department of Transportation, Federal Motor Carrier Safety Administration; Withdrawal of notice: proposed recommendations on obstructive sleep apnea [Internet] [released 2012 Apr 27; cited 2015 Feb 11]. Available at: https://www.federalregister.gov/articles/2012/04/27/2012-10176/proposed-recommendations-on-obstructive-sleep-apnea. [Google Scholar]
- 67. H.R. 3095 (2013), Pub. L. No 113-45. U.S. [Internet became law 2013 Oct 15; cited 2015 Feb 11]. Available at: https://www.congress.gov/bill/113th-congress/house-bill/3095l.
- 68.Eisner N. Washington DC: U.S. Department of Transportation [Internet]; 2012. Rulemaking requirements. [cited 2015 Apr 27]. Available from: http://www.dot.gov/regulations/rulemaking-requirements. [Google Scholar]
- 69.U.S. National Transportation Safety Board. Washington DC: U.S. National Transportation Safety Board; NTSB 2015 most wanted transportation safety improvements: require medical fitness for duty factsheet [Internet] [released 2015 Jan 13; cited 2015 Feb 11]. Available at: http://www.ntsb.gov/safety/mwl/Documents/MWL_2015_Factsheet_08.pdf. [Google Scholar]
- 70.Xie W, Chakrabarty S, Levine R, Johnson R, Talmage JB. Factors associated with obstructive sleep apnea among commercial motor vehicle drivers. J Occup Environ Med. 2011;53:169–73. doi: 10.1097/JOM.0b013e3182068ceb. [DOI] [PubMed] [Google Scholar]
- 71.Colvin LJ, Dace GA, Colvin RM, Ojile J, Collop NA. Commercial motor vehicle driver positive airway pressure therapy adherence in a sleep center. J Clin Sleep Med. doi: 10.5664/jcsm.5670. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lin CY, Shih TS, Liou SH, Lin MH, Chang CP, Chou TC. Predictors for progression of sleep disordered breathing among public transport drivers: a 3-year follow-up study. J Clin Sleep Med. 2015;11:419–25. doi: 10.5664/jcsm.4596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Platt AB, Wick LC, Hurley S, et al. Screening commercial drivers for obstructive sleep apnea using guidelines recommended by a joint task force. J Occup Environ Med. 2013;55:1035–40. doi: 10.1097/JOM.0b013e318298fb0e. [DOI] [PubMed] [Google Scholar]


