Abstract
Many patients with obstructive sleep apnea (OSA) exhibit worsening event indices while supine. Positional therapy is an option if indices normalize in non-supine sleep. Although several methods are available for patients choosing positional therapy, monitoring adherence remains challenging in part because the reliability of self-reported sleep position is uncertain. We analyzed self-reported sleep position in a sample of 300 patients who underwent clinical polysomnography (PSG) in our center. We found a broad range of discrepancy with objective body position, which was not correlated with demographics, PSG metrics, or confidence in the self-report. The results suggest that objective position monitoring can be an important complement to self-report in the management of patients opting for positional therapy.
Citation:
Russo K, Bianchi MT. How reliable is self-reported body position during sleep? J Clin Sleep Med 2016;12(1):127–128.
Keywords: body position, supine, sleep apnea, self-report
The severity of obstructive sleep apnea (OSA) depends on several factors, including sleep stage and body position. Approximately 50% of patients will show greater severity while supine, and a subset of those will be so positional that breathing indices are mild or normal while in the lateral position.1–3 In cases of supine dominant or supine isolated OSA, position therapy may be a viable treatment alternative to positive airway pressure (PAP).4 Several consumer devices are available to help avoid supine sleep (shirts/vests with bumpers such as Rematee, Zzoma, SlumberBump). In addition, the prescription NightShift device actively prevents supine position and also tracks objective sleep patterns.5
When considering treatment options, OSA patients may report body position preference or the capability to control their body position during sleep. However, self-reported sleep position is by nature uncertain, as it refers to time when one is not conscious. Position-enforcing devices are clinically useful in part because they circumvent this uncertainty. A small study previously suggested that healthy adults were able to accurately recall whether most of their sleep time was spent supine or non-supine6; however, this has not been well-studied in patient populations.
The institutional review board approved the retrospective analysis of our clinical sleep laboratory database without requiring consent. We compared self-reported body position with objective position in a convenience sample of 300 consecutive patients undergoing polysomnography (PSG) to quantify the potential for subjective-objective position mismatch. We imposed no minimal criterion for total sleep time (TST); only 8 subjects had TST < 3 hours. Discrepancies between the five self-reported category and objective supine sleep time were investigated by first assigning percentage values to each category in two ways: (a) the mid-point of equal size bins (10%, 30%, 50%, 70%, 90%), or (b) the midpoint of skewed bins with narrow ranges at the extremes (5%, 25%, 50%, 75%, 95%). Then we subtracted the objective percent of sleep that was spent supine from this value. We also measured “error” through binary assignment (correct or not) if the objective value fell within the equal sized bins.
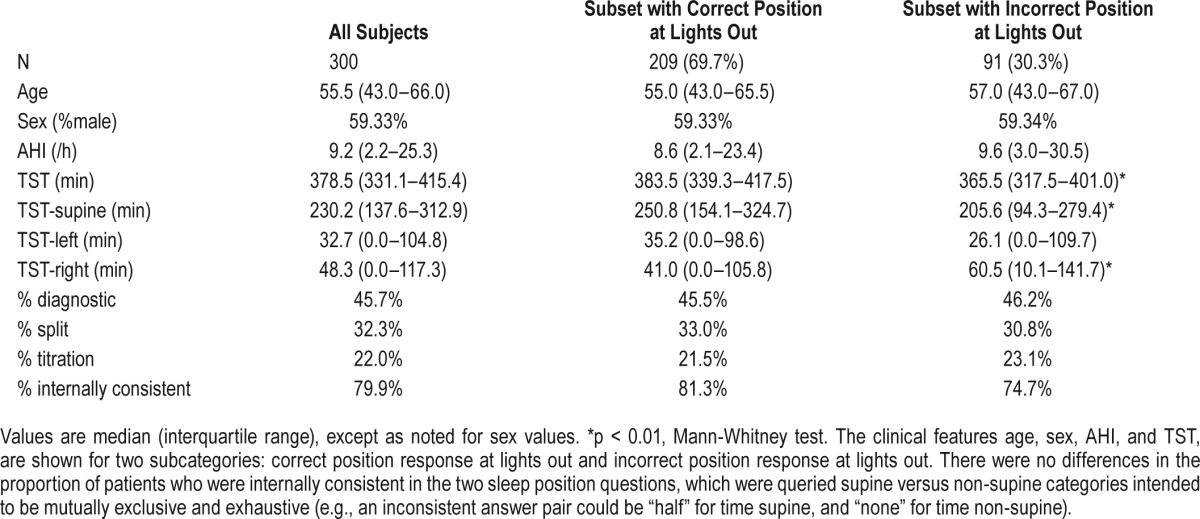
For each self-reported category of TST spent supine, the distribution of objective supine proportion of TST was broad (Figure 1). The discrepancy between self-reported and objective time in supine sleep, calculated in the previously described three ways, was not correlated with clinical features such as age, sex, apnea hypopnea index (AHI), TST, or type of PSG (Spearman correlation). The error was not correlated with the confidence of reporting their body position (7-point Likert-like scale from “complete guess” to “certain”). Interestingly, 30% of the cohort incorrectly reported their body position at the time of lights-out, suggesting that uncertainty exists even when recollecting position while awake. This waking recall discrepancy was not related to age, sex, or AHI (although patients with incorrect waking recall had slightly lower TST values than those with correct recall; Table 1).
Figure 1. Objective supine sleep duration for each self-report category.
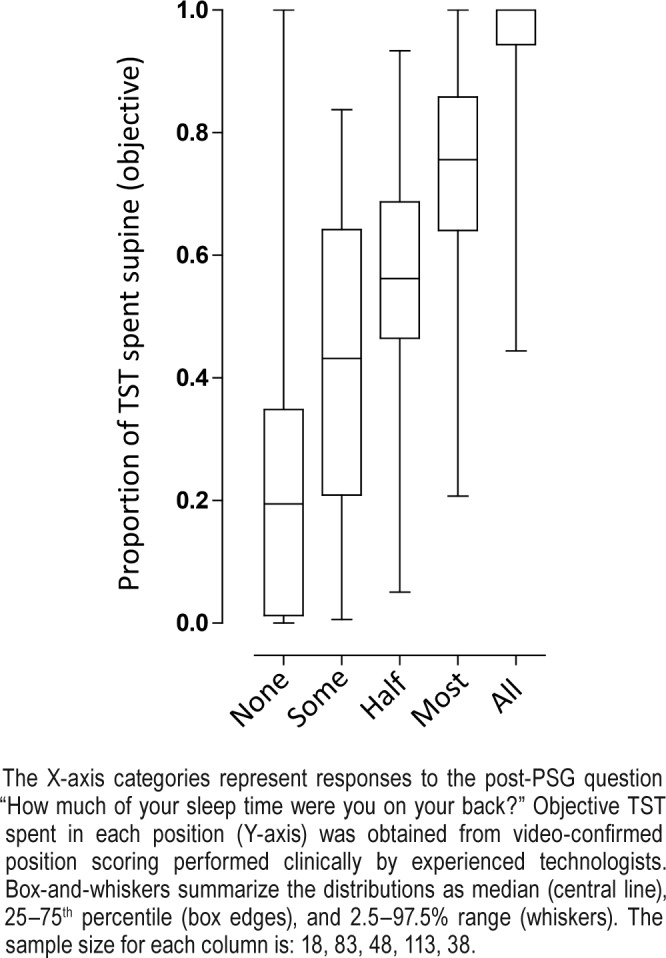
The X-axis categories represent responses to the post-PSG question “How much of your sleep time were you on your back?” Objective TST spent in each position (Y-axis) was obtained from video-confirmed position scoring performed clinically by experienced technologists. Box-and-whiskers summarize the distributions as median (central line), 25–75th percentile (box edges), and 2.5–97.5% range (whiskers). The sample size for each column is: 18, 83, 48, 113, 38.
Table 1.
Clinical features of entire cohort and subdivided by correct versus incorrect position responses at lights out.
Our results suggest that self-reported body position may not reliably match objective position during sleep, and thus should not be the sole assessment of compliance with position therapy. Lack of reliability may be multifactorial, and further research could elucidate pertinent factors that were not assessed in our sample, such as attention, memory, or understanding instructions. Objective position monitoring holds promise for optimizing position therapy in the subset of OSA patients with supine dominant disease.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. Bianchi receives funding from the Department of Neurology, Massachusetts General Hospital, the Center for Integration of Medicine and Innovative Technology, the Milton Family Foundation, and the MGH-MIT Grand Challenge. Dr Bianchi has a patent pending on a home sleep monitoring device. Dr. Bianchi received travel funding from Servier, has consulting agreements with Foramis, MC10, and GrandRounds, and has provided expert testimony in sleep medicine.
ABBREVIATIONS
- AHI
apnea-hypopnea index
- OSA
obstructive sleep apnea
- PAP
positive airway pressure
- PSG
polysomnography
- TST
total sleep time
REFERENCES
- 1.Eiseman NA, Westover MB, Ellenbogen JM, Bianchi MT. The impact of body posture and sleep stages on sleep apnea severity in adults. J Clin Sleep Med. 2012;8:655–66. doi: 10.5664/jcsm.2258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oksenberg A, Silverberg DS. The effect of body posture on sleep-related breathing disorders: facts and therapeutic implications. Sleep Med Rev. 1998;2:139–62. doi: 10.1016/s1087-0792(98)90018-1. [DOI] [PubMed] [Google Scholar]
- 3.Mador MJ, Choi Y, Bhat A, et al. Are the adverse effects of body position in patients with obstructive sleep apnea dependent on sleep stage? Sleep Breath. 2010;14:13–7. doi: 10.1007/s11325-009-0269-z. [DOI] [PubMed] [Google Scholar]
- 4.Ravesloot MJ, van Maanen JP, Dun L, de Vries N. The undervalued potential of positional therapy in position-dependent snoring and obstructive sleep apnea-a review of the literature. Sleep Breath. 2013;17:39–49. doi: 10.1007/s11325-012-0683-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Levendowski DJ, Seagraves S, Popovic D, Westbrook PR. Assessment of a neck-based treatment and monitoring device for positional obstructive sleep apnea. J Clin Sleep Med. 2014;10:863–71. doi: 10.5664/jcsm.3956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gordon SJ, Grimmer KA, Trott P. Self-reported versus recorded sleep position: an observational study. Internet J Allied Health Sci Pract. 2004;2:1–10. [Google Scholar]


