Abstract
Study Objectives:
This is the first study to compare reflux events during wake and sleep in obese and non-obese individuals with obstructive sleep apnea (OSA) and obese individuals without OSA. The primary aim of the study was to investigate any additive effect of OSA on gastroesophageal reflux (GER) above that of obesity.
Methods:
Twenty obese individuals (body mass index, BMI > 30 kg/m2), 9 non-obese individuals (BMI < 30 kg/m2) with moderate-to-severe OSA, and 17 obese control subjects (BMI > 30 kg/m2) underwent high-resolution esophageal manometry, 24-h esophageal pH-impedance monitoring, and in-laboratory polysomnography.
Results:
Mean body mass index was 40 ± 6 and 27 ± 4 kg/m2 for the obese and non-obese OSA groups, respectively, and 34 ± 5 kg/m2 for the obese control group. Apnea-hypopnea index (AHI) was 50 ± 30 and 30 ± 25 per hour for the obese and non-obese OSA groups (p > 0.05), significantly higher than that of the obese control group (3 ± 3 per hour, p < 0.05). The two obese groups did not show any significant differences in the total number of acidic reflux events (41 ± 20 vs 28 ± 16); however, the obese OSA group had a greater number of acidic reflux events compared to the non-obese OSA group (22 ± 12 events, p < 0.05). In multivariate analysis, BMI significantly predicted number of acidic reflux events (r2 = 0.16, p = 0.01) during the 24-h period; however, AHI showed no significant association with any measure of GER severity.
Conclusions:
This study confirms an important role for obesity, rather than OSA per se in the relationship between OSA and GER.
Citation:
Shepherd K, Orr W. Mechanism of gastroesophageal reflux in obstructive sleep apnea: airway obstruction or obesity? J Clin Sleep Med 2016;12(1):87–94.
Keywords: esophageal pH monitoring, gastroesophageal reflux, obesity, obstructive sleep apnea, sleep
INTRODUCTION
Obstructive sleep apnea (OSA) is characterized by repetitive narrowing or collapse of the upper airway during sleep with the development of large negative intrathoracic pressures. Gastroesophageal reflux (GER) is a common condition where there is retrograde flow of stomach contents into the esophagus, characterized by symptoms such as heartburn and acid regurgitation.1 Gastroesophageal reflux appears to be a particular problem for patients with OSA, as they exhibit an increase in GER symptoms and events during waking and sleep compared to individuals without OSA.2–8
The precise mechanism underlying the increase in nocturnal GER in OSA patients remains unclear. Previous hypotheses, including the specific development of negative intrathoracic pressures generated during obstructive events, have not been substantiated by recent studies. Kuribayashi et al.9,10 and Shepherd et al.11 have shown that the barrier provided by the lower esophageal sphincter (LES) is actually stronger during obstructed breathing events, particularly during inspiratory efforts against an obstructed airway. Additionally, it is unlikely that individual obstructed breathing events or the associated arousals are precipitating individual reflux events as the number of breathing events and arousals overnight in an individual with OSA far outweighs the number of sleep-related reflux events. Furthermore, while several studies have found reflux events in temporal association with an obstructed airway, this relationship is weak at best.4,7,12
BRIEF SUMMARY
Current Knowledge/Study Rationale: This study compares reflux events during wake and sleep in obese patients with and without OSA and lean individuals with OSA.
Study Impact: This study confirms an important role for obesity, rather than OSA per se in the relationship between OSA and GER.
The role of obesity in the link between OSA and GER remains unclear. Obesity is a risk factor common to both OSA and GER and therefore represents a potential mechanism for the link between the two conditions. Ing et al.,7 however, showed that in a group of 41 control subjects and 63 OSA subjects (matched for age, BMI, FEV1, and alcohol consumption) that individuals with OSA had a great number of acidic reflux events and spent more time at a pH below 4, suggesting a role for OSA independent of obesity. Further supporting this finding, are several studies,8,13,14 which also show an effect of OSA on GER independent of BMI. Shepherd et al.8 in a population based study showed that independent of BMI, OSA increases the risk of nighttime GER symptoms by 3 times (in the case of severe OSA). In contrast, there are several studies which suggest that OSA had no effect on GER symptoms and that the relationship is a result of the obesity shared by both conditions.4,15–17
This is the first study to compare frequency of reflux events during wake and sleep, as well as lower esophageal sphincter motility and esophageal function in obese patients with and without OSA and non-obese individuals with OSA. The primary aim of the study was to investigate any additive effect of OSA on GER above that of obesity.
METHODS
Subjects
Three groups of subjects were studied: a group of non-obese individuals with moderate-to-severe OSA; a group of obese individuals with moderate-to-severe OSA; and a group of obese individuals without OSA (obese controls). These patients had been identified from our sleep clinic population or had responded to advertisements in local media. Participants were 18 to 70 years of age and were excluded if they were currently taking over-the-counter or prescription medications for GER that they were not willing to stop during the study; if they had any chronic medical condition, gastrointestinal conditions which might affect esophageal function or acid secretion, or previous surgery to the stomach and/or esophagus.
Protocol
The study was approved by Schulman Institutional Review Board and written informed consent was obtained from each patient prior to participation.
All patients attended our gastroesophageal testing laboratory for esophageal motility testing as well as 24-h pH/impedance monitoring and in-laboratory polysomnography (PSG). Initially, all subjects underwent PSG for screening purposes to rule out sleep disorders other than OSA and to confirm the presence and severity of OSA. The apnea-hypopnea index (AHI, number of apneas and hypopneas per hour of sleep) was used to stratify participants into two groups: those without OSA (AHI < 5 events/h) and those with moderate-to-severe OSA (AHI > 15 events/h).
Patients attended the gastroesophageal motility laboratory at Lynn Health Science Institute in the early morning and underwent esophageal motility testing and insertion of the 24-h pH/impedance catheter. They returned that evening where they were fed a standardized meal consisting of soup, a sandwich, chips, and a cookie. They then underwent PSG with simultaneous pH/impedance monitoring.
Subjects were required to cease any proton-pump inhibitors (PPIs) 5 days prior to the study, H2-receptor antagonists for 48 h prior to the study, and antacids or caffeinated, acidic, and high-fat foods and drinks for 24 h prior to the study. Each subject was required to fast for a minimum of 6 h prior to the study.
Polysomnography
Overnight PSG was conducted according to the American Academy of Sleep Medicine recommendations. These data were collected on a computerized data acquisition system (Grass Aurora polysomnography systems; Grass Telefactor, West Warwick, RI).
Categorization of sleep stage and respiratory events were performed according to standard criteria. Severity of sleep disordered breathing was defined by the AHI.19 Additional detail regarding sleep parameters is provided in the supplemental material.
The PSG was used to divide the study time into the sleep period and the wake period. Sleep period was defined as the time between sleep onset and waking in the morning. The wake period incorporates the remainder of the 24-h period.
Subjects were required to cease using any existing therapies for OSA for 48 hours prior to the study.
24-Hour pH/Impedance Testing
pH/impedance monitoring was performed using a pH/impedance catheter (O.D. 2.3 mm, Comfortec Z/pH catheters, Sandhill Scientific, Highlands Ranch, CO). Recordings were analyzed using the Bioview Analysis Software (Sandhill Scientific, Highlands Ranch, CO, USA), and automatic analyses were adjusted manually where required.
The pH sensor was used to determine percent acid clearance time (percentage of recording time with pH < 4). The impedance sensors were used in combination with the pH sensor to determine longest reflux event, acid time, non-acid time, and number of distal and proximal reflux events (acid, non-acid). These parameters were determined for the 24-h recording period as well as the wake and sleep periods. Additional detail regarding pH/impedance testing is available in the supplemental material.
Esophageal Motility Testing
Motility studies were conducted using a solid state high resolution manometry impedance catheter (O.D. 4.0 mm) (Sandhill Scientific InSIGHT, Highlands Ranch, CO, USA).
An electronic sleeve was applied on the LES, enabling accurate monitoring of the high pressure within the LES while accounting for sphincter movement during respiration and swallowing (details in supplemental material).18
Manometric recordings were analyzed using the Bioview Analysis Software (Sandhill Scientific, Highlands Ranch, CO, USA), and the automatic analyses were adjusted manually where necessary.
LES pressure, LES length (total and intra-abdominal), nadir LES pressure during LES relaxation and duration of LES relaxation, esophageal peristaltic amplitude and velocity, and percent complete bolus transit were assessed. Additional detail regarding esophageal motility testing is available in the supplemental material.
Questionnaires
The Gastroesophageal Reflux Questionnaire (GERQ) was used to define frequency of daytime and nighttime symptoms of GER.20,21 GER symptoms were classified as follows: heartburn or acid regurgitation experienced at least once in the last 12 months was defined as any GER and, if experienced at least once a week, was defined as frequent GER.20,22 The term GER symptoms refers to symptoms experienced at any time during the day or night, while nighttime GER (nGER) symptoms specifically refers to symptoms which woke the patient from sleep.
Participants also completed the Pittsburgh Sleep Quality Index (PSQI), the Carlsson Gastroesophageal Reflux Disease questionnaire, and the Epworth Sleepiness Scale (ESS) (details in the supplemental material).
Statistical Analyses
Results are presented as mean ± standard deviation. Statistical analyses were performed using SigmaStat (SysStat Software Inc., San Jose, USA). ANOVA was used to compare pH, sleep, and manometric variables between groups. When data were not normally distributed, ANOVA on ranks was performed. Proportions of each group reporting GER symptoms or medications were compared using χ2 tests or Fisher exact tests. Linear regression analyses were performed on the entire study population to determine the association between obesity and/or OSA severity and reflux severity. Reflux variables were examined for independent association with AHI or BMI only if they exhibited evidence of a univariate association (p < 0.1). Age and gender were also entered into any multivariate analyses because of reported associations with GER. Colinearity diagnostics were performed on all variables prior to entry in any multivariate model. A p value < 0.05 was considered significant for all tests.
RESULTS
Group Characteristics
Results are presented in Table 1. Nineteen obese individuals without OSA; 10 non-obese individuals with moderate-severe OSA; and 25 obese individuals with moderate-severe OSA and were entered into the study. Two of the obese control group; 5 of the obese OSA group and 1 of the non-obese OSA group withdrew during the motility visit; therefore data were available in: 17 obese individuals (BMI 34 ± 5 kg/m2) without OSA; 20 individuals who were obese (BMI 40 ± 6 kg/m2) with moderate to severe OSA; and 9 individuals who were not obese (BMI 27 ± 4 kg/m2) with moderate to severe OSA (Table 1). pH data were only available on 8 of 9 of the non-obese OSA group due to equipment failure in one individual.
Table 1.
Subject characteristics.
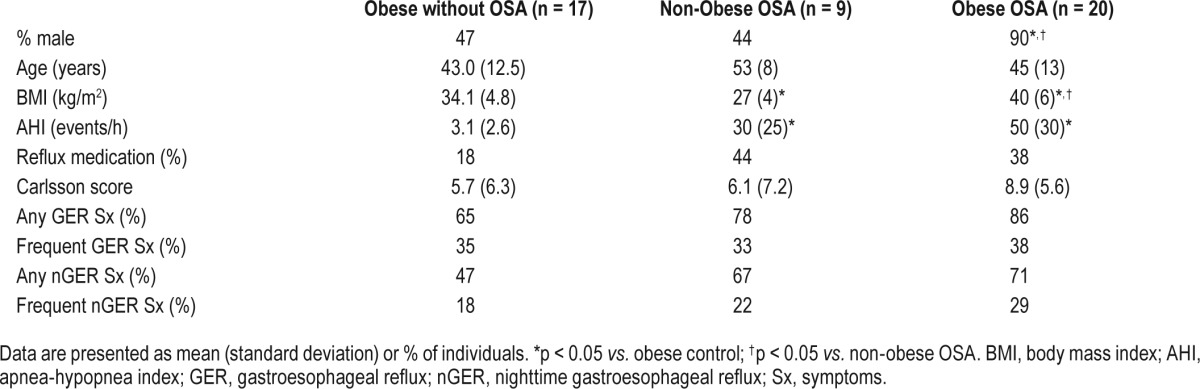
There were significantly more males in the obese OSA group than either the obese control or non-obese OSA groups. Mean age was not statistically different between groups. BMI was significantly greater in the obese OSA group compared to either the obese control or non-obese OSA groups, and the obese control group was significantly greater than the non-obese OSA group. AHI was not different between the non-obese and obese OSA groups. The AHI in the obese control group was well within normal limits (< 5 events/h) and significantly lower than either of the OSA groups. The proportion of each group who were taking prescription medication for GER symptoms (i.e. PPIs or H2 antagonists) was similar between groups. The proportion of each group reporting GER or nGER symptoms was also similar (Table 1).
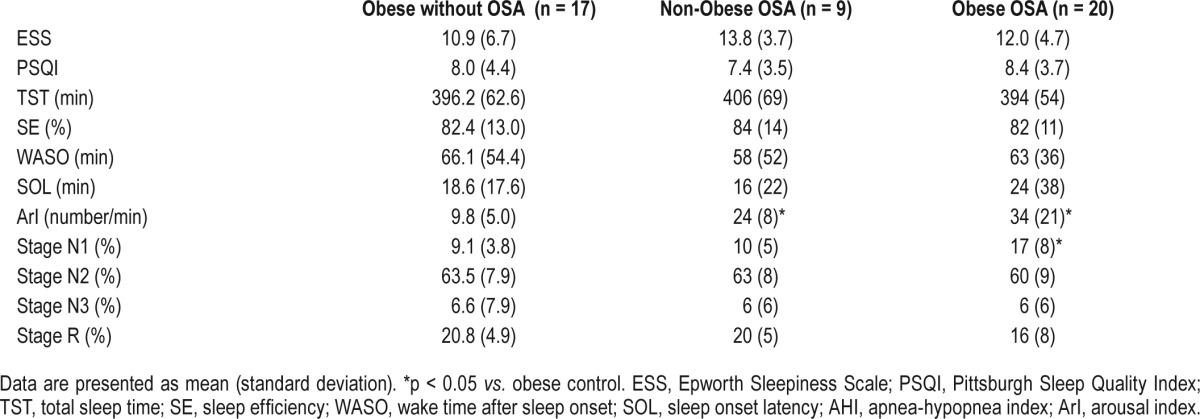
ESS and PSQI scores were similar between groups, as were total sleep time, sleep efficiency, wake time after sleep onset, and sleep onset latency (Table 2). Arousal index was significantly higher in both the obese and non-obese OSA groups than the obese control group. Stage N1 sleep was higher in the obese OSA group than the obese control groups.
Table 2.
Sleep data.
pH/Impedance Monitoring
24-H Recording Period
Number of acidic reflux events over the entire recording period was significantly greater in the obese OSA group than the non-obese OSA group (Table 3). However, there was no significant difference between the 2 obese groups. The acid exposure time was not significantly different among the groups.
Table 3.
pH/impedance data (24-h).
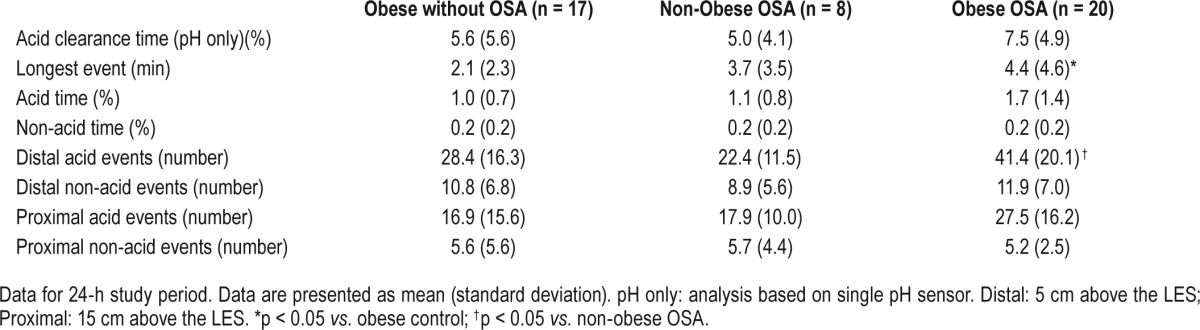
There was a significant main effect between groups for longest reflux event (p = 0.04), with the obese OSA group having a longer event than the obese control group. There were no differences between non-acid episodes between groups and no differences in number of proximal episodes between groups (Table 3).
Wake Period
During the wake period, the number of acidic reflux events was significantly different between groups (Table 4). The obese OSA group had significantly more events than both the non-obese OSA group and the obese control group. There was no significant difference between the non-obese OSA and the obese control group. The number of proximal acidic events was also different between groups, with the obese OSA group having significantly more events than the obese control group (Table 4).
Table 4.
pH/impedance data (wake period).
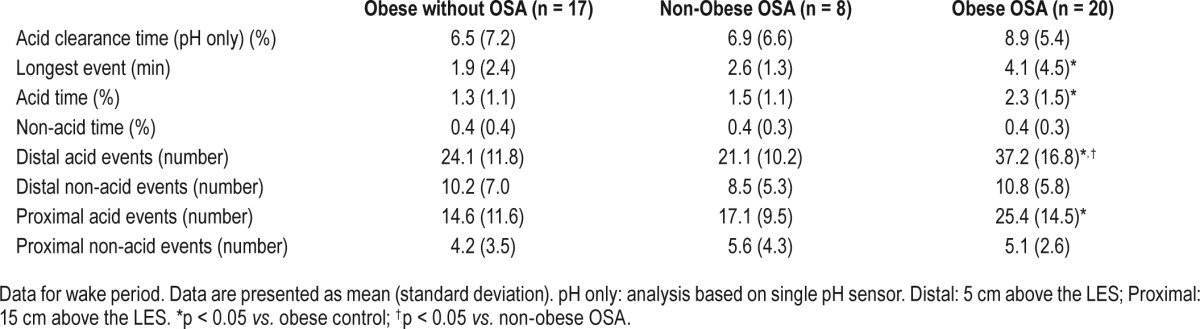
There was a significant difference between groups with regards to longest reflux event (p = 0.02). Post hoc testing showed that the obese OSA group had a significantly longer event than the obese control group. There was a trend for increasing length of longest event across the 3 groups with the obese control group having the shortest events and the obese OSA group having the longest. There was a significant main effect for acid exposure time, with the obese OSA group having significantly greater acid exposure than the obese control group.
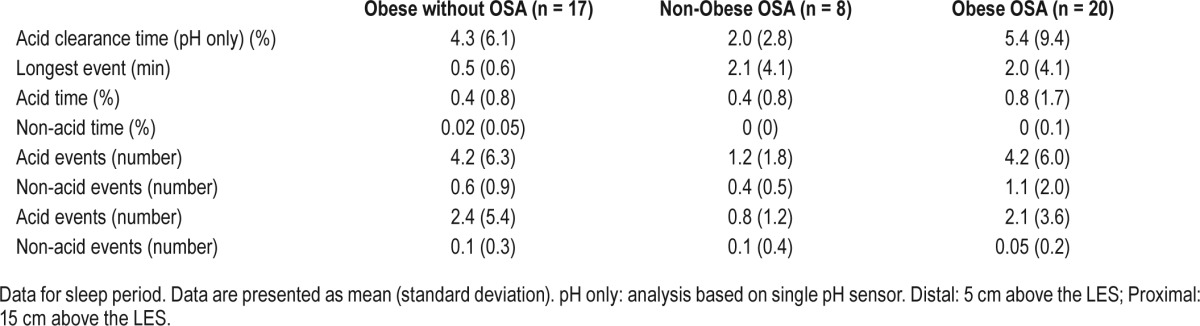
Sleep Period
Although there were no statistically significant differences between groups for the sleep period, some observations on the raw data are helpful (Table 5). First, the number of sleep related events is comparatively small with substantial variability especially in the 2 obese groups. However, it should be noted that the non-obese OSA group has only an average of slightly more than one episode noted during the sleeping interval. Both obese groups have approximately 4 times this number of events during the sleeping interval, albeit still relatively few in number. Thus, even though it is very difficult to obtain statistical significance under these circumstances, these observations are useful in the overall interpretation of these data. Furthermore, in all the data presented a similar pattern emerges which is that the non-obese OSA group has the fewest number of reflux events, and this is statistically significant in the overall and wake data when compared to the obese OSA group.
Table 5.
pH/impedance data (sleep period).
Esophageal/LES Motility
Lower Esophageal Sphincter
The mean LES pressure was not significantly different among the study groups (Table 6). However, 10 of the obese control group (59%), 4 of the obese OSA group (40%), and 2 of the non-obese OSA group (25%) had a resting LES pressure which would be classified as low (i.e., < 10 mm Hg). LES length and intra-abdominal LES length were significantly different (p = 0.02 and p = 0.04, respectively). Post hoc testing revealed that both LES length and intra-abdominal length were significantly greater in the obese OSA than the obese control group.
Table 6.
Manometry data.
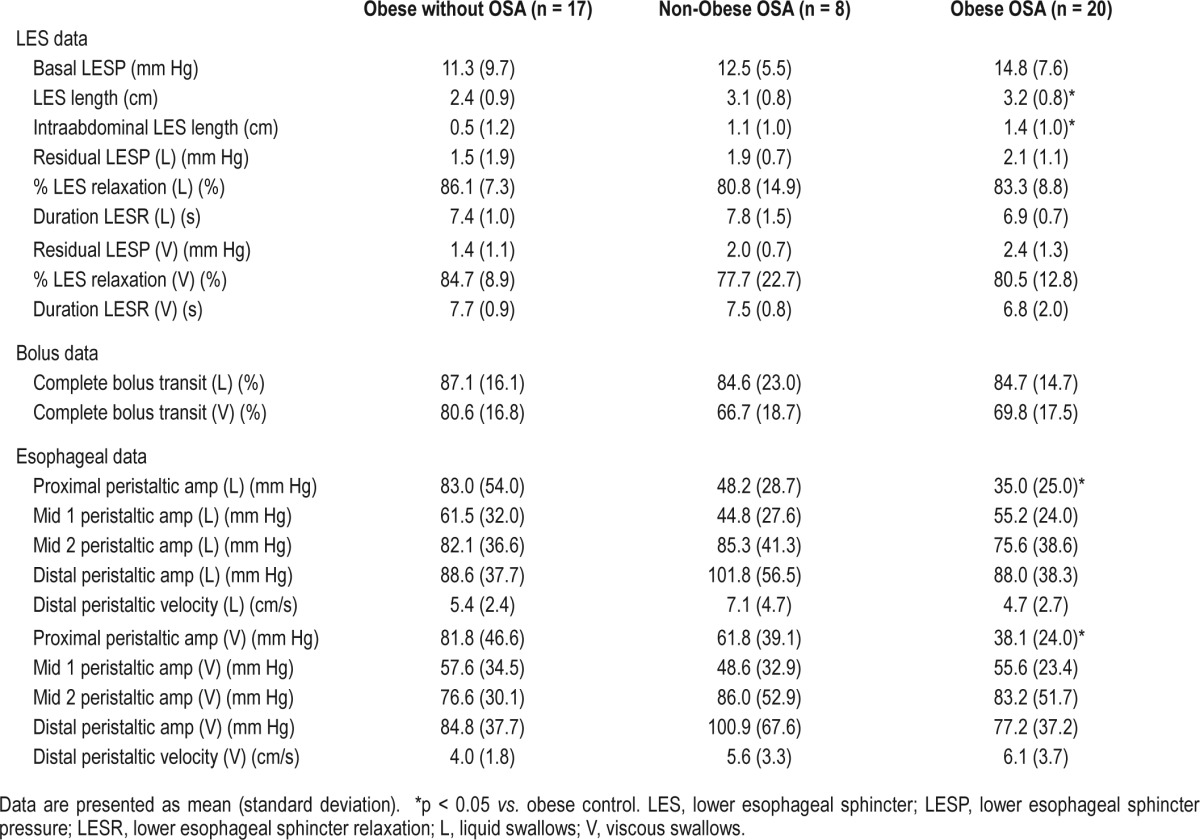
Esophageal Function
No individual in any group was classified as having ineffective esophageal motility. Proximal esophageal peristaltic amplitude with both liquid and viscous swallows was significantly different between groups, being lower in the obese OSA group than the obese control group.
There were no differences in the percentage of swallows associated with complete bolus transit for either liquid or viscous swallows between groups.
Univariate and Multivariate Associations between OSA, BMI, and GER
Individuals from all 3 groups were considered together for linear regression analyses (n = 45). Due to the relatively low proportion of non-acid events, acid and non-acid events were considered together. Results from univariate linear regression analysis are available in the supplemental material.
When gender, age, BMI, and AHI were entered into the multivariate model, BMI was significantly associated with number of distal events in the wake period and over the total recording period (r2 = 0.14, p = 0.01 and r2 = 0.16, p = 0.01, respectively). AHI was not significantly associated with any reflux variable.
DISCUSSION
This study investigated the roles of obesity and upper airway obstruction in the occurrence of GER in individuals with OSA. This was accomplished by objectively assessing GER and measures of esophageal function in obese controls without OSA and in order to assess the role of OSA per se we evaluated these measures in obese and non-obese individuals with moderate to severe OSA. The main findings of this study were: (1) the obese OSA group had more reflux episodes over the 24-h study period than the non-obese OSA group; (2) the two obese groups did not show any significant differences in the total number of reflux events; (3) the obese OSA group had significantly more reflux episodes throughout the day than either the obese control group or the non-obese OSA group; (4) during sleep, the number of reflux events in the obese control group and the obese OSA group was identical and both were numerically (although not statistically significant) almost four times greater than the non-obese controls; and (5) BMI was significantly associated with measures of GER severity. These data support to the notion that obesity, compared to upper airway obstruction alone, plays a more important role in the pathogenesis of GER in patients with OSA.
The present study demonstrated a greater number of acidic reflux events over the total recording time in the obese OSA group compared to the non-obese OSA group. The obese control group was not significantly different from the obese OSA group. During the wake period, the obese OSA group had significantly more acidic reflux events than either the obese control or non-obese OSA groups. Although this result does not support the obesity hypothesis, we feel this can be explained by the substantially greater BMI in the obese OSA and its likely greater effect on reflux events during the day. In spite of the lack of statistical significance of the sleep data, a more careful examination of the numerical data is instructive. It can be seen in Table 5 that the number of reflux events during the sleeping interval is virtually identical for both of the obese groups and nearly 4 times greater than the non-obese OSA control group. It is likely that this result weighed heavily in the multivariate result showing a significant relationship between BMI and GER severity. These argue in favor of obesity as opposed to airway obstruction per se, as the prevailing factor in the pathogenesis of GER in patients with OSA.
To our knowledge, this is the first study to compare obese individuals without OSA to obese and non-obese OSA patients with regard to the frequency of GER, which precludes a comparison to earlier work. However previous studies comparing GER in individuals with OSA to normal controls have suggested that individuals with OSA have more reflux symptoms as well as a greater number of reflux events than those without OSA.7,8,23–25 There have now been several investigations into the mechanism underlying this reported increase in GER in OSA patients; however, the factors which create risk for reflux remain unclear. Our data use critical control groups such as an obese group without OSA as well as a non-obese group with OSA to assess and compare to role of OSA and obesity in creating risk for GER.
Studies by Shepherd et al. and Kurybayashi et al. have negated the suggestion that negative intrathoracic pressure causes acid to move into the esophagus.10,11 While some studies suggest a temporal relationship between obstructed breathing events and sleep reflux events,4,12 previous studies have not demonstrated a consistent association. In addition, the number of obstructed breathing events far outweighs the number of sleep reflux events; therefore, there is a high likelihood that these two phenomena may occur by chance.
In an epidemiological study, Shepherd et al. showed that in the general population, individuals at high risk of OSA were twice as likely to suffer frequent GER symptoms during sleep than those at low risk; furthermore, individuals with polysomnographically defined severe OSA were more than three times as likely to experience frequent GER symptoms during sleep independent of BMI.8 In the only study to compare GER in OSA and non-OSA groups matched for age and BMI, Ing et al.7 found that the OSA group had significantly more reflux events and greater acid contact time overnight than the non-OSA group. They reported a staggering mean number of reflux events overnight of more than 100, compared to the upper limit of 5 events during sleep in the present study. The reason for the inflated number of reflux events in Ing's study is unclear; however, our findings are in line with several other studies investigating reflux during sleep in OSA which have reported a mean number of GER events of approximately 1–10 events.4,5,9,10 These previous studies suggest that OSA may play a role in the pathogenesis of GER. However, the findings of the present study do not support an independent role for AHI in the pathogenesis of GER since both the obese control and obese OSA groups had more reflux events than the non-obese OSA group for a given severity of OSA.
In an attempt to investigate potential mechanisms underlying any differences we observed in pH/impedance variables among the three groups, we conducted esophageal motility testing on all subjects. There was no difference in basal LES pressure between groups; however, LES length and intra-abdominal LES length were significantly greater in the obese OSA group than the obese control group. The difference between the obese OSA and non-obese OSA groups was not significant. The segment of the LES that is exposed to intra-abdominal pressure has been shown to be an important determinant of the competence of the LES in preventing GER.26,27 That the OSA groups had a greater intra-abdominal LES length suggests that OSA is associated with anatomical features which may be protective of GER. With regard to esophageal peristalsis, proximal peristaltic amplitude during liquid and viscous swallows was significantly higher in the obese OSA than the obese control group, however this was not significantly different from the non-obese OSA group. Given the lack of effect on esophageal function (bolus clearance) and given the absence of additional differences; the significance of this finding is not likely to be important. There were no differences in peristaltic amplitude or velocity between groups.
While esophageal motility has not been studied in OSA patients previously, several studies have compared esophageal and LES motility in obese vs. non-obese individuals. While one study reported that obese individuals have higher LES pressure,28 several other studies report a negative relationship between BMI and LES pressure.29,30 The effects of obesity on esophageal peristaltic amplitude vary from no effect29 to an increase in amplitude with increasing BMI.28 Pandolfino et al.31 demonstrated that the pressure morphology within and across the esophago-gastric junction is altered in obesity in a fashion that may augment flow of fluid into the esophagus. Additionally, they demonstrated that obesity was associated with increased axial separation between the crural diaphragm and the LES which may precipitate the development of hiatus hernia, a significant contributor to the occurrence of GER. These findings support our conclusion that obesity creates a greater risk for GER than OSA.
The present study suggests that the increase in the number of reflux events in the obese OSA group is not explained by differences in LES function or esophageal motility. We do not, however, have information regarding rate of transient LES relaxation (TLESR, the primary mechanism underlying GER events) in these individuals during the postprandial period. It is possible that the underlying mechanism for the increase in GER events in the obese group lies with TLESRs. A previous study by Che Yuen et al.32 investigated the rate of TLESR in normal, overweight, and obese individuals, and they reported a significant increase in postprandial TLESR in the overweight and obese groups compared to the normal group in a dose-dependent fashion. They suggested that this is due to an increase in intragastric pressure. They also reported no relationship between OSA and TLESRs and suggest that OSA may be an epiphenomenon in the relationship between obesity and GER disease. Although we do not have this comparison between groups, the lack of a difference in motility variables in our study and the increase in number of events in the obese OSA group and obese control group compared to non-obese OSA group supports this previous interpretation.
Limitations
We acknowledge there are several limitations to this study. First, while we endeavored to match the OSA groups according to AHI and while there was no significant difference between groups, the AHI was 20 events per hour greater in the obese OSA group. This is reflective of the strong relationship between BMI and the presence of OSA. Second, while we endeavored to match BMI between the obese groups, the OSA group had a significantly greater BMI than the obese control group, again reflective of the strong relationship between OSA and obesity. To address these limitations, all individuals were considered together and multivariate regression analysis was performed which supported BMI as the primary factor in predicting the occurrence of GER. Third, given the low numbers in the non-obese OSA group there is the possibility of a type II error; however, the majority of our statistical tests demonstrated adequate power. Finally, we do not have individuals with mild OSA, which may have been useful in determining additive effects of OSA and obesity on GER.
In conclusion, this study confirms an important role for obesity, rather than OSA per se in the relationship between OSA and GER. Furthermore, the increase in GER in individuals with OSA does not appear to be due to changes in esophageal or LES motility or function.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank the sleep technologists at the Lynn Health Science Institute for their assistance with patient set-up and monitoring; Dr. Suanne Goodrich for scoring the sleep studies and administrative and technical assistance and Stacy Wright and Stephanee Smith for technical assistance. We also thank Professor Peter Eastwood for his critical review of the manuscript.
ABBREVIATIONS
- AHI
apnea hypopnea index
- BMI
body mass index
- ESS
Epworth Sleepiness Scale
- GER
gastroesophageal reflux
- GERQ
Gastroesophageal reflux questionnaire
- LES
lower esophageal sphincter
- nGER
nighttime gastroesophageal reflux
- OSA
obstructive sleep apnea
- PPI
proton pump inhibitor
- PSG
polysomnography
- PSQI
Pittsburgh Sleep Quality Index
REFERENCES
- 1.Klauser AG, Schindlbeck NE, Muller-Lissner SA. Symptoms in gastrooesophageal reflux disease. Lancet. 1990;335:205–8. doi: 10.1016/0140-6736(90)90287-f. [DOI] [PubMed] [Google Scholar]
- 2.Friedman M, Gurpinar B, Lin H, Schalch P, Joseph N. Impact of treatment of gastroesophageal reflux on obstructive sleep apnea-hypopnea syndrome. Ann Otol Rhinol Laryngol. 2007;116:805–11. doi: 10.1177/000348940711601103. [DOI] [PubMed] [Google Scholar]
- 3.Graf KI, Karaus M, Heinemann S, Korber S, Dorow P, Hampel KE. Gastroesophageal reflux in patients with sleep apnea syndrome. Z Gastroenterol. 1995;33:689–93. [PubMed] [Google Scholar]
- 4.Penzel T, Becker HF, Brandenburg U, Labunski T, Pankow W, Peter JH. Arousal in patients with gastro-oesophageal reflux and sleep apnoea. Eur Respir J. 1999;14:1266–70. doi: 10.1183/09031936.99.14612669. [DOI] [PubMed] [Google Scholar]
- 5.Sabate JM, Jouet P, Merrouche M, et al. Gastroesophageal reflux in patients with morbid obesity: a role of obstructive sleep apnea syndrome? Obes Surg. 2008;18:1479–84. doi: 10.1007/s11695-008-9508-9. [DOI] [PubMed] [Google Scholar]
- 6.Green BT, Broughton WA, O'Connor B. Marked improvement in nocturnal gastroesophageal reflux in a large cohort of patients with obstructive sleep apnea treated with continuous positive airway pressure. Arch Intern Med. 2003;163:41–5. doi: 10.1001/archinte.163.1.41. [DOI] [PubMed] [Google Scholar]
- 7.Ing AJ, Ngu MC, Breslin AB. Obstructive sleep apnea and gastroesophageal reflux. Am J Med. 2000;108:120S–5S. doi: 10.1016/s0002-9343(99)00350-2. [DOI] [PubMed] [Google Scholar]
- 8.Shepherd K, James A, Musk A, Hunter M, Hillman D, Eastwood P. Gastroesophageal reflux symptoms are related to the presence and severity of obstructive sleep apnea. J Sleep Res. 2010;20:241–49. doi: 10.1111/j.1365-2869.2010.00843.x. [DOI] [PubMed] [Google Scholar]
- 9.Kuribayashi S, Kusano M, Kawamura O, et al. Mechanism of gastroesophageal reflux in patients with obstructive sleep apnea syndrome. Neurogastroenterol Motil. 2010;22:611–e172. doi: 10.1111/j.1365-2982.2010.01485.x. [DOI] [PubMed] [Google Scholar]
- 10.Kuribayashi S, Massey BT, Hafeezullah M, et al. Upper esophageal sphincter and gastroesophageal junction pressure changes act to prevent gastroesophageal reflux and esophagopharyngeal reflux in patients with obstructive sleep apnea. Chest. 2010;137:769–76. doi: 10.1378/chest.09-0913. [DOI] [PubMed] [Google Scholar]
- 11.Shepherd KL, Hillman D, Holloway RH, Eastwood P. Mechanisms of nocturnal gastroesophageal reflux events in obstructive sleep apnea. Sleep Breath. 2010;15:561–70. doi: 10.1007/s11325-010-0404-x. [DOI] [PubMed] [Google Scholar]
- 12.Ozturk O, Ozturk L, Ozdogan A, Oktem F, Pelin Z. Variables affecting the occurrence of gastroesophageal reflux in obstructive sleep apnea patients. Eur Arch Otorhinolaryngol. 2004;261:229–32. doi: 10.1007/s00405-003-0658-z. [DOI] [PubMed] [Google Scholar]
- 13.Heinemann S, Graf KI, Karaus M, Dorow P. Occurrence of obstructive sleep related respiratory disorder in conjunction with gastroesophageal reflux. Pneumologie. 1995;49:139–41. [PubMed] [Google Scholar]
- 14.Teramoto S, Ohga E, Matsui H, Ishii T, Matsuse T, Ouchi Y. Obstructive sleep apnea syndrome may be a significant cause of gastroesophageal reflux disease in older people. J Am Geriatr Soc. 1999;47:1273–74. doi: 10.1111/j.1532-5415.1999.tb05216.x. [DOI] [PubMed] [Google Scholar]
- 15.Morse CA, Quan SF, Mays MZ, Green C, Stephen G, Fass R. Is there a relationship between obstructive sleep apnea and gastroesophageal reflux disease? Clin Gastroenterol Hepatol. 2004;2:761–68. doi: 10.1016/s1542-3565(04)00347-7. [DOI] [PubMed] [Google Scholar]
- 16.Kim HN, Vorona RD, Winn MP, Doviak M, Johnson DA, Ware JC. Symptoms of gastro-oesophageal reflux disease and the severity of obstructive sleep apnoea syndrome are not related in sleep disorders center patients. Aliment Pharmacol Ther. 2005;21:1127–33. doi: 10.1111/j.1365-2036.2005.02447.x. [DOI] [PubMed] [Google Scholar]
- 17.Valipour A, Makker HK, Hardy R, Emegbo S, Toma T, Spiro SG. Symptomatic gastroesophageal reflux in subjects with a breathing sleep disorder. Chest. 2002;121:1748–53. doi: 10.1378/chest.121.6.1748. [DOI] [PubMed] [Google Scholar]
- 18.Clouse R, Parks T, Staiano A, Harolan L. AGA Abstracts. Gastroenterology. 2004;126:A–111. [Google Scholar]
- 19.Iber C, Ancoli-Israel S, Chesson A, Quan S. 1st ed. Westchester, IL: American Academy of Sleep Medicine; 2007. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. [Google Scholar]
- 20.Locke GR, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ., III Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology. 1997;112:1448–56. doi: 10.1016/s0016-5085(97)70025-8. [DOI] [PubMed] [Google Scholar]
- 21.Locke GR, Talley NJ, Weaver AL, Zinsmeister AR. A new questionairre for gastroesophageal reflux disease. Mayo Clin Proc. 1994;69:539–47. doi: 10.1016/s0025-6196(12)62245-9. [DOI] [PubMed] [Google Scholar]
- 22.Chiocca JC, Olmos JA, Salis GB, Soifer LO, Higa R, Marcolongo M. Prevalence, clinical spectrum and atypical symptoms of gastro-oesophageal reflux in Argentina: a nationwide population-based study. Aliment Pharmacol Ther. 2005;22:331–42. doi: 10.1111/j.1365-2036.2005.02565.x. [DOI] [PubMed] [Google Scholar]
- 23.Demeter P, Visy KV, Magyar P. Correlation between severity of endoscopic findings and apnea-hypopnea index in patients with gastroesophageal reflux disease and obstructive sleep apnea. World J Gastroenterol. 2005;11:839–41. doi: 10.3748/wjg.v11.i6.839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fass R, Quan SF, O'Connor GT, Ervin A, Iber C. Predictors of heartburn during sleep in a large prospective cohort study. Chest. 2005;127:1658–66. doi: 10.1378/chest.127.5.1658. [DOI] [PubMed] [Google Scholar]
- 25.Gislason T, Janson C, Vermeire P, et al. Respiratory symptoms and nocturnal gastroesophageal reflux: a population-based study of young adults in three european countries. Chest. 2002;121:158–63. doi: 10.1378/chest.121.1.158. [DOI] [PubMed] [Google Scholar]
- 26.DeMeester TR, Wernly JA, Bryant GH, Little AG, Skinner DB. Clinical and in vitro analysis of determinants of gastroesophageal competence. A study of the principles of antireflux surgery. Am J Surg. 1979;137:39–46. doi: 10.1016/0002-9610(79)90008-4. [DOI] [PubMed] [Google Scholar]
- 27.O'Sullivan GC, DeMeester TR, Joelsson BE, et al. Interaction of lower esophageal sphincter pressure and length of sphincter in the abdomen as determinants of gastroesophageal competence. Am J Surg. 1982;143:40–7. doi: 10.1016/0002-9610(82)90127-1. [DOI] [PubMed] [Google Scholar]
- 28.Fornari F, Callegari-Jacques SM, Dantas RO, Scarsi AL, Ruas LO, de Barros SG. Obese patients have stronger peristalsis and increased acid exposure in the esophagus. Dig Dis Sci. 2011;56:1420–26. doi: 10.1007/s10620-010-1454-4. [DOI] [PubMed] [Google Scholar]
- 29.Anggiansah R, Sweis R, Anggiansah A, Wong T, Cooper D, Fox M. The effects of obesity on oesophageal function, acid exposure and the symptoms of gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2013;37:555–63. doi: 10.1111/apt.12208. [DOI] [PubMed] [Google Scholar]
- 30.Derakhshan MH, Robertson EV, Fletcher J, et al. Mechanism of association between BMI and dysfunction of the gastro-oesophageal barrier in patients with normal endoscopy. Gut. 2012;61:337–43. doi: 10.1136/gutjnl-2011-300633. [DOI] [PubMed] [Google Scholar]
- 31.Pandolfino JE, El-Serag HB, Zhang Q, Shah N, Ghosh SK, Kahrilas PJ. Obesity: a challenge to esophagogastric junction integrity. Gastroenterology. 2006;130:639–49. doi: 10.1053/j.gastro.2005.12.016. [DOI] [PubMed] [Google Scholar]
- 32.Wu JC, Mui LM, Cheung CM, Chan Y, Sung JJ. Obesity is associated with increased transient lower esophageal sphincter relaxation. Gastroenterology. 2007;132:883–9. doi: 10.1053/j.gastro.2006.12.032. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


