Abstract
The objective of this study was to develop a model to aid clinicians in better predicting 1-year mortality rate for patients with an acute exacerbation of chronic obstructive pulmonary disease admitted to the medical intensive care unit (ICU) with the goal of earlier initiation of palliative care and end-of-life communications in this patient population. This retrospective cohort study included patients from a medical ICU from April 1, 1995, to November 30, 2009. Data collected from the Acute Physiology and Chronic Health Evaluation III database included demographic characteristics; severity of illness scores; noninvasive and invasive mechanical ventilation time; ICU and hospital length of stay; and ICU, hospital, and 1-year mortality. Statistically significant univariate variables for 1-year mortality were entered into a multivariate model, and the independent variables were used to generate a scoring system to predict 1-year mortality rate. At 1-year follow-up, 295 of 591 patients died (50%). Age and hospital length of stay were identified as independent determinants of mortality at 1 year by using multivariate analysis, and the predictive model developed had an area under the operating curve of 0.68. Bootstrap analysis with 1000 iterations validated the model, age, and hospital length of stay, entered the model 100% of the time (area under the operating curve=0.687; 95% CI, 0.686–0.688). A simple model using age and hospital length of stay may be informative for providers willing to identify patients with chronic obstructive pulmonary disease with high 1-year mortality rate who may benefit from end-of-life communications and from palliative care.
Chronic obstructive pulmonary disease (COPD), the fourth ranked cause of death in the United States, is a heterogeneous disease with an unpredictable course.1,2 Previous work oriented toward prognosis and advance care planning aimed to identify factors associated with mortality during and after a hospitalization for an acute exacerbation of COPD.2–10 Despite our increased understanding, there remains a disconnect between this knowledge and its application to patient care. Clinicians struggle to reliably predict outcomes for patients hospitalized with a COPD exacerbation.1,11,12 In particular, a hospital admission for a COPD exacerbation that requires intensive care represents a significant milestone that may merit advanced care planning and could be an opportunity to initiate end-of-life communications. Early referral to palliative care has been shown to improve quality of life, patient satisfaction, and survival in patients with incurable lung cancer.13–15 Interestingly, when compared with those with a malignancy, despite equal or higher ratings of symptom severity, including pain and dyspnea, patients with COPD are less likely to be offered palliative care services.16–18 It has been demonstrated that patients with COPD and their health care providers are hesitant to discuss goals of care and palliative treatment and are more likely to have conversations about end-of-life care when these patients are in extremis or hospitalized than when stable in the outpatient setting.17,19
The objective of this study was to develop a model with simple variables robust enough to predict mortality rate at 1 year in a patient population with high risk of death, like those with an acute exacerbation of COPD requiring admission to an intensive care unit (ICU), in a time frame appropriate to initiate palliative care. The latter could have a substantial effect on the quality of life of patients and caregivers and on our health care system by avoiding unnecessary hospitalizations.
PATIENTS AND METHODS
This retrospective cohort study reviewed admissions to the medical ICU of a tertiary academic medical center from April 1, 1995, to November 30, 2009. Data were abstracted from an Acute Physiology and Chronic Health Evaluation III (APACHE III) database for patients 18 years or older. This study was approved by the Mayo Foundation Institutional Review Board (number 1283-01).
Baseline demographic characteristics collected included age, sex, and race. Factors from the hospital course retrieved from the database were ICU admission diagnosis, Sequential Organ Failure Assessment (SOFA) score on admission, APACHE III score on admission, ICU and hospital length of stay, and the use and duration of invasive or noninvasive mechanical ventilation. ICU, hospital, and 1-year mortality data were collected by reviewing survival status and date of death in the medical record.
Data were summarized as mean ± SD, median (interquartile range), or percentage. Univariate analysis was performed to identify variables associated with 1-year mortality. Those of statistical significance were then entered into a stepwise multivariate logistic regression analysis to identify independent variables affecting 1-year mortality. Once the independent variables were identified, we transformed the continuous predictor variables into categorical variables by using their quartile values. Nominal logistic analysis was performed by using the subgroups to predict 1-year mortality. The odds ratio for 1-year mortality for each subgroup was then used to assign a score for each quartile, a method previously reported.20 Odds ratios were rounded up or down to assign a score. Those odds ratios with a 95%CI crossing 1 were not assigned points. The scores for all the independent predictor variables were added, and a total mortality score was generated for each patient. The capability of the scoring system was evaluated by using area under the operating curve (AUC).
Bootstrap analysis was performed for confirmation of internal validity of the model because it has been shown to be an acceptable means to internally validate predictive models.21 This is a statistical method that randomly samples with replacement a study sample of the same size from the original study sample from which the prediction model was developed. The bootstrap samples are similar but not identical to the study sample and a model is created from each bootstrap sample with its own AUC. The AUC from a bootstrap analysis reflects how the model would likely perform when applied to similar individuals from a new or external population.22
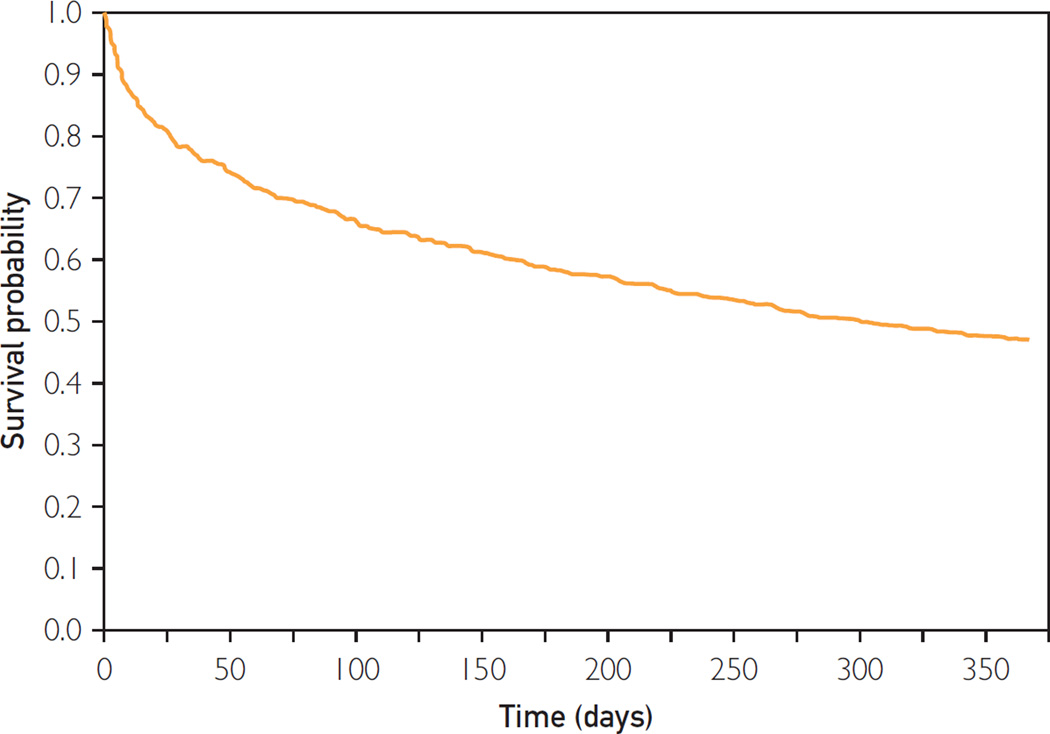
Model calibration was evaluated on the basis of goodness of fit by using the Hosmer-Lemeshow chi-square statistic, with lower chi-square values and higher P values indicative of better fit. Model discrimination was assessed on the basis of receiver operating characteristics-AUC, with a receiver operating characteristic -AUC of 0.5 indicative of the effects of chance alone and a receiver operating characteristic-AUC of 1 indicative of faultless discrimination. A Cox proportional hazards regression model comparing years 1995–2000, 2001–2005, and 2006–2009 was used to determine whether the year of admission affected the mortality rate. A Kaplan-Meier survival curve for the 1-year period was constructed.
RESULTS
There were 25,287 admissions to the medical ICU, based on the documented admission diagnosis by ICU nurses trained in APACHE definitions; 761 admissions (3%) were for acute exacerbation of COPD. Of these admissions, 130 patients had more than 1 episode of care in the ICU, and for these patients, data from only the first hospital admission were used for analysis. After excluding 40 patients lost to follow-up at 1 year, a total of 591 patients were included in the analysis. Similar to previous studies, the population analyzed represents a small portion of all ICU admissions.2,23
Among the 591 patients, 51% were men, 93% were Caucasian, and the mean age was 70±11 years. The mean APACHE III and SOFA scores on the day of admission were 41±19 and 3±2, respectively. At 1 year from the time of ICU admission, 295 of 591 patients had died (50%). Forty-one patients (7%) died while in the ICU, and 87 patients (15%) died before discharge from the hospital. The median ICU length of stay was 2 days (interquartile range, 1–3), and the median hospital length of stay was 5 days (interquartile range, 3–9).
The variables with a statistically significant univariate association with 1-year mortality were age, ICU and hospital length of stay, use of noninvasive ventilation, and SOFA and APACHE III scores on the day of admission. There was no statistically significant association between 1-year mortality and race, sex, or the use of invasive mechanical ventilation.
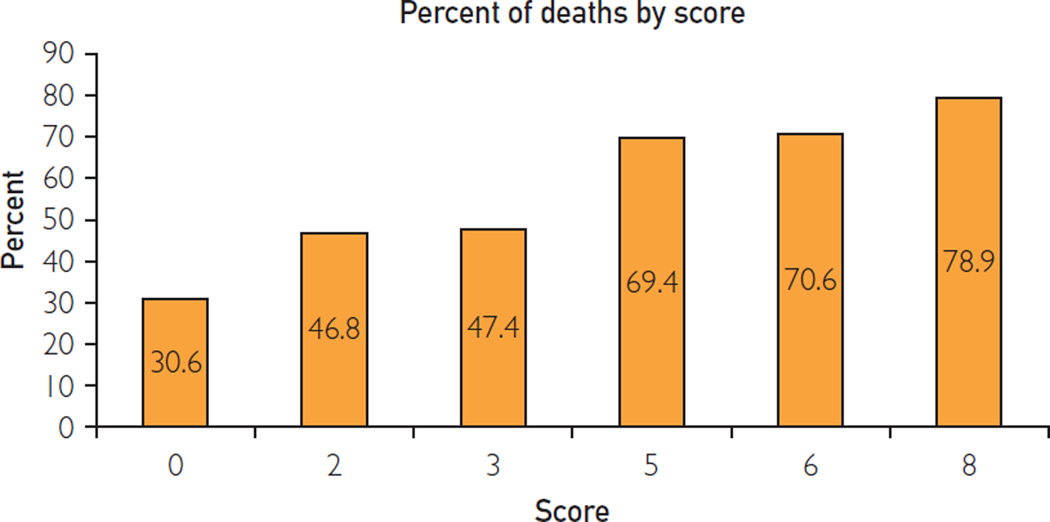
The stepwise multivariate logistic regression model showed age and hospital length of stay to be independently associated with 1-year mortality as shown in Table 1. The quartile subgroups of hospital length of stay and age as well as the odds ratio for mortality are described in Table 2. After creating a mortality score by using the odds ratios, the model showed an increased chance of death at 1 year with increasing scores and had an AUC of 0.68. Bootstrap analysis was performed with 1000 bootstraps of the logistic model. The score variable entered the model 100% of the time. The estimated AUC was 0.687, with a 95% CI of 0.686 to 0.688. The probability of death for each possible score is shown in Figure 1. The model calibration was confirmed on the basis of goodness of fit by using the Hosmer-Lemeshow chi-square statistic (P=.759). The analysis was repeated with exclusion of patients who expired before hospital discharge, and there was no change in the development or predictive capacity of the model. The Cox proportional hazards regression model comparing the mortality rate between years 1995 and 2000, 2001 and 2005, and 2006 and 2009 showed that there was no significant difference in the mortality rate based on the year of admission (P=.76). The Kaplan-Meier survival curve constructed for the 1-year time period is shown in Figure 2.
TABLE 1.
Multivariate Logistic Regression Analysis of Variables Predictive of 1-Year Mortality in Patients With COPD Admitted to the ICU With Acute Exacerbation
| Variables | Likelihood ratio | |
|---|---|---|
| χ2 | Probability>χ2 | |
| Age | 44.43 | <.0001 |
| Hospital length of stay | 13.12 | .003 |
| SOFA score on admission | 2.95 | .09 |
| ICU length of stay | 1.50 | .22 |
| Use of noninvasive ventilation | 0.55 | .46 |
| APACHE III score on admission | 0.17 | .68 |
APACHE III = Acute Physiology and Chronic Health Evaluation III; COPD = chronic obstructive pulmonary disease; ICU = intensive care unit; SOFA = Sequential Organ Failure Assessment.
TABLE 2.
Points Assigned on the Basis of Odds Ratio of Mortality for Quartiles of Age and HLOSa
| Odds Ratio Estimates | ||||
|---|---|---|---|---|
| Effect | Point estimate | 95% Wald confidence limits |
Points assigned | |
| Age 80+ y vs <65 y | 6.217 | 3.575 | 10.812 | 6 |
| Age 70–79 y vs <65 y | 2.757 | 1.783 | 4.261 | 3 |
| Age 65–69 y vs <65 y | 1.605 | 0.950 | 2.713 | 0b |
| HLOS >9 d vs <4 d | 2.511 | 1.599 | 3.944 | 2 |
| HLOS >7–9 d vs <4 d | 2.011 | 1.110 | 3.644 | 2 |
| HLOS >5–7 d vs <4 d | 1.245 | 0.755 | 2.054 | 0b |
| HLOS 4–5 d vs <4 d | 1.322 | 0.705 | 2.477 | 0b |
HLOS = hospital length of stay.
Indicates that no points were assigned as the 95% CI crossed 1.
FIGURE 1.
Probability of 1-year mortality based on proposed scoring system.
FIGURE 2.
Kaplan-Meier survival curve for the 1-year period.
DISCUSSION
Our study found that a simple model using age and hospital length of stay had good ability to inform clinicians about predicting 1-year mortality rate for patients with COPD admitted to the ICU with an acute exacerbation. The proposed easy-to-use model can add to the physician’s intuition about the advent of end of life. We believe that predicting 1-year survival in this clinical situation is important because it may facilitate timely referral to palliative care, a well-reported deficit in our current COPD care.13,18,24 As an example in our model, a patient aged 72 years with a hospital length of stay of 7 days would be assigned a score of 5 points. This score corresponds to a predicted 1-year mortality rate of 70%. In our cohort, 32% of the patients had a score of 5 points or more. If we consider that our sample is representative, using this simple model may allow health care providers to consider the initiation of palliative care services in that percentage of individuals.
Our hospital and 1-year mortality rate of 14% and 49% fall in line with previously reported data on hospital and 1-year mortality, which ranged from 11% to 24% and from 17% to 59%, respectively.2,3,5–7 Interestingly, in our study, markers of disease severity including APACHE III and SOFA scores and the use of mechanical ventilation were not independently associated with 1-year mortality once accounting for age and hospital length of stay. The lack of relation between APACHE III and SOFA scores and 1-year mortality is not surprising because these scores are related to short-term mortality end points primarily. The lack of significance between the use of invasive or noninvasive mechanical ventilation and mortality was surprising because previous studies have shown better outcomes associated with the use of noninvasive ventilation.25–27 However, given the small sample of mechanically ventilated patients in this study, it may not be adequately powered to address this topic.
The development and use of models to predict mortality is clinically relevant because many studies have shown that a physician’s ability to predict the outcome of a patient with COPD hospitalized with an acute exacerbation is unreliable.4,5,11,12 Predictive models and scoring systems are used more frequently today as an adjunct to clinical decision making and provider’s intuition regarding patient prognosis and ideal next steps in care. Although models and scoring systems are developed from cohorts of patients, the overall goal of developing them would be to apply their use not only to a cohort of patients but also to be able to use them on an individual case-by-case basis as additional prognostic tools to aid in clinical decision making. To date, most models predict solely in-hospital mortality and, or, are moderately complex with incorporation of 5 or more clinically relevant variables. One of the strengths of our work is its simplicity and use of objective factors that are easily accessible. Our model’s predictive capability is not meaningfully inferior to those of similar studies looking at short-term mortality after hospital discharge.5,12 Connors et al5 developed a multivariate model from seriously ill patients with acute exacerbation of COPD that had good discrimination (AUC 0.73) to predict survival at 180 days by using age, body mass index (calculated as the weight in kilograms divided by the height in meters squared), acute physiology score, albumin, presence of congestive heart failure or cor pulmonale, arterial partial pressure of oxygen/fraction of inspired oxygen concentration, and activities of daily living. Roche et al28 developed a model with good discrimination (AUC 0.79) of hospital mortality, but it incorporated the subjective indices, lower limb edema, and use of accessory muscles of respiration. The use of subjective variables represents a limitation because consistent translation to other studies cannot be guaranteed. In addition, their study excluded patients admitted to the ICU, a significant “at-risk population.”
More recently, a model with strong predictive value of hospital and 30-daymortality for patients with acute exacerbations of COPD (AUC 0.86) was based on dyspnea score, eosinopenia, consolidation, atrial fibrillation, and acidemia.21 However, it excluded patients in an ICU setting and did not examine the model’s utility beyond 30 days posthospitalization, making it less practical for initiation of the palliative process. The model of Wildman et al12 predicted 180-day mortality after admission to an ICU for acute exacerbation of COPD that had good discrimination (AUC 0.747).12 Although this model performed better than clinicians in predicting 180-day mortality, it requires the collection of more than 15 data points/factors, making it difficult to use in clinical settings.
Similar to our results, Seneff et al2 identified age 65 years and older as having a significant association with 1-year mortality. Consistent with our findings, related work has identified no association between factors such as physiologic derangement, use of mechanical ventilation, or multiorgan dysfunction, and likelihood of death at 2 or 5 years after ICU admission for acute exacerbation of COPD.8,9 A recent review by Messer et al4 found that length of hospital stay before ICU admission and abnormally high acute physiology score were independently predictive of 6-month mortality.4 However, in contrast to our work and because of the nature of the publication, a literature review, they were unable to create a model for translation to clinical use.
The results of our study could have a significant effect by stimulating the early involvement of palliative care services. Palliative care has been associated with better symptom control and improved quality of life and health care for patients.13–15 In this patient population in which it has been shown that patients have little understanding of their disease and significant anxieties regarding what their end of life will entail, it is especially important to identify those patients who are appropriate for palliative care referral.16–19,29 We believe that our analysis targeted a population at high risk of short-term mortality: approximately 40% of Medicare decedents in 2009 with a diagnosis of COPD had an ICU stay within the last months of life and 20% had 3 or more hospitalizations within the last 90 days of life.30
Limitations
Our study focused solely on patients with an acute exacerbation of COPD admitted to a single center, tertiary referral medical ICU. Our study population was largely Caucasian. The analysis did not include some potentially important variables such as body mass index, an assessment of dyspnea, forced expiratory volume over 1 second, or cardiovascular comorbidities. However, we included comprehensive physiologic data (APACHE) that ended up not being more meaningful than age and hospital length of stay. Information regarding the dismissal disposition and resuscitation, or code, status of patients in our study sample was not reliably ascertainable from the medical record and may have provided clinically useful information. The model’s AUC is lower than that of the other predictive models referenced. However, in comparison to those models, many of which incorporate a greater number of variables, use subjective factors, or exclude patients in an ICU setting, this model is simple with use of only 2 objective factors. As such, this work and model can still provide meaningful contributions because it can be easily applied to patient care. The model’s performance on internal validation was good; however, further external validation of the model in other patient populations may be prudent. The effect of hospital length of stay may not be the same in other institutions because ICU and hospital length of stay can be affected by variation in ICU admission policies, as well as by availability of nursing home or other acute care beds.
CONCLUSION
Patients with COPD admitted with an acute exacerbation to a medical ICU have a substantial risk of mortality within 1 year after admission. The simple factors of age and hospital length of stay can be used to predict the likelihood of mortality within 1 year and help guide the timing of critical end-of-life care discussions and involvement of palliative care services with the goal of improving patient quality of life and reducing the costs of end-of-life care.
Acknowledgments
This work is dedicated to the memory of Dr Bekele Affesa, a pioneer in research regarding the outcome of intensive care patients. His thoughts were seminal to this project. Dr Afessa died on January 10, 2013, at the age of 57 years. He is survived by his 3 brothers, 1 sister, many nieces and nephews, and innumerable friends.
Grant Support: This publication was supported by Grant NIH–NHLBI 5R01HL094680-05) (PI Roberto Benzo).
Abbreviations and Acronyms
- APACHE III
Acute Physiology and Chronic Health Evaluation III
- AUC
area under the operating curve
- COPD
chronic obstructive pulmonary disease
- ICU
intensive care unit
- SOFA
Sequential Organ Failure Assessment
REFERENCES
- 1.Mannino DM, Watt G, Hole D, et al. The natural history of chronic obstructive pulmonary disease. Eur Respir J. 2006;27(3):627–643. doi: 10.1183/09031936.06.00024605. [DOI] [PubMed] [Google Scholar]
- 2.Seneff MG, Wagner DP, Wagner RP, Zimmerman JE, Knaus WA. Hospital and 1-year survival of patients admitted to intensive care units with acute exacerbation of chronic obstructive pulmonary disease. JAMA. 1995;274(23):1852–1857. [PubMed] [Google Scholar]
- 3.Breen D, Churches T, Hawker F, Torzillo PJ. Acute respiratory failure secondary to chronic obstructive pulmonary disease treated in the intensive care unit: a long term follow up study. Thorax. 2002;57(1):29–33. doi: 10.1136/thorax.57.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Messer B, Griffiths J, Baudouin SV. The prognostic variables predictive of mortality in patients with an exacerbation of COPD admitted to the ICU: an integrative review. QJM. 2012;105(2):115–126. doi: 10.1093/qjmed/hcr210. [DOI] [PubMed] [Google Scholar]
- 5.Connors AF, Jr, Dawson NV, Thomas C, et al. Outcomes following acute exacerbation of severe chronic obstructive lung disease. The SUPPORT investigators (Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments) Am J Respir Crit Care Med. 1996;154(4, Pt 1):959–967. doi: 10.1164/ajrccm.154.4.8887592. [DOI] [PubMed] [Google Scholar]
- 6.Piquet J, Chavaillon JM, David P, Martin F, Blanchon F, Roche N. French College of General Hospital Respiratory Physicians (CPHG). High-risk patients following hospitalisation for an acute exacerbation of COPD(78/90) Eur Respir J. 2013;42(4):946–955. doi: 10.1183/09031936.00180312. [DOI] [PubMed] [Google Scholar]
- 7.Groenewegen KH, Schols AM, Wouters EF. Mortality and mortality-related factors after hospitalization for acute exacerbation of COPD. Chest. 2003;124(2):459–467. doi: 10.1378/chest.124.2.459. [DOI] [PubMed] [Google Scholar]
- 8.Raurich JM, Pérez J, Ibáñez J, Roig S, Batle S. In-hospital and 2-year survival of patients treated with mechanical ventilation for acute exacerbation of COPD [in Spanish] Arch Bronconeumol. 2004;40(7):295–300. doi: 10.1016/s1579-2129(06)60305-4. [DOI] [PubMed] [Google Scholar]
- 9.Ai-Ping C, Lee KH, Lim TK. In-hospital and 5-year mortality of patients treated in the ICU for acute exacerbation of COPD: a retrospective study. Chest. 2005;128(2):518–524. doi: 10.1378/chest.128.2.518. [DOI] [PubMed] [Google Scholar]
- 10.Bustamante-Fermosel A, De Miguel-Yanes JM, Duffort-Falcó M, Muñoz J. Mortality-related factors after hospitalization for acute exacerbation of chronic obstructive pulmonary disease: the burden of clinical features. Am J Emerg Med. 2007;25(5):515–522. doi: 10.1016/j.ajem.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 11.Wildman MJ, Sanderson C, Groves J, et al. Implications of prognostic pessimism in patients with chronic obstructive pulmonary disease (COPD) or asthma admitted to intensive care in the UK within the COPD and asthma outcome study (CAOS): multicentre observational cohort study. BMJ. 2007;335(7630):1132. doi: 10.1136/bmj.39371.524271.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wildman MJ, Sanderson C, Groves J, et al. Predicting mortality for patients with exacerbations of COPD and Asthma in the COPD and Asthma Outcome Study (CAOS) QJM. 2009;102(6):389–399. doi: 10.1093/qjmed/hcp036. [DOI] [PubMed] [Google Scholar]
- 13.Leung JM, Udris EM, Uman J, Au DH. The effect of end-of-life discussions on perceived quality of care and health status among patients with COPD. Chest. 2012;142(1):128–133. doi: 10.1378/chest.11-2222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yoong J, Park ER, Greer JA, et al. Early palliative care in advanced lung cancer: a qualitative study. JAMA Intern Med. 2013;173(4):283–290. doi: 10.1001/jamainternmed.2013.1874. [DOI] [PubMed] [Google Scholar]
- 15.Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363(8):733–742. doi: 10.1056/NEJMoa1000678. [DOI] [PubMed] [Google Scholar]
- 16.Giacomini M, DeJean D, Simeonov D, Smith A. Experiences of living and dying with COPD: a systematic review and synthesis of the qualitative empirical literature. Ont Health Technol Assess Ser. 2012;12(13):1–47. [PMC free article] [PubMed] [Google Scholar]
- 17.Carlucci A, Guerrieri A, Nava S. Palliative care in COPD patients: is it only an end-of-life issue? Eur Respir Rev. 2012;21(126):347–354. doi: 10.1183/09059180.00001512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Curtis JR. Palliative and end-of-life care for patients with severe COPD. Eur Respir J. 2008;32(3):796–803. doi: 10.1183/09031936.00126107. [DOI] [PubMed] [Google Scholar]
- 19.Curtis JR, Engelberg RA, Nielsen EL, Au DH, Patrick DL. Patient-physician communication about end-of-life care for patients with severe COPD. Eur Respir J. 2004;24(2):200–205. doi: 10.1183/09031936.04.00010104. [DOI] [PubMed] [Google Scholar]
- 20.Kim JY, Schierle CF, Subramanian VS, et al. A prognostic model for the risk of development of upper extremity compartment syndrome in the setting of brachial artery injury. Ann Plast Surg. 2009;62(1):22–27. doi: 10.1097/SAP.0b013e3181776327. [DOI] [PubMed] [Google Scholar]
- 21.Steer J, Gibson J, Bourke SC. The DECAF Score: predicting hospital mortality in exacerbations of chronic obstructive pulmonary disease. Thorax. 2012;67(11):970–976. doi: 10.1136/thoraxjnl-2012-202103. [DOI] [PubMed] [Google Scholar]
- 22.Moons KG, Kengne AP, Woodward M, et al. Risk prediction models: I. Development, internal validation, and assessing the incremental value of a new (bio)marker. Heart. 2012;98(9):683–690. doi: 10.1136/heartjnl-2011-301246. [DOI] [PubMed] [Google Scholar]
- 23.Rivera-Fernández R, Navarrete-Navarro P, Fernández-Mondejar E, Rodriguez-Elvira M, Guerrero-López F, Vázquez-Mata G. Project for the Epidemiological Analysis of Critical Care Patients (PAEEC) Group. Six-year mortality and quality of life in critically ill patients with chronic obstructive pulmonary disease. Crit Care Med. 2006;34(9):2317–2324. doi: 10.1097/01.CCM.0000233859.01815.38. [DOI] [PubMed] [Google Scholar]
- 24.Steer J, Gibson GJ, Bourke SC. Predicting outcomes following hospitalization for acute exacerbations of COPD. QJM. 2010;103(11):817–829. doi: 10.1093/qjmed/hcq126. [DOI] [PubMed] [Google Scholar]
- 25.Lightowler JV, Wedzicha JA, Elliott MW, Ram FS. Non-invasive positive pressure ventilation to treat respiratory failure resulting from exacerbations of chronic obstructive pulmonary disease: Cochrane systematic review and meta-analysis. BMJ. 2003;326(7382):185. doi: 10.1136/bmj.326.7382.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Plant PK, Owen JL, Elliott MW. Early use of non-invasive ventilation for acute exacerbations of chronic obstructive pulmonary disease on general respiratory wards: a multicentre randomised controlled trial. Lancet. 2000;355(9219):1931–1935. doi: 10.1016/s0140-6736(00)02323-0. [DOI] [PubMed] [Google Scholar]
- 27.Dikensoy O, Ikidag B, Filiz A, Bayram N. Comparison of non-invasive ventilation and standard medical therapy in acute hypercapnic respiratory failure: a randomised controlled study at a tertiary health centre in SE Turkey. Int J Clin Pract. 2002;56(2):85–88. [PubMed] [Google Scholar]
- 28.Roche N, Zureik M, Soussan D, Neukirch F, Perrotin D. Urgence BPCO (COPD Emergency) Scientific Committee. Predictors of outcomes in COPD exacerbation cases presenting to the emergency department. Eur Respir J. 2008;32(4):953–961. doi: 10.1183/09031936.00129507. [DOI] [PubMed] [Google Scholar]
- 29.Gardiner C, Gott M, Small N, et al. Living with advanced chronic obstructive pulmonary disease: patients concerns regarding death and dying. Palliat Med. 2009;23(8):691–697. doi: 10.1177/0269216309107003. [DOI] [PubMed] [Google Scholar]
- 30.Teno JM, Gozalo PL, Bynum JP, et al. Change in end-of-life care for Medicare beneficiaries: site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA. 2013;309(5):470–477. doi: 10.1001/jama.2012.207624. [DOI] [PMC free article] [PubMed] [Google Scholar]