ABSTRACT
Infections with Sudan virus (SUDV), a member of the genus Ebolavirus, result in a severe hemorrhagic fever with a fatal outcome in over 50% of human cases. The paucity of prophylactics and therapeutics against SUDV is attributed to the lack of a small-animal model to screen promising compounds. By repeatedly passaging SUDV within the livers and spleens of guinea pigs in vivo, a guinea pig-adapted SUDV variant (SUDV-GA) uniformly lethal to these animals, with a 50% lethal dose (LD50) of 5.3 × 10−2 50% tissue culture infective doses (TCID50), was developed. Animals infected with SUDV-GA developed high viremia and died between 9 and 14 days postinfection. Several hallmarks of SUDV infection, including lymphadenopathy, increased liver enzyme activities, and coagulation abnormalities, were observed. Virological analyses and gross pathology, histopathology, and immunohistochemistry findings indicate that SUDV-GA replicates in the livers and spleens of infected animals similarly to SUDV infections in nonhuman primates. These developments will accelerate the development of specific medical countermeasures in preparation for a future disease outbreak due to SUDV.
IMPORTANCE A disease outbreak due to Ebola virus (EBOV), suspected to have emerged during December 2013 in Guinea, with over 11,000 dead and 28,000 infected, is finally winding down. Experimental EBOV vaccines and treatments were administered to patients under compassionate circumstances with promising results, and availability of an approved countermeasure appears to be close. However, the same range of experimental candidates against a potential disease outbreak caused by other members of the genus Ebolavirus, such as Sudan virus (SUDV), is not readily available. One bottleneck contributing to this situation is the lack of a small-animal model to screen promising drugs in an efficient and economical manner. To address this, we have generated a SUDV variant (SUDV-GA) that is uniformly lethal to guinea pigs. Animals infected with SUDV-GA develop disease similar to that of SUDV-infected humans and monkeys. We believe that this model will significantly accelerate the development of life-saving measures against SUDV infections.
INTRODUCTION
The genus Ebolavirus contains 5 genetically distinct filoviruses: Ebola virus (EBOV), Sudan virus (SUDV), Bundibugyo virus, Taï Forest virus, and Reston virus. The first four of those filoviruses are associated with severe hemorrhagic fever in humans. The first documented infections occurred in 1976, when EBOV and SUDV emerged almost simultaneously in Zaire (presently Democratic Republic of the Congo) and Sudan (presently South Sudan), respectively (1, 2). In that year, EBOV infections resulted in a case fatality rate (CFR) of 88% (280 deaths, 318 infected), and SUDV infections resulted in a CFR of 53% (151 deaths, 284 infected). Since then, ebolaviruses have sporadically reemerged in sub-Saharan Africa, with the most infections and deaths caused by EBOV, followed by SUDV.
As of September 2015, 18 months after it was first reported, the EBOV disease outbreak centered in the western African nations of Guinea, Sierra Leone, and Liberia had resulted in over 11,000 deaths and 28,000 infections (3). Experimental vaccines and therapeutics which had been in development for over 15 years prior to the outbreak were deployed for use in humans on a compassionate basis, and several candidates, including the vesicular stomatitis Indiana virus (VSV)-vectored and chimpanzee adenovirus type 3 (ChAd3)-vectored vaccines (4, 5), a small molecule (favipiravir) (6), and a monoclonal antibody (MAb) cocktail (ZMapp) (7), are now being evaluated in clinical trials. One of the reasons for the availability of experimental candidates against EBOV was the development of EBOV variants adapted to rodents such as mice in 1998 (8) and guinea pigs in 1999 (9). These advances allowed researchers to test potentially efficacious drugs in an efficient and economical manner and to press forward with the most promising compounds in nonhuman primates (NHPs), which are considered the gold standard model to study filovirus infections.
SUDV is endemic in South Sudan and the Republic of Uganda. By definition, the pathogen is classified as SUDV if the full-length viral genome differs by ≥30% from the EBOV genome and by <30% from the SUDV type virus (10). SUDV infections are highly lethal to humans, killing 421 patients in 786 total cases (CFR of 53.6%) from all past documented outbreaks, with the most recent occurring in 2012 to 2013 (11). Before the EBOV disease outbreak in western Africa, the largest filovirus outbreak was seen with SUDV in Uganda during 2000 to 2001 and resulted in 224 deaths in 425 total cases (CFR of 53%).
Unlike EBOV, there is a comparative lack of experimental medical countermeasures against SUDV due to the absence of a small-animal model to screen antivirals against SUDV. Past studies showed that AG129 (alpha/beta interferon [IFN-α/βCFR R−/−) mice are susceptible to wild-type SUDV infections (12) and that an adapted SUDV was partially lethal to approximately 25% of guinea pigs (13). A more stringent intermediate animal model is needed to screen candidate drugs more effectively before progression to studies in NHPs. The goal of this study was to develop and characterize a guinea pig-adapted SUDV variant that is fully lethal to guinea pigs (SUDV-GA). Analysis of the SUDV-GA genome and calculation of the median lethal dose (LD50) as well as the clinical profiles and pathologies of animals after infection are presented.
MATERIALS AND METHODS
Ethics statement.
The animal work described in this study was performed in the biosafety level 4 (BSL-4) facility at the National Microbiology Laboratory located in Winnipeg, Canada, and was approved by the Animal Care Committee (ACC) based at the Canadian Science Center for Human and Animal Health (CSCHAH), in accordance with Canadian Council on Animal Care (CCAC) guidelines. Animals were acclimatized for 14 days before infection, given food and water ad libitum, and monitored twice daily.
Animals, cells, and viruses.
Female guinea pigs, strain Hartley (Charles River) (6 to 8 weeks of age), were used for the studies. Wild-type Sudan virus, isolate Boneface (GenBank accession no. FJ968794.1), was isolated from the acute-phase blood of a patient during the 1976 outbreak in Sudan. The progenitor isolate used for the initial inoculations in guinea pigs was a stock preparation from the original clinical sample that had previously been passaged once in guinea pigs and twice on VeroE6 cells. This progenitor virus was designated Sudan virus/C.porcellus-lab/SSD/1976/Nzara-Boneface (SUDV-p), in accordance with established guidelines (14, 15). The sequence is not identical to that of wild-type SUDV; thus, the viral sequence of SUDV-p has been deposited in GenBank. The guinea pig-adapted virus generated in this study was designated Sudan virus/NML/C.porcellus-lab/SSD/1976/Nzara-Boneface-GP (SUDV-GA), in accordance with the guidelines referenced above. Stock SUDV-p and SUDV-GA were grown on Vero E6 cells (ATCC).
Serial passaging.
Two guinea pigs were each given an intraperitoneal (i.p.) injection with ∼105 TCID50 of SUDV-p–1 ml of Dulbecco's modified Eagle's medium (DMEM), supplemented with 2% heat-inactivated fetal bovine serum (FBS) (Sigma). The liver and spleen were removed from euthanized animals at 7 days postinfection (dpi), pooled, and then homogenized by grinding the organs against a steel mesh using a sterile plastic plunger. Cells were then suspended in 10 ml of phosphate-buffered saline (PBS) and centrifuged at 400 × g for 5 min. The supernatant was passed through a cell strainer, and the cell pellet was then homogenized with a tissue homogenizer. The supernatant was also passed through the cell strainer after centrifugation at 400 × g for 5 min. Two naive guinea pigs were then injected i.p. with 1 ml of the filtered supernatant each and euthanized at 7 dpi to harvest livers and spleens for the next passage. This process was repeated until passage 25. The resultant SUDV-GA at passage 25 was not plaque purified.
Infection experiments.
To determine the median (50%) lethal dose (LD50) of SUDV-GA, guinea pigs (n = 3 per dilution) were infected i.p. with serial 10-fold dilutions of virus ranging between 3.55 × 10−2 and 3.55 × 103 50% tissue culture infective doses (TCID50). Animals were weighed daily and monitored for survival, weight change, and clinical signs of disease.
To characterize the pathogenesis of the adapted virus, groups of guinea pigs (n = 3 per time point) were infected i.p. with 1,000× LD50 (53 TCID50) of SUDV-GA or with an equivalent dose of SUDV-p. Sampling occurred at 0, 5, 9, and 11 dpi. Whole blood was collected in K2 EDTA Plus blood collection tubes (BD Biosciences) for blood counts and determination of viremia. Blood was collected in SST Plus blood collection tubes (BD Biosciences) for serum biochemistry and in sodium citrate blood collection tubes (BD Biosciences) for coagulation studies. For serum biochemistry and coagulation studies, the samples were centrifuged at 2,500 rpm (1,000 × g) for 10 min before the serum and plasma, respectively, were collected for analysis. Groups of guinea pigs (n = 3 per time point) from each infection group were also euthanized at 0, 5, 9, and 11 dpi with the aim of harvesting the livers and spleens of these animals. Parts of the organs were stored in 1 ml of DMEM supplemented with 2% heat-inactivated FBS and were then homogenized in a tissue homogenizer. Samples were then spun at 400 × g for 5 min and frozen at −80°C until processing.
Histopathology and IHC.
Liver and spleen tissues harvested from guinea pigs were fixed in 10% neutral phosphate-buffered formalin, routinely processed, sectioned at 5-μm intervals, and stained with hematoxylin and eosin (HE) for histopathologic examination. For immunohistochemistry (IHC) analyses, paraffin tissue sections were quenched for 10 min in aqueous 3% hydrogen peroxide. Epitopes were retrieved using Dako Target Retrieval solution (Dako, USA) in a Biocare Medical Decloaking Chamber. The primary antibody applied to the sections was a mouse anti-SUDV glycoprotein (GP) monoclonal antibody (F344G5 [a MAb against the glycoprotein of SUDV generated in house]), which was used at a 1:800 dilution for 30 min. The slides were then visualized using a horseradish peroxidase-labeled polymer, Envision+ (anti-mouse) system (Dako, USA) and reacted with the chromogen diaminobenzidine (DAB). The sections were then counterstained with Gill's hematoxylin.
Blood counts and serum biochemistry.
Complete blood counts were performed using a VetScan HM5 hematology system (Abaxis Veterinary Diagnostics) per manufacturer instructions. Analysis of serum biochemistry was done with a VetScan VS2 analyzer (Abaxis Veterinary Diagnostics) per manufacturer instructions. Coagulation studies were performed on a STart4 instrument (Diagnostica Stago) per manufacturer instructions.
Determination of virus titers by reverse transcription-quantitative PCR (RT-qPCR).
Total RNA was extracted from whole blood with a QIAamp viral RNA minikit (Qiagen) or from tissue homogenates with an RNeasy minikit (Qiagen). Viral genomes were detected with a LightCycler 480 RNA master hydrolysis probe kit (Roche), with the RNA polymerase as the target gene. The reaction conditions used with an ABI StepOnePlus instrument were as follows: 63°C for 3 min, 95°C for 30 s, and then 45 cycles of 95°C for 15 s and 60°C for 30 s. Primer and probe sequences used in the reactions were as follows: forward, CAGAAGACAATGCAGCCAGA; reverse, TTGAGGAATATCCCACAGGC; probe, 6-carboxyfluorescein [FAM]-CTGCTAGCTTGGCCAAAGTCACAAG-black hole quencher [BHQ].
Sequencing of the SUDV-GA viral genome.
SUDV-GA was sequenced using the same methods as previously described (16). The sequences were then assembled in DNAStar Lasergene 12 SeqMan using the sequence available under GenBank accession number FJ968794.1 as the reference sequence.
Statistical analysis.
Statistical comparisons of the data on serum biochemistry, blood counts, and viremia as well as liver and spleen titers were carried out as described in a previous publication (16). Log transformations were not applied to any parameters, with the exception of viremia (which was heteroscedastic), because they all passed Levene's test. For all analyses, statistical significance was set at a P value of <0.05. A P value of <0.05 was considered significant, a P value of <0.01 was considered very significant, and a P value of <0.001 was considered extremely significant.
Nucleotide sequence accession number.
The sequence of SUDV-GA has been deposited in GenBank, and the accession number is KT750754. The viral sequence of SUDV-p has been deposited in GenBank, and the accession number is KT878488.
RESULTS
Generation of a guinea pig-adapted SUDV by serial passaging and viral genome analysis.
Infection of Hartley guinea pigs with a progenitor SUDV (SUDV-p), isolate Boneface, did not result in any observable signs of disease. SUDV-p is a stock preparation of the wild-type, clinical SUDV isolate from the 1976 outbreak in Sudan and had already been previously passaged once in guinea pigs and twice on VeroE6 cells. Sequencing of SUDV-p showed that the progenitor virus (GenBank accession no. KT878488) had seven point mutations compared to wild-type SUDV (GenBank accession no. FJ968794.1). SUDV-GA was generated by 25 successive rounds of passage of SUDV-p within the livers and spleens of 6-to-8-week-old, strain Hartley female guinea pigs. During the serial passaging, the inoculated animal got progressively sicker, as evidenced by weight loss, and eventually succumbed to the infection by passage 25. SUDV-GA viral RNA was then extracted from the liver and spleen of this guinea pig and sent for full-genome sequencing using methods described in a past publication (16) with primers designed in house (see Table S1 in the supplemental material). It was shown that SUDV-GA possessed only 16 nucleotide changes from the genome of SUDV-p. Only six of these mutations resulted in an amino acid change in the virus (Table 1), with one in viral protein 35 (VP35) (N51D), one in VP40 (P309S), three in GP (A30T, Y151H, and F153L), and one in VP24 (P204L).
TABLE 1.
Summary of all mutations between SUDV-p and SUDV-GA
| Gene | Nucleotide position | Progenitora | GAb | Amino acid changec |
|---|---|---|---|---|
| NP | 34 | T | C | |
| NP | 850 | G | A | |
| NP | 2965 | T | C | |
| VP35 | 3288 | A | G | N-51-D |
| VP35 | 4348 | T | C | |
| VP40 | 4966 | T | C | |
| VP40 | 5378 | C | T | P-309-S |
| VP40 | 5767 | C | T | |
| GP | 6085 | G | A | A-30-T |
| GP | 6448 | T | C | Y-151-H |
| GP | 6454 | T | C | F-153-L |
| GP | 6471 | T | C | |
| VP30 | 9678 | A | G | |
| VP24 | 10909 | C | T | P-204-L |
| L | 12266 | T | C | |
| L | 15047 | C | T |
The progenitor SUDV (SUDV-p) viral sequence has been deposited to GenBank under accession number KT878488.
GA, guinea pig adapted. The viral sequence has been deposited in GenBank under accession number KT750754.
The amino acid changes are indicated as follows: old amino acid-residue number in protein-new amino acid.
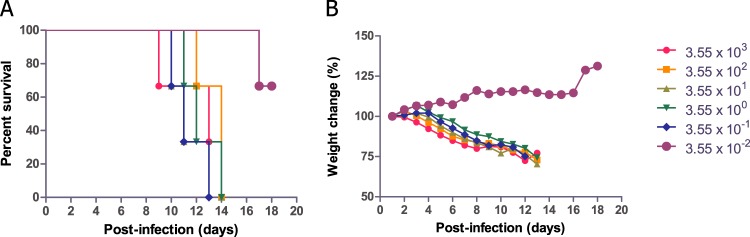
Calculation of the LD50 for SUDV-GA.
The median (50%) lethal dose (LD50) was then calculated with SUDV-GA. Guinea pigs were inoculated with 10-fold serial dilutions of SUDV-GA, ranging between 3.55 × 103 and 3.55 × 10−2 TCID50 of SUDV-GA per animal. Moribund guinea pigs started losing weight at 5 days postinfection (dpi), and in the infected groups with 100% mortality, the animals died between 9 and 14 dpi, with an average time to death of 12.1 ± 1.7 dpi (Fig. 1). The LD50 was calculated to be 5.3 × 10−2 TCID50.
FIG 1.
Determination of LD50 with SUDV-GA in guinea pigs. Animals were infected with 10-fold serial dilutions of SUDV-GA and monitored for survival (A) and weight loss (B) over the next 17 days.
Clinical findings in guinea pigs infected with SUDV-GA and SUDV-p.
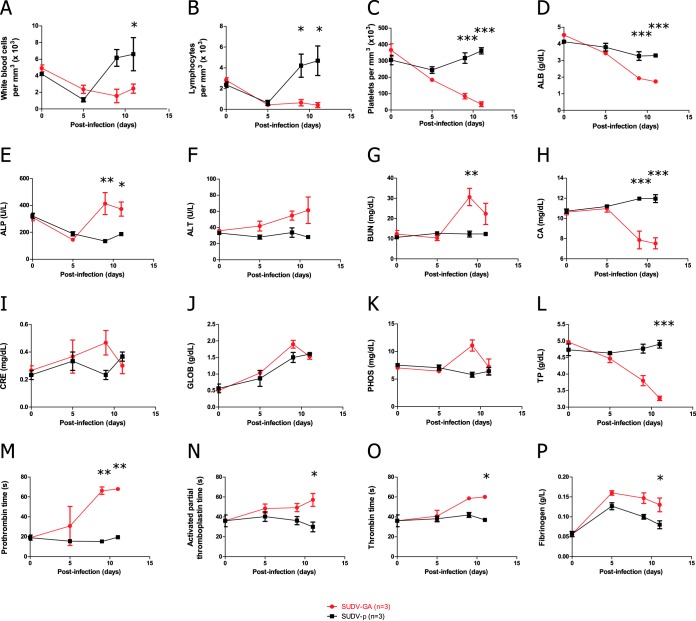
To investigate clinical parameters in guinea pigs after infection with SUDV-GA, groups of three animals were inoculated via the intraperitoneal (i.p.) route with SUDV-GA at a dose of 1,000× LD50 (53 TCID50) or an equal amount of SUDV-p as a control. Blood was collected at 0, 5, 9, and 11 dpi, and a complete blood count with differential was performed, in addition to quantification of serum biochemistry parameters, coagulation factors, and viremia. A transient decrease in the absolute counts of white blood cells (WBC) and lymphocytes (LYM) was observed in SUDV-p animals (Fig. 2A and B), after which the counts of WBC and LYM rose above the baseline by day 9 and stayed elevated through 11 dpi. In contrast, WBC and LYM counts were depressed by more than 67% throughout the course of infection in SUDV-GA animals (Fig. 2A and B). Animals given SUDV-GA had a decrease of over 90% in the number of platelets (PLT) during the infection, but this reduction was not observed with SUDV-p animals (Fig. 2C). Except for a steady increase in globulin (GLOB) concentrations after infection with SUDV-p, changes in the serum biochemistry parameters were not detected. However, substantial changes were observed with animals inoculated with SUDV-GA, specifically in the concentrations of albumin (ALB), alkaline phosphatase (ALP), alanine aminotransferase (ALT), blood urea nitrogen (BUN), calcium (CA), creatinine (CRE), GLOB, phosphate (PHOS), and total protein (TP) (Fig. 2D to L), and some changes in the parameters were statistically significant compared to the SUDV-p group data late after infection, at 9 and 11 dpi. The combination of these findings in SUDV-GA guinea pigs suggests abnormalities in multiple organs during advanced disease. Sustained increases in the coagulation parameters prothrombin time (PT), activated partial thromboplastin time (APTT), and thrombin time (TT) as well as in fibrinogen (FIB) concentrations were also observed for animals infected with SUDV-GA, whereas only a transient increase in FIB was detected in SUDV-p animals. The difference between the two groups was statistically significant at late time points (Fig. 2M to P). This suggests that SUDV-GA animals were exhibiting coagulation disorders during late stages of infection.
FIG 2.
Clinical parameters of guinea pigs infected with SUDV-GA or SUDV-p. Animals were infected with 1,000× LD50 of SUDV-GA (53 TCID50) or an equivalent dose of SUDV-p. Blood and serum samples were taken at 0, 5, 9, and 11 dpi. The following parameters are shown: (A) counts of white blood cells (WBC); (B) counts of lymphocytes; (C) counts of platelets (PLT); (D) concentrations of albumin (ALB); (E) concentrations of alkaline phosphatase (ALP); (F) concentrations of alanine aminotransferase (ALT); (G) concentrations of blood urea nitrogen (BUN); (H) concentrations of calcium (CA); (I) concentrations of creatinine (CRE); (J) concentrations of globulin (GLOB); (K) concentrations of phosphate (PHOS); and (L) concentrations of total protein (TP). Other parameters shown include prothrombin time (PT) (M), activated partial thromboplastin time (APTT) (N), thrombin time (TT) (O), and fibrinogen (FIB) concentration (P). The data are expressed as means ± standard errors. *, P < 0.05; **, P < 0.01; ***, P < 0.001 (statistical significance was determined by comparing the values in the SUDV-p and SUDV-MA groups at the same time points).
Virus titers in the blood, liver, and spleen of infected guinea pigs.
To investigate virological parameters after a SUDV-p or SUDV-GA infection, whole blood harvested from the animals was used to determine viremia at various time points by reverse transcription-quantitative PCR (RT-qPCR). To determine virus titers in the livers and spleens of infected animals, groups of three animals were inoculated with either SUDV-p or SUDV-GA and then euthanized at 0, 5, 9, and 11 dpi with the purpose of harvesting the organs for virology as well as pathology studies. Levels in guinea pigs infected with SUDV-p reached ∼104 genome equivalents (GEQ) per ml of blood (GEQ/ml) by 5 dpi but decreased by 9 dpi, and animals had cleared the infection from the blood by 11 dpi (Fig. 3A). In contrast, levels in SUDV-GA animals reached over ∼105 GEQ/ml by 5 dpi and rose to ∼106 GEQ/ml by 9 and 11 dpi (Fig. 3A). Evidence of enhanced replication by SUDV-GA compared to SUDV-p could be detected in the livers and spleens of guinea pigs. Animals inoculated with SUDV-p reached a peak of ∼105 GEQ/g of liver tissue, but those infected with SUDV-GA reached a peak of ∼106 GEQ/g of liver tissue (Fig. 3B). Along the same lines, SUDV-p guinea pigs reached over ∼105 GEQ/g of spleen tissue after infection, but SUDV-GA animals reached ∼106 GEQ/g of spleen tissue (Fig. 3C). The viral genome could still be detected at 11 dpi in the liver and spleen of SUDV-p animals despite clearance of the virus from the blood.
FIG 3.
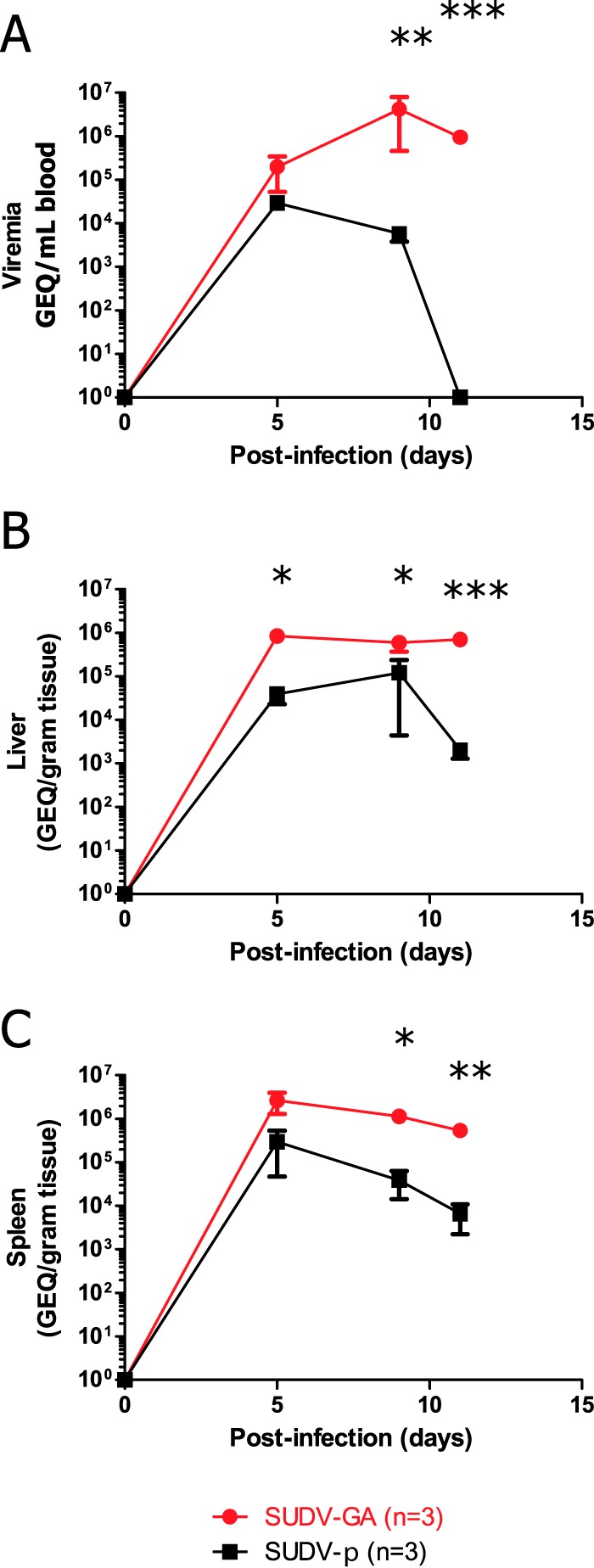
Virus titers in the blood, liver, or spleen of guinea pigs infected with SUDV-p or SUDV-GA. Whole blood and tissues were collected from animals (n = 3 per time point) infected with 1,000× LD50 of SUDV-GA (53 TCID50) or an equivalent dose of SUDV-p at 0, 5, 9, and 11 dpi. Viremia (A), as well as virus titers in the livers (B) and spleens (C), was determined by RT-qPCR. The data are expressed as means ± standard errors. *, P < 0.05; **, P < 0.01; ***, P < 0.001 (statistical significance was determined by comparing the values in the SUDV-p and SUDV-MA groups at the same time points).
Gross pathology, histopathology, and immunohistochemistry findings in the liver and spleen of guinea pigs infected with SUDV-GA.
Gross examination of the liver and spleen of guinea pigs infected with SUDV-GA revealed enlargement and discoloration of the liver which was apparent by 9 dpi (Fig. 4A). Enlarged spleens were also observed by 9 dpi, but discoloration of the organs was not readily apparent to the naked eye (Fig. 4B).
FIG 4.
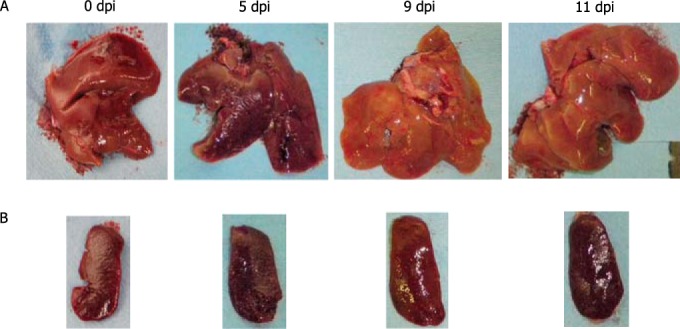
Gross pathology of organs from animals infected with SUDV-GA. Representative images of the livers (A) and spleens (B) of animals infected i.p. with 1,000× LD50 of SUDV-GA (53 TCID50) in animals euthanized at 0, 5, 9, and 11 dpi are shown.
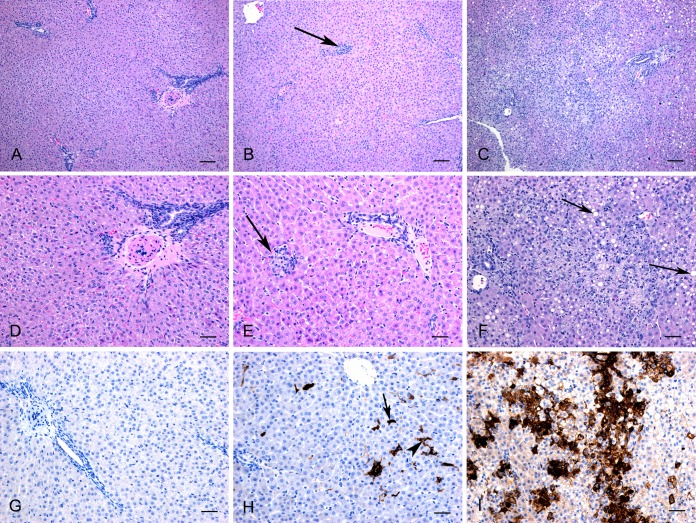
Histopathology and immunohistochemistry (IHC) findings in the livers of guinea pigs after infection with 1,000× LD50 of SUDV-GA are summarized in Fig. 5. At 5 dpi, lesions were mild, with a few small foci of inflammation and scattered degenerating hepatocytes. Moderate amounts of viral antigen could be detected throughout the section primarily within sinusoids and occasionally in individual hepatocytes or associated with the areas of inflammation. At 9 dpi, moderate-to-severe lesions were observed and were characterized by diffuse vacuolation of hepatocytes, with multifocal areas of necrotizing hepatitis and neutrophil infiltration. The distribution of immunostaining for viral antigen was similar to that observed at 5 dpi; however, there was more-abundant staining and, in addition, there was intense immunopositivity associated with areas of necrosis.
FIG 5.
Histopathology and immunohistochemistry (IHC) findings in the livers of guinea pigs infected with SUDV-GA. The top row represents hematoxylin and eosin staining (HE) at lower magnification (bar, 100 μm), the middle row represents HE staining at higher magnification (bar, 50 μm), and the bottom row represents IHC staining performed using a monoclonal antibody against SUDV (bar, 100 μm). No histopathological changes (A and D) or antigen (G) was detected by IHC at 0 dpi. Scattered small areas of inflammation (B and E; arrow) were observed at 5 dpi. Positive immunostaining (H) was detected in hepatocytes (arrow) and within sinusoids (arrowhead) at 5 dpi. Focally extensive necrotizing hepatitis with destruction of normal architecture (C and F) was seen at 9 dpi. Hepatocytes were diffusely vacuolated (F; arrows). Intense positive immunostaining were associated with areas of necrosis (I).
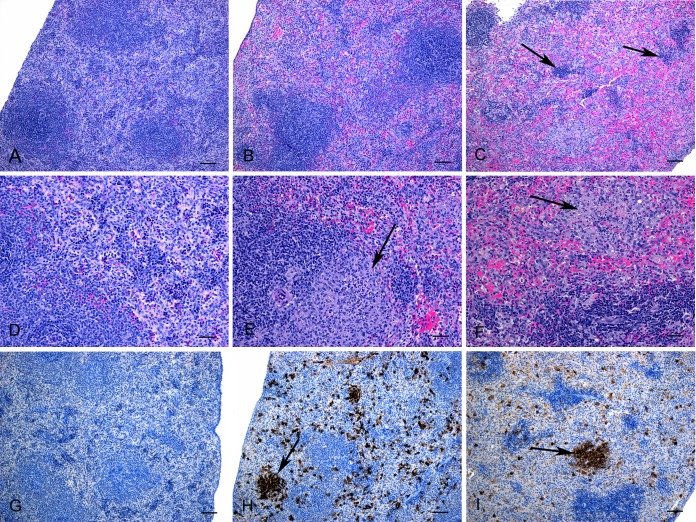
Histopathology and IHC findings in the spleens of animals infected with SUDV-GA are summarized in Fig. 6. At 5 dpi, there was an increase in neutrophil numbers throughout the red pulp, with scattered degenerating cells and formation of periarteriolar accumulations of macrophages (known as ellipsoids). There was widespread and intense immunostaining of viral antigen throughout the red pulp in cells which appeared by morphology to be macrophages. At 9 dpi, there was extensive neutrophil infiltration into red pulp, with numerous degenerating cells and an occasional larger area of necrosis. There was less viral antigen detected at this time point compared to 5 dpi, but the distributions were similar.
FIG 6.
Histopathology and immunohistochemistry (IHC) findings in the spleens of guinea pigs infected with SUDV-GA. The top row represents hematoxylin and eosin stain (HE) at lower magnification (bars, 100 μm), the middle row represents HE stain at higher magnification (bars, 50 μm), and the bottom row represents IHC staining performed using a monoclonal antibody against SUDV (bars, 100 μm). No histopathological changes (A and D) or antigen (G) was detected by IHC at 0 dpi. Scattered small areas of inflammation (B and E; arrow) were observed at 5 dpi. Increased numbers of neutrophils throughout the red pulp with disruption of splenic cords (B) and formation of ellipsoids (E; arrow) were observed at 5 dpi. Abundant positive immunostaining in cells throughout the red pulp (H) and intense staining associated with ellipsoids (arrow) were also seen. White pulp depletion (C; arrows) and areas of necrosis with neutrophil accumulation within the red pulp (F, arrow) were detected at 9 dpi. Intense positive immunostaining was associated with areas of necrosis (I; arrow).
DISCUSSION
The majority of preclinical development of medical countermeasures against SUDV infections had in the past been performed in NHPs. Although multiple vaccines have been tested, including VSV (17, 18), complex adenovirus (CAdVax) (19), Venezuelan equine encephalitis virus (VEEV) (20), and virus-like particles (VLPs) (21), candidate drugs have not yet been tested against SUDV infections in NHPs. One factor that can hinder these studies is the high cost of producing and testing compounds in large animals; it is simply not financially feasible to screen potential candidates in NHPs. For example, this is especially true of monoclonal antibodies (MAbs), such as those that comprise ZMapp, as production costs can reach up to $20,000/g of MAbs (22). In contrast, live attenuated vaccine candidates can be more easily scaled up to accommodate experimental needs in NHP studies. However, ethical considerations limit testing in NHPs to compounds that have already shown a strong potential for efficacy. Currently, these types of preliminary experiments are not possible for SUDV because a suitable small-animal model is unavailable.
The results of this study demonstrate, for the first time, the successful generation of an adapted SUDV variant that is uniformly lethal to guinea pigs. The Boneface isolate of SUDV is better characterized due to its use as the prototype SUDV in past vaccine studies involving NHPs (18–21); thus, the Boneface isolate was chosen over other SUDV isolates to establish the guinea pig-adapted variant. Animals challenged with SUDV-GA succumb to infection between 9 to 14 dpi, which is within a time frame similar to that seen with cynomolgus macaques given an intramuscular (i.m.) infection of 1,000 PFU of SUDV (between 7 and 12 dpi) (18–21). Hallmarks of SUDV infection of NHPs, including lymphopenia and thrombocytopenia, were also detected with SUDV-GA-inoculated guinea pigs and were accompanied by coagulation disorders in these animals, as evidenced by increased readings in PT, APTT, TT, and FIB values. Changes in the blood profile after infection, including elevations in liver enzyme activities such as ALP and ALT and accumulation of waste products such as BUN and CRE, were noted in both SUDV-infected NHPs (18) and the SUDV-GA guinea pigs. Therefore, this model closely mimics the characteristics of SUDV infection in NHPs and should be a useful precursor model for investigating the efficacy of candidate medical countermeasures against SUDV infections.
Similarly to filovirus infections, the liver and spleens were also major target organs in SUDV-p as well as SUDV-GA infections in guinea pigs. In the case of SUDV-p, virus replication was quickly controlled and viremia was undetectable by PCR by 11 dpi, whereas SUDV-GA was able to replicate at levels that were at least 10-fold higher, as detected from the blood, liver, and spleen of infected animals, eventually killing the host. Comparison of the viral genomes showed that one nonsilent mutation was detected in each of the viral protein 35 (VP35) and VP24 genes. Through studies with other filoviruses, both genes are known to play a role in evading host type I interferon responses (23, 24). Furthermore, mutations in the glycoprotein (GP) and VP40 genes may have resulted in a SUDV variant that is able to infect and replicate more efficiently in the guinea pig host. More studies will be necessary to address these issues.
Due to the EBOV outbreak in western Africa, the world has now seen the devastating impact that filoviruses can have if outbreaks are not handled properly at the outset. The scientific community must be proactive in devising strategies to prevent and treat filovirus infections, should a future outbreak occur. The guinea pig-based model for SUDV constitutes an important step toward this goal and will provide a solid basis for bridging in vitro results to NHP studies, greatly accelerating the development and characterization of novel medical countermeasures.
Supplementary Material
ACKNOWLEDGMENTS
This work was supported by the Public Health Agency of Canada (PHAC) and a grant from the Canadian Safety and Security Program (CSSP; grant number CP-1017) awarded to G.P.K. and X.Q. G.W. is the recipient of a Banting Postdoctoral Fellowship from the Canadian Institutes of Health Research (CIHR) and the President's International Fellowship Initiative from the Chinese Academy of Sciences (CAS).
We declare that we have no conflicts of interests.
Footnotes
Supplemental material for this article may be found at http://dx.doi.org/10.1128/JVI.02331-15.
REFERENCES
- 1.WHO. 1978. Ebola haemorrhagic fever in Zaire, 1976. Report of an international commission. Bull World Health Organ 56:271–293. [PMC free article] [PubMed] [Google Scholar]
- 2.WHO. 1978. Ebola haemorrhagic fever in Sudan, 1976. Report of a WHO/international study team. Bull World Health Organ 56:247–270. [PMC free article] [PubMed] [Google Scholar]
- 3.WHO International 2015, posting date. Ebola situation report 30 September 2015. World Health Organization, Geneva, Switzerland: http://apps.who.int/ebola/current-situation/ebola-situation-report-30-september-2015. [Google Scholar]
- 4.Jones SM, Feldmann H, Stroher U, Geisbert JB, Fernando L, Grolla A, Klenk HD, Sullivan NJ, Volchkov VE, Fritz EA, Daddario KM, Hensley LE, Jahrling PB, Geisbert TW. 2005. Live attenuated recombinant vaccine protects nonhuman primates against Ebola and Marburg viruses. Nat Med 11:786–790. doi: 10.1038/nm1258. [DOI] [PubMed] [Google Scholar]
- 5.Stanley DA, Honko AN, Asiedu C, Trefry JC, Lau-Kilby AW, Johnson JC, Hensley L, Ammendola V, Abbate A, Grazioli F, Foulds KE, Cheng C, Wang L, Donaldson MM, Colloca S, Folgori A, Roederer M, Nabel GJ, Mascola J, Nicosia A, Cortese R, Koup RA, Sullivan NJ. 2014. Chimpanzee adenovirus vaccine generates acute and durable protective immunity against ebolavirus challenge. Nat Med 20:1126–1129. [DOI] [PubMed] [Google Scholar]
- 6.Oestereich L, Ludtke A, Wurr S, Rieger T, Munoz-Fontela C, Gunther S. 2014. Successful treatment of advanced Ebola virus infection with T-705 (favipiravir) in a small animal model. Antiviral Res 105:17–21. doi: 10.1016/j.antiviral.2014.02.014. [DOI] [PubMed] [Google Scholar]
- 7.Qiu X, Wong G, Audet J, Bello A, Fernando L, Alimonti JB, Fausther-Bovendo H, Wei H, Aviles J, Hiatt E, Johnson A, Morton J, Swope K, Bohorov O, Bohorova N, Goodman C, Kim D, Pauly MH, Velasco J, Pettitt J, Olinger GG, Whaley K, Xu B, Strong JE, Zeitlin L, Kobinger GP. 2014. Reversion of advanced Ebola virus disease in nonhuman primates with ZMapp. Nature 514:47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bray M, Davis K, Geisbert T, Schmaljohn C, Huggins J. 1999. A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. J Infect Dis 179(Suppl 1):S248–S258. doi: 10.1086/514292. [DOI] [PubMed] [Google Scholar]
- 9.Connolly BM, Steele KE, Davis KJ, Geisbert TW, Kell WM, Jaax NK, Jahrling PB. 1999. Pathogenesis of experimental Ebola virus infection in guinea pigs. J Infect Dis 179(Suppl 1):S203–S217. doi: 10.1086/514305. [DOI] [PubMed] [Google Scholar]
- 10.Kuhn JH, Becker S, Ebihara H, Geisbert TW, Johnson KM, Kawaoka Y, Lipkin WI, Negredo AI, Netesov SV, Nichol ST, Palacios G, Peters CJ, Tenorio A, Volchkov VE, Jahrling PB. 2010. Proposal for a revised taxonomy of the family Filoviridae: classification, names of taxa and viruses, and virus abbreviations. Arch Virol 155:2083–2103. doi: 10.1007/s00705-010-0814-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.CDC. 20 October 2015, posting date. Outbreaks chronology: Ebola virus disease. Centers for Disease Control and Prevention, Atlanta, GA: http://www.cdc.gov/vhf/ebola/outbreaks/history/chronology.html. [Google Scholar]
- 12.Chen G, Koellhoffer JF, Zak SE, Frei JC, Liu N, Long H, Ye W, Nagar K, Pan G, Chandran K, Dye JM, Sidhu SS, Lai JR. 2014. Synthetic antibodies with a human framework that protect mice from lethal Sudan ebolavirus challenge. ACS Chem Biol 9:2263–2273. doi: 10.1021/cb5006454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mire CE, Geisbert JB, Versteeg KM, Mamaeva N, Agans KN, Geisbert TW, Connor JH. 2015. A single-vector, single-injection trivalent filovirus vaccine: proof of concept study in outbred guinea pigs. J Infect Dis 212(Suppl 2):S384–S38. doi: 10.1093/infdis/jiv126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kuhn JH, Andersen KG, Bao Y, Bavari S, Becker S, Bennett RS, Bergman NH, Blinkova O, Bradfute S, Brister JR, Bukreyev A, Chandran K, Chepurnov AA, Davey RA, Dietzgen RG, Doggett NA, Dolnik O, Dye JM, Enterlein S, Fenimore PW, Formenty P, Freiberg AN, Garry RF, Garza NL, Gire SK, Gonzalez JP, Griffiths A, Happi CT, Hensley LE, Herbert AS, Hevey MC, Hoenen T, Honko AN, Ignatyev GM, Jahrling PB, Johnson JC, Johnson KM, Kindrachuk J, Klenk HD, Kobinger G, Kochel TJ, Lackemeyer MG, Lackner DF, Leroy EM, Lever MS, Muhlberger E, Netesov SV, Olinger GG, Omilabu SA, Palacios G, et al. 2014. Filovirus RefSeq entries: evaluation and selection of filovirus type variants, type sequences, and names. Viruses 6:3663–3682. doi: 10.3390/v6093663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kuhn JH, Bao Y, Bavari S, Becker S, Bradfute S, Brister JR, Bukreyev AA, Cai Y, Chandran K, Davey RA, Dolnik O, Dye JM, Enterlein S, Gonzalez JP, Formenty P, Freiberg AN, Hensley LE, Honko AN, Ignatyev GM, Jahrling PB, Johnson KM, Klenk HD, Kobinger G, Lackemeyer MG, Leroy EM, Lever MS, Lofts LL, Muhlberger E, Netesov SV, Olinger GG, Palacios G, Patterson JL, Paweska JT, Pitt L, Radoshitzky SR, Ryabchikova EI, Saphire EO, Shestopalov AM, Smither SJ, Sullivan NJ, Swanepoel R, Takada A, Towner JS, van der Groen G, Volchkov VE, Wahl-Jensen V, Warren TK, Warfield KL, Weidmann M, Nichol ST. 2013. Virus nomenclature below the species level: a standardized nomenclature for laboratory animal-adapted strains and variants of viruses assigned to the family Filoviridae. Arch Virol 158:1425–1432. doi: 10.1007/s00705-012-1594-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Qiu X, Wong G, Audet J, Cutts T, Niu Y, Booth S, Kobinger GP. 2014. Establishment and characterization of a lethal mouse model for the Angola strain of Marburg virus. J Virol 88:12703–12714. doi: 10.1128/JVI.01643-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Geisbert TW, Daddario-DiCaprio KM, Williams KJ, Geisbert JB, Leung A, Feldmann F, Hensley LE, Feldmann H, Jones SM. 2008. Recombinant vesicular stomatitis virus vector mediates postexposure protection against Sudan Ebola hemorrhagic fever in nonhuman primates. J Virol 82:5664–5668. doi: 10.1128/JVI.00456-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Geisbert TW, Geisbert JB, Leung A, Daddario-DiCaprio KM, Hensley LE, Grolla A, Feldmann H. 2009. Single-injection vaccine protects nonhuman primates against infection with Marburg virus and three species of Ebola virus. J Virol 83:7296–7304. doi: 10.1128/JVI.00561-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pratt WD, Wang D, Nichols DK, Luo M, Woraratanadharm J, Dye JM, Holman DH, Dong JY. 2010. Protection of nonhuman primates against two species of Ebola virus infection with a single complex adenovirus vector. Clin Vaccine Immunol 17:572–581. doi: 10.1128/CVI.00467-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Herbert AS, Kuehne AI, Barth JF, Ortiz RA, Nichols DK, Zak SE, Stonier SW, Muhammad MA, Bakken RR, Prugar LI, Olinger GG, Groebner JL, Lee JS, Pratt WD, Custer M, Kamrud KI, Smith JF, Hart MK, Dye JM. 2013. Venezuelan equine encephalitis virus replicon particle vaccine protects nonhuman primates from intramuscular and aerosol challenge with ebolavirus. J Virol 87:4952–4964. doi: 10.1128/JVI.03361-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Warfield KL, Dye JM, Wells JB, Unfer RC, Holtsberg FW, Shulenin S, Vu H, Swenson DL, Bavari S, Aman MJ. 2015. Homologous and heterologous protection of nonhuman primates by Ebola and Sudan virus-like particles. PLoS One 10:e0118881. doi: 10.1371/journal.pone.0118881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kelley B. 2009. Industrialization of mAb production technology: the bioprocessing industry at a crossroads. MAbs 1:443–452. doi: 10.4161/mabs.1.5.9448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bale S, Julien JP, Bornholdt ZA, Kimberlin CR, Halfmann P, Zandonatti MA, Kunert J, Kroon GJ, Kawaoka Y, MacRae IJ, Wilson IA, Saphire EO. 2012. Marburg virus VP35 can both fully coat the backbone and cap the ends of dsRNA for interferon antagonism. PLoS Pathog 8:e1002916. doi: 10.1371/journal.ppat.1002916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Valmas C, Basler CF. 2011. Marburg virus VP40 antagonizes interferon signaling in a species-specific manner. J Virol 85:4309–4317. doi: 10.1128/JVI.02575-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.