Summary
Background
Leprosy is the most common form of treatable peripheral neuropathy. However, in spite of effective chemotherapeutic agents, neuropathy and associated deformities are seldom ameliorated to a significant extent. This necessitates early diagnosis and treatment. Clinical examination of peripheral nerves is highly subjective and inaccurate. Electrophysiological studies are painful and expensive. Ultrasonography circumvents these demerits and has emerged as the preferred modality for probing peripheral nerves.
Case Report
We describe a 23-year-old male who presented with weakness and clawing of the medial digits of the right hand (main-en-griffe) and a few skin lesions since eighteen months. The right ulnar nerve was thickened and exquisitely tender on palpation. Ultrasonography revealed an extensive enlargement of the nerve with presence of intraneural color Doppler signals suggestive of acute neuritis. Skin biopsy was consistent with borderline tuberculoid leprosy with type 1 lepra reaction. The patient was started on WHO multidrug therapy for paucibacillary leprosy along with antiinflammatory drugs. Persistence of vascular signals at two months’ follow-up has led to continuation of the steroid therapy. The patient is compliant with the treatment and is on monthly follow-up.
Conclusions
In this manuscript, we review multitudinous roles of ultrasonography in examination of peripheral nerves in leprosy. Ultrasonography besides diagnosing enlargement of nerves in leprosy and acute neuritis due to lepra reactions, guides the duration of anti-inflammatory therapy in lepra reactions. Further, it is relatively inexpensive, non-invasive and easily available. All these features make ultrasonography a preferred modality for examination of peripheral nerves.
MeSH Keywords: Leprosy, Ulnar Neuropathies, Ultrasonography
Background
Leprosy is caused by Mycobacterium leprae which has a propensity to affect cooler regions of the body like skin, peripheral nerves, testes, anterior chamber of the eye and nasal cavity [1,2]. The hallmarks of leprosy are hypo-pigmented, hypo-aesthetic skin lesions with thickening of the peripheral nerves [1,2].
On ultrasonography, a normal nerve has hypoechoic fascicles with intervening echogenic peri-epineurium with no color Doppler signals. This appearance of nerves has been called ‘honeycomb’ or ‘bundle of straws’ on transverse and longitudinal scans, respectively [1–3]. Leprosy-afflicted nerves tend to lose these normal characteristics [1–3]. In this article we describe the appearances of the leprosy-affected nerves as well as importance of ultrasonography regarding the same.
Case Report
A 23-year-old male presented with gradual-onset weakness and clawing of medial two digits (Figures 1, 2) of the right hand since eighteen months. Besides, he had a few skin lesions over the right forearm for the same duration. There was, however, no trauma to the arm or forearm nor any history of allergy, drug reaction or insect bite.
Figure 1.

Photograph of the right hand depicts flattening of hypothenar eminence with ulnar claw hand (main-en-griffe).
Figure 2.

Photograph shows extension at metacarpophalangeal joints and flexion at proximal and distal interphalangeal joints of the fourth and fifth digit.
The general examination was normal. On local examination, the skin lesions were found to be hypopigmented macules as well as plaques that had erythematous borders. The lesions were dry, anhidrotic and hypesthetic. On palpation behind the medial epicondyle, the right ulnar nerve was thickened, cord-like and exquisitely tender. The patient also experienced tingling along the course of the nerve during palpation. The contralateral nerve was, however, normal. There was diminution of sensation along the medial aspect of the ipsilateral hand and medial one and a half fingers with wasting of the hypothenar muscles. There was reduction in power of medial two lumbricals and the interossei.
Ultrasonography of the right ulnar nerve was performed. It showed normal morphology of the nerve in the proximal arm (Figure 3) with an extensive fusiform enlargement of the nerve from mid-arm till the cubital tunnel (Figure 4). In the mid-arm, there was preservation of the fascicular architecture with thickening of individual fascicles (Figure 5). The fascicular morphology was, however, lost in the lower arm (Figures 6–8). The maximal thickening was proximal to the cubital tunnel (Figures 4, 7, 8). On Doppler interrogation, there was presence of low-resistance flow within the thickened nerve suggestive of acute neuritis (Figure 7). The nerve morphology was normal again in the forearm (Figures 9, 10). The contralateral nerve was also normal. Based on clinical and radiological findings, a provisional diagnosis of leprosy with lepra reaction was considered and the patient was promptly started on anti-inflammatory medication.
Figure 3.
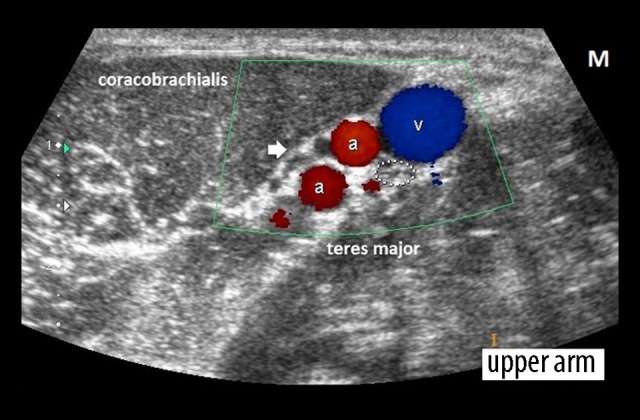
Transverse scan at the upper arm (just distal to the axilla) shows normal appearance of the right ulnar nerve (dotted ellipse; Cross-sectional area=5 mm2). The nerve comprises of multiple hypoechoic dot-like nerve fascicles (honeycomb appearance on a transverse scan). The arrow points to nerve fascicles of the median nerve that are not oriented transversely on the present scan. [a=high bifurcation of the brachial artery, v=basilic vein, M=medial aspect].
Figure 4.

Panoramic view of the right ulnar nerve from the arm to the upper forearm through the cubital tunnel (d) demonstrates normal segments of the nerve (a, f), transition zones (b, e), region of fusiform thickening (c, d). The nerve is maximally thickened (c) proximal to the segment within the cubital tunnel (d).
Figure 5.
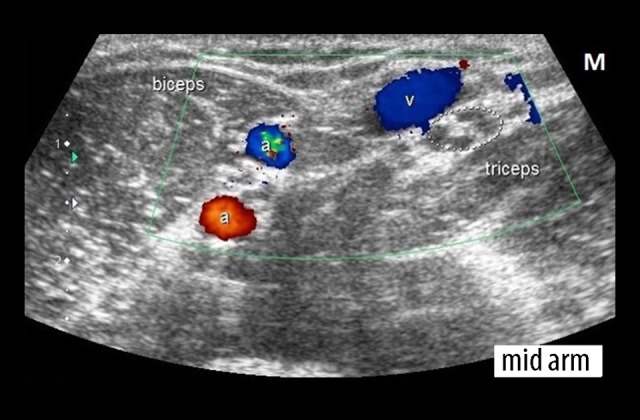
Transverse ultrasonogram reveals thickening (cross-sectional area=16.8 mm2) of each of the nerve fascicles of the right ulnar nerve (dotted ellipse). However, individual fascicle can be seen distinctly.
Figure 6.
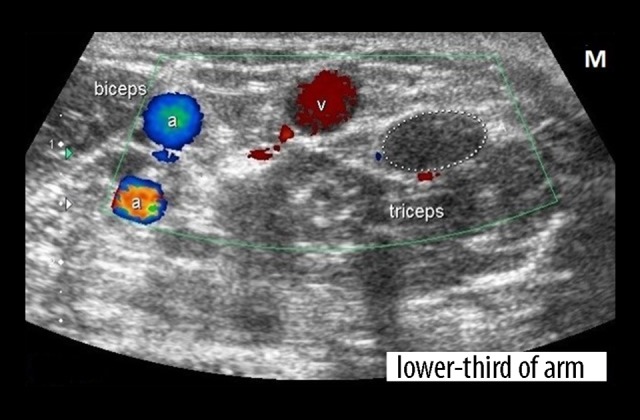
At lower-thirds of the arm, the thickened right ulnar nerve shows loss of internal architecture (dotted ellipse). It measures 33.6 mm2 in cross-section. The enlarged nerve indents the margin of the triceps.
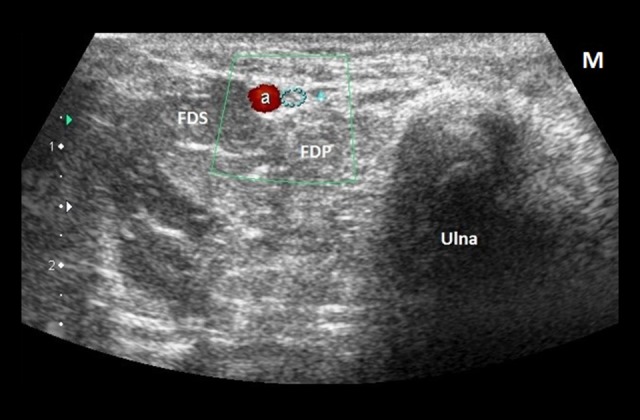
Figure 7.
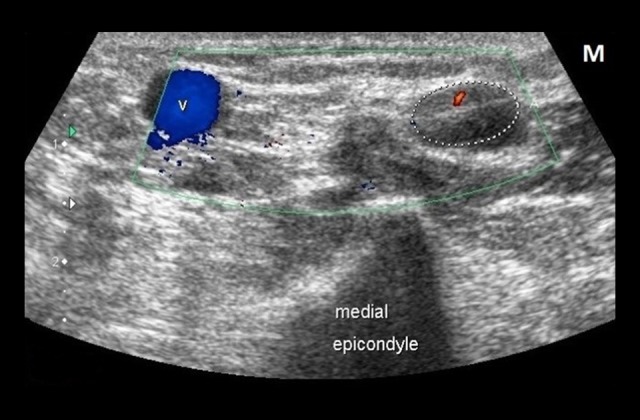
Axial scan just proximal to the medial epicondyle shows presence of Doppler signals within the substance of the thickened nerve. The spectral waveform was suggestive of low-resistance flow (not shown). The nerve measures 37.9 mm2 in cross-section.
Figure 8.
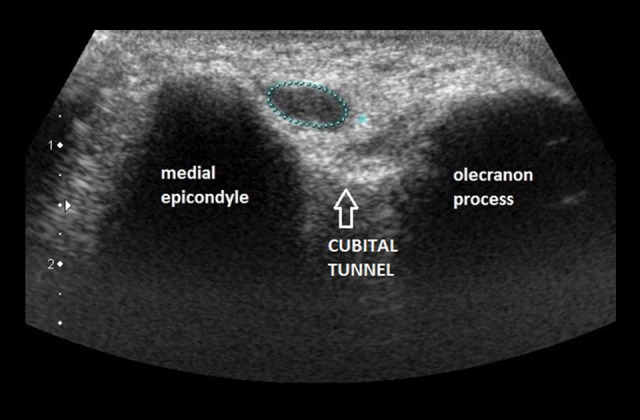
Ultrasonogram performed with the transducer positioned posteromedially on the medial epicondyle and olecranon process with the elbow in mid-flexion demonstrates thickened ulnar nerve (cross-sectional area=18.2 mm2) in the cubital tunnel.
Figure 9.
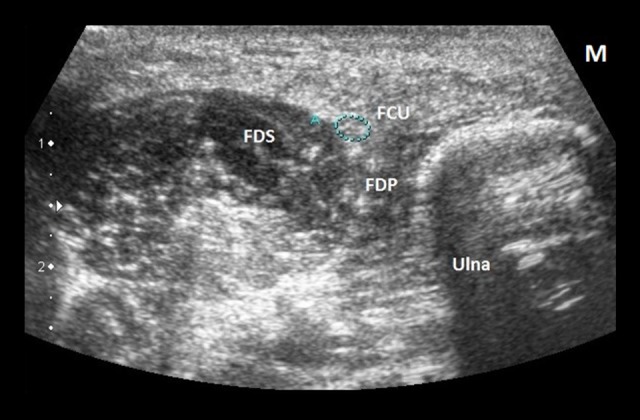
Axial view at upper forearm reveals normal fascicular morphology of the right ulnar nerve (cross-sectional area=4.2 mm2). In the figure, the nerve rests on flexor digitorum profundus (FDP). Flexor digitorum superficialis (FDS) lies laterally and flexor carpi ulnaris (FCU) is medial to the nerve.
Figure 10.
At mid-forearm, the ulnar nerve retains its normal sieve-like morphology on a transverse scan (cross-sectional area= 2.2 mm2). The nerve is accompanied by the ulnar artery.
Histopathology was simultaneously performed from the growing edge of the skin lesion which was consistent with borderline tuberculoid leprosy with type 1 reaction. The patient was started on WHO paucibacillary multidrug therapy. After 2 months of therapy, there was mild improvement in extension of the fourth and fifth digit with partial resolution of the cutaneous lesions. However, there was persistence of Doppler signals within the substance of the nerve and the patient was advised to continue steroids. He is currently on monthly follow-up.
Discussion
Peripheral nerve involvement is a common occurrence in leprosy with a predilection for ulnar nerve [1,2]. The disease is most commonly seen in the second or third decade with a male predominance [4]. Once in human body (via inhalation, contact with moist-infected soil or insect vectors) [4], the bacillus invades the peri-neural macrophages and schwann cells [5]. It may, however, take an average of 3–5 years or sometimes as long as twenty years for the symptoms to manifest [4,5]. The deformities that ensue following neuropathy include claw hand, wrist or foot drop, exposure keratitis due to lagophthalmos, trophic ulcers and auto-amputation of digits [4,5].
Assessment of thickening of peripheral nerves clinically bears significant inter-observer variation [2]. Further, it may be difficult to palpate all the peripheral nerves [2]. Moreover, clinically diagnosed neuropathy occurs quite late in the pathogenesis when substantial damage has already occurred [2]. Nerve conduction studies are highly sensitive but are not widely available [2]. Also, the pain while the test is being performed as well as the expensive nature of this modality makes it a lesser preferred one. Ultrasonography overcomes all of the above mentioned limitations of both clinical as well as electrophysiological examination. Besides, electrophysiological studies have been reported to be normal in early stages of the disease when USG may depict neural involvement [1]! USG thus emerges as an objective tool to assess the peripheral nerves [2]. MRI is an alternative imaging modality for peripheral nerves. However, longer acquisition time, cost and general contraindications to the modality make it a less preferred one [2].
Neural involvement in leprosy may appear as enlargement of the nerves which may be due to thickened but distinct individual nerve fascicles or there may be total loss of internal morphology [1–3]. The enlargement may be fusiform and typically proximal to entrapment sites [2]. Besides, there may be focal hypoechoic or echogenic foci within the nerve or an abscess may form. The nerve thickening, however, is not specific for leprosy and may be seen in diabetes, amyloidosis and hereditary neuropathies as well [6]. The hallmark of leprosy is extensive enlargement along a long segment of the nerve [2,6]. Besides, a relative absence of symptoms with an enlarged nerve on USG is also highly suggestive of leprosy.
Color Doppler is an extremely useful tool to assess acute neuritis (a feature of lepra reaction) [2]. This acute neural inflammation may precede or follow the onset of anti-leprotic treatment. Presence of intraneural vascularity signifies acute neuritis (lepra reaction). This increase in Doppler signals is not observed in nerves affected by leprosy alone and thus helps in differentiating leprotic involvement of nerves from acute neuritis due to lepra reactions [2]. It thus follows that regular USG can help guide the duration of anti-inflammatory medication [2]. Besides, an increase in vascularity may be seen in nerves with preserved fascicular morphology which has been known to occur in early stages of involvement [2]. Hence, institution of chemotherapy at this stage may prevent ulcers and deformities.
Finally, we believe that USG may obviate the need for nerve biopsy in the appropriate clinical scenario. Moreover, pure-neuritic type of leprosy with no skin manifestations may also be diagnosed using USG [6].
Conclusions
Ultrasonography has a key role in examination of peripheral nerves in leprosy. The Doppler signals give valuable information about the presence of acute neuritis and hence guides the duration of steroid intake. Finally, ease of availability, lesser cost of examination and non-invasive nature make ultrasonography a preferred modality for probing peripheral nerves.
References
- 1.Elias J, Nogueira-Barbosa MH, Feltrin LT, et al. Role of ulnar nerve sonography in leprosy neuropathy with electrophysiologic correlation. J Ultrasound Med. 2009;28:1201–9. doi: 10.7863/jum.2009.28.9.1201. [DOI] [PubMed] [Google Scholar]
- 2.Jain S, Visser LH, Praveen TLN, et al. High-resolution sonography: A new technique to detect nerve damage in leprosy. PLoS Negl Trop Dis. 2009;3(8):e498. doi: 10.1371/journal.pntd.0000498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lawande AD, Warrier SS, Joshi MS. Role of ultrasound in evaluation of peripheral nerves. Indian J Radiol Imaging. 2014;24(3):254–58. doi: 10.4103/0971-3026.137037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park K. Leprosy. In: Park K, editor. Park’s textbook of Preventive and social medicine. 23rd ed. M/s Banarsidas Bhanot; India: 2015. pp. 314–29. [Google Scholar]
- 5.Gelber RH. Leprosy (Hansen’s disease) In: Fauci AS, Braunwald E, Kasper DL, et al., editors. Harrison’s principles of internal medicine. 17th ed. Vol. 1. McGraw-hill companies; USA: 2008. pp. 1021–26. [Google Scholar]
- 6.Jain S, Visser LH, Yerasu MR, et al. Use of high resolution ultrasonography as an additional tool in the diagnosis of primary neuritic leprosy: a case report. Lepr Rev. 2013;84:161–65. [PubMed] [Google Scholar]


