Abstract
Since the 1988 resolution of the World Health Assembly to eradicate polio, significant progress has been made toward achieving this goal, with the result that only Afghanistan, Nigeria, and Pakistan have never successfully interrupted endemic transmission of wild poliovirus. However, one of the greatest challenges of the Global Polio Eradication Initiative has been that of maintaining the polio-free status of countries in unstable regions with weak healthcare infrastructure, a challenge exemplified by Somalia, a country in the Horn of Africa region. Somalia interrupted indigenous transmission of wild poliovirus in 2002, four years after establishing its national polio eradication programme. But political instability and protracted armed conflict, with significant disruption of the healthcare system, left the country vulnerable to two subsequent imported outbreaks of wild poliovirus. The first occurred during 2005–2007, resulting in over 200 cases of paralytic polio, while the second importation in 2013 is currently ongoing. Despite immense challenges, the country has a sensitive surveillance system that has facilitated prompt detection of outbreaks, but its weak routine immunization system means that supplementary immunization activities constitute the primary strategy for reaching children with polio vaccines. Conducting vaccination campaigns in a setting of conflict has been at times hazardous but the country’s polio programme has demonstrated resilience in overcoming many obstacles to ensure that children receive life-saving polio vaccines. Regaining and maintaining Somalia’s polio-free status will, however, depend on finding innovative and lasting solutions to the challenge of administering vaccines in a setting of ongoing conflict and instability.
Keywords: Polio, Somalia, Disease Eradication, Wild Poliovirus (WPV), Acute Flaccid Paralysis (AFP), Oral Polio Vaccine (OPV), Immunization, Surveillance
Introduction
Somalia, a country located in the Horn of Africa, is an exemplar of some of the successes and enduring challenges of the Global Polio Eradication Initiative. A decade after the World Health Assembly resolved to eradicate polio (1, 2), the country established its own polio eradication programme in 1998. Four years later, in 2002, Somalia successfully interrupted indigenous transmission of wild poliovirus (WPV) (3), a remarkable accomplishment considering that the country has been embroiled in war and armed conflict since 1991 (4, 5). This success has been punctuated by two importations and subsequent outbreaks of wild poliovirus. The first occurred during 2005 – 2007, resulting in 228 cases of paralytic polio, but was successfully interrupted (6). The second is currently ongoing, having first been reported on May 9, 2013, when stool specimens from a 32-month-old girl with acute flaccid paralysis (AFP) from Banadir region tested positive for wild poliovirus (7).
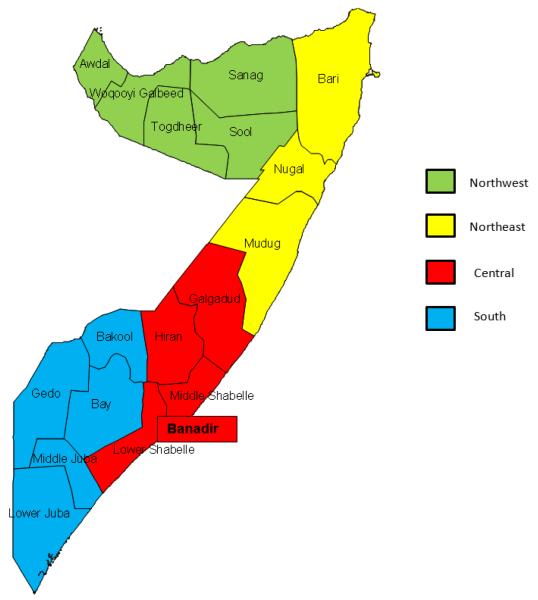
Since the fall of the central government in 1991, the prevailing situation in Somalia has been characterized by continuing strife, armed conflict, and political instability (5). Lacking a central government, the country administers services through three relatively autonomous areas derived from its four geo-political zones i.e., South, Central, Northeast, and Northwest, which are further subdivided into 19 regions and over a hundred districts (Figure 1). The South and Central zones are administered by the Federal Government of Somalia; the Northwest zone constitutes the self-declared state of Somaliland; and the Northeast is administered as the semi-autonomous region of Puntland (8, 9). While the Northwest and Northeast zones of the country are relatively stable with intermittent areas of conflict, the South and Central zones remain under a fragile security situation, with several territories controlled by armed militia and factions opposed to the government (5). The impact of the unstable political situation is a severely weakened healthcare system, unable to meet the needs of a vulnerable population. This is the context in which the country’s polio eradication programme has had to carry out its activities, often under immense constraints and sometimes with danger to the lives of its polio workers (10). Guided by the four key strategies for polio eradication, i.e., surveillance, supplementary immunization, routine immunization and mop-up activities (2, 11), the country’s programme has demonstrated resilience in its commitment to the goal of polio eradication.
Figure 1.
Map of Somalia Showing Geopolitical (Administrative) Zones and Regions
This paper describes the progress made by Somalia’s polio eradication programme over the past 15 years, highlighting pertinent challenges and obstacles that have been confronted during this period. We provide details of AFP surveillance and supplementary immunization activities (SIAs), as well as the constraints of administering routine immunization through the country’s weakened healthcare infrastructure. We describe how obstacles have been surmounted, intercurrent challenges, and strategies that have been devised to overcome them.
Methods
This country progress report was developed based on review and analysis of existing data and documents provided by the WHO Somalia Country Office.
Acute Flaccid Paralysis (AFP) Surveillance
We reviewed and analyzed AFP surveillance records from January 1998 through October 2013. Our analysis of AFP cases reported during this period focused on the following areas: the non-polio AFP rate; adequacy of stool specimen collection for case investigation; WPV incidence, including outbreaks occurring during this time period; and circulating vaccine-derived poliovirus (cVDPV) incidence. AFP cases were analyzed for key demographic characteristics, such as age, sex, geographic location, as well as their immunity profile, i.e., number of oral polio vaccine (OPV) doses received, as documented based on parental recall. AFP cases that were neither WPV nor cVDPV were characterized as: 1.) compatible, if they lacked adequate stool specimens but had residual paralysis or a pattern of clinical presentation consistent with polio after 60 days of onset; 2.) discarded, if they had adequate stool specimens but tested negative for poliovirus or lacked adequate stool specimens and did not have residual paralysis or a pattern of clinical presentation consistent with polio after 60 days of onset. Surveillance indicators were compared with standards stipulated by WHO guidelines, e.g., ≥2 non-polio AFP cases reported per 100,000 persons <15 years per year as an indicator of sensitive surveillance. Non-polio AFP rates were calculated based on discarded AFP cases and using denominators derived from UNDP estimates of the target population (children <15 years). We also calculated the proportion of AFP cases with adequate stool specimens, i.e., two specimens collected at least 24 hours apart within 14 days of the onset of paralysis and arriving at the laboratory in good condition, and the non-polio enterovirus isolation rate, to determine the quality of surveillance. AFP case status results were reported based on testing by the Regional Reference Laboratory in Nairobi, Kenya and the final determination for compatible and discarded cases was made by the National Polio Expert Committee.
Supplementary Immunization Activities (SIAs)
Using vaccination campaign records provided by the WHO Somalia Country Office, we assessed the quality of SIAs conducted in Somalia during 1998 through 2012. Since the South and Central zones are typically treated as one administrative block, planning and implementation of SIAs was done by dividing the country into three SIA zones: South Central, Northwest and Northeast. Hence, for each year, we summarized the number of SIAs carried out by zone and the number of districts reached during campaigns. We estimated the coverage levels achieved in areas where campaigns were conducted based on administrative data. For years in which data were collected on vaccine refusals (2006–2012), we estimated the proportion of children who could not be vaccinated on account of refusals. We also identified areas where SIAs could not be conducted (i.e., inaccessible areas) during the period under review.
Routine Immunization
Estimates of routine immunization coverage against polio in Somalia during 1998 through 2012 were obtained from WHO and UNICEF official documents providing details of OPV3 coverage (12, 13). These estimates were derived from coverage surveys and administrative data and compared with those reported by the government. Starting in 2009, the government has supplemented routine immunization coverage estimates with figures derived from Child Health Days (CHDs) (13), a special intervention geared toward reaching children under five years with basic health services, including essential vaccines (9, 14).
Special Strategies
In addition to available AFP and SIA data, we reviewed field reports and other documents provided by the WHO Somalia Country Office in order to ascertain details of special strategies employed in carrying out polio eradication activities. We sought details on the choice of vaccines used during campaigns, the target age groups, methods of community engagement and social mobilization, and strategies for reaching children in hard-to-reach and inaccessible areas.
Data were analyzed using SAS 9.3 (SAS Institute Inc., Cary, NC, USA) and Microsoft Excel 2010 (Microsoft Excel. Redmond, Washington: Microsoft, 2010). Owing to the long duration of the period under review, we reported statistical averages, with accompanying ranges where applicable, in lieu of actual estimates, for ease of presentation and interpretation of results.
Results
Country Demographics and Polio Staffing
Somalia has an estimated population of 10.5 million persons (15); approximately 2 million of these are children under five years of age. The South and Central zones are the most densely populated areas of the country, accounting for approximately two-thirds of the total population. Of the 19 regions, Banadir is the most densely populated and is home to the capital city of Mogadishu.
The polio eradication programme, led by the government and supported by WHO and UNICEF, is organized in such a way that there are two national and four zonal level coordinators, one for each zone. Each region has a polio eradication officer who coordinates activities at that level and directly supervises the district polio officers, who oversee the day-to-day running of polio eradication activities at the district level. Additionally, several temporary polio workers, including vaccinators, social mobilizers, and logistical staff, are hired during the course of vaccination campaigns.
Surveillance
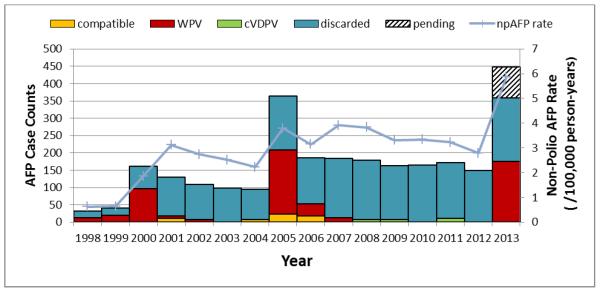
AFP Surveillance (Figure 2)
Figure 2.
Epidemic Curve of AFP Cases in Somalia with Line Graph of Non-Polio AFP Rate during 1998–2013
Abbreviations and AFP Case Definitions
AFP: Acute flaccid paralysis
WPV: Wild poliovirus
cVDPV: Circulating vaccine-derived poliovirus
npAFP: Non-polio AFP
Compatible: AFP cases lacking adequate stool specimens but having residual paralysis or a pattern of clinical presentation consistent with polio after 60 days of onset
Discarded: AFP cases with adequate stool specimens but testing negative for poliovirus, or lacking adequate stool specimens and not having residual paralysis or a pattern of clinical presentation consistent with polio after 60 days of onset
Pending: AFP cases pending final classification
AFP surveillance in Somalia began in 1998. The majority of AFP cases reported in each of the years during 1998–2012 were male, with a consistent sex distribution of approximately three males to two females. The median age of AFP cases has been approximately two years of age over the past decade. The proportion of AFP cases that have not received OPV (zero-dose children) dropped from a high of 51% in 2000 to 8% in 2010. As of August 2013, the percentage of zero-dose AFP cases has again increased to 38%.
During 1998–2012, the annual non-polio AFP rates ranged from 0.62 cases per 100,000 persons <15 years of age in 1998 to 3.91 cases per 100,000 persons <15 years of age in 2007. Beginning in 2001, non-polio AFP rates consistently exceeded the minimum standard of 2 cases per 100,000 persons <15 years of age. As of August 2013, the country has achieved an annualized non-polio AFP rate of 5.86 cases per 100,000 persons <15 years of age for the year 2013.
With respect to other key surveillance indicators, the proportion of AFP cases reported within seven days of onset steadily improved through the years from a low of 19% in 1998 to a high of 90% in 2011 and 2012. The percentage of AFP cases with adequate stool specimens also improved from 35% in 1999 to 99% in 2009 and 2010, and remained at 98% during 2011–2012. National estimates of the non-polio enterovirus isolation rate, an indicator of the quality of the reverse cold chain system for stool specimens, were consistently above the target of ≥10%, except in 2003, when the rate was 9%. However, the estimate in the Northwest zone fluctuated and was below the target level on several occasions during 1998–2012.
WPV Incidence (Figure 2)
The number of reported WPV cases increased from 12 in 1998 to 96 in 2000, but sharply declined to seven and three cases in 2001 and 2002, respectively. Indigenous poliovirus transmission was interrupted in 2002, as no WPV cases were reported in Somalia in 2003 and 2004. In 2005, the country experienced a large, imported WPV outbreak which lasted until 2007 and resulted in 228 cases of paralytic polio, the majority of cases occurring during 2005. Somalia subsequently remained polio-free until April 2013, when another WPV importation initiated a widespread outbreak, which is currently ongoing and has led to 173 additional cases as of October 2013. Both polio outbreaks began in Banadir region, which also accounted for a majority of cases in the first outbreak and has so far reported the highest number of cases (69) in the current outbreak.
cVDPV Incidence (Figure 2)
During March 2008 through January 2013, 22 cVDPV cases were reported in Somalia. In 2008, two cases were reported, one each from Bari and Lower Shabelle regions. The number of cases increased to seven in 2009 but reduced again to two cases in 2010. In 2011, the cVDPV outbreak peaked, with nine cases reported, but subsequently declined in 2012, with only a single case reported. The most recent case was reported in January 2013. The country has now gone nine months without a single cVDPV case being reported. Of the 22 cases reported during 2008–2013, a majority were located in the contiguous and densely populated regions of Banadir (eight cases) and Lower Shabelle (six cases). All but two cases occurred in the South and Central zones; the other two cases occurred in the Northeast zone.
Immunization Activities
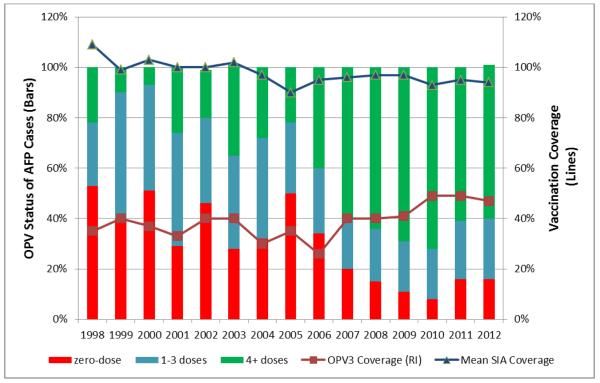
Routine Immunization (Figure 3)
Figure 3.
Bar Graph Showing Immunity Profile of AFP Cases with Line Graphs of Routine and Supplementary Immunization (Mean) Coverage, Somalia 1998–2012.
Routine immunization across Somalia is administered through Maternal and Child Health (MCH) centers using the EPI schedule, in which OPV is administered at birth (OPV0), 6 weeks (OPV1), 10 weeks (OPV2) and 14 weeks (OPV3). WHO-UNICEF estimates of OPV3 coverage remained consistently low (<50%) during 1998–2012. In 1998, OPV3 coverage was estimated at 35%; coverage estimates fluctuated between 30% and 40% until 2006, when it reached a low of 26%. Although OPV3 coverage estimates improved thereafter, reaching a high of 49% in 2010 and 2011, they still remain way below the desired national coverage level of ≥90%.
Beginning in 2009, Child Health Days (CHDs) have been carried out in Somalia as a means of delivering life-saving health interventions, including augmenting routine immunization services, as part of the Accelerated Young Child Survival (AYCS) strategy (14). During CHDs essential vaccines, such as measles-containing vaccine (MCV), diphtheria-pertussis-tetanus vaccine (DPT) and OPV, are typically administered as part of a health package that also includes vitamin A and deworming tablets. CHD coverage estimates have been incorporated into the calculation of OPV3 coverage since 2009.
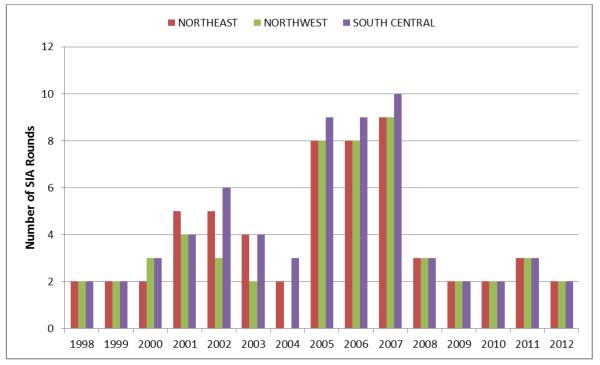
Polio SIAs (Figure 3, 4)
Figure 4.
Distribution of Polio Supplementary Immunization Activities (SIAs) by Year and Zone, Somalia 1998–2012.
During 1998–2012, at least two rounds of SIAs targeting children under five years were conducted in at least two administrative zones in each year under review. The number of SIAs conducted ranged from two rounds in multiple years to nine rounds in 2007 for the Northwest and Northeast zones, except for 2004 when no SIAs were conducted in the Northwest zone. Similarly, the number of SIAs conducted in South Central Somalia during 1998–2012 ranged from two (multiple years) to ten in 2007 (Figure 4). Examining the number of SIAs conducted annually in each of the three zones by smaller time intervals, five or fewer SIAs were conducted per year during 1998–2004, 8–10 SIAs during 2005–2007, and three or fewer SIAs were carried out during 2008–2012. SIAs in South Central Somalia also covered a much smaller median number of districts (29–35 districts) per year during 2010–2012 compared with previous years (59–79 districts). Administrative SIA coverage estimates in all three zones was high – reaching or exceeding 100% on several occasions – during the period under review. During 1998–2012, mean coverage estimates ranged from 73% (1999) to 106% (2011) in the Northeast zone; 86% (2002) to 105% (1999) in the Northwest zone; and 88% (2010) to 125% (1998) in South Central Somalia (Figure 3). For the years in which data were available (2006–2012), vaccine refusals were consistently <1%.
The onset of a WPV outbreak in 2013 has again been followed by an increase in the number of SIAs, as at least seven rounds of SIAs have been conducted in accessible districts in each zone of the country. However, at least 27 districts, all in South Central Somalia, have remained completely inaccessible for the conduct of vaccination campaigns owing to a ban imposed by anti-government elements. Among districts where campaigns have been conducted, some have only been partially accessible while others have posed significant security challenges to both vaccinators and recipients of the polio vaccine. Data from these campaigns is still being compiled but preliminary results suggest high (>90%) administrative coverage. Three more rounds of campaigns are planned from October through December.
Special Strategies
Trivalent OPV (tOPV) is the designated vaccine for routine immunization against polio and has been the most commonly used vaccine for immunization campaigns in Somalia. However, in response to the 2005–2007 WPV outbreak, monovalent OPV type 1 (mOPV1) was used during a majority of vaccination campaigns, with the country reverting back to tOPV for campaigns after the outbreak was successfully interrupted. With the onset of the 2013 WPV outbreak, bivalent OPV (bOPV) has be en the vaccine of choice for campaigns. Further, the target age group for vaccination has been expanded from the typical group of children under five years of age to children under ten years and, in some instances, all age groups. Campaigns have also been synchronized with the neighboring countries of Kenya and Ethiopia, where feasible, just as was the case during the earlier outbreak.
To foster vaccine acceptance and high participation levels during campaigns, strong emphasis is placed on community engagement and social mobilization in the build-up to and during campaigns. This is often accomplished through mass media, social mobilizers/announcers, and engagement of political and religious leaders within the community. For children in hard-to-reach and inaccessible areas, a special fixed-site/transit-point vaccination strategy has been established with the aim of vaccinating children commuting between accessible and inaccessible areas through permanent vaccination teams assigned to designated transit points.
Discussion
Over the past 15 years, Somalia’s polio eradication programme has been marked by significant triumphs and setbacks. Three major periods have defined the most critical events in the country’s progress toward polio eradication: 1998–2002, which culminated in the interruption of indigenous transmission of WPV; 2003–2007, during which the country was initially polio-free but, beginning in 2005, experienced an outbreak of WPV that was successfully interrupted in 2007; 2008–2013 (present), a period marked by, first, a prolonged outbreak of circulating vaccine-derived poliovirus and then, in 2013, the occurrence of a second outbreak of WPV.
During the years leading up to the interruption of WPV circulation in 2002, AFP surveillance activities were intensified, as were efforts to improve the population immunity through supplementary immunization activities. By 2001, the non-polio AFP rate had improved to 3.1 cases per 100,000 persons <15years, well above the benchmark of ≥2 cases per 100,000 persons <15 years for countries in regions where endemic circulation of polio has not been interrupted (16). Concurrently, at least four SIAs were conducted in each zone during the same year, a standard that was sustained the following year, when endemic transmission of wild poliovirus was halted. This was accomplished in spite of routine immunization coverage that was only at 40% in 2002 (12, 13) and ongoing conflict that made the conduct of vaccination campaigns hazardous (5, 10).
Somalia’s initial polio-free status was short-lived, as an imported WPV case in 2005 precipitated a large and widespread outbreak that continued until March 2007 (6). Vulnerability to the outbreak may not only have been due to the enabling conditions created by continuing internal conflict and low routine immunization, but also owing to an apparent decline in the number of vaccination campaigns conducted in all three zones to three or fewer in 2004. This situation was promptly rectified in response to the outbreak, as an average of 8–10 campaigns were conducted annually in each zone during 2005–2007, with the then newly licensed mOPV1 (17) as the vaccine of choice in many of these campaigns. The superior immunogenicity of this type of OPV against WPV 1 relative to tOPV (18, 19), coupled with the number of campaigns conducted, greatly enhanced the ability of response activities to interrupt the outbreak. Of note, the country’s surveillance system remained strong in the years prior to and during the outbreak, with non-polio AFP rates consistently ≥2 per 100,000 persons <15 years and >80% of AFP cases having adequate stool specimens in each year during 2003–2007. The quality of surveillance not only enabled the country to detect the outbreak in the first place, it also provided assurance of its successful interruption.
A different form of challenge emerged after the 2005–2007 WPV outbreak. Two cases of circulating vaccine-derived poliovirus were reported from Bari and Lower Shabelle regions with dates of onset in 2008, reflecting gaps in population immunity against type 2 vaccine-derived poliovirus. They were to become the first of 22 cases in a prolonged cVDPV outbreak that had its most recent case reported in January 2013 and spread to refugee camps in neighboring parts of Kenya (20). All cases identified during the outbreak have been type 2 cVDPV, a scenario that could have arisen owing to the use of mOPV1 during most of the 2005–2007 campaigns in a setting of low routine immunization coverage, thus allowing for the establishment of an immunity gap and population vulnerability to cVDPV type 2 (21). Another factor which could have accounted for the protracted nature of this outbreak was the ban imposed by anti-government elements on the conduct of vaccination campaigns in several districts of South Central Somalia. Beginning in 2009, when the ban was imposed, fewer districts were covered during campaigns in South Central Somalia, resulting in approximately one million children under ten years of age being unvaccinated against polio.
In the midst of prevailing challenges with conducting vaccination campaigns, the country’s AFP surveillance system detected an imported WPV type 1 case in May 2013 (date of paralysis onset: April 18, 2013), representing the first WPV case in Somalia in over six years. As of October 2013, 173 additional cases have been reported, representing a large and widespread outbreak, which is currently ongoing. As in the previous outbreak, the index case was detected in Banadir region, which has yet again turned out to be the epicenter of the current outbreak. Genetic sequencing has shown that the WPV outbreak strain is closely related to strains circulating in West Africa (7). Several factors could explain the occurrence of this outbreak. First, owing to the ban on vaccination campaigns, the large pool of susceptible children in South Central Somalia left the population highly vulnerable to a polio outbreak. Second, poor sanitation occasioned by high population density in urban areas and movement of internally displaced persons due to ongoing conflict created the conditions for ease of spread of WPV, given its fecal-oral route of transmission (22). Third, a major humanitarian crisis occurred in the Horn of Africa region in 2011, in which drought and famine left millions of Somali children malnourished and many families displaced (4, 23); factors that have further degraded the already weak population immunity profile against polio. All these factors occurring in a country with a dilapidated healthcare system and poor routine immunization coverage meant that it was only a matter of time for the country to experience another WPV outbreak.
The response to the current outbreak has again been swift, robust and innovative. Seven rounds of vaccination campaigns have been completed since the onset of the outbreak and three more are scheduled to take place before the end of the year. Bivalent OPV, owing to its superior immunogenicity (24), is being used for campaigns, target age groups have been expanded – sometimes to include all age groups – and special strategies, such as vaccination at transit points and cross border sites, are being implemented to reach children in areas that are inaccessible for the conduct of campaigns. Preliminary results suggest high coverage in areas where vaccination campaigns have been conducted and monitored. The frequency and quality of these campaigns, coupled with the intensification of surveillance activities, gives reason for cautious optimism that Somalia will again interrupt WPV transmission. If again achieved, maintaining Somalia’s polio-free status will depend on finding strategies to deliver polio vaccines on a consistent basis in a setting of ongoing conflict and a country with severely weakened healthcare infrastructure.
Acknowledgements
We acknowledge the support of Ali Abdi Hassan and Carolyne Gathenji with compiling and updating the databases used in the preparation of this manuscript.
Funding Sources/Disclaimer: None. This manuscript was prepared as part of the official duties of the authors at the US Centers for Disease Control and Prevention and World Health Organization, Somalia Liaison Office. However, the findings and conclusions in this paper are those of the authors and do not necessarily represent the official position of the organizations they work for.
Footnotes
Disclosures/Conflicts of Interest: We have not previously published the contents of this manuscript nor are we submitting it elsewhere for consideration. There are no situations that might be perceived as a conflict of interest with the publication of this manuscript.
References
- 1.World Health Assembly [Accessed September 16, 2013];WHA Resolution 41.28. 1988 Available at: http://www.polioeradication.org/content/publications/19880513_resolution.pdf.
- 2.Hull HF, Birmingham ME, Melgaard B, Lee JW. Progress toward global polio eradication. J Infect Dis. 1997;175(Suppl 1):S4–9. doi: 10.1093/infdis/175.supplement_1.s4. [DOI] [PubMed] [Google Scholar]
- 3.CDC Progress toward poliomyelitis eradication--Ethiopia, Somalia, and Sudan, January 2002-August 2003. MMWR Morb Mortal Wkly Rep. 2003;52(44):1076–9. [PubMed] [Google Scholar]
- 4.Mahomed Z, Moolla M, Motara F, Laher A. A Somalia mission experience. S Afr Med J. 2012;102(8):659–660. doi: 10.7196/samj.5970. [DOI] [PubMed] [Google Scholar]
- 5.Grunewald F. Aid in a city at war: the case of Mogadishu, Somalia. Disasters. 2012;36(S1):S105–S125. doi: 10.1111/j.1467-7717.2012.01287.x. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization Somalia is again polio-free. Wkly Epidemiol Rec. 2008;83(14):117–8. [PubMed] [Google Scholar]
- 7.CDC Notes from the field: outbreak of poliomyelitis--Somalia and Kenya, May 2013. MMWR Morb Mortal Wkly Rep. 2013;62(23):484. [PMC free article] [PubMed] [Google Scholar]
- 8.Kohler JC, Pavignani E, Michael M, Ovtcharenko N, Murru M, Hill PS. An examination of pharmaceutical systems in severely disrupted countries. BMC International Health and Human Rights. 2012;12:34. doi: 10.1186/1472-698X-12-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kamadjeu R, Assegid K, Naouri B, Mirza IR, Hirsi A, Mohammed A, Omer M, Dualle AH, Mulugeta A. Measles control and elimination in Somalia: the good, the bad, and the ugly. J Infect Dis. 2011;204(Suppl 1):S312–7. doi: 10.1093/infdis/jir066. [DOI] [PubMed] [Google Scholar]
- 10.Bower H. Arming the population against polio in Somalia. Lancet. 2000;356(9225):229. doi: 10.1016/s0140-6736(05)74482-2. [DOI] [PubMed] [Google Scholar]
- 11.Global Polio Eradication Initiative [Accessed September 16, 2013];Strategic Plan 2010–2012. Available at: http://www.polioeradication.org/Portals/0/Document/StrategicPlan/StratPlan2010_2012_ENG.pdf.
- 12.WHO [Accessed September 16, 2013];WHO vaccine-preventable diseases: monitoring system. 2013 global summary. Available at: http://apps.who.int/immunization_monitoring/globalsummary/coverages?c=SOM.
- 13.WHO [Accessed September 16, 2013];Somalia: WHO and UNICEF estimates of immunization coverage: 2012 revision. Available at: http://www.who.int/immunization_monitoring/data/som.pdf.
- 14.Mirza IR, Kamadjeu R, Assegid K, Mulugeta A. Somalia: supporting the child survival agenda when routine health service is broken. J Infect Dis. 2012;205(Suppl 1):S126–33. doi: 10.1093/infdis/jir776. [DOI] [PubMed] [Google Scholar]
- 15.United Nations, Population Division . The World Population Prospects - the 2012 revision. New York: 2013. [Google Scholar]
- 16.CDC Evaluating Surveillance Indicators Supporting the Global Polio Eradication Initiative, 2011–2012. MMWR Morb Mortal Wkly Rep. 2013;62(14):270–4. [PMC free article] [PubMed] [Google Scholar]
- 17.Farag MM. Licensing of monovalent OPV1 vaccine. Biologicals. 2006;34(2):145–9. doi: 10.1016/j.biologicals.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 18.Grassly NC, Wenger J, Durrani S, Bahl S, Deshpande JM, Sutter RW, Heymann DL, Aylward RB. Protective efficacy of a monovalent oral type 1 poliovirus vaccine: a case-control study. Lancet. 2007;369(9570):1356–62. doi: 10.1016/S0140-6736(07)60531-5. [DOI] [PubMed] [Google Scholar]
- 19.Jenkins HE, Aylward RB, Gasasira A, Donnelly CA, Abanida EA, Koleosho-Adelekan T, Grassly NC. Effectiveness of immunization against paralytic poliomyelitis in Nigeria. N Engl J Med. 2008;359(16):1666–74. doi: 10.1056/NEJMoa0803259. [DOI] [PubMed] [Google Scholar]
- 20.CDC Update on vaccine-derived polioviruses— worldwide, April 2011–June 2012. MMWR. 2012;61:741–6. [PubMed] [Google Scholar]
- 21.Kew OM, Sutter RW, de Gourville EM, Dowdle WR, Pallansch MA. Vaccine-derived polioviruses and the endgame strategy for global polio eradication. Annu Rev Microbiol. 2005;59:587–635. doi: 10.1146/annurev.micro.58.030603.123625. [DOI] [PubMed] [Google Scholar]
- 22.Fine PE, Carneiro IA. Transmissibility and Persistence of Oral Polio Vaccine Viruses: Implications for the Global Poliomyelitis Eradication Initiative. Am J Epidemiol. 1999;150(10):1001–1019. doi: 10.1093/oxfordjournals.aje.a009924. [DOI] [PubMed] [Google Scholar]
- 23.Loewenberg S. Humanitarian response inadequate in Horn of Africa crisis. Lancet. 2011;13(378(9791)):555–8. doi: 10.1016/s0140-6736(11)61276-2. [DOI] [PubMed] [Google Scholar]
- 24.Sutter RW, John TJ, Jain H, Agarkhedkar S, Ramanan PV, Verma H, Deshpande J, Singh AP, Sreevatsava M, Malankar P, Burton A, Chatterjee A, Jafari H, Aylward RB. Immunogenicity of bivalent types 1 and 3 oral poliovirus vaccine: a randomised, double-blind, controlled trial. Lancet. 2010;376(9753):1682–8. doi: 10.1016/S0140-6736(10)61230-5. [DOI] [PubMed] [Google Scholar]