Abstract
BACKGROUND
Coronary computed tomography angiography plays an expanding role managing symptomatic patients with suspected coronary artery disease. Prospective intermediate-term outcomes are lacking.
OBJECTIVE
To compare coronary CT angiography with conventional non-invasive testing.
DESIGN
Randomized, controlled comparative effectiveness trial.
SETTING
Telemetry-monitored wards of one inner-city medical center.
PATIENTS
400 acute chest pain patients (mean age 57); 63% women; 54% Hispanic, 37% African-American; low socioeconomic status.
INTERVENTION
Coronary CT angiography (CT) or radionuclide stress myocardial perfusion imaging (MPI).
MEASUREMENTS
The primary outcome was cardiac catheterization not leading to revascularization within one year. Secondary outcomes included length of stay, resource utilization and patient experience. Safety outcomes included death, major cardiovascular events and radiation exposure.
RESULTS
30(15%) CT patients and 32(16%) MPI patients underwent cardiac catheterization within one year, of which 15(7.5%) and 20(10%), respectively, were not revascularized (-2.5% difference, 95%CI −8.6%–+3.5%; hazard ratio 0.77, 95%CI 0.40–1.49, p=0.44). Median length of stay was 28.9 hours for CT and 30.4 hours for MPI (p=0.057). Median follow-up was 40.4 months. For CT and MPI, the incidences of death (0.5% vs 3%, p=0.12), non-fatal cardiovascular events (4.5% vs 4.5%), re-hospitalization (43% vs 49%), emergency visit (63% vs 58%) and outpatient cardiology visit (23% vs 21%) were not different. Long-term, all-cause radiation was lower for CT (24 vs 29 milliSieverts, p<0.001). More CT patients graded their experience favorably (p=0.001) and would undergo the exam again (p=0.003).
LIMITATIONS
Single site study; primary outcome dependent on clinical management decisions.
CONCLUSIONS
There were no significant differences between CT and MPI in outcomes or resource utilization over 40 months. CT had lower associated radiation and was more positively-experienced than MPI.
PRIMARY FUNDING SOURCE
American Heart Association.
INTRODUCTION
Cardiovascular disease, including coronary heart disease, is the leading cause of mortality worldwide (1–2). Chest pain with clinical suspicion of coronary artery disease is among the most frequent reasons for urgent care and leads to several million Emergency Department visits and hospitalizations yearly (3). Clinical evaluation is often supplemented with non-invasive cardiac imaging despite the lack of evidence for outcomes benefits and a low diagnostic yield (4). The choice of modality is a focus area for comparative effectiveness research (5).
Coronary computed tomography angiography (CT), a relatively new diagnostic modality, has become a dominant means for evaluating chest pain patients and has impressive diagnostic (6–8) and prognostic (9–11) power. Registry data suggests that CT appropriately selects patients for cardiac catheterization and coronary revascularization (12–13). Randomized trials conducted in low-risk Emergency Department chest pain patients demonstrate that CT is more time-efficient and inexpensive than standard triage protocols which usually involve electrocardiography-, echocardiography- or radionuclide scintigraphy stress testing (14–17).
Concerns regarding CT remain, including false positive results (6,8) leading to invasive management, high radiation dose (17–18), increased downstream resource utilization (17, 19–20) and the relatively low risk profile and short duration of follow-up in the published prospective studies (14–17). Women and ethnic minorities are underrepresented in the existing literature (21–23). It is widely appreciated that results of studies performed in men and in homogeneous ethnic populations require validation before widespread clinical application.
We set out to study coronary CT in an ethnically diverse, inner-city, majority women population of intermediate risk chest pain patients admitted to telemetry with a planned intermediate term of follow-up. As a comparison, we used radionuclide stress myocardial perfusion imaging (MPI), our institution’s default imaging modality and perhaps the best-studied non-invasive exam for detecting severe coronary heart disease (24). We hypothesized that CT would provide superior selection of patients for invasive management and decrease length of stay without compromise of patient safety, as compared to MPI.
METHODS
Design Overview
PROSPECT (Prospective Randomized Outcome trial comparing radionuclide Stress myocardial Perfusion imaging and ECG-gated coronary CT angiography) was a randomized, controlled comparative effectiveness trial comparing initial CT with MPI in chest pain patients admitted to telemetry at a single center who clinically required non-invasive imaging to determine management and met pre-defined intermediate risk criteria. Patients were clinically assigned to any one of a group of approximately 30 managing physicians, most of which were hospitalists on the physician assistant telemetry service. Assessors of the primary outcome were blinded to trial arm; patients, imagers, coronary angiographers and managing clinicians were not blinded. The complete trial design and rationale has been previously described (25). The study was approved by our institutional review board, HIPAA compliant, overseen by an independent Data and Safety Monitoring Board and registered at ClinicalTrials.gov (NCT00705458).
Setting and Participants
Patients were identified by screening telemetry admissions for chest pain from July 2008 through March 2012 (when the recruitment goal was reached) at our inner-city academic medical center. Patients without known coronary artery disease, as determined by patient and physician interview and review of medical records, were potentially eligible if there was no acute myocardial infarction/ ischemia on ECG or serum cardiac biomarkers. At least one intermediate risk criterion for short-term death or myocardial infarction derived from an unstable angina management guideline (26) was required: (1) pain for >20 minutes, (2) pain onset at exertion within the previous two weeks, (3) age >70 years, (4) sub-threshold elevation of serum troponin-T, or (5) non-specific ST-segment or T-wave changes on presentation ECG. Exclusion criteria included: prior coronary CT, MPI or cardiac catheterization within 6 months and contraindications to coronary CT including renal insufficiency, active asthma, poor venous access, intravenous contrast allergy or other serious allergy and dysrhythmia precluding cardiac gating. All patients provided written, informed consent (English and Spanish forms provided). No patients were excluded due to language as a telephone interpretation service was used. Patients were not compensated for participation.
Randomization and Interventions
Blocked, 1:1 randomization was performed by an experienced biostatistician (KDF) using SAS software-generated codes. Codes were concealed in sequentially-numbered, sealed, opaque envelopes. Trial coordination staff enrolled participants and assigned the initial imaging intervention which was then formally ordered by the managing hospitalist. Imaging was performed immediately and interpreted with complete access to clinical information and without blinding. After imaging, clinical care decisions were made by the managing physicians.
Coronary computed tomography angiography (CT) was performed on conventional 64-detector-row scanners with heart rate control by intravenous metoprolol tartrate, when needed. Coronary calcium was scored. CT angiography was retrospectively gated with ECG-triggered current modulation or prospectively gated, depending on availability and heart rate. Patients received intravenous iodixanol-320 followed by a saline chaser at 5 ml/second. Scanner voltage and current, contrast injection protocol and pre-medication with sublingual nitroglycerin were tailored by the cardiothoracic radiologist. One of multiple experienced, subspecialty fellowship trained cardiothoracic radiologists interpreted the studies using multiplanar, curved planar and maximum intensity projection reconstructions.
Radionuclide stress myocardial perfusion imaging (MPI) was generally performed using one-day dual-isotope (201-Tl rest / 99m-Tc-sestamibi stress) or 99m-Tc-sestamibi rest/stress imaging. The default stressor was treadmill exercise per the Bruce protocol. Patients unable to exercise received intravenous adenosine or regadenoson with or without low-level exercise. The exact administered dose, radiotracers and mode of stress were tailored by the nuclear cardiologist. Single photon emission computed tomography, gated and attenuation-corrected images were generated. One of multiple experienced, certified, nuclear cardiologists or nuclear medicine physicians interpreted the studies using standard quantification algorithms.
Outcomes and Follow-up
The primary outcome was catheterization not leading to percutaneous or surgical revascularization within one year. The primary goal of non-invasive coronary imaging is to select patients who may benefit from revascularization and to obviate cardiac catheterization in the remaining patients. Although debate rages regarding the appropriate use of coronary revascularization, catheterization that does not lead to intervention confers limited incremental value and entails risk. This outcome was measured up to one year as non-invasive imaging should inform the decision to perform catheterization for a significant period of time and there may be patient-related reasons for delay of revascularization. Since the decision to revascularize is multifactorial, a subgroup analysis was performed for patients with significantly abnormal initial non-invasive imaging (at least one ≥70% stenosis or ≥50% left main stenosis on CT; global interpretation of ischemia or probable ischemia on MPI). More detailed description of imaging results is deferred as our primary outcomes were clinical rather than imaging findings.
Length of hospital stay was calculated from randomization to discharge for all patients. Safety outcomes included complications from imaging and revascularization, post-test renal dysfunction, all-cause mortality and non-fatal major adverse cardiovascular events (myocardial infarction, cardiac arrest and cerebrovascular accident). Subsequent resource utilization (hospitalization, Emergency Department visit, cardiac and non-cardiac imaging and changes in pharmacotherapy) was recorded. Patients’ subjective experiences of imaging were assessed on a 10-point Likert-type scale (1 is best), by comparison to other diagnostic testing on an ordinal scale, by willingness to undergo the procedure again on an ordinal scale and by recorded complaints immediately after imaging. The persistence of chest pain was assessed at telephone follow-up. Radiation from CT was estimated using the dose-length product and a conversion factor of .017 microSieverts / milliGray * cm. Radiation from MPI was estimated using recorded standard dose of isotope and a public calculator (27). Doses from subsequent imaging and catheterization were determined with a public calculator (28).
Outcomes were assessed by review of electronic medical records (spanning numerous health system sites) and telephone questionnaires at 6 and 12 months after discharge and at study completion (December 2013). Patients unreachable by telephone and without institutional electronic records were followed-up by contacting providers’ offices. When patients, physicians or records indicated that cardiac care was rendered outside our health system, records were requested for review.
Statistical Analysis
The study had 84% power to detect a reduction of catheterization not leading to revascularization from 11% to 3% with a sample size of 200 per arm at α=0.05 (25). All randomized patients were included in the analysis in the trial arm to which they randomized. The primary outcome was assessed by a Cox proportional hazards model (PROC PHREG in SAS version 9.2) with the proportional hazards assumption tested by log-rank and inspection of survival curves. A post-hoc exploratory analysis for the primary outcome was performed in patients with severely abnormal non-invasive testing. Safety outcome and resource utilization analyses included all patients over the complete follow-up period. Proportions were compared using Fisher’s exact tests (29) and confidence intervals were computed for differences (30). The Mann-Whitney U test for independent samples was used for non-parametric data using SPSS version 20. All tests were two-tailed and performed at α=0.05.
Role of the Funding Source
This study was supported by American Heart Association Clinical Research Program Grant 0885024D (funded conduct of the study). This study was also supported in part by the CTSA Grants 1 UL1 TR001073-01, 1 TL1 TR001072-01, 1 KL2 TR001071-01 from the National Center for Advancing Translational Sciences, a component of the National Institutes of Health (funded part of the data analysis). No funding source influenced the design, conduct or reporting of the study.
RESULTS
Study Patients
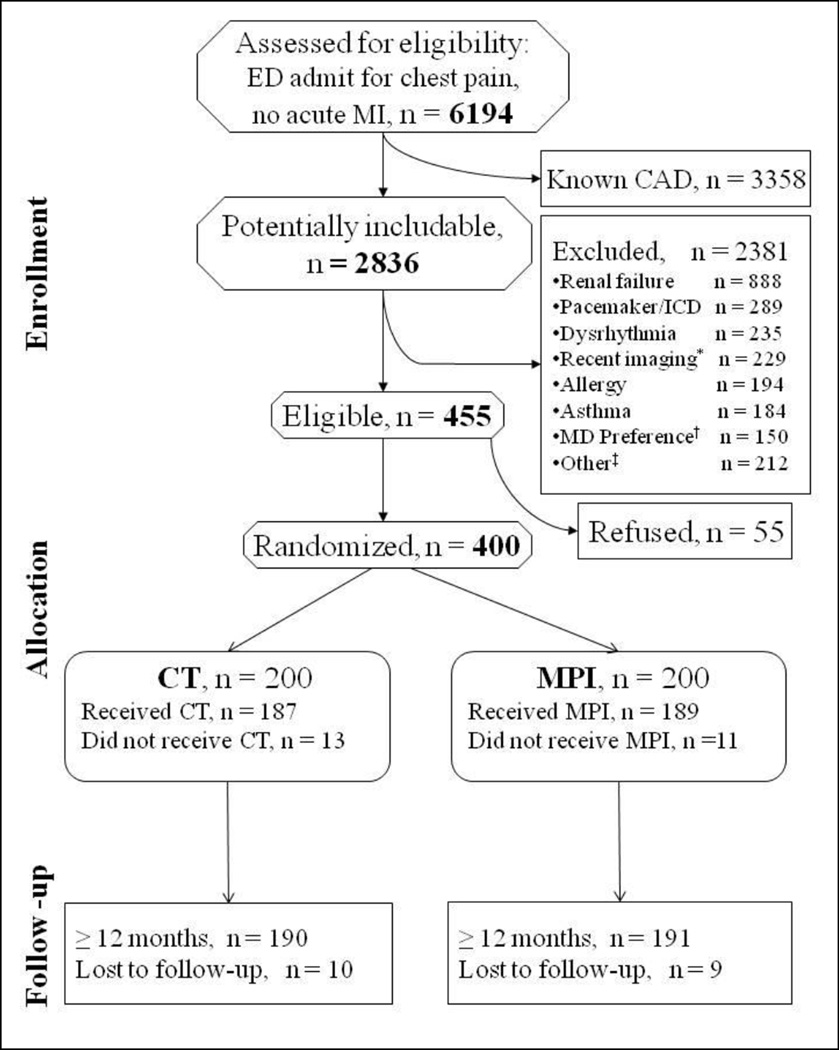
Of 400 patients, 200 were randomly assigned to each arm (Fig. 1). The mean age was 57 years, 251 (63%) participants were women and 379 (95%) were ethnic minorities (Table 1). The randomized test was completed in similar proportions of patients for CT (94%) and MPI (95%). Follow-up of at least one year for the primary outcome and adverse events was complete in 381 (95%). The 19 patients lost to follow-up had similar demographics (mean age 56; 9 women).
Figure 1.
CONSORT Flow Diagram.
Footnote: CAD, coronary artery disease; CT, coronary computed tomography angiography; ED, emergency department; ICD, implanted cardioverter/defibrillator; MI, myocardial infarction; MPI, radionuclide stress myocardial perfusion imaging.
*Recent imaging means coronary CT, MPI or cardiac catheterization within 6 months
†MD preference means the managing physician had already chosen a non-invasive imaging modality and would not allow the patient to be randomized.
‡Other reasons for exclusion are listed in Supplementary Online Table 1.
CT was not performed in 13 patients because of patient refusal (9), physician decision (1), technical difficulty (1) and safety concerns (2); of these, 7 patients received MPI. MPI was not performed in 11 patients because of patient refusal (6), physician decision (4), and technical difficulty (1); of these, 0 patients received CT. During hospitalization, 6 patients that received initial CT had additional MPI and 4 patients that received initial MPI underwent additional CT. Lost patients could not be contacted by any means including identification and inquiry of any treating physicians. All patients were included in the primary analysis (Cox proportional hazards model).
Table 1.
Baseline Characteristics
| Characteristic | Total (n=400) | CT (n=200) | MPI (n=200) |
|---|---|---|---|
| Demographics | |||
| Female | 251 (62.8) | 126 (63.0) | 125 (62.5) |
| Mean Age (SD) | 56.6 (11.2) years | 56.8 (11.8) years | 56.3 (10.5) years |
| Ethnicity (self-reported) | |||
| Hispanic | 213 (53.7) | 105 (52.8) | 108 (54.6) |
| African-American | 145 (36.5) | 78 (39) | 67 (34) |
| Asian | 18 (4.5) | 7 (4) | 11 (5.6) |
| Caucasian | 18 (4.5) | 8 (4) | 10 (5.1) |
| Other | 3 (0.8) | 1 (0.5) | 2 (1) |
| Interpreter used | 103 (25.8) | 50 (25) | 53 (27) |
| Mean SES Z-score* | −4.2 | −4.1 | −4.3 |
| Risk Factors | |||
| Mean BMI (SD) | 30.6 (6.4) kg/m2 | 30.5 (6.2) kg/m2 | 30.7 (6.6) kg/m2 |
| Diabetes mellitus | 127 (31.8) | 66 (33) | 61 (31) |
| Hypertension | 288 (72.0) | 141 (70.5) | 147 (73.5) |
| Mean Systolic / Diastolic Blood Pressure (SD) |
127 (20) / 75 (13) mmHg | 129 (20) / 76 (12) mmHg | 126 (20) / 75 (14) mmHg |
| Dyslipidemia | 296 (51.5) | 97 (49) | 109 (55) |
| Taking statin | 135 (33.8) | 61 (31) | 74 (37) |
| Current smoker | 59 (15) | 33 (17) | 26 (13) |
| 1° relative with CAD | 148 (37.0) | 75 (38) | 73 (37) |
| Taking aspirin | 149 (37.5) | 77 (39) | 72 (36) |
| No regular exercise | 180 (45.0) | 98 (49) | 82 (41) |
| Post-menopausal women | 174 (43.5) | 87 (44) | 87 (44) |
| Presentation / Risk Criteria | |||
| Pain > 20 minutes | 248 (62.0) | 123 (61.5) | 125 (62.5) |
| New pain on exertion within last 2 weeks |
151 (37.8) | 72 (36) | 79 (40) |
| ST or T wave abnormality on ECG |
113 (28.3) | 49 (25) | 64 (32) |
| Age ≥ 70 years | 54 (14) | 34 (17) | 20 (10) |
| Sub-clinical Troponin elevation |
19 (4.8) | 8 (4) | 11 (5.5) |
| Diamond-Forrester | |||
| Mean Pre-test probability | 37% | 36% | 37% |
| Retrosternal pain | 278 (69.5) | 134 (67.0) | 144 (72.0) |
| Extertional pain | 160 (40.0) | 77 (39) | 83 (42) |
| Relieved by rest or nitroglycerin |
189 (47.3) | 95 (48) | 94 (47) |
| Mean TIMI Score (SD) | 1.3 (1.0) | 1.3 (1.0) | 1.2 (1.0) |
| Past Medical History | |||
| Gastroesophageal reflux or ulcer disease |
182 (45.5) | 88 (44) | 94 (47) |
| Chest wall, rib or muscle pain |
109 (27.3) | 48 (24) | 61 (31) |
| Panic attacks or anxiety disorders |
96 (24) | 41 (21) | 55 (28) |
BMI, body mass index; CAD, coronary artery disease; CT, coronary computed tomography angiography; ECG, electrocardiogram; MPI, radionuclide stress myocardial perfusion imaging; SD, standard deviation; SES, socioeconomic status; TIMI, thrombolysis in myocardial infarction
Numbers in parentheses represent percents unless otherwise noted.
Socioeconomic status score is based on the patient's address zip code (median household income, median value of housing units, percentage of households receiving interest/dividend/rental income, education, percentage of adults who completed college, and percentage of employed individuals in executive/managerial/professional positions) and is normalized to the New York state average.
Outcomes
30 (15%) CT patients and 32 (16%) MPI patients underwent one or more cardiac catheterizations within one year (p=0.89), (Table 2). Of these, 15 CT and 20 MPI patients were not revascularized (unadjusted hazard ratio 0.77 [95% confidence interval = 0.40 −1.49], p=0.44). The median times to catheterization and revascularization were 3.5 (inter-quartile range [IQR] 2 – 28.5) and 2 (IQR 1.5 – 3.5) days, respectively, for CT and 2 (IQR 1 – 5) and 1.5 (IQR 1 – 4) days, respectively, for MPI. In the exploratory subgroup of patients with significantly abnormal CT or MPI, 5/20 (25%) and 16/31 (52%) had catheterization that did not lead to revascularization, respectively (absolute difference −27%, 95% confidence interval = -50% to +3.9%, p=0.083). The median lengths of stay in the CT and MPI arms were 28.9 (IQR 11.0 – 48.4) hours and 30.4 (IQR 23.9 – 51.3) hours, respectively (p=0.057). No patients in either arm had post-test renal dysfunction. The median follow-up for safety outcomes was 41.7 (IQR 28.6 – 51.0) and 39.0 (IQR 28.3 – 51.6) months for CT and MPI, respectively. One CT patient and 6 MPI patients died during follow-up (p=0.122) at a median of 24.5 months after recruitment. 9 CT patients and 9 MPI patients had non-fatal major adverse cardiovascular events.
Table 2.
Primary, Secondary and Safety Outcomes
| Outcome | CT (%) (n=200) |
MPI (%) (n=200) |
% Difference* (95% CI) |
P |
|---|---|---|---|---|
|
Cardiac catheterization within 1 year |
30 (15) | 32 (16) | −1.0 (−8.5, 6.5) | 0.89 |
|
Cardiac catheterization without revascularization within 1 year |
15 (7.5) | 20 (10) | −2.5 (−8.6, 3.5) | 0.41 |
| CABG within 1 year | 7 (4) | 1 (0.5) | 3.0 (−0.3, 6.9) | 0.068 |
| PCI within 1 year | 8 (4) | 11 (5.5) | −1.5 (−6.4, 3.3) | 0.64 |
|
Median length of stay in hours (IQR) |
28.9 (11.0, 48.4) |
30.4 (23.9, 51.3) |
0.057 | |
|
Serious complications of imaging |
0 | 0 | 0 (−2.4, 2.4) | 1 |
|
Serious complications of revascularization† |
3 (2) | 1 (0.5) | 1.0 (−1.9, 4.2) | 0.62 |
| All-cause death | 1 (0.5) | 6 (3) | −2.5 (−6.3, .7) | 0.122 |
| Non-fatal MACE ‡ | 9 (5) | 9 (5) | 0 (−4.7, 4.7) | 1 |
| Death + MACE § | 9 (5) | 15 (7.5) | −3.0 (−8.3, 2.2) | 0.29 |
CABG, coronary artery bypass grafting; CI, confidence interval; CT, coronary computed tomography angiography; IQR, inter-quartile range; MACE, major adverse cardiovascular events (consisting of myocardial infarction, stroke and cardiac arrest); MPI, radionuclide stress myocardial perfusion imaging; PCI, percutaneous coronary intervention
% Difference equals proportion in the MPI arm minus proportion in the CT arm
Two CT patients had complications after coronary artery bypass grafting (one sternal wound infection and one prolonged mechanical ventilation). One MPI patient had coronary artery dissection during percutaneous intervention. One CT patient had coronary artery perforation during percutaneous intervention for a subsequent acute myocardial infarction.
Two MPI patients each had two separate cerebrovascular accidents.
One CT patient had a non-fatal myocardial infarction and later died.
Clinical and imaging resource utilization is shown in Table 3.
Table 3.
Resource utilization over the complete follow-up period
| Resource | CT (%) (n=200) |
MPI (%) (n=200) |
% Difference* (95% CI) |
P |
|---|---|---|---|---|
|
Clinical | ||||
| Any re-hospitalization | 86 (43) | 98 (49) | −6.0 (−16, 4.1) | 0.27 |
| Cardiac re-hospitalization | 50 (25) | 61 (31) | −5.5 (−15, 3.6) | 0.26 |
| Any cause ED visit | 126 (63.0) | 115 (57.5) | 5.5 (−4.4, 15) | 0.31 |
| Cardiac ED visit | 41 (21) | 40 (20) | 0.5 (−7.7, 8.7) | 1 |
| Primary care visit | 114 (57.0) | 112 (56.0) | 1.0 (−9.0, 11) | 0.92 |
|
Cardiology outpatient visit |
46 (23) | 42 (21) | 2.0 (−6.5, 10) | 0.72 |
|
Pharmacotherapy | ||||
| New aspirin Rx | 79 (40) | 68 (34) | 5.5 (−4.3, 15) | 0.30 |
| New statin Rx | 50 (25) | 36 (18) | 7.0 (−1.4, 15) | 0.113 |
| Increased statin dose | 6 (3) | 6 (3) | 0 (−4.1, 4.1) | 1 |
|
Imaging | ||||
| Subsequent CT | 2 (1) | 5 (3) | −1.5 (−5.2, 1.8) | 0.45 |
| Subsequent MPI | 30 (15) | 26 (13) | 2.0 (−5.2, 9.2) | 0.67 |
| Subsequent SE | 13 (6.5) | 14 (7) | −0.5 (−6.0, 5.0) | 1 |
|
Subsequent catheterization† |
36 (18) | 38 (19) | 1.0 (−7.0, 9.0) | 0.90 |
|
Subsequent catheterization with PCI† |
9 (5) | 14 (7.0) | −2.5 (−7.7, 2.6) | 0.39 |
CI, confidence interval; CT, coronary computed tomography angiography; ED, emergency department; MPI, radionuclide stress myocardial perfusion imaging; PCI, percutaneous coronary intervention; Rx, prescription; SE, stress echocardiography
% Difference equals proportion in the MPI arm minus proportion in the CT arm
Figures differ from Table 2 and the text which report catheterizations within one year.
Three CT patients received non-coronary diagnoses that led to surgery (one ascending aortic aneurysm, one atrial septal defect and one adrenal pheochromocytoma). Seven CT patients had extra-cardiac diagnoses that explained their symptoms (4 acute pulmonary emboli, 3 pneumonias). MPI led to no non-coronary surgical diagnoses or extra-cardiac explanations of symptoms.
Radiation Doses
CT and MPI dose was available for 184/187 (98%) and 189/189 (100%) patients who received their randomized exam, respectively, (Table 4). The median effective dose was significantly lower for CT [9.6 (IQR 6.2 – 23) milliSieverts] than for MPI [27 (IQR 19 – 27) milliSieverts], (p<0.001). Marked dose reduction trends were noted in both arms over the study period. Through the end of the follow-up period, both CT and MPI patients underwent a median of 3 (IQR 1 – 9) non-cardiac studies involving radiation. The estimated median radiation dose was 2 mSv (IQR 0.003 – 16) for CT and 2 mSv (IQR 0.004 – 17) for MPI.
Table 4.
Estimated Radiation Exposure in milliSieverts
| Measurement | CT (IQR) | MPI (IQR) | P |
|---|---|---|---|
|
Initial assigned non- invasive imaging |
9.6 (6.2 – 23) [n=184] |
27 (19 – 27) [n=189] |
<0.001 |
|
Cardiac imaging over one year |
12 (6.4 – 26) [n=200] |
27 (19 – 27) [n=200] |
<0.001 |
|
Cardiac imaging over complete follow-up |
13 (6.9 –27) [n=200] |
27 (19 – 27) [n=200] |
<0.001 |
|
Non-cardiac imaging studies over complete follow-up |
2.0 (.003 – 16) [n=200] |
2.0 (.004 – 17) [n=200] |
0.91 |
|
All radiation over complete follow-up |
24 (8.7 – 39) [n=200] |
29 (27 – 48) [n=200] |
<0.001 |
CT, coronary computed tomography angiography; IQR, inter-quartile range; MPI, radionuclide stress myocardial perfusion imaging
Subjective patient experience
Subjective patient experience of the imaging exam was assessed in all patients who underwent their randomly assigned study, with complete data available for 186/187 CT and 188/189 MPI patients. The median exam rating scores out of 10 (1 being highest) were 2 (IQR 1 – 3) and 2 (IQR 1 – 3.5) for CT and MPI, respectively (p=0.149). 28 (14%) CT and 45 (23%) MPI patients rated their test less positively with an ordinal score of 5 (descriptor “OK”) or worse (p=0.038). CT patients graded their study more favorably than did MPI patients in comparison to other diagnostic tests (p=0.001) and in willingness to undergo the exam again (p=0.003).
45/186 (24%) CT and 46/188 (24%) MPI patients reported one or more general adverse reactions, most commonly headache, nausea, dizziness and warm feeling. One CT patient and 30 MPI patients complained of chest pain, shortness of breath or palpitations (p<0.001). Three CT patients and no MPI patients complained of rash or pruritus (p=0.25).
177 CT and 180 MPI patients provided information about symptoms at 6 or 12 month telephone interviews. 64 (36%) patients in each arm had continued chest pain, which was the same or worse in 28 CT and 23 MPI patients.
DISCUSSION
This single-center randomized controlled comparative effectiveness trial provides the first direct comparison of CT and MPI in acutely symptomatic, intermediate-risk chest pain patients with intermediate-term follow-up (median 40 months). The present study population – predominately women (63%) and ethnic minorities (95%) of low socioeconomic status and a high incidence of obesity (mean BMI 31) – is understudied and differs from prior randomized trials (14–17). Some studies have compared standard care with early CT (14,17); the present study gave parity to both modalities which were performed at the same place in the treatment algorithm. This study included only patients who clinically required non-invasive imaging unlike the largest Emergency Department CT trials in which many standard care patients received no imaging (16–17).
We found no significant difference between CT and MPI in the primary outcome, cardiac catheterizations not leading to revascularization. The moderate study sample size does limit the ability to detect a small difference between modalities, but the clinical importance of such a difference is uncertain. These data mirror a large retrospective study showing the majority of non-emergent cardiac catheterizations demonstrate no significant disease (31) and suggest that this holds true even for patients pre-screened with currently leading non-invasive imaging. In our exploratory subgroup analysis of patients with significantly abnormal initial imaging, there were non-significantly fewer catheterizations not leading to revascularization in the CT arm (25% vs 52%, p=0.083). The recently published PROMISE trial including 10,000 symptomatic outpatients demonstrates that CT results in a statistically significant, 0.9% reduction in catheterizations showing no obstructive coronary disease as compared to various forms of functional testing (32). The decision to catheterize patients remains dependent on factors other than initial non-invasive imaging, such as clinical presentation, persistence of symptoms, repeated clinical encounters, subsequent testing and clinician and patient preference. These data suggest a small potential benefit of initial CT.
We found no difference between CT and MPI in cardiac catheterizations within one year (15% vs 16%). This differs with research derived from a retrospective review of Medicare claims data (19), a meta-analysis of randomized trials in low risk Emergency Department patients (20) and a large multi-center trial of outpatients (32), all of which showed increased catheterizations after CT. We observed that the time to catheterization was longer for CT than MPI, which is likely a reflection of the desire to avoid potentially nephrotoxic, immediate consecutive administrations of intravenous contrast. We found no significant difference between CT and MPI in percutaneous coronary interventions (4% vs 5.5%) which also differs from the prior studies. Although the reasons for these differences are uncertain, the diverse patient settings (inpatient, Emergency Department, outpatient) could play a role.
We found an increase in coronary artery bypass in the CT versus MPI arm (4% vs 0.5%, p=.068), which is confirmed by a large trial in outpatients showing near doubling of the rate for patients undergoing CT (32). This could be explained by “balanced” ischemia, which is a known limitation of MPI. Alternatively, the increase in coronary bypass in the CT arm could be due to overtreatment since both CT and catheterization demonstrate anatomic stenosis and are more similar to each other than to MPI, a physiological modality. However, if this were the case we would have expected more percutaneous interventions in the CT arm, which we did not observe. Major adverse cardiovascular events were similar between the two groups; similar event rates are also reported in outpatients undergoing CT and functional testing (32). CT led to clinically important non-coronary diagnoses in 10 patients (5%), some of which led to surgery. These would not reasonably have been diagnosed by MPI and represent an advantage of CT.
Length of stay was not meaningfully different between the CT and MPI arms (median 29 vs 30 h), while prior published trials in Emergency Department patients favored CT (14–17). A likely reason for this difference is that patients in the current study were recruited without immediate, dedicated CT availability. In addition, our higher risk patients (with intermediate level criteria for short-term death or myocardial infarction) had a higher incidence of catheterization and revascularization. These interventions were usually performed during the same hospitalization. The speed of an imaging study is highly dependent on local facilities and practice patterns. This limits the generalizability of analysis of length of stay.
Downstream resource utilization including repeat hospitalizations and Emergency Department visits for cardiac and non-cardiac complaints, outpatient cardiologist and primary care visits, non-invasive cardiac imaging and catheterization did not differ between the CT and MPI arms. This is at variance with retrospectively analyzed Medicare claims data (19). New aspirin and statin therapy did not differ significantly between the CT and MPI arms.
Radiation doses for initial imaging were significantly lower for CT than MPI (median 9.6 vs 27 mSv) which decreased but remained highly significant over long-term follow-up when both cardiac and overall imaging was considered (median 24 vs 27 mSv). For comparison purposes, according to an accepted linear extrapolation (28), 10 mSv confers a lifetime risk of fatal cancer induction of 50/100,000 in 60 year old patients. The large reported doses in this study directly reflect the higher radiation Thallium isotope used for imaging most of our patients. Recent trends favor lower dose, sestamibi-only protocols which have been formally adopted at our institution (February, 2011) and elsewhere. Additional recent advances in radiation dose reduction have been achieved with high-efficiency MPI (33) and newer CT scanner technology (34).
Patients rated their non-invasive imaging experience with CT better than with MPI (fewer unfavorable experience ratings), in comparison with other diagnostic tests and greater willingness to undergo the exam again. This correlates with the higher incidence of patient complaints of chest pain, palpitations and shortness of breath with MPI. There was no significant difference between the CT and MPI groups in persistent chest pain; about one third remained symptomatic in each group.
This study has several limitations. Foremost, this was a single center study and institution-specific factors may limit generalizability. However, our majority female, ethnically diverse, low-income population remains understudied. Our sample size is comparable to most prior CT studies and the duration of follow-up is far longer. The current study only included patients who were appropriate candidates for both CT and MPI and did not assess other modalities. Second, the decisions to perform cardiac catheterization and revascularization, the components of our primary outcome, were made clinically without a pre-defined algorithm. The managing physicians were clinically assigned and not blinded. Factors other than initial imaging played a role in treatment decisions, closely resembling real-life practice, which is also not constrained by strict algorithms for management. Third, the identification of clinical events and subsequent resource utilization, including follow-up of incidental findings on CT, is limited to our health system network and follow-up discussions with patients and their physicians. Downstream events at other institutions could be missed as there is no unified system for medical records. This study is underpowered to detect potentially important differences in clinical events and resource utilization. Fourth, major advancements in CT (such as CT-fractional flow reserve (35) and perfusion (36)) and nuclear cardiology (such as positron emission tomography techniques (37), including coronary flow reserve (38)) are continuous and significantly alter the performance characteristics of these modalities over time. Fifth, radiation dose data is based on imaging protocols which have changed over the time of the study and rely on standardized recorded amounts of isotopes. Finally, we observed a greater proportion of patients over age 70 in the CT arm (17% vs 10%), a potential source of bias.
In conclusion, the present study demonstrated no significant difference between initial CT and MPI in catheterization not leading to revascularization, a measure of performance in selecting patients for invasive management. A trend towards more coronary bypass grafting in the CT arm remains of uncertain clinical impact. Length of stay, downstream resource utilization and clinical events also did not differ between the CT and MPI arms in this diverse, inner-city population at intermediate-term follow-up. CT was associated with lower radiation dose and a better patient experience.
Supplementary Material
Acknowledgments
We wish to thank study coordinators Rizwan Aslam, Prameela Banoth, Shimon Farkas, Adina Haramati, Raphael Hulkower, David Kawior, Kristen Launier, Rikah Lerer, Shey Mukundan, Dieudonne Nonga, Paul O’Connor, Danny Nhan, Shayne Sebold, Samantha Selesny, Daniel Sova, Christian Stanton and Shayna Vega. We thank Nina Ackerman for help with analyzing socioeconomic status. We wish to acknowledge the contribution of the study’s Data and Safety Monitoring Board members, Drs. Michael Farkouh, Gregory Pearson, Yungtai Lo, Michelle Johnson and James Godbold. J. Levsky had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Grant Support
This study was supported by American Heart Association Clinical Research Program Grant 0885024D and CTSA Grants 1 UL1 TR001073-01, 1 TL1 TR001072-01, 1 KL2 TR001071-01 from the National Center for Advancing Translational Sciences, a component of the National Institutes of Health.
Footnotes
This is the prepublication, author-produced version of a manuscript accepted for publication in Annals of Internal Medicine. This version does not include post-acceptance editing and formatting. The American College of Physicians, the publisher of Annals of Internal Medicine, is not responsible for the content or presentation of the author-produced accepted version of the manuscript or any version that a third party derives from it. Readers who wish to access the definitive published version of this manuscript and any ancillary material related to this manuscript (e.g., correspondence, corrections, editorials, linked articles) should go to Annals.org or to the print issue in which the article appears. Those who cite this manuscript should cite the published version, as it is the official version of record.
All authors declare no potential conflicts of interest relevant to this manuscript.
ClinicalTrials.gov: NCT007054585
REFERENCES
- 1.Nabel EG, Braunwald E. A tale of coronary artery disease and myocardial infarction. N Engl J Med. 2012;366(1):54–63. doi: 10.1056/NEJMra1112570. [DOI] [PubMed] [Google Scholar]
- 2.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Heart Disease and Stroke Statistics--2014 Update: A Report From the American Heart Association. Circulation. 2014;129(3):e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Amsterdam EA, Kirk JD, Bluemke DA, Diercks D, Farkouh ME, Garvey JL, et al. Testing of low-risk patients presenting to the emergency department with chest pain: a scientific statement from the American Heart Association. Circulation. 2010;122(17):1756–1776. doi: 10.1161/CIR.0b013e3181ec61df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hermann LK, Newman DH, Pleasant WA, Rojanasarntikul D, Lakoff D, Goldberg SA, et al. Yield of routine provocative cardiac testing among patients in an emergency department-based chest pain unit. JAMA Intern Med. 2013;173(12):1128–1133. doi: 10.1001/jamainternmed.2013.850. [DOI] [PubMed] [Google Scholar]
- 5.Hlatky MA, Douglas PS, Cook NL, Wells B, Benjamin EJ, Dickersin K, et al. Future directions for cardiovascular disease comparative effectiveness research: report of a workshop sponsored by the National Heart, Lung, and Blood Institute. J Am Coll Cardiol. 2012;60(7):569–580. doi: 10.1016/j.jacc.2011.12.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Budoff MJ, Dowe D, Jollis JG, Gitter M, Sutherland J, Halamert E, et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol. 2008;52(21):1724–1732. doi: 10.1016/j.jacc.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 7.Miller JM, Rochitte CE, Dewey M, Arbab-Zadeh A, Niinuma H, Gottlieb I, et al. Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med. 2008;359(22):2324–2336. doi: 10.1056/NEJMoa0806576. [DOI] [PubMed] [Google Scholar]
- 8.Meijboom WB, Meijs MF, Schuijf JD, Cramer MJ, Mollet NR, van Mieghem CA, et al. Diagnostic accuracy of 64-slice computed tomography coronary angiography: a prospective, multicenter, multivendor study. J Am Coll Cardiol. 2008;52(25):2135–2144. doi: 10.1016/j.jacc.2008.08.058. [DOI] [PubMed] [Google Scholar]
- 9.Min JK, Dunning A, Lin FY, Achenbach S, Al-Mallah M, Budoff MJ, et al. Age- and sex-related differences in all-cause mortality risk based on coronary computed tomography angiography findings results from the International Multicenter CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter Registry) of 23,854 patients without known coronary artery disease. J Am Coll Cardiol. 2011;58(8):849–860. doi: 10.1016/j.jacc.2011.02.074. [DOI] [PubMed] [Google Scholar]
- 10.Hulten E, Villines TC, Cheezum MK, Berman DS, Dunning A, Achenbach S, et al. Usefulness of coronary computed tomography angiography to predict mortality and myocardial infarction among Caucasian, African and East Asian ethnicities (from the CONFIRM [Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter] Registry) Am J Cardiol. 2013;111(4):479–485. doi: 10.1016/j.amjcard.2012.10.028. [DOI] [PubMed] [Google Scholar]
- 11.Hadamitzky M, Achenbach S, Al-Mallah M, Berman D, Budoff M, Cademartiri F, et al. Optimized prognostic score for coronary computed tomographic angiography: results from the CONFIRM registry (COronary CT Angiography EvaluatioN For Clinical Outcomes: An InteRnational Multicenter Registry) J Am Coll Cardiol. 2013;62(5):468–476. doi: 10.1016/j.jacc.2013.04.064. [DOI] [PubMed] [Google Scholar]
- 12.Shaw LJ, Hausleiter J, Achenbach S, Al-Mallah M, Berman DS, Budoff MJ, et al. Coronary computed tomographic angiography as a gatekeeper to invasive diagnostic and surgical procedures: results from the multicenter CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: an International Multicenter) registry. J Am Coll Cardiol. 2012;60(20):2103–2114. doi: 10.1016/j.jacc.2012.05.062. [DOI] [PubMed] [Google Scholar]
- 13.Min JK, Berman DS, Dunning A, Achenbach S, Al-Mallah M, Budoff MJ, et al. All-cause mortality benefit of coronary revascularization vs. medical therapy in patients without known coronary artery disease undergoing coronary computed tomographic angiography: results from CONFIRM (COronary CT Angiography EvaluatioN For Clinical Outcomes: An InteRnational Multicenter Registry) Eur Heart J. 2012;33(24):3088–3097. doi: 10.1093/eurheartj/ehs315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goldstein JA, Gallagher MJ, O'Neill WW, Ross MA, O'Neil BJ, Raff GL. A randomized controlled trial of multi-slice coronary computed tomography for evaluation of acute chest pain. J Am Coll Cardiol. 2007;49(8):863–871. doi: 10.1016/j.jacc.2006.08.064. [DOI] [PubMed] [Google Scholar]
- 15.Goldstein JA, Chinnaiyan KM, Abidov A, Achenbach S, Berman DS, Hayes SW, et al. The CT-STAT (Coronary Computed Tomographic Angiography for Systematic Triage of Acute Chest Pain Patients to Treatment) trial. J Am Coll Cardiol. 2011;58(14):1414–1422. doi: 10.1016/j.jacc.2011.03.068. [DOI] [PubMed] [Google Scholar]
- 16.Litt HI, Gatsonis C, Snyder B, Singh H, Miller CD, Entrikin DW, et al. CT angiography for safe discharge of patients with possible acute coronary syndromes. N Engl J Med. 2012;366(15):1393–1403. doi: 10.1056/NEJMoa1201163. [DOI] [PubMed] [Google Scholar]
- 17.Hoffmann U, Truong QA, Schoenfeld DA, Chou ET, Woodard PK, Nagurney JT, et al. Coronary CT angiography versus standard evaluation in acute chest pain. N Engl J Med. 2012;367(4):299–308. doi: 10.1056/NEJMoa1201161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Einstein AJ, Henzlova MJ, Rajagopalan S. Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography. JAMA. 2007;298(3):317–323. doi: 10.1001/jama.298.3.317. [DOI] [PubMed] [Google Scholar]
- 19.Shreibati JB, Baker LC, Hlatky MA. Association of coronary CT angiography or stress testing with subsequent utilization and spending among Medicare beneficiaries. JAMA. 2011;306(19):2128–2136. doi: 10.1001/jama.2011.1652. [DOI] [PubMed] [Google Scholar]
- 20.Hulten E, Pickett C, Bittencourt MS, Villines TC, Petrillo S, Di Carli MF, et al. Outcomes after coronary computed tomography angiography in the emergency department: a systematic review and meta-analysis of randomized, controlled trials. J Am Coll Cardiol. 2013;61(8):880–892. doi: 10.1016/j.jacc.2012.11.061. [DOI] [PubMed] [Google Scholar]
- 21.Meinert CL. The inclusion of women in clinical trials. Science. 1995;269(5225):795–796. doi: 10.1126/science.7638594. [DOI] [PubMed] [Google Scholar]
- 22.Harris DJ, Douglas PS. Enrollment of women in cardiovascular clinical trials funded by the National Heart, Lung, and Blood Institute. N Engl J Med. 2000;343(7):475–480. doi: 10.1056/NEJM200008173430706. [DOI] [PubMed] [Google Scholar]
- 23.Zhang T, Tsang W, Wijeysundera HC, Ko DT. Reporting and representation of ethnic minorities in cardiovascular trials: a systematic review. Am Heart J. 2013;166(1):52–57. doi: 10.1016/j.ahj.2013.03.022. [DOI] [PubMed] [Google Scholar]
- 24.Hendel RC, Berman DS, Di Carli MF, Heidenreich PA, Henkin RE, Pellikka PA, et al. ACCF/ASNC/ACR/AHA/ASE/SCCT/ SCMR/SNM 2009 appropriate use criteria for cardiac radionuclide imaging: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the American Society of Nuclear Cardiology, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, and the Society of Nuclear Medicine. Circulation. 2009;119(22):e561–e587. doi: 10.1161/CIRCULATIONAHA.109.192519. [DOI] [PubMed] [Google Scholar]
- 25.Levsky JM, Travin MI, Spevack DM, Menegus MA, Huang PW, Goldberg Y, et al. Rationale and design of a randomized trial comparing stress myocardial perfusion imaging and coronary CT angiography as the initial imaging test for intermediate risk patients admitted with chest pain. J Cardiovasc Comput Tomogr. 2009;3(4):264–271. doi: 10.1016/j.jcct.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 26.Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE, Jr, et al. 2012 ACCF/AHA focused update incorporated into the ACCF/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127(23):e663–e828. doi: 10.1161/CIR.0b013e31828478ac. [DOI] [PubMed] [Google Scholar]
- 27. [Last accessed December 23, 2014];Radiation Dose Assessment Resource (RADAR) Medical Procedure Radiation Dose Calculator at http://www.doseinfo-radar.com/RADARDoseRiskCalc.html.
- 28. [Last accessed December 23, 2014];Radiation Risk Calculator at http://www.xrayrisk.com.
- 29. [Last accessed March 9, 2015];GraphPad QuickCalcs Analyze a 2x2 Contingency Table, Fisher’s Exact Test at http://www.graphpad.com/quickcalcs/contingency1/
- 30. [Last accessed March 9, 2015];The Confidence Interval of a Proportion, 95% Confidence Interval Including Continuity Correction at http://vassarstats.net/prop1.html.
- 31.Patel MR, Peterson ED, Dai D, Brennan JM, Redberg RF, Anderson HV, et al. Low diagnostic yield of elective coronary angiography. N Engl J Med. 2010;362(10):886–895. doi: 10.1056/NEJMoa0907272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Douglas PS, Hoffmann U, Patel MR, Mark DB, Al-Khalidi HR, Cavanaugh B, et al. Outcomes of Anatomical versus Functional Testing for Coronary Artery Disease. N Engl J Med. 2015 Mar 14; doi: 10.1056/NEJMoa1415516. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Duvall WL, Savino JA, Levine EJ, Baber U, Lin JT, Einstein AJ, et al. A comparison of coronary CTA and stress testing using high-efficiency SPECT MPI for the evaluation of chest pain in the emergency department. J Nucl Cardiol. 2014;21(2):305–318. doi: 10.1007/s12350-013-9823-y. [DOI] [PubMed] [Google Scholar]
- 34.Chen MY, Shanbhag SM, Arai AE. Submillisievert median radiation dose for coronary angiography with a second-generation 320-detector row CT scanner in 107 consecutive patients. Radiology. 2013;267(1):76–85. doi: 10.1148/radiol.13122621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Min JK, Leipsic J, Pencina MJ, Berman DS, Koo BK, van Mieghem C, et al. Diagnostic accuracy of fractional flow reserve from anatomic CT angiography. JAMA. 2012;308(12):1237–1245. doi: 10.1001/2012.jama.11274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rochitte CE, George RT, Chen MY, Arbab-Zadeh A, Dewey M, Miller JM, et al. Computed tomography angiography and perfusion to assess coronary artery stenosis causing perfusion defects by single photon emission computed tomography: the CORE320 study. Eur Heart J. 2014;35(17):1120–1130. doi: 10.1093/eurheartj/eht488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mc Ardle BA, Dowsley TF, deKemp RA, Wells GA, Beanlands RS. Does rubidium-82 PET have superior accuracy to SPECT perfusion imaging for the diagnosis of obstructive coronary disease?: A systematic review and meta-analysis. J Am Coll Cardiol. 2012;60(18):1828–1837. doi: 10.1016/j.jacc.2012.07.038. [DOI] [PubMed] [Google Scholar]
- 38.Murthy VL, Naya M, Foster CR, Hainer J, Gaber M, Di Carli G, et al. Improved cardiac risk assessment with noninvasive measures of coronary flow reserve. Circulation. 2011;124(20):2215–2224. doi: 10.1161/CIRCULATIONAHA.111.050427. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.