Abstract
Infection due to Chromobacterium violaceum is rare. Diagnosis may be delayed since Chromobacterium sepsis may mimic melioidosis, especially in melioidosis-endemic areas. Management of Chromobacterium infection is challenging given the propensity of this pathogen to cause visceral abscesses, drug resistance, and relapse. Mortality rates are high despite treatment. We report a case of C. violaceum septicemia in an immunocompetent adult from south India, who was successfully treated with combination antibiotic therapy. Physicians in tropical and subtropical regions must be aware of C. violaceum infection as it can mimic melioidosis.
Introduction
Chromobacterium violaceum is an aerobic, gram-negative saprophytic bacillus found in soil and water. First reported in 1927, human infection with C. violaceum is rare.1,2 Most cases of C. violaceum occur in tropical and subtropical areas of Asia, Africa, South America, Australia, and southeastern United States.3 Diagnosis may be delayed since Chromobacterium sepsis may mimic melioidosis, especially in melioidosis-endemic areas.4 Management of Chromobacterium infection is challenging given the propensity of this pathogen to cause visceral abscesses, drug resistance, and relapse. Mortality rates are high (∼55%) despite treatment.3 We report a case of C. violaceum septicemia in an immunocompetent adult who was successfully treated with combination antibiotic therapy.
Case Report
In October 2013, a previously healthy 53-year-old lady from south India presented with a 5-day history of fever, abdominal pain, and vomiting. Two weeks before presentation, while working at a waterlogged farm, she sustained trauma to her left leg. She could not recall the precise details of her limb injury. The wound was complicated by an abscess necessitating incision and drainage by her family physician. Our patient did not have diabetes mellitus or any other comorbidities.
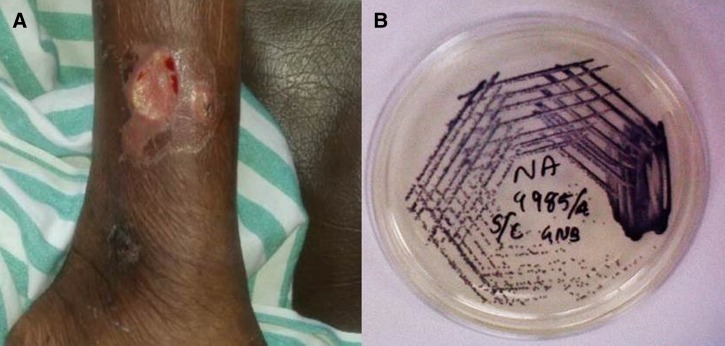
On admission, she was ill-appearing with a temperature of 101°F, pulse rate of 112 beats/minute, respiratory rate of 22 breaths/minute, oxygen saturation of 93% on room air, and blood pressure of 130/80 mmHg. Examination revealed scleral icterus, bilateral crackles, tender hepatomegaly, and an ulcerative skin lesion with surrounding cellulitis on her left leg (Figure 1A ).
Figure 1.
(A) Ulcerative skin lesion. (B) Nutrient agar showing colonies of Chromobacterium violaceum.
Laboratory investigations showed anemia, leukocytosis (white blood cell [WBC] count 22.9 × 109 cells/L with 85% neutrophils), normal platelet count, and elevated erythrocyte sedimentation rate (ESR; 103 mm/hour). Liver function tests revealed hypoalbuminemia and cholestatic hepatitis (total bilirubin 61.56 μmol/L [normal 5.13–20.52 μmol/L], direct bilirubin 58.14 μmol/L [normal 3.42 μmol/L], aspartate aminotransferase 0.71 μkat/L [normal 0.09–0.68 μkat/L], alanine aminotransferase 1.02 μkat/L [normal 0.09–0.68 μkat/L], and alkaline phosphatase 3.40 μkat/L [normal 0.68–2.19 μkat/L]). Chest radiograph showed bilateral infiltrates. Abdominal computed tomography scan revealed multiple hepatic abscesses. On admission, she developed respiratory distress requiring oxygen supplementation. We suspected septicemic melioidosis, and she was started on intravenous imipenem (0.5 g three times daily).
A gram-negative bacillus grew on both blood and wound cultures, which was identified as C. violaceum based on the characteristic morphology of round, smooth colonies with a dark violet pigmentation on blood, chocolate, and MacConkey agar plates. The isolate was subcultured on to nutrient agar for better appreciation of the nondiffusible violet pigment (Figure 1B). Identification was confirmed by conventional biochemical reactions and by the Vitek 2 Compact System (bioMerieux, Marcy l'Etoile, France). The isolate was sensitive to imipenem, meropenem, ciprofloxacin, aminoglycosides, trimethoprim–sulfamethoxazole, piperacillin–tazobactam, and cefaperazone–sulbactam but resistant to ampicillin, cefuroxime, cefotaxime, and ceftazidime.
Ciprofloxacin (500 mg orally every 12 hours) was added to imipenem regimen on hospital day 3. She remained hemodynamically stable but fever persisted with marked leukocytosis (WBC 47.1 × 109 cells/L) on day 5. At this point, intravenous piperacillin–tazobactam (4.5 g three times daily) was added to regimen of imipenem and ciprofloxacin. She improved slowly and became afebrile with negative blood culture on day 8. Piperacillin–tazobactam was administered for 10 days but imipenem and ciprofloxacin was continued. By day 21, WBC normalized, ESR decreased (40 mm/hour), and jaundice and hepatitis had resolved. On day 28, she was discharged on oral ciprofloxacin for 3 months. Follow-up ultrasound showed complete resolution of hepatic lesions. When last seen at follow-up in January 2015, the patient was well.
Discussion
Infection due to C. violaceum is unusual.3 The review of the literature revealed only six cases of Chromobacterium infection in adults from India.5–10 Among them only two case reports have documented C. violaceum septicemia.5,9 The outcome was fatal in one case,5 but unknown in the other case.9
Infection often occurs after skin injury in association with exposure to contaminated soil or water. Other risk factors for infection include young age, neutrophil dysfunction, and chronic granulomatous disease.3 C. violaceum infection frequently presents with localized cutaneous infection followed by sepsis and multiple abscesses in lungs, spleen, or liver with high mortality.3
Diagnosis requires isolation of the organism from wound or blood cultures. The organism grows on blood and MacConkey agar producing deep purple pigment (violacein). The organism is usually susceptible to fluoroquinolones, carbapenems, aminoglycosides, chloramphenicol, trimethoprim–sulfamethoxazole, or tetracyclines, but resistant to penicillin and cephalosporins.3 Anecdotal data suggest improved survival rates when combination antimicrobial therapy is used.3,11 In our patient, we added a third agent, piperacillin–tazobactam because of concerns of disease progression while receiving imipenem/ciprofloxacin regimen; however, the additional benefit of piperacillin–tazobactam is unclear. Combination antimicrobial therapy with a carbapenem and a quinolone appears to be a good option.3 Prolonged maintenance therapy with an oral antibiotic is needed to prevent recurrence.3
Our patient had history of trauma to her left leg while working in the farm after which she developed an ulcer on her leg and multiple liver abscesses. We initially suspected a septicemic form of melioidosis, another serious tropical infection commonly seen in our region.4 The diagnosis of C. violaceum was made in our patient on the basis of isolation of the organism from the wound and blood.
Physicians in tropical and subtropical regions must be aware of C. violaceum infection as it can mimic melioidosis. Combination antimicrobial therapy with appropriate antibiotics can reduce mortality.
Footnotes
Authors' addresses: Deepak R. Madi and John Ramapuram, Department of Medicine, Kasturba Medical College, Karnataka, India, E-mails: deepakmadi1234@gmail.com and john.ramapuram@manipal.edu. K. Vidyalakshmi, Department of Microbiology, Kasturba Medical College, Karnataka, India, E-mail: k.vidyalakshmi@lycos.com. Avinash K. Shetty, Department of Pediatrics, Wake Forest School of Medicine, Winston-Salem, NC, E-mail: ashetty@wakehealth.edu.
References
- 1.Sneath PHA, Whelan JPF, Singh RB, Edwards D. Fatal infection by Chromobacterium violaceum. Lancet. 1953;2:276–277. doi: 10.1016/s0140-6736(53)91132-5. [DOI] [PubMed] [Google Scholar]
- 2.Jitmuang A. Human Chromobacterium violaceum infection in southeast Asia: case reports and literature review. Southeast Asian J Trop Med Public Health. 2008;39:452–460. [PubMed] [Google Scholar]
- 3.Yang CH, Li YH. Chromobacterium violaceum infection: a clinical review of an important but neglected infection. J Chin Med Assoc. 2011;74:435–441. doi: 10.1016/j.jcma.2011.08.013. [DOI] [PubMed] [Google Scholar]
- 4.Vidyalakshmi K, Lipika S, Vishal S, Damodar S, Chakrapani M. Emerging clinico-epidemiological trends in melioidosis: analysis of 95 cases from western coastal India. Int J Infect Dis. 2012;16:e491–e497. doi: 10.1016/j.ijid.2012.02.012. [DOI] [PubMed] [Google Scholar]
- 5.Karthik R, Pancharatnam P, Balaji V. Fatal Chromobacterium violaceum septicemia in a south Indian adult. J Infect Dev Ctries. 2012;6:751–755. doi: 10.3855/jidc.1866. [DOI] [PubMed] [Google Scholar]
- 6.Mahapatra A, Roy D, Poddar N, Panda R, Sarangi G, Mallick B, Chayani N. Chromobacterium violaceum: a case report of an unusual bacterium causing puerperal sepsis. Indian J Pathol Microbiol. 2006;49:450–452. [PubMed] [Google Scholar]
- 7.Dutta S, Dutta SK. Multidrug resistant Chromobacterium violaceum: an unusual bacterium causing long standing wound abscess. Indian J Med Microbiol. 2003;21:217–218. [PubMed] [Google Scholar]
- 8.Kumar MR. Chromobacterium violaceum: a rare bacterium isolated from a wound over the scalp. Int J Appl Basic Med Res. 2012;2:70–72. doi: 10.4103/2229-516X.96814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rai R, Karnaker VK, Shetty V, Krishnaprasad MS. Chromobacterium violaceum septicaemia—a case report. Am J Med Sci. 2011;4:201–203. [Google Scholar]
- 10.Swain B, Otta S, Sahu KK, Panda K, Rout S. Urinary tract infection by Chromobacterium violaceum. J Clin Diagn Res. 2014;8:8. doi: 10.7860/JCDR/2014/9230.4703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Campbell JI, Lan NP, Qui PT, Dung LT, Farrar JJ, Baker S. A successful antimicrobial regime for Chromobacterium violaceum induced bacteremia. BMC Infect Dis. 2013;13:4. doi: 10.1186/1471-2334-13-4. [DOI] [PMC free article] [PubMed] [Google Scholar]