Abstract
Monitoring Wuchereria bancrofti infection in mosquitoes (xenomonitoring) can play an important role in determining when lymphatic filariasis has been eliminated, or in focusing control efforts. As mosquito infection rates can be low, a method for collecting large numbers of mosquitoes is necessary. Gravid traps collected large numbers of Culex quinquefasciatus in Tanzania, and a collection method that targets mosquitoes that have already fed could result in increased sensitivity in detecting W. bancrofti-infected mosquitoes. The aim of this experiment was to test this hypothesis by comparing U.S. Centers for Disease Control and Prevention (CDC) light traps with CDC gravid traps in northeastern Tanzania, where Cx. quinquefasciatus is a vector of lymphatic filariasis. After an initial study where small numbers of mosquitoes were collected, a second study collected 16,316 Cx. quinquefasciatus in 60 gravid trap-nights and 240 light trap-nights. Mosquitoes were pooled and tested for presence of W. bancrofti DNA. Light and gravid traps collected similar numbers of mosquitoes per trap-night, but the physiological status of the mosquitoes was different. The estimated infection rate in mosquitoes collected in light traps was considerably higher than in mosquitoes collected in gravid traps, so light traps can be a useful tool for xenomonitoring work in Tanzania.
Introduction
Lymphatic filariasis (LF) is a disease that, though not fatal, can cause serious health problems. Approximately 40 million people worldwide experience lymphedema, elephantiasis, or urogenital disorders as a consequence of LF infection.1 Because of several features of this disease, including the lack of an animal reservoir and the availability of safe and effective drugs, LF was targeted for elimination as a public health problem in 1997.2 Elimination of LF is based on repeated distribution of anthelmintic drugs, treatment of existing cases, and vector control, where appropriate.3
To ensure the progress of LF control efforts and to certify elimination, effective monitoring programs must be put in place. Monitoring can be done in one of two ways. First, human blood can be tested for the presence of the parasite. The testing of blood has been facilitated with the development of rapid diagnostic tests.4 Second, mosquitoes can be collected and tested (xenomonitoring), either through dissection to find the filarial larvae, or through the use of molecular methods to detect the DNA of the filarial worms.5
Light traps are commonly used for the collection of mosquitoes for LF xenomonitoring,6–8 and are usually placed indoors near a sleeping person who is protected with an untreated mosquito net. Other methods such as human landing catches have been used,9 but this method is used less often due to ethical concerns.10
Gravid traps have been used for the collection of mosquitoes for xenomonitoring, particularly in the United States for monitoring of Western Equine, St. Louis, and West Nile viruses.11–13 Gravid traps provide oviposition cues and preferentially collect gravid mosquitoes approaching the organic infusion in the pan below the trap. As gravid mosquitoes have typically fed at least once, it is expected that there is a greater chance of collecting infected mosquitoes. Reports have indicated that infection rates in mosquitoes collected in gravid traps was 33 times higher than in mosquitoes collected in dry-ice baited light traps in Delaware.14 A similar trend was found in New York, where infection rates in mosquitoes collected with gravid traps were 5.7 times higher than in mosquitoes from light traps.15 Muturi and others16 used gravid traps in a rice-growing area in Mwea, Kenya, and found that the traps collected several of the primary vectors of Wuchereria bancrofti in Africa, namely, Anopheles arabiensis, Anopheles funestus, and the most numerous in the traps, Culex quinquefasciatus. Similarly, Irish and others17 collected over 400 female Cx. quinquefasciatus per trap-night in gravid traps in Ifakara, Tanzania.
The studies described here aimed to compare gravid traps with light traps in an area endemic for LF, both in terms of the numbers of mosquitoes collected and the proportion of mosquitoes infected with W. bancrofti. An initial study was conducted at the end of the rainy season (September–October 2011). Because of the fairly small numbers of mosquitoes collected, a second study was conducted during the subsequent rainy season (June–July 2012).
Materials and Methods
Study sites.
Both the initial study and the secondary study were conducted in Tanga region. The initial study was performed in Masaika and the secondary study was conducted in Vyeru (Figure 1 ). Masaika is a village of approximately 1,000 inhabitants (S 05.27659, E 38.85017). It is primarily a village of subsistence farmers and has rainy seasons in March–June (heavy rains) and October–November (light rains).18,19 A detailed description of the village is provided by Rwegoshora and others.7 In this village, 12 households were recruited for mosquito trapping that was conducted from September 6 to October 14, 2011. Vyeru is a village on Manza Bay (S 04.95754, E 39.13483). The seasons are similar to Masaika, and fishing and subsistence agriculture are both practiced by inhabitants of this village. From this village 10 houses were selected and trapping was conducted between June 27 and July 31, 2012.
Figure 1.
A map of northeastern Tanzania showing the study villages Masaika and Vyeru.
In both locations, village leaders were consulted to see if the study would be acceptable. Once their approval was gained, homeowners were approached to see if they would be willing to participate in the study. The locations of consenting households were measured using a GPS unit (Garmin Ltd., Southampton, United Kingdom) to ensure that all participating households were at least 50 m from each other. As a condition of ethical clearance (LSHTM no. 5966, NIMR no. 1242), participating households were given long-lasting insecticide-treated bed nets (Olyset Net; Net Health Ltd., Arusha, Tanzania) before the trial.
Collection methods.
The model of light trap used, the U.S. Centers for Disease Control and Prevention (CDC) light trap (Bioquip Products, Inc., Rancho Dominguez, CA), was selected because it is the same model used by the study monitoring the Tanzanian National Lymphatic Filariasis Elimination Program to collect mosquitoes for xenomonitoring. Light traps were placed indoors and were hung from rafters next to the beds.
The gravid traps used were CDC gravid traps (John W. Hock Co., Gainesville, FL), which were shown to be the most effective model for collecting Cx. quinquefasciatus in a previous trial.17 The traps were run on 6 V batteries, which were placed inside the house for security, while the trap was placed outside the house under the eaves. The wire connecting the trap to the battery was passed through the door frame or a small hole in the wall (Figure 2 ).
Figure 2.
A gravid trap placed outside a house in Masaika, Tanzania.
Grass infusion was prepared by soaking grass in water for 2 days (approximately 4–5 g of grass per liter). While soaking the grass, the plastic bin was covered to prevent any mosquito oviposition. The grass was strained from the infusion using a sieve before it was added to the gravid traps. Of the grass infusion, 4 L was used per gravid trap.
Study design.
The initial study involved 12 households in Masaika at the end of the rainy season in 2011. Each night 10 light traps and two gravid traps were set at the 12 households, with one trap set at each house. Only two gravid traps were used because of the large numbers of Cx. quinquefasciatus, based on collections from previous experiments.17 The position of the traps was determined using a randomized Latin square design. The traps were set twice weekly for 6 weeks, resulting in 24 trap-nights for the gravid traps, and 120 trap-nights for the light traps.
In Vyeru, the study was conducted during the rainy season to increase total catch and better determine the difference between the two collection methods. Eight light traps and two gravid traps were set each night over 30 nights, resulting in 240 trap-nights for light traps and 60 trap-nights for gravid traps.
In both studies, traps were set between 5:00 and 7:00 pm and were collected the following morning between 06:00 and 07:30 am. Trap nets were returned to the laboratory and collected mosquitoes were killed in a −20°C freezer. Mosquitoes were identified to species, using available keys.20–23 After identification, mosquitoes were individually placed in Eppendorf tubes (1.5 mL). Each tube contained a small amount of anhydrous calcium sulfate (W. A. Hammond Drierite Company Ltd., Xenia, OH), topped with cotton wool, to prevent the growth of mold. Any nights in which either the trap battery/trap failed or ants were present in the trap were discounted and not included in the final analysis.
Detection of W. bancrofti in collected mosquitoes.
Female Cx. quinquefasciatus mosquitoes from Masaika were tested individually for the presence of W. bancrofti DNA using the method of Chambers and others,24 with the exception that BlueJuice loading buffer (Invitrogen, Carlsbad, CA) and ethidium bromide were used instead of GelRed (Biotium, Hayward, CA). In brief, DNA extractions using the Qiagen DNeasy Kit (Qiagen N.V., Venlo, The Netherlands) involved homogenizing the individual mosquitoes in 200 μL of phosphate-buffered saline. The AL buffer (200 μL) and 20 μL of proteinase K were added, and the homogenate incubated at 70°C for 10 minutes. An additional 20 μL of proteinase K was then added followed by incubation at 56°C for 1 hour. This was then followed by a centrifugation 14,500 g for 5 minutes to pellet the mosquito debris. The supernatant was transferred into new Eppendorf tube and mixed with 200 μL of 98% ethanol, and the entire sample loaded into DNeasy mini column. This was followed by centrifugation at 9,000 g for 1 minute where DNA bound to the DNeasy column membrane and other materials passed through. The DNA was then washed three times using two grade washing buffers to remove any contaminants, and thereafter eluted with 250 mL of elution buffer and stored at −20°C until used for polymerase chain reaction (PCR) amplifications.
Positive samples were retested to confirm presence of W. bancrofti DNA. Each run contained a negative control (double distilled water) and a positive control (DNA extract from mosquitoes fed on a patient with LF, previously tested positive for microfilaremia).
As the numbers of Cx. quinquefasciatus females from Vyeru were considerably higher than those from Masaika, mosquitoes were pooled in groups of 25 before DNA extraction. The same extraction method that was used for the individual mosquitoes from Masaika was used for the pools from Vyeru. Females of all physiological stages were used in the pools. Because of limited reagents, a subsample of pools to be tested was selected using a random number generator. The Anopheles mosquitoes were tested individually. The DNA was extracted in the same manner as the mosquitoes from Masaika, but was screened using quantitative PCR with Roche short hydrolysis universal probes (Roche Applied Science, Penzberg, Germany) substituted with locked nucleic acids, which allow greater specificity than standard PCR. Probes and corresponding primers were designed using the Roche ProbeFinder software to amplify genes to detect W. bancrofti (GenBank accession no. AY297458), Cx. quinquefasciatus (GenBank accession no. L34351.1), and the endosymbiotic bacterium of Cx. quinquefasciatus, Wolbachia pipientis wPip strain (GenBank accession no. AF020061.1). Synthetic long oligonucleotides of the amplified product were generated and 10-fold serial dilutions were carried out to produce a standard curve of gene copies per microliter for all genes assayed. Ten microliter PCR reactions containing 0.5 μM forward and reverse primers and 0.1 μM hydrolysis probe (final concentrations) were added to Roche FastStart essential DNA probes master mix. A Roche LightCycler 96 System was used to first preincubate the reactions at 95°C for 5 minutes, followed by 45 cycles of 60°C for 30 seconds and 95°C for 10 seconds. Two independent assays were run each with three replicates/sample and assays and included negative (no template) and positive controls. Wuchereria bancrofti infection levels were normalized to the host Cx. quinquefasciatus gene to generate a mean Wuchereria:Culex gene ratio for each DNA extract.
Statistical analysis.
The numbers of female Cx. quinquefasciatus collected per trap-night were checked for normality. If the data followed a negative binomial distribution, a negative binomial regression model was used to compare the means. The trap day, trap location, and trap type were tested using univariate analyses. Those having an effect on the numbers of female Cx. quinquefasciatus collected at the 10% level (P < 0.1), as tested using Wald tests, were retained for multivariable analysis. The final model included all variables significant at the 5% level (P < 0.05) when adjusted for other factors. All analyses were conducted using Stata 11.0 (Stata Corporation, College Station, TX).
For comparisons of the infection rates in individually analyzed female Cx. quinquefasciatus from Masaika and Anopheles gambiae from Vyeru, χ2 tests were used. As the numbers of infected mosquitoes were low, Fisher exact tests were used. For pooled Culex mosquitoes from Vyeru, infection rates were calculated using Poolscreen 2.0 software (Department of Biostatistics and Division of Geographic Medicine, University of Alabama at Birmingham, AL), providing maximum likelihood estimates for the rate of infection.25
Results
First study at the end of the rainy season in Masaika.
Over the course of the trial, 418 mosquitoes were collected. As some of the mosquitoes were damaged by the fans in the traps, a mosquito was counted if the thorax was present (which excludes excised heads and abdomens). Mosquitoes collected are shown in Table 1. Culex quinquefasciatus was the only LF vector collected in any of the traps. No Anopheles mosquitoes were collected. The median numbers of female Cx. quinquefasciatus and Cx. cinereus from the two types of trap are shown in Table 2. Of the 150 female Cx. quinquefasciatus collected in the gravid traps, 121 (81%) were gravid. Of the 12 female Cx. quinquefasciatus collected in light traps, three (25%) were gravid.
Table 1.
Species of mosquito collected in CDC light traps and CDC gravid traps in Masaika (September–October 2011) and Vyeru (June–July 2012), northeastern Tanzania
| Species | Masaika | Vyeru | ||
|---|---|---|---|---|
| Light (N = 120) | Gravid (N = 24) | Light (N = 207) | Gravid (N = 56) | |
| Culex quinquefasciatus | 12 | 150 | 12,650 | 3,666 |
| Culex cinereus | 40 | 173 | 14 | 2 |
| Mansonia uniformis | 1 | 0 | 40 | 8 |
| Lutzia tigripes | 1 | 1 | 11 | 17 |
| Mansonia africana | 1 | 0 | 16 | 2 |
| Anopheles gambiae s.l. | 0 | 0 | 12 | 0 |
| Culex macfiei | 0 | 0 | 0 | 9 |
| Culex univitattus | 0 | 0 | 8 | 0 |
| Culex decens | 1 | 2 | 3 | 1 |
| Culex poicilipes | 0 | 0 | 3 | 1 |
| Culex vansomereni | 0 | 0 | 2 | 0 |
| Stegomyia spp. | 0 | 0 | 1 | 1 |
| Coquillettidia metallica | 0 | 0 | 2 | 0 |
| Stegomyia aegypti | 1 | 1 | 0 | 0 |
| Culex bitaeniorhynchus | 0 | 0 | 1 | 0 |
| Culex thalassius | 0 | 0 | 1 | 0 |
| Mimomyia mimomyiaformis | 1 | 0 | 0 | 0 |
| Culex nebulosus | 0 | 1 | 0 | 0 |
| Culex insignis | 1 | 0 | 0 | 0 |
| Unidentified | 6 | 25 | 0 | 0 |
CDC = U.S. Centers for Disease Control and Prevention.
Table 2.
Total, median, IQR, and range of female Culex quinquefasciatus and Culex cinereus from gravid and light traps in Masaika, Tanga, Tanzania, which were set twice weekly in 12 houses between September 6 and October 14, 2011
| n | Cx. quinquefasciatus | Cx. cinereus | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Median | IQR | Range | Total | Median | IQR | Range | ||
| Light traps | 120 | 12 | 0 | 0–0 | 0–2 | 40 | 0 | 0–0 | 0–6 |
| Gravid traps | 24 | 150 | 5 | 1–8.5 | 1–19 | 173 | 0 | 0–5.5 | 0–66 |
IQR = interquartile range.
The numbers of females of Cx. quinquefasciatus were not distributed normally, so a negative binomial regression model was used to analyze the data. The trap day and trap type were retained in the final model. The gravid traps collected significantly more female Cx. quinquefasciatus than the light traps (z = 10.70, P < 0.001).
Molecular methods were used to test for the presence of W. bancrofti DNA. All of the female Cx. quinquefasciatus mosquitoes were tested. Two Cx. quinquefasciatus specimens tested positive for W. bancrofti were collected using gravid traps. Of the W. bancrofti positive Cx. quinquefasciatus, one of the mosquitoes was unfed at the time of collection, the other was gravid. Since only 150 Cx. quinquefasciatus from gravid traps were tested, this resulted in an infection rate of 1.3%.
Second study during the rainy season in Vyeru.
During the study conducted in Vyeru in the rainy season, 16,471 intact female mosquitoes were collected from light and gravid traps (Table 1). The Cx. quinquefasciatus were further separated by physiological status. As is shown in Table 3, the majority of Cx. quinquefasciatus collected in light traps were unfed, while the majority of Cx. quinquefasciatus collected in gravid traps were gravid.
Table 3.
Median and IQR of female Culex quinquefasciatus collected in light and gravid traps in Vyeru, Tanzania, showing physiological stage of collected mosquitoes and total numbers
| Light trap (N = 207) | Gravid trap (N = 56) | |||
|---|---|---|---|---|
| Median | IQR | Median | IQR | |
| Unfed | 36 | 17–68 | 2 | 1–4 |
| Blood-fed | 3 | 1–6 | 0 | 0–0 |
| Semigravid | 0 | 0–1 | 0 | 0–0 |
| Gravid | 3 | 1–7 | 53.5 | 32–80 |
| Total | 44 | 24–84 | 57 | 35.5–83.5 |
IQR = interquartile range.
The total numbers of Cx. quinquefasciatus collected in the two trap types were compared using a negative binomial regression model that included whether it had rained, the house where collections were made, and the trap type. The total collections of Cx. quinquefasciatus in the two trap types were not significantly different (z = 1.19, P = 0.23).
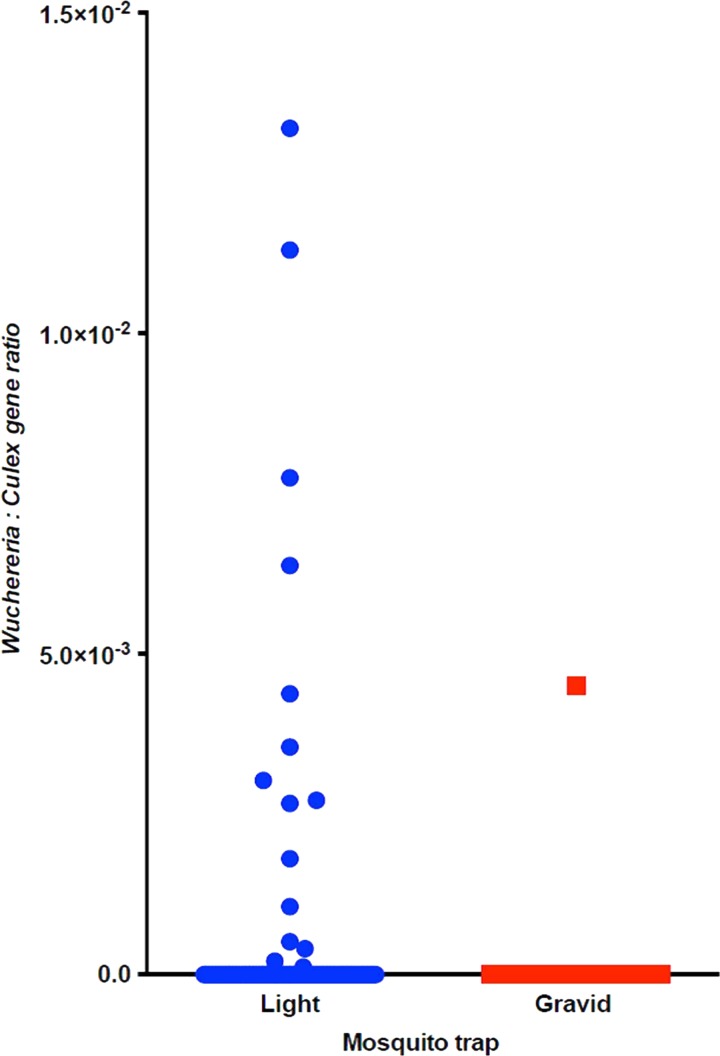
A total of 110 pools of 25 female Cx. quinquefasciatus from light traps and 113 pools of 25 female Cx. quinquefasciatus from gravid traps were tested for the presence of W. bancrofti DNA using quantitative PCR. Of the pools from light traps, 15 tested positive, while only one of the pools from gravid traps tested positive (Figure 3 ). Using the maximum likelihood estimates, 0.6% (0.31–0.99%) of Cx. quinquefasciatus would be expected to be positive for presence of W. bancrofti in mosquitoes from light traps, while only 0.03% (0.001–0.2%) of mosquitoes collected in gravid traps would be expected to be positive. All samples were positive for the endosymbiotic bacterium W. pipientis wPip strain, native to Cx. quinquefasciatus, confirming the mosquito species status. Pooling 25 mosquitoes for each DNA extract prevented a quantitative comparison of Wuchereria infection levels in individual mosquitoes from the two types of traps. However, statistical analysis using a χ2 test to compare the two infection rates, revealed a significant difference between the types of traps (P = 0.0004).
Figure 3.
Wuchereria bancrofti infection levels using quantitative polymerase chain reaction (qPCR) in pooled Culex quinquefasciatus DNA extracts collected from light (blue) and gravid (red) traps in Vyeru, Tanga Region of northeastern Tanzania. Roche universal probes and associated primers were used to detect Wuchereria infection levels, which were normalized to detected levels of a Cx. quinquefasciatus host gene.
None of the Anopheles tested positive for the presence of W. bancrofti DNA.
Discussion
This study conducted two similar studies in the Tanga region of Tanzania, where both Anopheles and Culex vectors are involved in transmission of W. bancrofti.18 In these studies, the primary outcomes measured were the numbers of mosquitoes collected and the proportion of mosquitoes infected.
In Masaika, significantly more Cx. quinquefasciatus were collected in gravid traps, whereas in Vyeru, the numbers collected in light and gravid traps were not significantly different. One of the potential reasons for this difference in results is the seasons in which collections were conducted. In Masaika, collections were made at the end of the rainy season, and rain did fall over the course of the study. As gravid traps attract mosquitoes by presenting potential breeding sites, their attractiveness may be decreased when alternative sites are present. Therefore, gravid traps might be more attractive during the dry season, when fewer mosquitoes are present and fewer breeding sites are available to gravid mosquitoes. The study in Vyeru was conducted during the rainy season, when many natural oviposition sites were available. The number of breeding sites available might have reduced the attractiveness of (and therefore the number collected in) gravid traps. These effects might also be affected by the difference in study site.
Another important factor to take into consideration is the difference in position of the two traps. The light traps were located indoors, next to the beds where humans were sleeping. The gravid traps were placed outdoors, under the eaves of the house. There are two reasons why this may have affected the numbers of mosquitoes collected. The first is the fact that pyrethroid-treated nets were distributed before the collection of mosquitoes, as required for ethical approval. Long-lasting Olyset nets have been shown to have an effect on the numbers of mosquitoes entering a house.26 However, Magbity and others27 found that numbers of An. gambiae s.s. collected in CDC light traps next to treated and untreated nets were not significantly different. Furthermore, although nets were distributed, it was clear from observations while setting the traps that not all nets were being used. Second, although in most cases, because of the small size of most of the houses used, the distance between the locations used for the two types of traps was not more than 5 m, the two traps were nevertheless placed in different climatic conditions, which may have affected the trap catches. This is acceptable, because the goal of this project was not to compare the trap efficacy as such, but rather their potential for xenomonitoring in a typical surveillance program.
A difference in infection rates was not found in Masaika, although infected mosquitoes were only found in gravid traps. However, with only 12 mosquitoes collected in light traps tested, it was not possible to determine whether the infection rates of mosquitoes collected with each method were different. In Vyeru, however, large numbers of mosquitoes were pooled and a significantly higher proportion of pools from light traps tested positive for W. bancrofti DNA than in pools from gravid traps.
The initial hypothesis of this study was that as gravid traps collect greater numbers of mosquitoes that have had at least one blood meal, a greater number of infected mosquitoes would be found in gravid traps. Although it is difficult to explain why there were more infected mosquitoes in pools from light traps, there are a few potential explanations. First, blood-fed mosquitoes were included in pools from both traps, but considerably higher numbers of blood-fed mosquitoes were collected with light traps. The presence of microfilariae in an undigested infective blood meal could result in a positive pool. In a comparison of infection rates between Anopheles punctulatus collected using light traps and human landing catches in Papua New Guinea, it was proposed that infection rates were higher in light trap catches because of the increased proportion of blood-fed mosquitoes in light trap catches.6 This presents an important question for xenomonitoring in general: how representative is a PCR-positive mosquito of W. bancrofti prevalence in a community? On one hand, if the xenomonitoring is intended to show whether transmission is possible in a community, the presence of a positive mosquito indicates that a mosquito has taken a blood meal from microfilaremic human in the immediate vicinity. On the other hand, it is considerably more difficult to estimate the prevalence in an entire community based on light traps that are placed in houses of individuals, who may or may not be infective to mosquitoes. Second, the fact that gravid traps were placed outdoors may result in collecting a more representative sample of all mosquitoes in a community, as mosquitoes entering the trap may have exited multiple houses, or bit people in multiple locations. However, Cx. quinquefasciatus are not exclusively anthropophilic,28 so gravid traps may include mosquitoes that have fed on birds or other animals, thereby decreasing the likelihood of infection. Sampling from inside houses may increase the likelihood of collecting anthropophilic mosquitoes. As W. bancrofti is only present in humans, any trapping bias toward anthropophilic mosquitoes is likely to result in an increased chance of collecting PCR-positive mosquitoes.
Culex quinquefasciatus are not the only vectors of W. bancrofti in Tanzania. Anopheles gambiae and An. funestus have also been found to play an important role in transmission.18 However, gravid traps baited with grass infusion are considerably less effective in collecting Anopheles mosquitoes than light traps.16 Depending on the local vectors of filariasis, light traps may be a more valuable sampling method, as they can collect not only Cx. quinquefasciatus that are more likely to be infected (as in this study), but also higher numbers of Anopheles vectors. However, even in Tanzania, where Anopheles vectors transmit the larvae of W. bancrofti, the importance of Cx. quinquefasciatus is increasing.8 The proportion of microfilariae ingested by Cx. quinquefasciatus that reach the infective L3 stage increases with declining numbers of microfilariae ingested (limitation), whereas the opposite is true for Anopheles vectors (facilitation).29 As mass drug administration reduces microfilarial intensity,30 it is likely that Cx. quinquefasciatus will be a more important vector than Anopheles as the goal of elimination is approached.
In conclusion, the two trapping experiments described herein provide further evidence of an inherent bias that is typical when using different collection methods. The gravid traps collected significantly more Cx. quinquefasciatus in Masaika at the end of the rainy season, but there was no significant difference when the trapping was conducted in the middle of the rainy season in Vyeru. This may indicate an effect of the presence of natural alternative breeding sites on the efficacy of the gravid trap, which essentially provides an artificial breeding site. In Masaika, there was no significant difference in the proportion of infected mosquitoes collected, which was likely due to the small numbers of mosquitoes collected. In Vyeru, where a larger sample size was used, a significantly higher proportion of infected Cx. quinquefasciatus were collected in light traps than in gravid traps. It seems that the light trap is more adapted toward xenomonitoring efforts in Tanzania, particularly as it is also used to collect Anopheles vectors, but the gravid trap may be useful where Cx. quinquefasciatus is the only vector.
ACKNOWLEDGMENTS
We are grateful to Mdira Yahya Kasembe, Aza Kimambo, Max Demitrius, and Hassan Sudi for their help in the preparation for the field work. Yahya Saidi is thanked for his help in setting and collecting traps in Masaika. We thank Abed Kassim Rashid and Ramadhani Mihungo for helping in the setting and collection of traps. The volunteers in Masaika are also thanked for their assistance over the course of the trial. Thanks to Matt Kirby for his help over the course of the trial. Max Demitrius, Lilian Charles, and Bernard Batengana are thanked for their help in the laboratory work. The staff at National Institute for Medical Research, Filariasis Laboratory in Bombo Hospital are also thanked for their cooperation.
Footnotes
Financial support: The funding for this project came from LSHTM and a grant from AgriSense BCS Ltd. (Wales, United Kingdom). Funding was also provided by a Wellcome Trust and Royal Society grant awarded to Thomas Walker.
Authors' addresses: Seth R. Irish, Entomology Branch, Department of Parasitic Disease and Malaria, Center for Global Health, Centers for Disease Control and Prevention, Atlanta, GA, E-mail: sirish@cdc.gov. William M. B. Stevens, St. Georges Roman Catholic School, London, United Kingdom, E-mail: w.stevens@stgeorgesrc.org. Yahya A. Derua, National Institute for Medical Research, Muheza, Tanzania, E-mail: yahyaathman@yahoo.com. Thomas Walker and Mary M. Cameron, Department of Disease Control, Faculty of Infectious and Tropical Diseases, London School of Hygiene and Tropical Medicine, London, United Kingdom, E-mails: thomas.walker@lshtm.ac.uk and mary.cameron@lshtm.ac.uk.
References
- 1.WHO Global programme to eliminate lymphatic filariasis: progress report on mass drug administration, 2010. Wkly Epidemiol Rec. 2011;35:377–388. [PubMed] [Google Scholar]
- 2.WHO . Elimination of Lymphatic Filariasis as a Public Health Problem. Geneva, Switzerland: WHO; 1997. [Google Scholar]
- 3.GAELF . Half-time in LF elimination: teaming up with NTDs. In: Addiss D, editor. Sixth Meeting of the Global Alliance to Eliminate Lymphatic Filariasis. Seoul, Korea: 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weil GJ, Lammie PJ, Weiss N. The ICT Filariasis Test: a rapid-format antigen test for diagnosis of bancroftian filariasis. Parasitol Today. 1997;13:401–404. doi: 10.1016/s0169-4758(97)01130-7. [DOI] [PubMed] [Google Scholar]
- 5.Bockarie MJ. Molecular xenomonitoring of lymphatic filariasis. Am J Trop Med Hyg. 2007;77:591–592. [PubMed] [Google Scholar]
- 6.Bockarie MJ, Fischer P, Williams SA, Zimmerman PA, Griffin L, Alpers MP, Kazura JW. Application of a polymerase chain reaction-ELISA to detect Wuchereria bancrofti in pools of wild-caught Anopheles punctulatus in a filariasis control area in Papua New Guinea. Am J Trop Med Hyg. 2000;62:363–367. doi: 10.4269/ajtmh.2000.62.363. [DOI] [PubMed] [Google Scholar]
- 7.Rwegoshora RT, Simonsen PE, Meyrowitsch DW, Malecela-Lazaro MN, Michael E, Pedersen EM. Bancroftian filariasis: house-to-house variation in the vectors and transmission—and the relationship to human infection—in an endemic community of coastal Tanzania. Ann Trop Med Parasitol. 2007;101:51–60. doi: 10.1179/136485907X154610. [DOI] [PubMed] [Google Scholar]
- 8.Simonsen PE, Pedersen EM, Rwegoshora RT, Malecela MN, Derua YA, Magesa SM. Lymphatic filariasis control in Tanzania: effect of repeated mass drug administration with ivermectin and albendazole on infection and transmission. PLoS Negl Trop Dis. 2010;4:e696. doi: 10.1371/journal.pntd.0000696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bockarie MJ, Hii JLK, Alexander NDE, Bockarie F, Dagoro H, Kazura JW, Alpers MP. Mass treatment with ivermectin for filariasis control in Papua New Guinea: impact on mosquito survival. Med Vet Entomol. 1999;13:120–123. doi: 10.1046/j.1365-2915.1999.00159.x. [DOI] [PubMed] [Google Scholar]
- 10.Silver JB. Mosquito Ecology: Field Sampling Methods. Dordrecht, The Netherlands: Springer; 2008. [Google Scholar]
- 11.Harrison BA, Whitt PB, Roberts LF, Lehman JA, Lindsey NP, Nasci RS, Hansen GR. Rapid assessment of mosquitoes and arbovirus activity after floods in southeastern Kansas, 2007. J Am Mosq Control Assoc. 2009;25:265–271. doi: 10.2987/08-5754.1. [DOI] [PubMed] [Google Scholar]
- 12.Reisen W, Lothrop H, Chiles R, Madon M, Cossen C, Woods L, Husted S, Kramer V, Edman J. West Nile virus in California. Emerg Infect Dis. 2004;10:1369–1378. doi: 10.3201/eid1008.040077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reiter P, Jakob WL, Francy DB, Mullenix JB. Evaluation of the CDC gravid trap for the surveillance of St. Louis encephalitis vectors in Memphis, Tennessee. J Am Mosq Control Assoc. 1986;2:209–211. [PubMed] [Google Scholar]
- 14.Williams GM, Gingrich JB. Comparison of light traps, gravid traps, and resting boxes for West Nile virus surveillance. J Vector Ecol. 2007;32:285–291. doi: 10.3376/1081-1710(2007)32[285:coltgt]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 15.Lukacik G, Anand M, Shusas EJ, Howard JJ, Oliver J, Chen H, Backenson PB, Kauffman EB, Bernard KA, Kramer LD, White DJ. West Nile virus surveillance in mosquitoes in New York State, 2000–2004. J Am Mosq Control Assoc. 2006;22:264–271. doi: 10.2987/8756-971X(2006)22[264:WNVSIM]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 16.Muturi EJ, Mwangangi J, Shililu J, Muriu S, Jacob B, Mbogo CM, John G, Novak R. Evaluation of four sampling techniques for surveillance of Culex quinquefasciatus (Diptera: Culicidae) and other mosquitoes in African rice agroecosystems. J Med Entomol. 2007;44:503–508. doi: 10.1603/0022-2585(2007)44[503:eofstf]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 17.Irish SR, Moore SJ, Derua YA, Bruce J, Cameron MM. Evaluation of gravid traps for the collection of Culex quinquefasciatus, a vector of lymphatic filariasis in Tanzania. Trans R Soc Trop Med Hyg. 2013;107:15–22. doi: 10.1093/trstmh/trs001. [DOI] [PubMed] [Google Scholar]
- 18.White GB. Studies on transmission of bancroftian filariasis in north-eastern Tanzania. Trans R Soc Trop Med Hyg. 1971;65:819–829. doi: 10.1016/0035-9203(71)90098-8. [DOI] [PubMed] [Google Scholar]
- 19.Meyrowitsch DW, Pedersen EM, Alifrangis M, Scheike TH, Malecela MN, Magesa SM, Derua YA, Rwegoshora RT, Michael E, Simonsen PE. Is the current decline in malaria burden in sub-Saharan Africa due to a decrease in vector population? Malar J. 2011;10:188. doi: 10.1186/1475-2875-10-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Edwards FW. Mosquitoes of the Ethiopian Region. III. Culicine Adults and Pupae. London, United Kingdom: British Museum; 1941. [Google Scholar]
- 21.Gillies MT, De Meillon B. The Anophelinae of Africa South of the Sahara. Vol. 54. Johannesburg, South Africa: Publications of the South African Institute for Medical Research; 1968. [Google Scholar]
- 22.Gillies MT, Coetzee M. A Supplement to the Anophelinae of Africa South of the Sahara (Afrotropical Region) Vol. 55. Johannesburg, South Africa: Publications of the South African Institute for Medical Research; 1987. [Google Scholar]
- 23.Service MW . Handbook to the Afrotropical Toxorhynchitine and Culicine Mosquitoes, Excepting Aedes and Culex. London, United Kingdom: British Museum; 1990. [Google Scholar]
- 24.Chambers EW, McClintock SK, Avery MF, King JD, Bradley MH, Schmaedick MA, Lammie PJ, Burkot TR. Xenomonitoring of Wuchereria bancrofti and Dirofilaria immitis infections in mosquitoes from American Samoa: trapping considerations and a comparison of polymerase chain reaction assays with dissection. Am J Trop Med Hyg. 2009;80:774–781. [PubMed] [Google Scholar]
- 25.Katholi CR, Toé L, Merriweather A, Unnasch TR. Determining the prevalence of Onchocerca volvulus infection in vector populations by PCR screen of pools of black flies. J Infect Dis. 1995;172:1414–1417. doi: 10.1093/infdis/172.5.1414. [DOI] [PubMed] [Google Scholar]
- 26.Dabire RK, Diabate A, Baldet T, Pare-Toe L, Guiguemde RT, Ouedraogo JB, Skovmand O. Personal protection of long lasting insecticide-treated nets in areas of Anopheles gambiae s.s. resistance to pyrethroids. Malar J. 2006;5:12. doi: 10.1186/1475-2875-5-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Magbity EB, Lines JD, Marbiah MT, David K, Peterson E. How reliable are light traps in estimating biting rates of adult Anopheles gambiae s.l. (Diptera: Culicidae) in the presence of treated bed nets? Bull Entomol Res. 2002;92:71–76. doi: 10.1079/BER2001131. [DOI] [PubMed] [Google Scholar]
- 28.Alencar J, Silva JDS, Oliveira LCM, Marcondes CB, Morone F, Lorosa ES. Feeding patterns of Culex quinquefasciatus (Diptera: Culicidae) from eastern Santa Catarina State, Brazil. J Med Entomol. 2012;49:952–954. doi: 10.1603/me11270. [DOI] [PubMed] [Google Scholar]
- 29.Pichon G. Limitation and facilitation in the vectors and other aspects of the dynamics of filarial transmission: the need for vector control against Anopheles-transmitted filariasis. Ann Trop Med Parasitol. 2002;96:S143–S152. doi: 10.1179/000349802125002509. [DOI] [PubMed] [Google Scholar]
- 30.Bockarie MJ, Alexander NDE, Hyun P, Dimber Z, Bockarie F, Ibam E, Alpers MP, Kazura JW. Randomised community-based trial of annual single-dose diethylcarbamazine with or without ivermectin against Wuchereria bancrofti infection in human beings and mosquitoes. Lancet. 1998;351:162–168. doi: 10.1016/S0140-6736(97)07081-5. [DOI] [PubMed] [Google Scholar]