Abstract
Alpha-ketoglutarate (AKG) is a key molecule in the Krebs cycle determining the overall rate of the citric acid cycle of the organism. It is a nitrogen scavenger and a source of glutamate and glutamine that stimulates protein synthesis and inhibits protein degradation in muscles. AKG as a precursor of glutamate and glutamine is a central metabolic fuel for cells of the gastrointestinal tract as well. AKG can decrease protein catabolism and increase protein synthesis to enhance bone tissue formation in the skeletal muscles and can be used in clinical applications. In addition to these health benefits, a recent study has shown that AKG can extend the lifespan of adult Caenorhabditis elegans by inhibiting ATP synthase and TOR. AKG not only extends lifespan, but also delays age-related disease. In this review, we will summarize the advances in AKG research field, in the content of its physiological functions and applications.
Keywords: Alpha-ketoglutarate, Functions, Lifespan extension, Applications
INTRODUCTION
Several decades ago, the list of key nutrients that may influence metabolic processes was limited studied. Currently, the list includes fatty acids, vitamins, microelements, nucleic acids and specific amino acids. Common research in nutrient support is beginning to investigate exerting organ-specific effects by modulating metabolic processes rather than by simply improving nutrition. Alpha-ketoglutarate (AKG), also referred to as 2-ketoglutaric acid, 2-oxoglutamate, 2-oxoglutaric acid, oxoglutaric acid and 2-oxopentanedioic acid (Harrison and Pierzynowski, 2008), is a rate-determining intermediate in the tricarboxylic acid (TCA) and has a crucial role in cellular energy metabolism. In cellular metabolism, the generation and decomposition of AKG involved in a variety of metabolic pathways. In the TCA cycle, AKG is decarboxylated to succinyl-CoA and CO2 by AKG dehydrogenase (encoded by ogdh-1), a key control point of the TCA cycle. Otherwise, AKG can be generated from isocitrate by oxidative decarboxylation catalysed by isocitrate dehydrogenase (IDH). Also, AKG can be produced anaplerotically from glutamate by oxidative deamination using glutamate dehydrogenase, and as a product of pyridoxal phosphate-dependent trans-amination reactions in which glutamate is a common amino donor. AKG can dissolve well in water, does not show toxic properties and its water solutions characterize has high stability.
AKG supplementation in human adult stage is sufficient whereas it is found to be insufficient in the senescent stage (Chin et al., 2014). In the cellular metabolism, it is impossible to utilize AKG from the TCA cycle in the synthesis of amino acids, for this to occur, one must provide AKG as a pure dietary supplement. It was demonstrated that AKG was significantly better absorbed from the upper small intestine than from the distal sections (Dąbek et al., 2005). Low pH, Fe2+ and/or SO2−4 ions can enhance AKG absorption. AKG has a short lifetime, is probably dependent on quick metabolism in the enteorcyetes and liver (Dąbek et al., 2005). Over 60% of enteral AKG passes through the intestine in different forms and is not oxidized to the degree of 100% as glutamine and glutamate (Junghans et al., 2006). In the enterocytes, AKG is converted into proline, leucine and other amino acids (Lambert et al., 2006). Moreover, enteric feeding of AKG supplements can significantly increase circulating plasma levels of such hormones as insulin, growth hormone and insulin like growth factor-1 (IGF-1) (Colomb et al., 2004; Cynober, 2004; Son et al., 2007) and all derivatives of AKG (e.g. glutamine or glutamate) are immediately converted to CO2 during their passage across the gut epithelium (Harrison and Pierzynowski, 2008). Precisely because AKG play crucial role in cellular energy metabolism and participate in a variety of metabolic pathways, in this review, we will summarize generally the advances in AKG research field to promote the understanding of AKG and calling for more research focus on AKG.
PHYSIOLOGICAL FUNCTIONS
AKG can modulate protein synthesis and bone development
In the cellular metabolism, AKG provides an important source of glutamine and glutamate that stimulates protein synthesis, inhibits protein degradation in muscle, and constitutes an important metabolic fuel for cells of the gastrointestinal tract (Hixt and Müller, 1996; Jones et al., 1999). Glutamine is an energy source for all types of cells in the organism constituting more than 60% of the total amino acid pool, so AKG as a precursor of glutamine, is a main source of energy for intestinal cells and a preferred substrate for both enterocytes and other rapidly dividing cells. In addition, glutamate, released from nerve fibers in bone tissue, is synthesized by the reductive amination of AKG in peri-vein hepatocytes (Stoll et al., 1991) and can give rise to an increase in proline synthesis, which plays a central role in the synthesis of collagen (Kristensen et al., 2002). In the liver, glutamine serves as a precursor for ureagenesis, gluconeogenesis and acute phase protein synthesis (Espat et al., 1996; Alpers, 2006), plays an important role in the inter-organ flow of nitrogen and carbon. Glutamine has traditionally been considered to be a non-essential amino acid in health, but in catabolic states and stress, it is an essential fuel source for cells of the gastrointestinal tract, rapidly dividing leucocytes and macrophages in the immune system and can be rapidly depleted despite the significant release from muscle tissue (Śliwa et al., 2009). Otherwise, it was also shown that AKG can improve absorption of Fe2+. Thus, AKG and its derivatives can play a role as a Fe2+ absorption enhancer both in rapidly growing animals and humans with Fe2+ insufficiency (Dąbek et al., 2005). Furthermore, AKG, ascorbate and Fe2+ steer hydroxylation of peptide-bound proline to hydroxyproline via prolyl hydrolase, increasing the conversion of pro-collagen to collagen and bone matrix formation (Tocaj et al., 2003). Therefore, AKG is an important source of amino acids for collagen synthesis in the cell and organism.
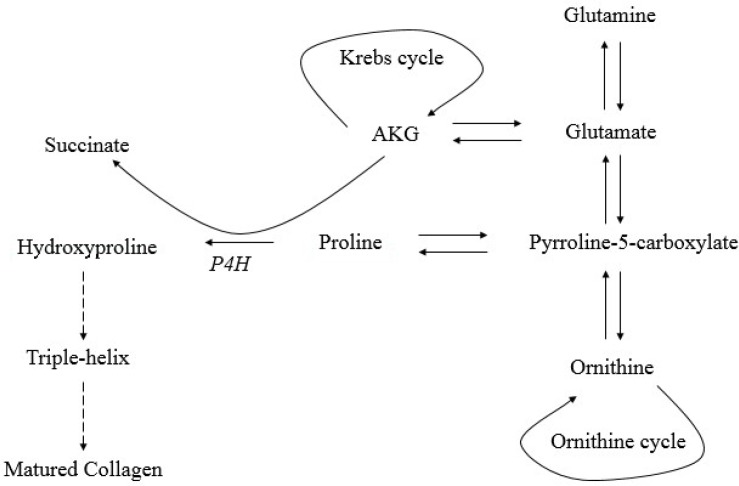
It has been demonstrated that AKG is involved in collagen metabolism through a variety of mechanisms. The main mechanism is presented in Fig. 1. First, AKG is a cofactor of prolyl-4-hydroxylase (P4H). P4H is located within the endoplasmic reticulum (ER), and catalyze the formation of 4-hydroxyproline, which is crucial for the formation of the collagen triple helix. Incomplete hydroxylation of proline residues within the repeated amino acid motif: any amino acid-proline-glycine (X-Pro-Gly), results in incomplete formation of the collagen triple helix. Incorrectly folded triple helices are not secreted into cytoplasm, and are subsequently degraded in the ER (Lamande and Bateman, 1999; Myllyharju, 2003). Second, AKG contributes to facilitate collagen synthesis by increasing the pool of proline residues via glutamate (Panosyan et al., 2004; Wu et al., 2004; Dakshayani and Subramanian, 2006; Lambert et al., 2006; Rani et al., 2012; Korkmaz et al., 2007; Son et al., 2007) and about 25% of the dietary AKG is converted to proline in the enterocytes (Kristensen et al., 2002). Proline is a primary substrate for collagen synthesis, and plays a central role in collagen metabolism. As seen in Fig. 1, proline is formed through the conversion of pyrroline 5-carboxylate (P5C), an intermediate in the inter-conversion of proline, ornithine and glutamate. Recently, it was reported that in addition to being a source of proline residues through the P5C-pathway, P5C activates collagen production through the activation of prolidase, a key enzyme in proline recyling (Son et al., 2007). This is a significant finding, because the P5C-pathway is a minor contributor to the proline pool during collagen synthesis; the major source of proline is through recycling of proline from collagen degradation products (Isemura et al., 1979; Myara et al., 1984; Bissonnette et al., 1993; Palka and Phang, 1997; Karna et al., 2013). In this regard, AKG, which is a precursor of P5C, also has a close relationship to proline metabolism in the cell and organism. In a study performed in growing pigs, it was displayed that enteral AKG administration increased the level of proline in the portal and arterial blood by 45% and 20%, respectively, when compared to animals that were not given AKG. Through improved proline and hydroxyproline formation, enteral AKG is believed to enhance bone tissue formation (Bellon et al., 1995; Kristensen et al., 2002).
Fig. 1.
Mechanism of AKG in collagen production.
Another mechanisms of AKG influence on bone tissue results from its impact on the endocrine system of the organism. Glutamine and glutamate is transformed in ornithine and then to arginine (Pierzynowski and Sjodin, 1998). Both ornithine and arginine stimulate the secretion of growth hormone (GH) and insulin-like growth factor I (IGF-I) (Harrison et al., 2004; Fayh et al., 2007). The osteotropic effect of functional axis GH-IGF-I is widely known and well described (Giustina et al., 2008; Tritos and Biller, 2009). AKG may also affect bone structure by the interaction of glutamate-glutamate receptors (GluR). The presence of GluR has been confirmed on osteoblasts (Gu et al., 2002) and osteoclasts (Mentaverri et al., 2003), whereas Genever et al (Spencer et al., 2007) reported its significance in bone tissue metabolism. Additionally, there is a preliminary evidence to show that dietary AKG counteracts the bone losses in rats with experimental osteopenia induced by ovariectomy (Bieńko et al., 2002; Radzki et al., 2002) and fundectomy (Dobrowolski et al., 2008). Although we can infer the importance of AKG in collagen metabolism based on these studies, the direct effects of AKG on collagen production have yet to be reported.
AKG can stabilize immune system homeostasis
AKG is also called the immune nutrient factor and it play an important role in the general immune metabolism (Abcouwer, 2000; Ziegler and Daignault, 2000; Yeh et al., 2004). It is already known that AKG is an important source of glutamine and glutamate, is defined as glutamine homologue and derivative (Pesty et al., 1997; Tapiero et al., 2002). Glutamine is an important fuel for lymphocytes and macrophages (Parry-Billings et al., 1990). Macrophages and neutrophils are involved in the early, non-specific host-defence responses and play an important role in the pathophysiology and/or protection against sepsis (Sawyer et al., 1989; Zimmerman and Ringer, 1992). Previous reports showed that during inflammatory states such as sepsis and injury, the consumption of glutamine by circulating and immune cells increases (Ashkanazi et al., 1980; Roth et al., 1982; Hammarqvist et al., 1989). Studies have revealed that supplemental glutamine augments the in vitro bactericidal activity of neutrophils in burned or postoperative patients (Ogle et al., 1994; Furukawa et al., 2000). Parry-Billings et al. (1990) (Parry-Billings et al., 1990) reported that depressed glutamine concentrations were associated with reduced phagocytosis by murine peritoneal macrophages. The study by Gianotti et al. (1995) (Gianotti et al., 1995) showed that oral glutamine supplementation decreases bacterial translocation in experimental gut-origin sepsis. Thus, AKG as glutamine homologue has immuno-enhancing properties, can maintain a gut barrier, increase immune cells and the activity of neutrophils and phagocytosis, reduce bacterial translocation in vivo (Le Boucher and Cynober, 1997; Danbolt, 2001; MacFie and McNaught, 2002; Salvalaggio and Campos, 2002).
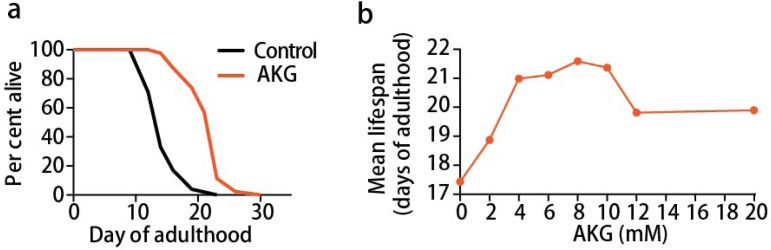
AKG can modulate aging
A recent study (Chin et al., 2014) shows that AKG can extend the lifespan of adult Caenorhabditis elegans by inhibiting ATP synthase and TOR. They discovered that the tricarboxylic acid cycle intermediate AKG delays ageing and extends the lifespan of C. elegans by ∼ 50% (Fig. 2A) with a concentration-dependent manner of 8 mM AKG producing the maximal lifespan extension in wild-type N2 worms (Fig. 2B). Chin et al (Chin et al., 2014) also demonstrated that AKG not only extends lifespan, but also delays age-related phenotypes, such as the decline in rapid, coordinated body movement. In this study, it reported that AKG has greater potential values in aging. Thus, we would like to generally describe the mechanism how AKG inhibits ATP synthase and TOR to extend the lifespan in the organisms.
Fig. 2.
AKG extends the adult lifespan of C. elegans. (A) AKG extends the lifespan of adult worms. (B) Dose-response curve of the AKG effect on longevity.
Mitochondrial ATP synthase is a significant ubiquitous enzyme in energy metabolism of virtually all living cells (Abrahams et al., 1994; Boyer, 1997). It is a membrane-bound rotary motor enzyme that is a key energy carrier for cellular energy metabolism. Chin et al (Chin et al., 2014) provided evidence that the lifespan increase by AKG requires ATP synthase subunit β and is dependent on target of rapamycin (TOR) downstream. They used a small-molecule target identification strategy termed drug affinity responsive target stability (DARTS) (Lomenick et al., 2009), found the ATP synthase subunit β is a novel binding protein of AKG. They discovered AKG inhibits ATP synthase, leads to reduced ATP content, decreased oxygen consumption, and increased autophagy in both C. elegans and mammalian cells, similar to ATP synthase 2 (ATP-2) knockdown. Together, the direct binding of ATP-2 by AKG, the related enzymatic inhibition, reduction in ATP levels and oxygen consumption, lifespan analysis, and other similarities to ATP-2 knockdown, they inferred AKG probably extends lifespan primarily by targeting ATP-2. In addition, previous studies also has shown that complete loss of mitochondrial function is detrimental, but partial suppression of the electron transport chain has been demonstrated to extend C. elegans lifespan (Tsang et al., 2001; Dillin et al., 2002; Lee et al., 2003; Curran and Ruvkun, 2007). Thus, AKG can inhibit the ATP synthase, so to achieve the effect of prolonging life is completely possible.
Target of rapamycin (TOR), belongs to a conserved group of serine/threonine kinases from the phosphatidylinositol kinase-related kinase (PIKK) family, regulates growth and metabolism in all eukaryotic cells. Previous researches have demonstrated that inhibition of TOR activity can delay the aging process, as evidenced by increased life span in yeast (Kaeberlein et al., 2007), worms (Vellai et al., 2003; Hansen et al., 2007), flies (Kapahi et al., 2004; Luong et al., 2006), and mice (Selman et al., 2009) with mutations in TOR pathway components. AKG does not interact with TOR directly and mainly decreases TOR pathway activity through the inhibition of ATP synthase (Fig. 3). AKG longevity partially depends on AMPK and FoxO (Urban et al., 2007). The AMP-activated protein kinase (AMPK) is an evolutionarily conserved cellular energy sensor with key roles in aging and lifespan (Hardie et al., 2012; Huang et al., 2013). AMPK is activated when the AMP/ATP ratio is high and subsequently, activated AMPK inhibits TOR signaling by activating phosphorylation of the TOR suppressor TSC2, sequentially adjusting the cell’s metabolic program to energy status (Toivonen et al., 2007). Fork head box ‘Other’ (FoxO) proteins, a subgroup of the Fork head transcription factor family, have an pivotal role in mediating the impacts of insulin and growth factors on diverse physiological functions, including cell proliferation, apoptosis and metabolism (Brunet, 2004; Barthel et al., 2005; Gross et al., 2008; Wang et al., 2014; Webb and Brunet, 2014). Consistent with the implicate of TOR in AKG longevity, the FoxO, a transcription factor PHA-4, which is required to extend lifespan in response to reduced TOR signaling (Sheaffer et al., 2008), is likewise essential for AKG-induced longevity. In addition, autophagy, which is activated both by TOR inhibition (Wullschleger et al., 2006; Stanfel et al., 2009) and by dietary restriction (Meléndez et al., 2003), is significantly increased in worms treated with AKG. Therefore, AKG treatment and TOR inactivation extend lifespan either through the same pathway (with AKG acting on or upstream of TOR), or through independent mechanisms or parallel pathways that converge on a downstream effector (Chin et al., 2014).
Fig. 3.
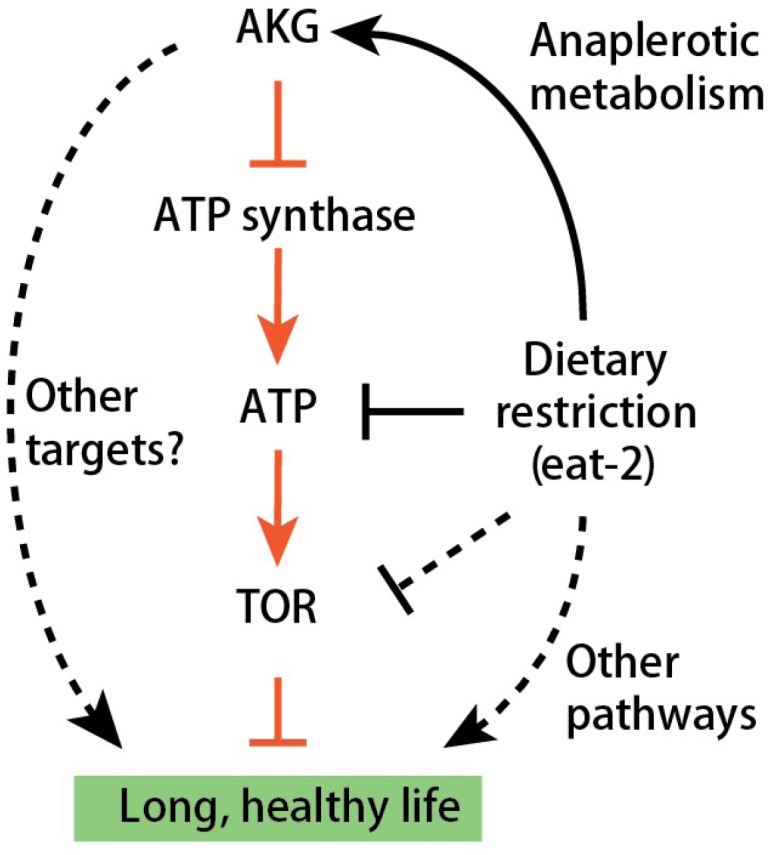
Model of α-KG-mediated longevity.
Furthermore, physiological increases in AKG levels have been shown in starved yeast and bacteria (Brauer et al., 2006), in the liver of starved pigeons (Kaminsky et al., 1982), and in humans after physical exercise (Brugnara et al., 2012). The biochemical basis for this increase of AKG is explained by starvation based anaplerotic gluconeogenesis, which activates glutamate-linked transaminases in the liver to generate carbon derived from amino acid catabolism. Consistent with this idea, Chin et al (Chin et al., 2014) observed that AKG levels are elevated in starved C. elegans and AKG does not extend the lifespan of dietary-restricted animals. These findings indicated a model in which AKG is a key metabolite mediating lifespan extension by starvation/dietary restriction (Fig. 3). It demonstrated new molecular links between a common metabolite, a universal cellular energy generator and dietary restriction in the regulation of organismal lifespan, thus indicated new strategies for the prevention and treatment of aging and age-related diseases.
THE APPLICATION OF AKG IN ANIMALS
AKG has been given to pigs (Kowalik et al., 2005; Andersen et al., 2008), turkeys (Tatara et al., 2005a; Tatara et al., 2005b), rats (Bieńko et al., 2002; Radzki et al., 2002) and sheep (Harrison et al., 2004; Tatara et al., 2007) with effects on the skeletal system and protein synthesis. Considering current knowledge of AKG, its metabolites and functions, it can be concluded that improved bone quality may be induced by higher glutamate synthesis and its utilization as signaling molecule in bone metabolism regulation (Stoll et al., 1991; Chenu, 2002a; Chenu, 2002b; Taylor, 2002). The other mechanism that may be involved in bone metabolism regulation by AKG is increased collagen formation as the result of higher proline synthesis and its following conversion to hydroxyproline, which was previously introduced (Kristensen et al., 2002).
In studies on animals, AKG administration has generated positive effects on skeletal development and homeostasis maintenance (Kowalik et al., 2005; Tatara et al., 2005a; Tatara et al., 2005b). In AKG-treated animals, significant increase of weight, length, bone mineral density, bone mineral content, cross-sectional area, second moment of inertia, mean relative wall thickness, cortical index, maximum elastic strength and ultimate strength of the bones was associated with improved serum concentration of IGF-1 and serum BAP activity when compared to the control group (Śliwa, 2010). Results of long bone analysis in slaughter pigs treated during 21 and 24 days of neonatal life with AKG has shown its positive effects on length, cortical bone mineral density, maximum elastic strength, ultimate strength and Young’s modulus that was connected with elevated plasma estrogen level (Andersen et al., 2008). In studies on growing turkeys, 14-week long administration with AKG eliminated neurectomy-induced osteopenia of radius increasing its weight, volumetric bone mineral density, the cross-sectional area, second moment of inertia, mean relative wall thickness, maximum elastic strength and ultimate strength (Tatara et al., 2005a). These advantageous effects were combined with higher serum concentration of proline and leucine in comparison to the control group birds (Tatara et al., 2005a). In other studies on sheep, two week long neonatal treatment with AKG improved the trabecular bone mineral density, cortical bone mineral density and maximum elastic strength of femur as well as increasing weight, length, cortical bone mineral density, maximum elastic strength and the moments of maximum elastic strength and ultimate strength (Harrison et al., 2004; Tatara et al., 2007).
The similar influence of AKG administration on bone tissue was also observed in studies performed on humans (Tocaj et al., 2003; Fayh et al., 2007). It can facilitate muscle protein synthesis in post-operative patients (Wernerman et al., 1990), to improve amino acid metabolism in haemo-dialysed patients (Riedel et al., 1996), and to accelerate the transport of organic anions in the kidneys (Welborn et al., 1998), when AKG was given as a supplement. Use of AKG or calcium-AKG as dietary supplements has mainly been studied on hospitalized adult humans, who are well nourished and have a normal functional metabolism (Pierzynowski et al., 2007). In clinical studies on septic, traumatic or surgical patients, AKG has been found to display beneficial effects by improving the body weight gain, nitrogen balance. A recent study has shown the potential usefulness of AKG treatment in preserving bone mass as well as lowering bone turnover in post-menopausal women (Tocaj et al., 2003). Results suggest a link between enteral AKG and an increase in oestrogen levels. Some studies have also reported that AKG is an efficient nutritional support in trauma situations, especially after burns (Wernerman et al., 1990; Le Boucher et al., 1997). Therefore, AKG can be an alternative for elderly patients after trauma and surgery and for people who execute intensive, but the short duration physical effort (Neu et al., 1996). It also is known that AKG has a beneficial effect on nitrogen metabolism (Wirén and Permert, 2002) and in reducing toxicity levels of ammonium ions as a protective agent for kidney function in the body (Stoll et al., 1991; Welborn et al., 1998; Velvizhi et al., 2002). In addition, Schlegel et al (Schlegel et al., 2000) observed that AKG supplementation can limit bacterial dissemination and metabolic changes after injury in rats and thus may be useful in protection of gut mucosa. Therefore, a number of studies have revealed the beneficial effects of AKG in human and animals.
SUMMARY AND FUTURE OUTLOOK
On the whole, the physiological significance of AKG are multi-directional and not all metabolic pathways have been well established. The mechanisms of AKG action on the skeletal system is associated with glutamate receptor activation, bone collagen production via proline and possible anti-catabolic and anabolic effects of 17b-oestradiol (Andersen et al., 2008), and is probably multifactorial. In addition, the positive influence of AKG might be expected to improve chest function and internal organ protection of premature and low birth-weight newborns (Tatara et al., 2007). The present findings may have important clinical implications, motivating for the testing of AKG in prevention and therapy of metabolic bone disorders in human and animals. Therefore, further studies are needed to understand the function of AKG, clarify of the mechanism of AKG and explore the potential application in human society or other fields.
In the aspect of aging, some exciting discoveries indicated that TORC1 is involved in a large number of human diseases, including diabetes, obesity, heart disease, and cancer (Inoki and Guan, 2006; Katewa and Kapahi, 2011). Aging is a common risk factor for these diseases, and it has been revealed that the mechanism of the link between cellular senescence, diseases and organismal aging is via TOR (Kapahi and Zid, 2004; Blagosklonny, 2006). Therefore, inhibition of TOR function by metabolism of AKG indicated that AKG may play an important role in tumor suppress.
Acknowledgments
The study were supported by the Program from Sichuan Agricultural University (#02920400) and The National Natural Science Foundation of China (#31402063).
Footnotes
CONFLICTS OF INTEREST
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
REFERENCES
- Abcouwer SF. Effects of glutamine on immune cells. Nutrition. 2000;16:67–69. doi: 10.1016/S0899-9007(99)00237-3. [DOI] [PubMed] [Google Scholar]
- Abrahams JP, Leslie AG, Lutter R, Walker JE. Structure at 2.8 A resolution of F1-ATPase from bovine heart mitochondria. Nature. 1994;370:621–628. doi: 10.1038/370621a0. [DOI] [PubMed] [Google Scholar]
- Alpers DH. Glutamine: do the data support the cause for glutamine supplementation in humans? Gastroenterology. 2006;130:S106–S116. doi: 10.1053/j.gastro.2005.11.049. [DOI] [PubMed] [Google Scholar]
- Andersen NK, Tatara MR, Krupski W, Majcher P, Harrison AP. The long-term effect of alpha-ketoglutarate, given early in postnatal life, on both growth and various bone parameters in pigs. J Anim Physiol Anim Nutr. 2008;92:519–528. doi: 10.1111/j.1439-0396.2007.00742.x. [DOI] [PubMed] [Google Scholar]
- Ashkanazi J, Carpertier Y, Michelsen C. Muscle and plasma amino acids following injury. Ann Surg. 1980;192:78–85. doi: 10.1097/00000658-198007000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barthel A, Schmoll D, Unterman TG. FoxO proteins in insulin action and metabolism. Trends Endocrinol Metab. 2005;16:183–189. doi: 10.1016/j.tem.2005.03.010. [DOI] [PubMed] [Google Scholar]
- Bellon G, Chaqour B, Wegrowski Y, Monboisse JC, Borel JP. Glutamine increases collagen gene transcription in cultured human fibroblasts. Biochim. Biophys. Acta. 1995;1268:311–323. doi: 10.1016/0167-4889(95)00093-8. [DOI] [PubMed] [Google Scholar]
- Bieńko M, Radzki R, Puzio I, Filip R, Pierzynowski S, Studziński T. The influence of alpha-ketoglutarate (AKG) on mineralization of femur in rats with established osteopenia. Acta Orthop Scand. 2002;73:52. [Google Scholar]
- Bissonnette R, Friedmann D, Giroux JM, Dolenga M, Hechtman P, Der Kaloustian VM, Dubuc R. Prolidase deficiency: a multisystemic hereditary disorder. J Am Acad Dermatol. 1993;29:818–821. doi: 10.1016/0190-9622(93)70245-O. [DOI] [PubMed] [Google Scholar]
- Blagosklonny MV. Aging and immortality: quasi-programmed senescence and its pharmacologic inhibition. Cell Cycle. 2006;5:2087–2102. doi: 10.4161/cc.5.18.3288. [DOI] [PubMed] [Google Scholar]
- Boyer PD. The ATP synthase-a splendid molecular machine. Annu Rev Biochem. 1997;66:717–749. doi: 10.1146/annurev.biochem.66.1.717. [DOI] [PubMed] [Google Scholar]
- Brauer MJ, Yuan J, Bennett BD, Lu W, Kimball E, Botstein D, Rabinowitz JD. Conservation of the metabolomic response to starvation across two divergent microbes. Proc Natl Acad Sci USA. 2006;103:19302–19307. doi: 10.1073/pnas.0609508103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brugnara L, Vinaixa M, Murillo S, Samino S, Rodriguez MA, Beltran A, Lerin C, Davison G, Correig X, Novials A. Metabolomics approach for analyzing the effects of exercise in subjects with type 1 diabetes mellitus. PloS one. 2012;7:e40600. doi: 10.1371/journal.pone.0040600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunet A. [The multiple roles of FOXO transcription factors] Med Sci. 2004;20:856–859. doi: 10.1051/medsci/20042010856. [DOI] [PubMed] [Google Scholar]
- Chenu C. Glutamatergic innervation in bone. Microsc Res Tech. 2002a;58:70–76. doi: 10.1002/jemt.10120. [DOI] [PubMed] [Google Scholar]
- Chenu C. Glutamatergic regulation of bone remodeling. J Musculoskelet Neuronal Interact. 2002b;2:282–284. [PubMed] [Google Scholar]
- Chin RM, Fu X, Pai MY, Vergnes L, Hwang H, Deng G, Diep S, Lomenick B, Meli VS, Monsalve GC. The metabolite α-ketoglutarate extends lifespan by inhibiting ATP synthase and TOR. Nature. 2014;510:397–401. doi: 10.1038/nature13264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colomb V, Dabbas M, Goulet O, Talbotec C, Corriol O, Ricour C. Prepubertal growth in children with long-term parenteral nutrition. Horm Res Paediatr. 2004;58:2–6. doi: 10.1159/000064760. [DOI] [PubMed] [Google Scholar]
- Curran SP, Ruvkun G. Lifespan regulation by evolutionarily conserved genes essential for viability. PLoS Genet. 2007;3:e56. doi: 10.1371/journal.pgen.0030056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cynober L. Ornithine α-ketoglutarate as a potent precursor of arginine and nitric oxide: a new job for an old friend. J Nutr. 2004;134:2858S–2862S. doi: 10.1093/jn/134.10.2858s. [DOI] [PubMed] [Google Scholar]
- Dąbek M, Kruszewska D, Filip R, Hotowy A, Pierzynowski Ł, Wojtasz-Pająk A, Szymanczyk S, Valverde Piedra J, Werpachowska E, Pierzynowski S. α-Ketoglutarate (AKG) absorption from pig intestine and plasma pharmacokinetics. J Anim Physiol Anim Nutr. 2005;89:419–426. doi: 10.1111/j.1439-0396.2005.00566.x. [DOI] [PubMed] [Google Scholar]
- Dakshayani K, Subramanian P. α-ketoglutarate modulates the circadian patterns of lipid peroxidation and antioxidant status during N-nitrosodiethylamine-induced hepatocarcinogenesis in rats. J. Med. Food. 2006;9:90–97. doi: 10.1089/jmf.2006.9.90. [DOI] [PubMed] [Google Scholar]
- Danbolt NC. Glutamate uptake. Prog Neurobiol. 2001;65:1–105. doi: 10.1016/S0301-0082(00)00067-8. [DOI] [PubMed] [Google Scholar]
- Dillin A, Hsu AL, Arantes-Oliveira N, Lehrer-Graiwer J, Hsin H, Fraser AG, Kamath RS, Ahringer J, Kenyon C. Rates of behavior and aging specified by mitochondrial function during development. Science. 2002;298:2398–2401. doi: 10.1126/science.1077780. [DOI] [PubMed] [Google Scholar]
- Dobrowolski PJ, Piersiak T, Surve VV, Kruszewska D, Gawron A, Pacuska P, Håkanson R, Pierzynowski SG. Dietary α-ketoglutarate reduces gastrectomy-evoked loss of calvaria and trabecular bone in female rats. Scand J Gastroenterol. 2008;43:551–558. doi: 10.1080/00365520701824951. [DOI] [PubMed] [Google Scholar]
- Espat NJ, Watkins KT, Lind DS, Weis JK, Copeland EM, Souba WW. Dietary modulation of amino acid transport in rat and human liver. J Surg Res. 1996;63:263–268. doi: 10.1006/jsre.1996.0258. [DOI] [PubMed] [Google Scholar]
- Fayh AP, Friedman R, Sapata KB, Oliveira AR. [Effect of L-arginine supplementation on secretion of human growth hormone and insulin-like growth factor in adults] Arq Bras Endocrinol Metabol. 2007;51:587–592. doi: 10.1590/S0004-27302007000400013. [DOI] [PubMed] [Google Scholar]
- Furukawa S, Saito H, Inoue T, Matsuda T, Fukatsu K, Han I, Ikeda S, Hidemura A. Supplemental glutamine augments phagocytosis and reactive oxygen intermediate production by neutrophils and monocytes from postoperative patients in vitro. Nutrition. 2000;16:323–329. doi: 10.1016/S0899-9007(00)00228-8. [DOI] [PubMed] [Google Scholar]
- Gianotti L, Alexander JW, Gennari R, Pyles T, Babcock GF. Oral glutamine decreases bacterial translocation and improves survival in experimental gut-origin sepsis. J Parenter Enteral Nutr. 1995;19:69–74. doi: 10.1177/014860719501900169. [DOI] [PubMed] [Google Scholar]
- Giustina A, Mazziotti G, Canalis E. Growth hormone, insulin-like growth factors, and the skeleton. Endocr Rev. 2008;29:535–559. doi: 10.1210/er.2007-0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross DN, van den Heuvel AP, Birnbaum MJ. The role of FoxO in the regulation of metabolism. Oncogene. 2008;27:2320–2336. doi: 10.1038/onc.2008.25. [DOI] [PubMed] [Google Scholar]
- Gu Y, Genever P, Skerry T, Publicover S. The NMDA type glutamate receptors expressed by primary rat osteoblasts have the same electrophysiological characteristics as neuronal receptors. Calcif Tissue Int. 2002;70:194–203. doi: 10.1007/s00223-001-2004-z. [DOI] [PubMed] [Google Scholar]
- Hammarqvist F, Wernerman J, Ali R, von der Decken A, Vinnars E. Addition of glutamine to total parenteral nutrition after elective abdominal surgery spares free glutamine in muscle, counteracts the fall in muscle protein synthesis, and improves nitrogen balance. Ann Surg. 1989;209:455–461. doi: 10.1097/00000658-198904000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen M, Taubert S, Crawford D, Libina N, Lee SJ, Kenyon C. Lifespan extension by conditions that inhibit translation in Caenorhabditis elegans. Aging Cell. 2007;6:95–110. doi: 10.1111/j.1474-9726.2006.00267.x. [DOI] [PubMed] [Google Scholar]
- Hardie DG, Ross FA, Hawley SA. AMPK: a nutrient and energy sensor that maintains energy homeostasis. Nat Rev Mol Cell Biol. 2012;13:251–262. doi: 10.1038/nrm3311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison AP, Pierzynowski S. Biological effects of 2-oxoglutarate with particular emphasis on the regulation of protein, mineral and lipid absorption/metabolism, muscle performance, kidney function, bone formation and cancerogenesis, all viewed from a healthy ageing perspective state of the art-review article. J Physiol Pharmacol. 2008;59:91–106. [PubMed] [Google Scholar]
- Harrison AP, Tygesen MP, Sawa-Wojtanowicz B, Husted S, Tatara M. α-Ketoglutarate treatment early in postnatal life improves bone density in lambs at slaughter. Bone. 2004;35:204–209. doi: 10.1016/j.bone.2004.03.016. [DOI] [PubMed] [Google Scholar]
- Hixt U, Müller H. L-alanyl-glutamine-a glutamine dipeptide for paraenteral nutrition. Environ Health Perspect. 1996;2:72–76. [Google Scholar]
- Huang X, Liu J, Withers BR, Samide AJ, Leggas M, Dickson RC. Reducing signs of aging and increasing lifespan by drug synergy. Aging Cell. 2013;12:652–660. doi: 10.1111/acel.12090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inoki K, Guan K-L. Complexity of the TOR signaling network. Trends Cell Biol. 2006;16:206–212. doi: 10.1016/j.tcb.2006.02.002. [DOI] [PubMed] [Google Scholar]
- Isemura M, Hanyu T, Gejyo F, Nakazawa R, Igarashi R, Matsuo S, Ikeda K, Sato Y. Prolidase deficiency with imidodipeptiduria. A familial case with and without clinical symptoms. Clin. Chim. Acta. 1979;93:401–407. doi: 10.1016/0009-8981(79)90291-2. [DOI] [PubMed] [Google Scholar]
- Jones C, Allan Palmer T, Griffiths R. Randomized clinical outcome study of critically ill patients given glutamine-supplemented enteral nutrition. Nutrition. 1999;15:108–115. doi: 10.1016/S0899-9007(98)00172-5. [DOI] [PubMed] [Google Scholar]
- Junghans P, Derno M, Pierzynowski S, Hennig U, Eberhard Rudolph P, Souffrant WB. Intraduodenal infusion of α-ketoglutarate decreases whole body energy expenditure in growing pigs. Clin Nutr. 2006;25:489–496. doi: 10.1016/j.clnu.2005.11.003. [DOI] [PubMed] [Google Scholar]
- Kaeberlein M, Burtner CR, Kennedy BK. Recent developments in yeast aging. PLoS Genet. 2007;3:e84. doi: 10.1371/journal.pgen.0030084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaminsky YG, Kosenko EA, Kondrashova MN. Metabolites of citric acid cycle, carbohydrate and phosphorus metabolism, and related reactions, redox and phosphorylating states of hepatic tissue, liver mitochondria and cytosol of the pigeon, under normal feeding and natural nocturnal fasting conditions. Comp Biochem Physiol B. 1982;73:957–963. doi: 10.1016/0305-0491(82)90343-1. [DOI] [PubMed] [Google Scholar]
- Kapahi P, Zid B. TOR pathway: linking nutrient sensing to life span. Sci Aging Knowledge Environ. 2004;2004:pe34. doi: 10.1126/sageke.2004.36.pe34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapahi P, Zid BM, Harper T, Koslover D, Sapin V, Benzer S. Regulation of lifespan in drosophila by modulation of genes in the TOR signaling pathway. Curr Biol. 2004;14:885–890. doi: 10.1016/j.cub.2004.03.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karna E, Szoka L, Palka JA. The mechanism of hydralazine-induced collagen biosynthesis in cultured fibroblasts. Naunyn Schmiedebergs ArchPharmacol. 2013;386:303–309. doi: 10.1007/s00210-013-0836-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katewa SD, Kapahi P. Role of TOR signaling in aging and related biological processes in Drosophila melanogaster. Exp Gerontol. 2011;46:382–390. doi: 10.1016/j.exger.2010.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korkmaz A, Yurdakok M, Yigit S, Tekinalp G. Long-term enteral glutamine supplementation in very low birth weight infants: effects on growth parameters. Turk J Pediatr. 2007;49:37–44. [PubMed] [Google Scholar]
- Kowalik S, Śliwa E, Tatara MR, Krupski W, Majcher P, Studziński T. Influence of alpha-ketoglutarate on mineral density and geometrical and mechanical parameters of femora during postnatal life in piglets. Bull. Vet. Inst. Pulawy. 2005;49:107–111. [Google Scholar]
- Kristensen NB, Jungvid H, Fernández JA, Pierzynowski S. Absorption and metabolism of α-ketoglutarate in growing pigs. J Anim Physiol Anim Nutr. 2002;86:239–245. doi: 10.1046/j.1439-0396.2002.00380.x. [DOI] [PubMed] [Google Scholar]
- Lamande SR, Bateman JF. Procollagen folding and assembly: the role of endoplasmic reticulum enzymes and molecular chaperones. Semin Cell Dev Biol. 1999;10:455–464. doi: 10.1006/scdb.1999.0317. [DOI] [PubMed] [Google Scholar]
- Lambert BD, Filip R, Stoll B, Junghans P, Derno M, Hennig U, Souffrant WB, Pierzynowski S, Burrin DG. First-pass metabolism limits the intestinal absorption of enteral α-ketoglutarate in young pigs. J Nutr. 2006;136:2779–2784. doi: 10.1093/jn/136.11.2779. [DOI] [PubMed] [Google Scholar]
- Le Boucher J, Coudray-Lucas C, Lasnier E, Jardel A, Ekindjian OG, Cynober LA. Enteral administration of ornithine alpha-ketoglutarate or arginine alpha-ketoglutarate: a comparative study of their effects on glutamine pools in burn-injured rats. Crit Care Med. 1997;25:293–298. doi: 10.1097/00003246-199702000-00017. [DOI] [PubMed] [Google Scholar]
- Le Boucher J, Cynober LA. Ornithine alpha-ketoglutarate: the puzzle. Nutrition. 1997;14:870–873. doi: 10.1016/s0899-9007(98)00118-x. [DOI] [PubMed] [Google Scholar]
- Lee SS, Lee RY, Fraser AG, Kamath RS, Ahringer J, Ruvkun G. A systematic RNAi screen identifies a critical role for mitochondria in C. elegans longevity. Nat Genet. 2003;33:40–48. doi: 10.1038/ng1056. [DOI] [PubMed] [Google Scholar]
- Lomenick B, Hao R, Jonai N, Chin RM, Aghajan M, Warburton S, Wang J, Wu RP, Gomez F, Loo JA. Target identification using drug affinity responsive target stability (DARTS) Proc Natl Acad Sci USA. 2009;106:21984–21989. doi: 10.1073/pnas.0910040106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luong N, Davies CR, Wessells RJ, Graham SM, King MT, Veech R, Bodmer R, Oldham SM. Activated FOXO-mediated insulin resistance is blocked by reduction of TOR activity. Cell Metab. 2006;4:133–142. doi: 10.1016/j.cmet.2006.05.013. [DOI] [PubMed] [Google Scholar]
- MacFie J, McNaught C. Glutamine and gut barrier function. Nutrition. 2002;18:433–434. doi: 10.1016/S0899-9007(02)00766-9. [DOI] [PubMed] [Google Scholar]
- Meléndez A, Tallóczy Z, Seaman M, Eskelinen EL, Hall DH, Levine B. Autophagy genes are essential for dauer development and life-span extension in C. elegans. Science. 2003;301:1387–1391. doi: 10.1126/science.1087782. [DOI] [PubMed] [Google Scholar]
- Mentaverri R, Kamel S, Wattel A, Prouillet C, Sevenet N, Petit J, Tordjmann T, Brazier M. Regulation of bone resorption and osteoclast survival by nitric oxide: Possible involvement of NMDA-receptor. J Cell Biochem. 2003;88:1145–1156. doi: 10.1002/jcb.10463. [DOI] [PubMed] [Google Scholar]
- Myara I, Charpentier C, Lemonnier A. Prolidase and prolidase deficiency. Life Sci. 1984;34:1985–1998. doi: 10.1016/0024-3205(84)90363-1. [DOI] [PubMed] [Google Scholar]
- Myllyharju J. Prolyl 4-hydroxylases, the key enzymes of collagen biosynthesis. Matrix Biol. 2003;22:15–24. doi: 10.1016/S0945-053X(03)00006-4. [DOI] [PubMed] [Google Scholar]
- Neu J, Shenoy V, Chakrabarti R. Glutamine nutrition and metabolism: where do we go from here? FASEB J. 1996;10:829–837. doi: 10.1096/fasebj.10.8.8666159. [DOI] [PubMed] [Google Scholar]
- Ogle CK, Ogle JD, Mao JX, Simon J, Noel JG, Li B-G, Alexander JW. Effect of glutamine on phagocytosis and bacterial killing by normal and pediatric burn patient neutrophils. J Parenter Enteral Nutr. 1994;18:128–133. doi: 10.1177/0148607194018002128. [DOI] [PubMed] [Google Scholar]
- Palka JA, Phang JM. Prolidase activity in fibroblasts is regulated by interaction of extracellular matrix with cell surface integrin receptors. J Cell Biochem. 1997;67:166–175. doi: 10.1002/(SICI)1097-4644(19971101)67:2<166::AID-JCB2>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- Panosyan EH, Grigoryan RS, Avramis IA, Seibel NL, Gaynon PS, Siegel SE, Fingert HJ, AVRAMIS VI. Deamination of glutamine is a prerequisite for optimal asparagine deamination by asparaginases in vivo (CCG-1961) Anticancer Res. 2004;24:1121–1126. [PubMed] [Google Scholar]
- Parry-Billings M, Calder P, Newsholme E, Evans J. Does glutamine contribute to immunosuppression after major burns? Lancet. 1990;336:523–525. doi: 10.1016/0140-6736(90)92083-T. [DOI] [PubMed] [Google Scholar]
- Pesty FH, Sultan F, Braun B. Glutamine homologues and derivatives: A limiting factor in current artificial nutrition? Nutrition. 1997;13:575–577. doi: 10.1016/S0899-9007(97)00025-7. [DOI] [PubMed] [Google Scholar]
- Pierzynowski S, Sjodin A. Perspectives of glutamine and its derivatives as feed additives for farm animals. J Anim Feed Sci. 1998;7:79–91. [Google Scholar]
- Pierzynowski SG, Filip R, Harrison A. Effect of feed supplementation with alpha-ketoglutarate, combined with vitamin B∼ 6 or C, on the performance and haemoglobin and amino acid levels in growing rats. Bull. Vet. Inst. Pulawy. 2007;51:289–296. [Google Scholar]
- Radzki R, Bienko M, Puzio I, Filip R, Pierzynowski S, Studzinski T. The effect of alpha-ketoglutarate (AKG) on mineralization of femur in ovariectomized rats. Acta Orthop Scand. 2002;73:52. [Google Scholar]
- Rani RS, Leela AC, Rao GN. Effect of dielectric constant on protonation equilibria of l-aspartic acid and ethylenediamine in 1, 2-propanediol-water mixtures. P Natl A Sci India A. 2012;82:313–316. doi: 10.1007/s40010-012-0047-3. [DOI] [Google Scholar]
- Riedel E, Nundel M, Hampl H. alpha-Ketoglutarate application in hemodialysis patients improves amino acid metabolism. Nephron. 1996;74:261–265. doi: 10.1159/000189319. [DOI] [PubMed] [Google Scholar]
- Roth E, Funovics J, Mühlbacher F, Schemper M, Mauritz W, Sporn P, Fritsch A. Metabolic disorders in severe abdominal sepsis: glutamine deficiency in skeletal muscle. Clin Nutr. 1982;1:25–41. doi: 10.1016/0261-5614(82)90004-8. [DOI] [PubMed] [Google Scholar]
- Salvalaggio PR, Campos AC. Bacterial translocation and glutamine. Nutrition. 2002;18:435–437. doi: 10.1016/S0899-9007(02)00770-0. [DOI] [PubMed] [Google Scholar]
- Sawyer DW, Donowitz GR, Mandell GL. Polymorphonuclear neutrophils: an effective antimicrobial force. 1989;11:S1532–S1544. doi: 10.1093/clinids/11.supplement_7.s1532. [DOI] [PubMed] [Google Scholar]
- Schlegel L, Coudray-Lucas C, Barbut F, Le Boucher J, Jardel A, Zarrabian S, Cynober L. Bacterial dissemination and metabolic changes in rats induced by endotoxemia following intestinal E. coli overgrowth are reduced by ornithine α-ketoglutarate administration. J Nutr. 2000;130:2897–2902. doi: 10.1093/jn/130.12.2897. [DOI] [PubMed] [Google Scholar]
- Selman C, Tullet JM, Wieser D, Irvine E, Lingard SJ, Choudhury AI, Claret M, Al-Qassab H, Carmignac D, Ramadani F. Ribosomal protein S6 kinase 1 signaling regulates mammalian life span. Science. 2009;326:140–144. doi: 10.1126/science.1177221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheaffer KL, Updike DL, Mango SE. The target of rapamycin pathway antagonizes pha-4/FoxA to control development and aging. Curr Biol. 2008;18:1355–1364. doi: 10.1016/j.cub.2008.07.097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Śliwa E. 2-Oxoglutaric acid administration diminishes fundectomy-induced osteopenia in pigs. J Anim Physiol Anim Nutr. 2010;94:e86–e95. doi: 10.1111/j.1439-0396.2009.00985.x. [DOI] [PubMed] [Google Scholar]
- Śliwa E, Dobrowolski P, Tatara M, Piersiak T, Siwicki A, Rokita E, Pierzynowski S. Alpha-ketoglutarate protects the liver of piglets exposed during prenatal life to chronic excess of dexamethasone from metabolic and structural changes. J Anim Physiol Anim Nutr. 2009;93:192–202. doi: 10.1111/j.1439-0396.2007.00805.x. [DOI] [PubMed] [Google Scholar]
- Son ED, Choi GH, Kim H, Lee B, Chang IS, Hwang JS. Alpha-ketoglutarate stimulates procollagen production in cultured human dermal fibroblasts, and decreases UVB-induced wrinkle formation following topical application on the dorsal skin of hairless mice. Biol Pharm Bull. 2007;30:1395–1399. doi: 10.1248/bpb.30.1395. [DOI] [PubMed] [Google Scholar]
- Spencer GJ, McGrath CJ, Genever PG. Current perspectives on NMDA-type glutamate signalling in bone. Int J Biochem Cell Biol. 2007;39:1089–1104. doi: 10.1016/j.biocel.2006.11.002. [DOI] [PubMed] [Google Scholar]
- Stanfel MN, Shamieh LS, Kaeberlein M, Kennedy BK. The TOR pathway comes of age. Biochim. Biophys. Acta. 2009;1790:1067–1074. doi: 10.1016/j.bbagen.2009.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoll B, McNelly S, Buscher HP, Häussinger D. Functional hepatocyte heterogeneity in glutamate, aspartate and α-ketoglutarate uptake: A histoautoradiographical study. Hepatology. 1991;13:247–253. doi: 10.1002/hep.1840130208. [DOI] [PubMed] [Google Scholar]
- Tapiero H, Mathe G, Couvreur P, Tew K. II. Glutamine and glutamate. Biomed Pharmacother. 2002;56:446–457. doi: 10.1016/S0753-3322(02)00285-8. [DOI] [PubMed] [Google Scholar]
- Tatara M, Brodzki A, Krupski W, Silmanowicz P, Majcher P, Pierzynowski S, Studziński T. Effects of alpha-ketoglutarate on bone homeostasis and plasma amino acids in turkeys. Poult Sci. 2005a;84:1604–1609. doi: 10.1093/ps/84.10.1604. [DOI] [PubMed] [Google Scholar]
- Tatara M, Tygesen MP, Sawa-Wojtanowicz B, Krupski W, Majcher P, Harrison AP. Bone development: The effect of short-term alpha-ketoglutarate administration on long-term mechanical properties of ribs in ram lambs. Small Ruminant Res. 2007;67:179–183. doi: 10.1016/j.smallrumres.2005.09.031. [DOI] [Google Scholar]
- Tatara MR, Silmanowicz P, Majcher P, Krupski W, Studziński T. Influence of alpha-ketoglutarate on cortical bone atrophy after denervation of the humerus in turkey. Bull. Vet. Inst. Pulawy. 2005b;49:113–116. [Google Scholar]
- Taylor A. Osteoblastic glutamate receptor function regulates bone formation and resorption. J Musculoskelet Neuronal Interact. 2002;2:285–290. [PubMed] [Google Scholar]
- Tocaj A, Filip R, Lindergard B, Wernerman J, Studzinski T, Ohman K, Pierzynowski S. Alpha-ketoglutarate (AKG) inhibit osteoporosis development in postmenopausal women; Journal of Bone and Mineral Research; 2003. pp. S267–S267. Amer Soc Bone & Mineral Res 2025 M St, Nw, Ste 800, Washington Dc 20036-3309 USA. [Google Scholar]
- Toivonen JM, Walker GA, Martinez-Diaz P, Bjedov I, Driege Y, Jacobs HT, Gems D, Partridge L. No influence of Indy on lifespan in Drosophila after correction for genetic and cytoplasmic background effects. PLoS Genet. 2007;3:e95. doi: 10.1371/journal.pgen.0030095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tritos NA, Biller BM. Growth hormone and bone. Curr Opin Endocrinol Diabetes Obes. 2009;16:415–422. doi: 10.1097/MED.0b013e3283319e6d. [DOI] [PubMed] [Google Scholar]
- Tsang WY, Sayles LC, Grad LI, Pilgrim DB, Lemire BD. Mitochondrial respiratory chain deficiency in Caenorhabditis elegans results in developmental arrest and increased life span. J Biol Chem. 2001;276:32240–32246. doi: 10.1074/jbc.M103999200. [DOI] [PubMed] [Google Scholar]
- Urban J, Soulard A, Huber A, Lippman S, Mukhopadhyay D, Deloche O, Wanke V, Anrather D, Ammerer G, Riezman H. Sch9 Is a Major Target of TORC1 in Saccharomyces cerevisiae. Mol. Cell. 2007;26:663–674. doi: 10.1016/j.molcel.2007.04.020. [DOI] [PubMed] [Google Scholar]
- Vellai T, Takacs-Vellai K, Zhang Y, Kovacs AL, Orosz L, Müller F. Influence of TOR kinase on lifespan in C. elegans. Nature. 2003;426:620. doi: 10.1038/426620a. [DOI] [PubMed] [Google Scholar]
- Velvizhi S, Dakshayani KB, Subramanian P. Effects of α-ketoglutarate on antioxidants and lipid peroxidation products in rats treated with ammonium acetate. Nutrition. 2002;18:747–750. doi: 10.1016/S0899-9007(02)00825-0. [DOI] [PubMed] [Google Scholar]
- Wang Y, Zhou Y, Graves DT. FOXO transcription factors: their clinical significance and regulation. Biomed Res Int. 2014;2014:925350. doi: 10.1155/2014/925350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb AE, Brunet A. FOXO transcription factors: key regulators of cellular quality control. Trends Biochem Sci. 2014;39:159–169. doi: 10.1016/j.tibs.2014.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welborn JR, Shpun S, Dantzler WH, Wright SH. Effect of α-ketoglutarate on organic anion transport in single rabbit renal proximal tubules. Am J Physiol Renal Physiol. 1998;274:F165–F174. doi: 10.1152/ajprenal.1998.274.1.F165. [DOI] [PubMed] [Google Scholar]
- Wernerman J, Hammarqvist F, Vinnars E. α-Ketoglutarate and postoperative muscle catabolism. Lancet. 1990;335:701–703. doi: 10.1016/0140-6736(90)90811-I. [DOI] [PubMed] [Google Scholar]
- Wirén M, Permert J. α-ketoglutarate-supplemented enteral nutrition: effects on postoperative nitrogen balance and muscle catabolism. Nutrition. 2002;18:725–728. doi: 10.1016/S0899-9007(02)00844-4. [DOI] [PubMed] [Google Scholar]
- Wu G, Fang YZ, Yang S, Lupton JR, Turner ND. Glutathione metabolism and its implications for health. J Nutr. 2004;134:489–492. doi: 10.1093/jn/134.3.489. [DOI] [PubMed] [Google Scholar]
- Wullschleger S, Loewith R, Hall MN. TOR signaling in growth and metabolism. Cell. 2006;124:471–484. doi: 10.1016/j.cell.2006.01.016. [DOI] [PubMed] [Google Scholar]
- Yeh SL, Lai YN, Shang HF, Lin MT, Chen WJ. Effects of glutamine supplementation on innate immune response in rats with gut-derived sepsis. Br J Nutr. 2004;91:423–430. doi: 10.1079/BJN20031069. [DOI] [PubMed] [Google Scholar]
- Ziegler TR, Daignault NM. Glutamine regulation of human immune cell function. Nutrition. 2000;16:458–459. doi: 10.1016/S0899-9007(00)00359-2. [DOI] [PubMed] [Google Scholar]
- Zimmerman JJ, Ringer TV. Inflammatory host responses in sepsis. Crit Care Clin. 1992;8:163–189. [PubMed] [Google Scholar]