Abstract
Acute myocardial infarction (AMI) remains a leading cause of morbidity and mortality worldwide. The exploration of new biomarkers with high sensitivity and specificity for early diagnosis of AMI therefore becomes one of the primary task. In the current study, we aim to detect whether there is any heart specific long noncoding RNA (lncRNA) releasing into the circulation during AMI, and explore its function in the neonatal rat cardiac myocytes injury induced by H2O2. Our results revealed that the cardiac-specific lncRNA MHRT (Myosin Heavy Chain Associated RNA Transcripts) was significantly elevated in the blood from AMI patients compared with the healthy control (*p<0.05). Using an in vitro neonatal rat cardiac myocytes injury model, we demonstrated that lncRNA MHRT was upregulated in the cardiac myocytes after treatment with hydrogen peroxide (H2O2) via real-time RT-PCR (qRT-PCR). Furthermore, we knockdowned the MHRT gene by siRNA to confirm its roles in the H2O2-induced cardiac cell apoptosis, and found that knockdown of MHRT led to significant more apoptotic cells than the non-target control (**p<0.01), indicating that the lncRNA MHRT is a protective factor for cardiomyocyte and the plasma concentration of MHRT may serve as a biomarker for myocardial infarction diagnosis in humans AMI.
Keywords: Acute myocardial infarction, Long noncoding RNAs, MHRT, Apoptosis
According to the whole-genome sequencing project, it has been revealed that only ∼2% of the human genome can be translated into proteins and the others are non-coding RNAs (ncRNAs) (Mercer and Mattick, 2013). They are classified into small regulatory ncRNAs defined as those with <200 nucleotides in length and long ncRNAs (lncRNAs) with >200 nucleotides in length (Ounzain et al., 2013). Recently, many lncRNAs have been identified as important regulators in gene transcription and translation, cell differentiation, ontogenetic, genetic, epigenetic and other cellular activities (Mercer et al., 2009; Kanduri, 2015).
Acute myocardial infarction (AMI) is one of the most serious cardiovascular diseases (Li et al., 2013). An early and timely diagnosis engages for an immediate initiation of reperfusion therapy to reduce the mortality rate largely (Pedrazzini, 2015). Recently, some miRNAs were reported to be deregulated in myocardial infarction, which could be used as the biomarker and played important roles in cell apoptosis (Wang et al., 2014). However, studies of lncRNAs in the cardiovascular diseases are still in their infancy, although ample of evidence suggests that lncRNAs are also involved in common cardiovascular diseases (Jiang and Ning, 2015). Several lncRNAs are regulated during acute myocardial infarction and heart failure (Vausort et al., 2014), whereas others control hypertrophy, mitochondrial function and apoptosis of cardiomyocytes (Uchida and Dimmeler, 2015). Considering the complex genetic variants in AMI, further investigation is needed to ascertain whether lncRNAs are associated with AMI.
The lncRNA MHRT (Myosin Heavy Chain Associated RNA Transcripts) is an up-to-the-minute identified cardioprotective lncRNA, and its transcripts are demonstrated as a new ATP-dependent chromatin-remodelling factors lncRNA for heart failure. In mice, the Mhrt lncRNA transcripts are cardiac-specific and abundant in adult hearts; human MHRT also originates from MYH7 loci and is repressed in various types of myopathic hearts, suggesting a conserved lncRNA mechanism in human cardiomyopathy (Han et al., 2014). However, expressions and roles of MHRT lncRNA in other heart diseases have not been explored till now. In this study, we aim to study the level of serum lncRNA MHRT in patients with AMI, which could be used to detect and monitor the myocardial injury, and explore functions of MHRT in the neonatal rat cardiac myocytes injury induced by H2O2.
MATERIALS AND METHODS
Patient samples
We assessed 47 AMI patients admitted to the Department of Emergency and the Department of Cardiology in the Maternity and Child Care Hospital of Weihai City from March 2011 to October 2013. The inclusion criteria for patients with AMI were based on the newly developed universal definition of MI (Thygesen et al., 2007). Briefly, these patients with AMI were clinically diagnosed by biochemical markers (cardiac troponin I), acute ischaemic-type chest pain, electrocardiogram change, and coronary angiography. Patients were excluded if they had received intravenous thrombolytic or anticoagulant therapy before the initial blood samples were obtained. Additionally, 28 adult healthy volunteers were enrolled in this study. This study was approved by the Medical Ethics Committee in Maternity and Child Care Hospital of Weihai City. Signed informed consent was obtained from all the participants before enrolment.
Cell culture
In brief, the hearts from 1- to 2- day-old Sprague-Dawley rats were isolated after hypothermia anesthesia immersion in ice water and placed in ice-cold phosphate-buffered saline (PBS) solution. After repeated rinsing, the atria were cut off, and the ventricles were minced with scissors. The minced tissue and ventricular cells were dispersed by digestion with 0.45 mg/ml of collagenase type IV (Sigma-Aldrich, St. Louis, MO, USA), 0.1% trypsin, and 15 μg/ml of DNase I (Life Technologies, Inc., Grand Island, NY, USA). Cardiomyocytes (0.5×106 cells/ml) were cultured in Dulbecco's modified Eagle's medium supplemented with 10% serum, 4 μg/ml of transferrin, 0.7 ng/ ml of sodium selenite, 2 g/L of bovine serum albumin (fraction V), 3 mmol/L of pyruvic acid, 15 mmol/L of HEPES, 100 μmol/L of ascorbic acid, 100 μg/ml of ampicillin, 5 μg/ml of linoleic acid, 1% penicillin and 1% streptomycin, and 100 μmol/L of 5-bromo-2′-deoxyuridine, and seeded into six-well plates.
siRNA transfection
The MHRT specific siRNA was commercially synthesized by Ribo Ltd. (Guangzhou, China), and siRNA transfection was performed using Lipofectamine 2000 (Invitrogen, Carlsbad, CA, USA). In brief, 5 μl of siRNA was added into 245 μl Opti-MEM medium, 3 μl of Lipofectamine 2000 was added into 247 μl Opti-MEM medium and then mixed the siRNA mixture and the Lipofectamine 2000 mixture together for 30 minutes at room tempreture. The mixture was added to the plated cells and incubated for 6 h before replacing the medium. Total RNA were prepared 48 h after transfection and were used for qRT-PCR analysis.
RNA extraction and qRT-PCR analyses
Total RNAs were extracted either from cardiomyocytes or blood by using TRIzol reagent (Invitrogen, Carlsbad, CA, USA) according to the manufacturer’s protocol. RNA was reversely transcribed to cDNA by using a Reverse Transcription Kit (Takara, Dalian, China). Real-time PCR was performed with SYBR Green (Takara, Dalian, China). 5S rRNA was used as reference for MHRT in serum and 18S rRNA was used in rat cardiomyocytes. Each sample was analyzed in triplicate. The primers were listed as follows: MHRT(Homo): F 5′-ACACGGCGTTCTTGAGTTT-3′, R 5′-AGTATGAGGAGTCGCAGTCG-3′; Mhrt(Rat): F 5′-TCATTGCGGCTGCGTGTC-3′, R 5′-GCCCAGCTAGAGTTCAACCAGA-3′; 18S rRNA: F 5′-GTAACCCGTTGAACCCCATT-3′, R 5′-CCATCCAATCGGTAGTAGCG-3′; 5S rRNA: F 5′-ATCAGACGGGATGCGGT-3′, R 5′-ACQGCATCCCGTCTGAT-3′.
Flow-cytometric analysis
200 μM of H2O2 (Sigma-Aldrich, St Louis, MO, USA) was used for mimicking oxidative stress-induced injury in cardiomyocytes. The cardiomyocytes were harvested after 12 h treatment with H2O2. After the double staining of Annexin V-FITC and propidium iodide (PI), cardiomyocytes were subjected to apoptosis assay using flow cytometry and analyzed with a Cell Quest software (BD Biosciences, CA, USA).
TUNEL assay
Cultured cardiomyocyte apoptosis were also measured by terminal deoxynucleotide transferase dUTP nick end labelling (TUNEL) staining. Briefly, cardiac myocytes cultured on coverslips in 6-well plates were fixed in 4% paraformaldehyde. The TUNEL staining was done using the in situ cell death detection kit (Minneapolis, MN, USA) according to the manufacturer’s protocol. The numbers of TUNEL-positive cells and the total cells were counted under a fluorescence microscope.
Statistical analyses
SPSS 17.0 (SPSS Inc., CA, USA) was used for statistical analysis. Results are expressed as the mean ± SEM. The correlation between MHRT and cTnT expression was analyzed using GraphPad Software, p<0.05 was defined as significant negative correlation. Statistical differences among groups were analyzed by two-way analysis of variance, followed by the least significant difference test. Statistical significance was indicated when p<0.05.
RESULTS
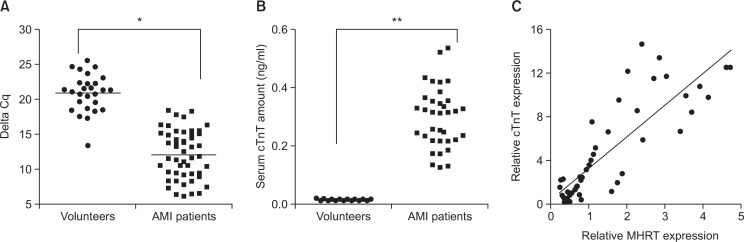
Plasma MHRT level is highly elevated after AMI
We firstly detected the serum level of the heart-associated lncRNA MHRT in AMI patients' plasma compared with health volunteers. All blood samples were collected within 1 hour after hospitalization. Thereafter, we compared the delta Cq values of the both groups, which indicates that a higher delta Cq value corresponds to a lower expression of the genes. Our result showed that the lncRNA MHRT was greatly elevated in the AMI patient group compared with the control subjects (Fig. 1A). Subsequently, we assessed the correlation between the plasma level of the lncRNA MHRT with serum levels of cTnT (cardiac troponin T), a cardiac injury markers. As shown in the Fig. 1B, cTnT concentrations were significantly increased in AMI patients compared with health volunteers. These results indicated lncRNA MHRT correlates with cardiac injury and might be served as a new biomarker for AMI diagnosis (Fig. 1B). In addition, we also detect the correlation of MHRT and the nTnT. Our results showed a negative correlation between the mRNA level of MHRT and cTnT (R2=0.7106, p<0.05), which strongly support the possibility that MHRT may serve as a biomarker for AMI diagnosis (Fig. 1C).
Fig. 1.
Plasma MHRT level is highly elevated in AMI patients. (A) Expression level of the non-coding RNA MHRT was detected via qRT-PCR analysis in health volunteers and AMI patients. (B) The amount of cTnT in blood was detected via automatic electro-chemiluminescence immunoassay analyzer in health volunteers and AMI patients. In this figure, we compared the delta Cq values of the both groups, indicating that the higher delta Cq value corresponds to the lower expression of the genes. (C) correlation between the MHRT and cTnT was analyzed using GraphPad Software. *p<0.05 compared with control; **p<0.01 compared with control.
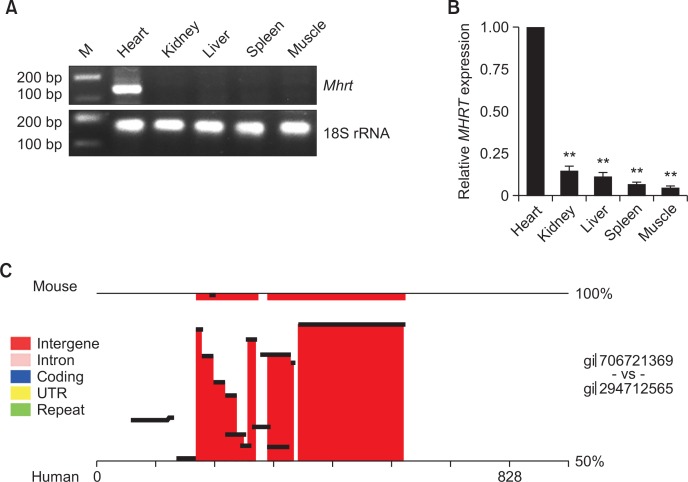
MHRT is a myocardium specific lncRNA
Next, we set out to determine whether MHRT is a myocardium specific lncRNA, and evaluate the value as a potential biomarker for myocardial injury. For this purpose, the MHRT expression was detected in different the rat organs, including heart, kidney, liver, spleen and muscle using PCR. The result suggested that MHRT are produced exclusively in the heart (Fig. 2A), and when we set the relative expression of MHRT in the heart as a standard, the expressions of MHRT in the other organs were significantly lower (Fig. 2B). Furthermore, we compared the MHRT sequence in human and mouse with software rVista 2.0 (http://zpicture.dcode.org/), the result showed that there is conserved sequence between human and mouse (Fig. 2B), indicating that MHRT might exert its biological function in cardiomyocytes.
Fig. 2.
MHRT is a myocardium specific lncRNA. (A) RT-PCR showed the mRNA expression of MHRT in the rat organs, including heart, kidney, liver, spleen, and muscle. The cycles for PCR amplification was 25 cycles and the reaction volume was 25 μl. (B) Expression profile of the MHRT was confirmed in different tissues via qRT-PCR analysis, including rat heart, kidney, liver, spleen and muscle. The experiment was repeated at least three times. (C) The conservative analysis was carried on via rVista 2.0 software, and the conserved sequence was showed with red. **p<0.01 compared with control.
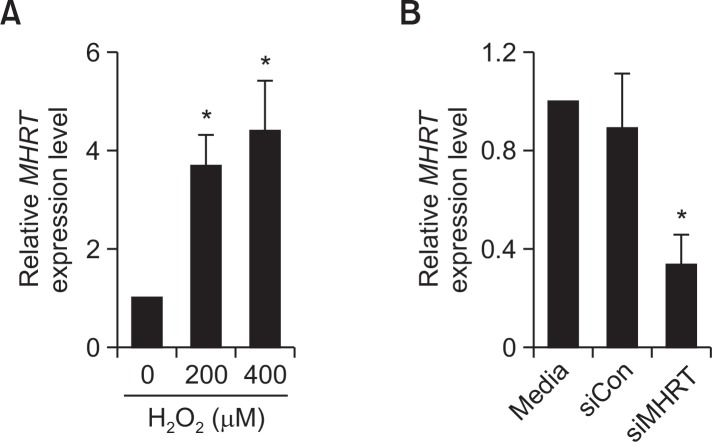
H2O2 induced MHRT expression in cardiomyocytes
We determined concentrations of H2O2 for mimicking oxidative stress-induced injury in cardiomyocytes. In the study, cardiomyocytes were treated with 200 μM and 400 μM of H2O2 for 12 hours, and the result showed that the expression of MHRT was increased by nearly four-fold at the concentration of 200 μM, however, there was no significant difference between the treatment of 200 μM and 400 μM (Fig. 3A). To further determine the biological function of MHRT in cardiomyocytes, siR-NA specially targeting MHRT was designed and transfected to cardiomyocytes, and the qRT-PCR analysis was employed to confirm the efficiency of knockdown. As shown in the Fig. 3B, MHRT mRNA level has been successfully suppressed in the rat cardiomyocytes.
Fig. 3.
H2O2 induces MHRT expression in cardiomyocytes. (A) Expression level of MHRT was verified via qRT-PCR assay in cardiomyocytes exposed to different concentration H2O2 for 12 h. (B) The efficiency of MHRT knockdown was examined in cardiomyocytes via qRT-PCR assay. Both experiments were repeated at least three times. *p<0.05 compared with control.
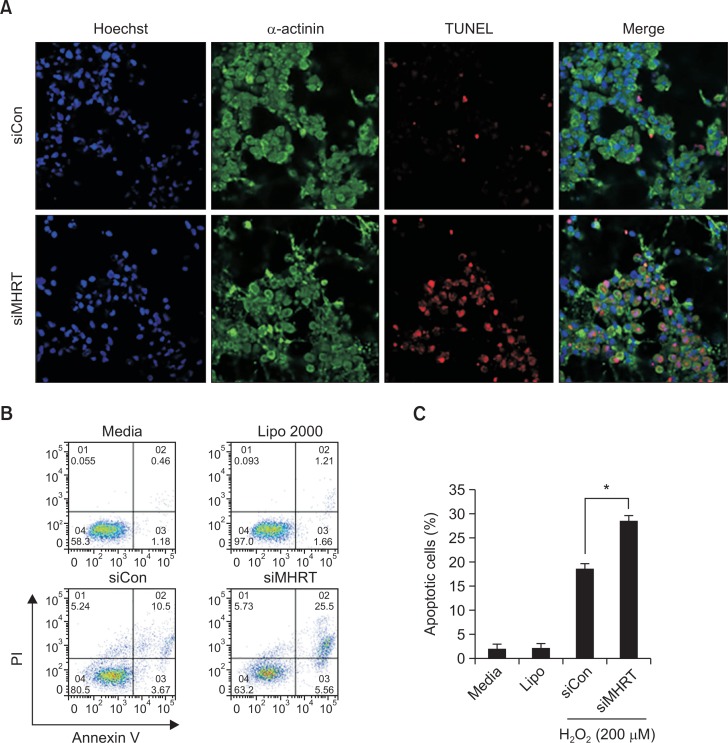
MHRT Knockdown enhances the apoptosis in cardiomyocytes
Therefore, we evaluated the function of lncRNA MHRT in cardiomyocytes. To eliminate the effect of MHRT on apoptosis, we used siRNA to downregulate MHRT gene expression and then treated with 200 μM of H2O2 in cardiomyocytes for 12 hours. We employed the TUNEL assay to show the apoptotic cells, as well as immunocytochemistry staining for α-actinin, which is a mature myocardial marker, to identify the cardiomyocytes. At the same time, flow cytometry with FITC-conjugated Annexin V and PI staining was also used to detect the apoptotic cells. Both of TUNEL assay (Fig. 4A) and Annexin-V/PI double staining assays (Fig. 4B) showed that the percentage of apoptotic cells induced by H2O2 treatment was significantly increased in the MHRT knockdown cells (siMHRT) compared with siRNA control (siCon). These results indicated that MHRT was resistant to H2O2-induced apoptosis of cardiomyocytes.
Fig. 4.
MHRT Knockdown enhances apoptosis in cardiomyocytes. (A) The influence on apoptosis with MHRT knockdown was examined via TUNEL assay. Blue, Hoest staining for nuclear; green, FITC staining for α-actinin protein; red, TUNEL positive staining for apoptotic cells. (B) The effect of MHRT on apoptosis was determined via Annexin-V/PI double staining assays. The upper right quadrant and lower right quadrant indicated apoptosis cells. (C) Analysis of percentage of apoptotic cells in the flow cytometry experiment. Both experiments were repeated at three times, the representative images was chosen for presentation (*p<0.05 compared with control).
DISCUSSION
AMI is one of the major causes of mortality and morbidity in the world, heart of patients with AMI cannot continue to function without adequate blood flow, and if it is severely compromised, death is inevitable (Ounzain et al., 2014). Therefore, specific and early-stage biomarkers, which can be used to establish a timely diagnosis in patients with AMI, become more and more important in clinic (Xu et al., 2012; Yao et al., 2014).
There is an explosion of interest in regulatory noncoding RNAs, especially lncRNAs. LncRNAs act as regualtors to target specific elements in both the transcriptome and the genome (Batista and Chang, 2013). They also act as specific molecular scaffolds for protein-protein interactions and play roles as molecular decoys in both nucleic acids and proteins (Mercer and Mattick, 2013). Hence, lncRNAs are emerging primarily as important regulators of gene expression at the transcriptional and post-transcriptional level. They demonstrate distinctive roles in modulating tissue-specific epigenetic states and nuclear organization, which are critical for correct gene regulatory network activity (Batista and Chang, 2013).
However, the role of lncRNA in adult hearts is rarely known, let alone to identify a specific lncRNA that can serve as the biomarker for AMI. As to the lncRNA MHRT, it was firstly identified by Han et al as a cardiac-specific lncRNA and abundant in adult hearts (Han et al., 2014), Wu et al described MHRT as molecular crowbar unravel insights into heart failure treatment (Wu and Arora, 2015). However, the function of MHRT in AMI patients is still unclear. In this study, the expression of MHRT was evaluated in blood from AMI patients and we revealed that the expression level of MHRT was significantly upregulated in the very early stage of AMI, which indicated MHRT might be used as the biomarker for AMI.
It is well known that high levels of reactive oxygen species (ROS)-induced cardiac cell injury plays an important role in the pathogenesis of many heart diseases including AMI (Berg et al., 2005). Recent studies have revealed that ROS, such as superoxide and hydrogen peroxide (H2O2), can elicit expression changes of multiple genes and is partly responsible for ROS-mediated cardiac cell injury. Currently, the effects of ROS on lncRNA expression and the roles of lncRNAs in ROS-mediated injury on cardiac myocytes are uncertain to our knowledge. In this paper, we created a model of H2O2-induced oxidative stress in rat cardiomyocytes, and found that H2O2 exposure led to the elevated expression of MHRT in cardiomyocytes. Furthermore, the potential protective effect of MHRT on H2O2-induced oxidative stress was investigated in rat cardiomyocytes in vitro, which offered an original therapeutic target for AMI in future.
In conclusion, our study reported for the first time that the lncRNA MHRT is a protective factor for cardiomyocyte and the plasma concentration of MHRT may serve as a biomarker for myocardial infarction diagnosis in humans’ AMI.
Acknowledgments
This study was supported by the Scientific Research Program of Weihai City (No. 2012GNS0428).
Footnotes
INTEREST OF CONFLICTS
All authors declare no interest of conflicts.
REFERENCES
- Batista PJ, Chang HY. Long noncoding RNAs: cellular address codes in development and disease. Cell. 2013;152:1298–1307. doi: 10.1016/j.cell.2013.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg K, Jynge P, Bjerve K, Skarra S, Basu S, Wiseth R. Oxidative stress and inflammatory response during and following coronary interventions for acute myocardial infarction. Free Radic Res. 2005;39:629–636. doi: 10.1080/10715760400028027. [DOI] [PubMed] [Google Scholar]
- Han P, Li W, Lin CH, Yang J, Shang C, Nurnberg ST, Jin KK, Xu W, Lin CY, Lin CJ, Xiong Y, Chien HC, Zhou B, Ashley E, Bernstein D, Chen PS, Chen HS, Quertermous T, Chang CP. A long noncoding RNA protects the heart from pathological hypertrophy. Nature. 2014;514:102–106. doi: 10.1038/nature13596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang X, Ning Q. The emerging roles of long noncoding RNAs in common cardiovascular diseases. Hypertens Res. 2015;38:375–379. doi: 10.1038/hr.2015.26. [DOI] [PubMed] [Google Scholar]
- Kanduri C. Long noncoding RNAs: lessons from genomic imprinting. Biochim. Biophys. Acta. 2015. [Epub ahed of print] [DOI] [PubMed]
- Li C, Fang Z, Jiang T, Zhang Q, Liu C, Zhang C, Xiang Y. Serum microRNAs profile from genome-wide serves as a fingerprint for diagnosis of acute myocardial infarction and angina pectoris. BMC Med. Genomics. 2013;6:16. doi: 10.1186/1755-8794-6-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercer TR, Dinger ME, Mattick JS. Long non-coding RNAs: insights into functions. Nat. Rev. Genet. 2009;10:155–159. doi: 10.1038/nrg2521. [DOI] [PubMed] [Google Scholar]
- Mercer TR, Mattick JS. Structure and function of long noncoding RNAs in epigenetic regulation. Nat Struct Mol Biol. 2013;20:300–307. doi: 10.1038/nsmb.2480. [DOI] [PubMed] [Google Scholar]
- Ounzain S, Crippa S, Pedrazzini T. Small and long non-coding RNAs in cardiac homeostasis and regeneration. Biochim. Biophys. Acta. 2013;1833:923–933. doi: 10.1016/j.bbamcr.2012.08.010. [DOI] [PubMed] [Google Scholar]
- Ounzain S, Pezzuto I, Micheletti R, Burdet F, Sheta R, Nemir M, Gonzales C, Sarre A, Alexanian M, Blow MJ, May D, Johnson R, Dauvillier J, Pennacchio LA, Pedrazzini T. Functional importance of cardiac enhancer-associated noncoding RNAs in heart development and disease. J Mol Cell Cardiol. 2014;76:55–70. doi: 10.1016/j.yjmcc.2014.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedrazzini T. [In the heart of noncoding RNA: a long way to go] Med Sci. 2015;31:261–267. doi: 10.1051/medsci/20153103011. [DOI] [PubMed] [Google Scholar]
- Thygesen K, Alpert JS, White HD, Joint, E. S. C. A. A. H. A. W. H. F. T. F. f. t. R. o. M. I. Universal definition of myocardial infarction. J Am Coll Cardiol. 2007;50:2173–2195. doi: 10.1016/j.jacc.2007.09.011. [DOI] [PubMed] [Google Scholar]
- Uchida S, Dimmeler S. Long noncoding RNAs in cardiovascular diseases. Circ Res. 2015;116:737–750. doi: 10.1161/CIRCRESAHA.116.302521. [DOI] [PubMed] [Google Scholar]
- Vausort M, Wagner DR, Devaux Y. Long noncoding RNAs in patients with acute myocardial infarction. Circ Res. 2014;115:668–677. doi: 10.1161/CIRCRESAHA.115.303836. [DOI] [PubMed] [Google Scholar]
- Wang J, Jia Z, Zhang C, Sun M, Wang W, Chen P, Ma K, Zhang Y, Li X, Zhou C. miR-499 protects cardiomyocytes from H2O2-induced apoptosis via its effects on Pdcd4 and Pacs2. RNA Biol. 2014;11:339–350. doi: 10.4161/rna.28300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu C, Arora P. Long noncoding Mhrt RNA: molecular crowbar unravel insights into heart failure treatment. Circ Cardiovasc Genet. 2015;8:213–215. doi: 10.1161/CIRCGENETICS.115.001019. [DOI] [PubMed] [Google Scholar]
- Xu J, Zhao J, Evan G, Xiao C, Cheng Y, Xiao J. Circulating microRNAs: novel biomarkers for cardiovascular diseases. J Mol Med. 2012;90:865–875. doi: 10.1007/s00109-011-0840-5. [DOI] [PubMed] [Google Scholar]
- Yao Y, Du J, Cao X, Wang Y, Huang Y, Hu S, Zheng Z. Plasma levels of microRNA-499 provide an early indication of perioperative myocardial infarction in coronary artery bypass graft patients. PLoS One. 2014;9:e104618. doi: 10.1371/journal.pone.0104618. [DOI] [PMC free article] [PubMed] [Google Scholar]