Summary
A provider-assisted, counseling-based, pediatric HIV disclosure model was developed and implemented at two tertiary-care hospitals in Bangkok, Thailand. All undisclosed perinatally acquired HIV-infected children, ages 7–18 years, and their caretakers were offered the four-step disclosure service, including: screening, readiness assessments and preparation, disclosure sessions, and follow-up evaluations. To assess psychosocial outcomes of disclosure, we compared the scores of the Children Depression Inventory and the PedsQL 4.0™ at baseline and at 2-month and 6-month follow-up visits, and compared the scores of the Child Behavioral Checklist at baseline and at 6-month follow-up. Disclosure was made to 186 children, 160 of whom completed post-disclosure assessments. The median Children’s Depression Inventory score in 135 children decreased significantly from 11 at baseline to 8 at 2-month and 6-month follow-up (p < 0.01). The median PedsQL 4.0™ scores in 126 children increased significantly from 78 at baseline to 80 at 2-month and 84 at 6-month follow-up (p = 0.04). The median Child Behavioral Checklist scores were not significantly changed. In conclusion, pediatric HIV diagnosis disclosure using this model was found to have positive effect on the children’s mood and quality of life, and no negative effect on children’s behaviours. This disclosure program should be expanded to improve psychosocial health of HIV-infected children.
Keywords: HIV, pediatric, disclosure, psychosocial, outcomes, Thailand
Introduction
With increased availability of highly active anti-retroviral therapy, increasing numbers of children with perinatally-acquired HIV infection are surviving into adolescence and adulthood. Disclosure of HIV diagnosis to these children is presently one of the clinical challenges for caretakers and healthcare providers. The American Academy of Pediatrics recommends that school-aged children and adolescents living with HIV should be told about their diagnosis.1 Adolescents, particularly, should be fully informed about their HIV status in order to maximise their involvement in care and to reduce the risk of virus transmission through sexual behaviours.2,3
Despite this recommendation, it was found that a substantial proportion of HIV-infected children world-wide had not been made fully aware of their HIV diagnosis.4 Clinical reports from western countries, as well as from Thailand, suggest that caretakers have a number of reasons for not disclosing HIV diagnosis to their infected children, including concerns that children are too young to understand or to keep the diagnosis secret, and fears that children might be psychologically harmed by the disclosure.5
Studies on the effects of HIV diagnosis disclosure on HIV-infected children are limited and reveal mixed results. Bachanas et al.6 found that HIV-infected children who had not been told their diagnosis tend to report more psychological distress than children who knew that they have HIV disease. On the other hand, New et al.7 found that children who were aware of their HIV diagnosis were more likely to have internalising behavioural problems. Other studies, however, found no association between disclosure and psychosocial outcomes.8,9 The variation of the results might be in part due to the difference in the population and study method of these studies.
As specific disclosure guidelines are lacking and data on disclosure outcomes are limited, starting in 2005 a group of multidisciplinary professionals involved in HIV care at Siriraj Hospital, Queen Sirikit National Institute for Child Health (QSNICH), and the Thailand MOPH-US CDC Collaboration developed a provider-assisted pediatric HIV disclosure model and implemented the model at the two hospitals (Siriraj and QSNICH). The model program provides counseling to caretakers to assess their readiness for and preparing them for the disclosure process. We recently reported the development and the evaluation of the model.10 It was found that the model was feasible to implement, and beneficial for healthcare providers to use as a guideline on supporting HIV-infected children and their caretakers. The aim of this study was to assess the changes in psychosocial status in the children after disclosure. We hypothesised that disclosure by this model would not be associated with negative psychological outcomes, as measured by standardised instruments for children’s behaviours, mood, and health-related quality of life.
Methods
Study design and population
This was an observational prospective cohort study to evaluate psychosocial outcomes in children after their HIV diagnosis was disclosed to them. Between February 2005 and December 2008, all caretakers of perinatally HIV-infected children aged 7–18 years who were receiving treatment at either of the two pediatric HIV treatment centers (Siriraj Hospital and QSNICH) and unaware of their HIV status were offered the HIV diagnosis disclosure service. Exclusion criteria included children with severe cognitive impairment, psychosis, suicidality, or urgent medical conditions, and caretakers with severe medical or psychiatric conditions that would interfere with participation in the program.
The disclosure model
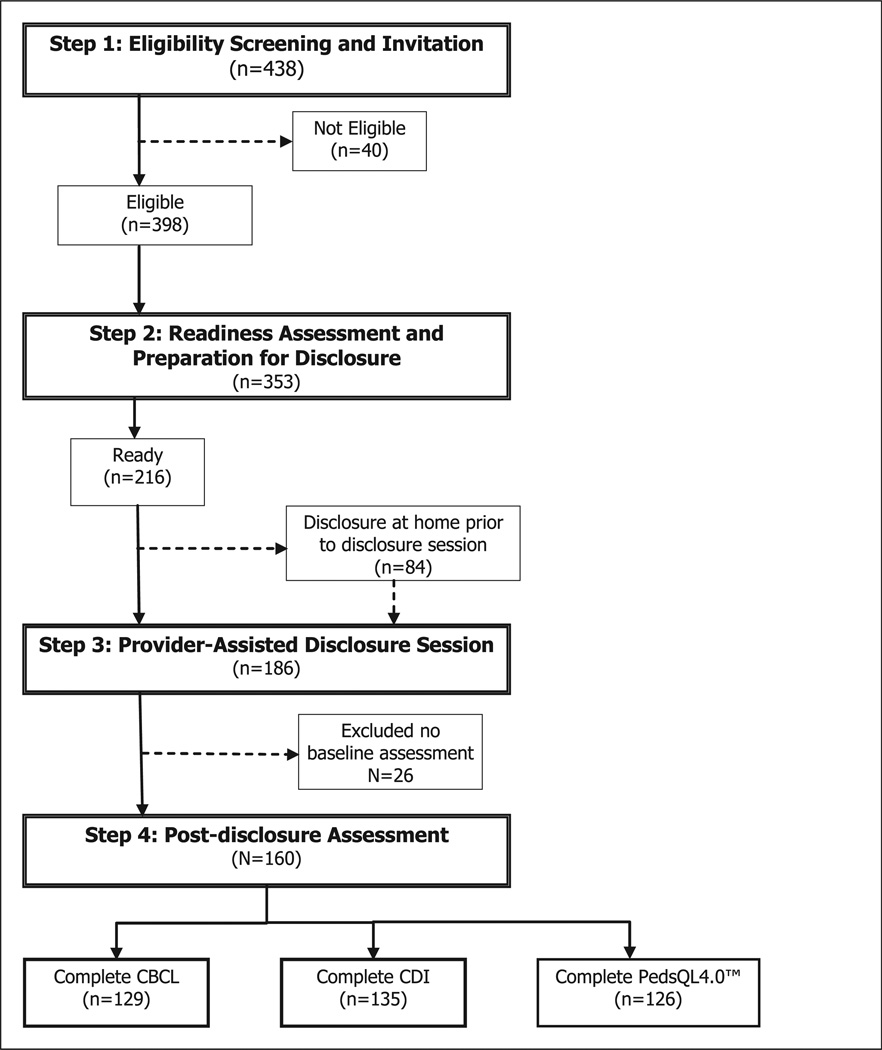
The disclosure model is a counseling-based model that guides healthcare providers to assist caretakers in disclosing HIV status to infected children, providing HIVrelated health information to children and caretakers, and supporting children’s emotional reactions related to disclosure. The model comprises four steps as outlined in Figure 1.
Figure 1.
Disclosure algorithm and number of children participating in the disclosure program and received psychometric assessments, Bangkok, Thailand, 2005–2009.
The first step of the model involves screening HIV-infected children and their caretakers for eligibility and offering disclosure counseling service to the caretakers. In the step of readiness assessment (step 2), counselors interview caretakers separately from their child following the program guidelines. The guidelines are written as a manual with clear instruction how to conduct counseling (available online at www.cqihiv.com/ViewDocumentDetail.aspx?ID = 3&Title=Pediatric HIV Disclosure Manual). In this step, counselors explore caretakers’ attitudes, fears, and perceptions on benefits and disadvantages regarding disclosure. Through the counseling process, counselors work with caretakers to determine the caretaker’s and the child’s readiness. A caretaker was considered ready if the caretaker (a) perceived that their child was ready and (b) had made the decision to disclose the child’s HIV diagnosis to the child. Counselors and caretakers had to agree on the child’s readiness upon review of the child’s clinical and psychosocial status, including developmental level and ability to communicate. If it is determined that both caretakers and children are ready,10 a provider-assisted disclosure session (step 3) is scheduled. Caretakers may choose to disclose at home prior to coming to the disclosure session. If caretakers or children are not ready, further assessment and counseling is provided.
In the disclosure session (step 3), children are scheduled to have their HIV status disclosed, either by counselors or by caretakers in the presence of counselors. Children are counseled about medication adherence, prevention of virus transmission, and confidentiality of diagnosis. Counselors facilitate communication between caretakers and children. In step 4, children and caretakers are assessed for outcomes related to disclosure at 2 - and 6-month follow-up visits.
Instruments
Child behavioural checklist
The Child Behavioural Checklist (CBCL) is a parent-reported instrument designed to identify problem behaviours in children and adolescents. Originally developed by Achenbach, this instrument has been translated into many languages and widely used in clinical studies.11 The present study used the school age form (for ages 4–18 years), which has been translated into Thai and validated in Thai children.12 The Thai version contains 118 problem items of the original CBCL plus additional 24 items. These items inquire about behavioural and emotional symptoms over the past 6 months, with scores ranging from 0 to 2 (0 = none, 1 = occasional, and 2 = frequent). The total scores are categorised into “normal”, “problem”, and “clinical” ranges. For children aged 6–11 years, “problem” ranges are total scores of 49–66 in boys and 48–65 in girls; and “clinical” ranges are above 66 in boys and above 65 in girls. For children aged 12 and older of both genders, scores of 42–57 and above 57 are considered “problem”, and “clinical” ranges, respectively.12 In this study, the CBCL was administered at baseline (in the step 2 of the model) and at 6-month post-disclosure follow-up.
Children’s depression inventory
The Children’s Depression Inventory (CDI), developed by Kovacs, is a widely-used rating scale for assessing depressive symptoms in children and adolescents aged 7–17 years.13 The CDI consists of 27 self-reported items. Each item is scored from 0 to 2 (0 = no, 1 = often, and 2 = always) for severity of depressive symptoms in the preceding two weeks, with total scores ranging from 0 to 52. The Thai version of CDI was developed and validated by Trangkasombat and Likanapichitkul.14 A score of 15 and above was found to be an optimal cut-off in identifying depression, with a sensitivity of 78.9% and specificity of 91.3%, as compared to psychiatric interview.14 In this study, the children completed the CDI at baseline, and at 2-month and 6-month post-disclosure follow-up.
The PedsQL 4.0™ Generic Core Scales
The PedsQL 4.0™ Generic Core Scales is an instrument for assessing health-related quality of life in children and adolescents.15 It consists of 23 items representing four domains: Physical Functioning, Emotional Functioning, Social Functioning, and School Functioning, and is composed of parallel child self-report and parent proxy-report formats. Each item is scored from 0 (never a problem) to 4 (almost always a problem). Items are reverse-scored and linearly transformed to a 0–100 scale (0 = 100, 1 = 75, 2 = 50, 3 = 25, and 4 = 0), so that higher scores indicate better HRQOL. The PedsQL 4.0™ Generic Core Scales has been translated into many languages including Thai. It has been widely used in a variety of chronic diseases including HIV-infected children and adolescents.16 In this study, the child self-report versions for ages 5–7, 8–12, and 13– 18 years were used and data were collected at baseline, and at 2-month and 6-month post-disclosure follow-up.
Evaluation
To assess the disclosure outcome by this model, we analysed data from children who were determined eligible between February 2005 and December 2008 and had follow-up data through June 2009. Medical records and counseling notes were abstracted for demographic and clinical data.
Data analysis
Data were entered into an MS Access database, and descriptive data were analysed using SPSS Statistics 17.0 and Stata 12. Non-parametric tests were used for analysis. Median scores for CDI and PedsQL 4.0™ at baseline and at 2-month and 6-month post-disclosure follow-up were compared by using the Friedman test. We only analysed results with complete data for all three time points. Median scores for CBCL at baseline and at 6-month post-disclosure visit were compared by using the Wilcoxon signed rank test. The differences in proportion of CBCL at baseline and at 6-month post-disclosure follow-up were compared by marginal homogeneity Chi square test and those of CDI at baseline, 2-month, and 6-month post-disclosure follow-up were compared by Cochran test.
Human subjects protections
Data were collected by clinic staff as part of routine services at both hospitals. Human subjects research ethics approval for the project was obtained from the US Centers for Disease Control and Prevention IRB, and the research ethic review committees of the two hospitals.
Results
Of 438 children who were screened (step 1), 398 (91%) were eligible for disclosure. Forty (9%) children were not eligible due to a lack of informed consent, having conditions that precluded effective communication, or having had their HIV status disclosed to them prior to screening. Readiness assessment (step 2) was completed in 353/398 (91%) caretakers of the eligible children. Forty-five caretakers did not undergo readiness assessment because the children were referred to other hospitals (n = 18), died (n = 5), lost to follow-up (n = 1), or had not yet been scheduled for assessment at the time of this analysis (n = 21). Of those who underwent readiness assessment, 216/353 (61%) were determined to be ready for disclosure. Disclosure (step 3) was provided to 186/216 (86%) children. The time spent for the assessment and preparation, measured between the points of eligibility screening and disclosure, ranged from 0 to 49 months, with a mean of 15.2 months. The remaining 30 children were awaiting disclosure appointments at the time of this analysis. Post-disclosure assessment (step 4) was completed for 160/186 (86%) children; these data were included in this analysis (Figure 1).
Of the 160 children for whom all steps were completed, the mean age (±SD) of the children was 11.8 (±1.9) years, and 60% were women. Sixty-seven percent of the children were cared for by someone other than a biological parent, and were living in households with extended family. Demographic and clinical characteristics of the children are shown in Table 1.
Table 1.
Characteristics of children who received HIV diagnosis disclosure and completed pre- and post-disclosure assessments.
| Characteristicsa | |
|---|---|
| Age at disclosure: mean ± SD (years) | 11.8 ± 1.9 |
| Gender: N (%) | |
| Female | 111 (60) |
| Male | 75 (40) |
| Caregivers: N (%) | |
| Father and/or mother | 53 (33) |
| Someone other than a biological parent | 107 (67) |
| Family structure: N (%) | |
| Single | 41(16) |
| Extended | 101 (63) |
| Foster | 16 (10) |
| Immunologic classification: N (%) | |
| CD4 ≥ 25% | 41 (26) |
| CD4 15–24% | 67 (42) |
| CD4 < 15% | 50 (32) |
Not include missing data.
Changes in psychological outcomes
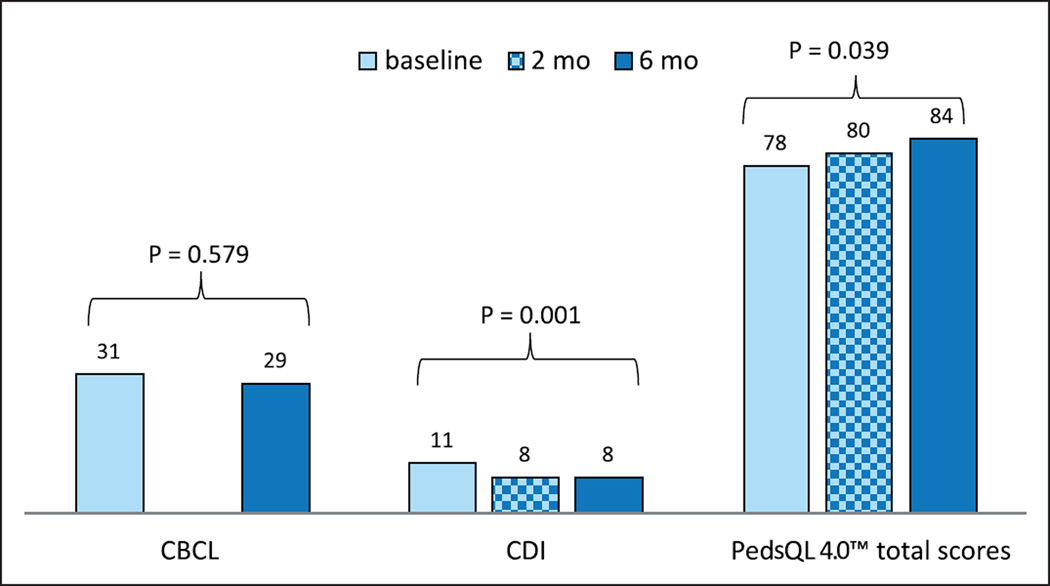
There were no significant changes in the median CBCL scores at baseline and at 6-month post-disclosure follow-up (n = 129, p = 0.58). The median CDI scores were decreased slightly, but significantly, from 11 at baseline to 8 at 2-month and 6-month post-disclosure follow-up (n = 135, p = 0.001). The total PedsQL 4.0™ scores were increased from 78 at baseline to 80 at 2-month, and 84 at 6-month post-disclosure follow-up (n = 126, p = 0.039) (Figure 2).
Figure 2.
Changes in CBCL, CDI, and PedQL 4.0™ median scores before and after disclosure.
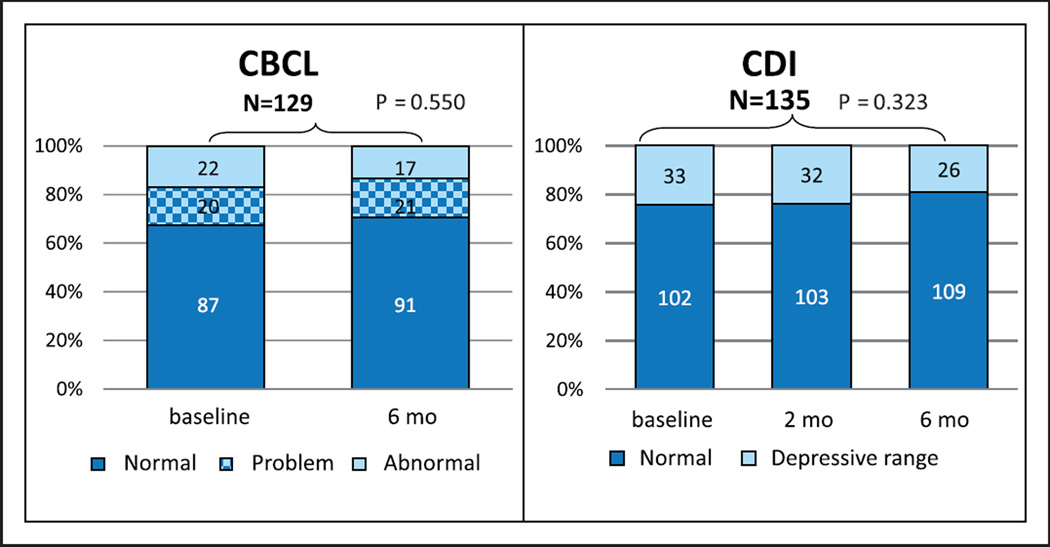
The percentage of the children who scored in the clinical range of CBCL decreased from 22 at baseline to 17 at 6-month post-disclosure follow-up, but this decrease was not significant (p = 0.550). The percentage of children who had CDI scores in the depressive range was also decreased but not significantly changed after disclosure (p = 0.323) (Figure 3).
Figure 3.
Changes in the percentages of children who scored in each category of CBCL and CDI after disclosure.
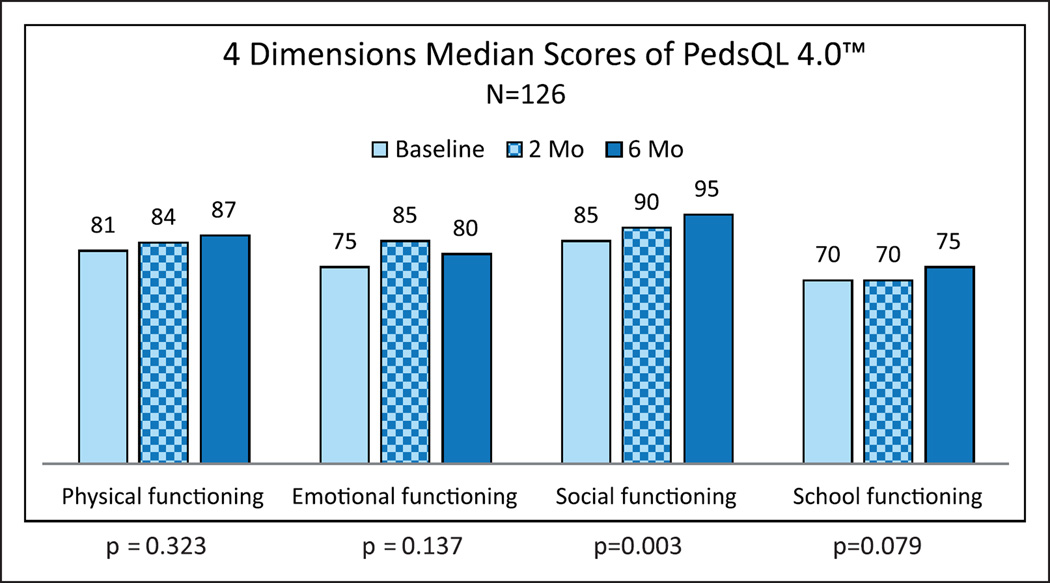
When the scores in each domain of the PedsQL 4.0™ at baseline and at 2-month and 6-month post-disclosure follow-up were compared, it was found that only the Social Functioning domain scores were significantly increased after disclosure (p = 0.003), while other domain scores were not significantly changed (Figure 4).
Figure 4.
Changes in the scores of each domain of PedQL 4.0™ after disclosure.
Discussion
This study assessed psychosocial outcomes in perinatally HIV-infected children whose HIV diagnoses were disclosed to them through a provider-assisted paediatric HIV disclosure model. We found no changes in children’s behavioural problems, a slight but significant decrease in children’s depression level, and an increase in children’s Social Functioning quality of life scores after disclosure.
The findings from this study confirm the results of our previous study indicating that there were no negative outcomes in children’s emotional and behavioural status after disclosure.10 While some of the previous studies reported higher emotional problems associated with disclosure; for instance, New and colleagues reported that children who were told their HIV status had higher internalising problem behaviors as compared to non-disclosed children;7 other studies reported lower6 or not different behavioural problem scores among disclosed as compared to non-disclosed children.17,18 A recent large study by Santamaria et al.19 revealed that HIV-infected youth who had been told their diagnosis did not show an increase of emotional problem. All of these previous studies were retrospective or cross-sectional in nature comparing between the group of disclosed and non-disclosed children. The present study, however, was a prospective cohort which allowed us to systematically compare psychological status before and after disclosure in same subjects. The results of this study, therefore, provide stronger evidence to support the hypothesis that disclosure (with systematic preparation), when carefully done, does not cause a negative psychological impact on the children.
Besides measuring problem behaviours and depressed mood, we also measured health-related quality of life of these children. Health-related quality of life measures have been increasingly used to assess children and caregiver perspectives of health and functioning in many chronic health conditions including HIV infection.16 However, there have been few studies examining the effect of disclosure on quality of life of HIV-infected children. A prospective cohort study by Butler et al.20 quality of life scores were found not to be affected by disclosure. The findings from our study confirm that disclosure of HIV status to child using this model can be accomplished with no negative impact on children’s quality of life, and also demonstrate a significant increase in the total scores and the Social Functioning domain scores of the PedsQL 4.0™ after disclosure. We found, however, that the children in this cohort had lowest scores in the School Functioning domain. This suggests that interventions to improve school functioning are needed for these children.
The present study has some limitations which may affect interpretation of the results. First, positive outcomes found in the study may be due to selection bias related to good relationships between the clinicians and the children and caretakers who received long-term services in the clinics. Second, this study was conducted in only perinatally acquired HIV-infected children, and disclosure was done through a model that emphasises preparing caregivers and supporting the children and caretakers. The results found in this study may not apply to children who acquired HIV by other routes or who may be disclosed without preparation. Third, there were no data in non-disclosed children available for comparison. Fourth, we did not assess the children’s psychological status beyond the period of 6 months after disclosure.
Despite these limitations, the findings from this study add to evidence that HIV status disclosure with systematic preparation can be accomplished without negative impact on children’s psychosocial status, and may positively affect children’s mood and quality of life. Trainings for this disclosure model have been organised for over 600 public healthcare providers from 90 hospitals throughout Thailand, and also for professionals from neighbor countries including Indonesia, Malaysia, Myanmar, and Vietnam.
Conclusions
We found that disclosure of HIV diagnosis to perinatally acquired HIV-infected children with this provider-assisted paediatric disclosure model had no negative psychosocial effect on the children, and may reduce depression and improve quality of life. This disclosure model enables healthcare providers to confidently help children and caretakers with HIV disclosure, which is one of the critical steps in the comprehensive treatment of HIV-infected children.
Acknowledgements
The authors wish to thank the staff of the Infectious Disease Division, Department of Medicine Siriraj Hospital, the QSNICH, and the U.S. CDC Collaboration, Global AIDS Program for their support of this project. We also thank the children and families who participated in this project.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research has been supported by the President’s Emergency Plan for AIDS Relief (PEPFAR) through CDC under the terms of 5U19GH000004-05.
Footnotes
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.American Academy of Pediatrics Committee on Pediatrics AIDS. Disclosure of illness status to children and adolescents with HIV infection. Pediatrics. 1999;103:164–166. doi: 10.1542/peds.103.1.164. [DOI] [PubMed] [Google Scholar]
- 2.Lee CL, Johann-Liang R. Disclosure of the diagnosis of HIV/AIDS to children born of HIV-infected mothers. AIDS Patient Care STDS. 1999;13:41–45. doi: 10.1089/apc.1999.13.41. [DOI] [PubMed] [Google Scholar]
- 3.Battles HB, Wiener LS. From adolescence through young adulthood: psychosocial adjustment associated with long-term survival of HIV. J Adolesc Health. 2002;30:161–168. doi: 10.1016/s1054-139x(01)00341-x. [DOI] [PubMed] [Google Scholar]
- 4.Wiener L, Mellins CA, Marhefka S, et al. Disclosure of an HIV diagnosis to children: history, current research, and future directions. J Dev Behav Pediatr. 2007;28:155–166. doi: 10.1097/01.DBP.0000267570.87564.cd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boon-yasidhi V, Kottapat U, Durier Y, et al. Diagnosis disclosure in HIV-infected Thai children. J Med Assoc Thai. 2005;88(Suppl 8):S100–S105. [PubMed] [Google Scholar]
- 6.Bachanas PJ, Kullgren KA, Schwartz KS, et al. Predictors of psychological adjustment in school-age children infected with HIV. J Pediatr Psychol. 2001;26:343–352. doi: 10.1093/jpepsy/26.6.343. [DOI] [PubMed] [Google Scholar]
- 7.New MJ, Lee SS, Elliott BM. Psychological adjustment in children and families living with HIV. J Pediatr Psychol. 2007;32:123–131. doi: 10.1093/jpepsy/jsj121. [DOI] [PubMed] [Google Scholar]
- 8.Lester P, Chesney M, Cooke M, et al. When the time comes to talk about HIV: factors associated with diagnostic disclosure and emotional distress in HIV-infected children. J Acquir Immune Defic Syndr. 2002;31:309–317. doi: 10.1097/00126334-200211010-00006. [DOI] [PubMed] [Google Scholar]
- 9.Wiener LS, Battles HB. Untangling the web: a close look at diagnosis disclosure among HIV-infected adolescents. J Adolesc Health. 2006;38:307–309. doi: 10.1016/j.jadohealth.2005.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boon-yasidhi V, Chokephaibulkit K, McConnell MS, et al. Development of a diagnosis disclosure model for perinatally HIV-infected children in Thailand. AIDS Care. 2013;25:756–762. doi: 10.1080/09540121.2012.749331. [DOI] [PubMed] [Google Scholar]
- 11.Achenbach TM, Ruffle TM. The Child Behavior Checklist and related forms for assessing behavioral/emotional problems and competencies. Pediatr Rev. 2000;21:265–271. doi: 10.1542/pir.21-8-265. [DOI] [PubMed] [Google Scholar]
- 12.Weisz JR, Suwanlert S, Chaiyasit W, et al. Epidemiology of behavioral and emotional problems among Thai and American children: parent reports for ages 6 to 11. J Am Acad Child Adolesc Psychiatry. 1987;26:890–897. doi: 10.1097/00004583-198726060-00014. [DOI] [PubMed] [Google Scholar]
- 13.Kovacs M. The Children’s Depression, Inventory (CDI) Psychopharmacol Bull. 1985;21:995–998. [PubMed] [Google Scholar]
- 14.Trangkasombat U, Likanapichitkul D. The Children’s Depression Inventory as a screen for depression in Thai children. J Med Assoc Thai. 1997;80:491–499. [PubMed] [Google Scholar]
- 15.Varni JW, Seid M, Rode CA. The PedsQL: measurement model for the pediatric quality of life inventory. Med Care. 1999;37:126–139. doi: 10.1097/00005650-199902000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Punpanich W, Boon-yasidhi V, Chokephaibulkit K, et al. Health-related quality of life of Thai children with HIV infection: a comparison of the Thai Quality of Life in Children (ThQLC) with the Pediatric Quality of Life Inventory version 4.0 (PedsQL 4.0) Generic Core Scales. Qual Life Res. 2010;19:1509–1516. doi: 10.1007/s11136-010-9708-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Riekert KA, Wiener LS, Battles HB. Prediction of psychological distress in school-age children with HIV. Children’s Health Care. 1999;28:201–220. [Google Scholar]
- 18.Mellins CA, Brackis-Cott E, Dolezal C, et al. Patterns of HIV status disclosure to perinatally HIV-infected children and subsequent mental health outcomes. Clin Child Psychol Psychiatry. 2002;7:101–114. [Google Scholar]
- 19.Santamaria EK, Dolezal C, Marhefka SL, et al. Psychosocial implications of HIV serostatus disclosure to youth with perinatally acquired HIV. AIDS Patient Care STDS. 2011;25:257–264. doi: 10.1089/apc.2010.0161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Butler AM, Williams PL, Howland LC, et al. Impact of disclosure of HIV infection on health-related quality of life among children and adolescents with HIV infection. Pediatrics. 2009;123:935–943. doi: 10.1542/peds.2008-1290. [DOI] [PMC free article] [PubMed] [Google Scholar]