Abstract
Background
Uniportal video-assisted thoracic surgery (VATS) is becoming popular, and uniportal lobectomy in semiprone position was reported in 2014. This study aimed to investigate the feasibility and safety of uniportal VATS in semiprone position.
Methods
From May 28, 2014 to October 19, 2015, we attempted uniportal VATS lobectomy in semiprone position in 105 cases. Forty-five patients were male, and 60 patients were female. Average age was 57.1±10.6 years (24–76 years). Perioperative parameters were documented.
Results
There were two conversions to three-port lobectomy, one conversion to double-port lobectomy, and three conversions to thoracotomy. Among the patients who received uniportal VATS in semiprone position, mean operation duration was 137.4±47.8 minutes. Mean estimated blood loss was 60.7±102.7 mL. Mean time of drainage was 3.0±2.1 days, and postoperative length of stay averaged 4.9±2.3 days. In the cases of primary lung cancer, the mean number of nodal stations explored was 7.2±1.3, with a mean of 20.8±6.3 lymph nodes resected. As to the mediastinal lymph node specifically, a mean of 4.4±1.0 nodal stations were explored, and the number of resected mediastinal lymph nodes averaged 12.8±5.1. No perioperative death or major complication occurred.
Conclusions
Uniportal VATS lobectomy in semiprone position is feasible and safe.
Keywords: Video-assisted thoracic surgery (VATS), uniportal, semiprone position
Introduction
Video-assisted thoracic surgery (VATS) has developed rapidly in the past two decades, and has become the first choice for treating early-stage non-small cell lung cancer. Since Gonzalez Rivas first described uniportal VATS for lobectomy in 2011 (1), the feasibility and safety of uniportal VATS have been demonstrated. Uniportal VATS has been adopted for segmentectomy (2), sleeve lobectomy (3), and the treatment of advanced lung cancer (4). The advantages of uniportal VATS are decreased pain of patients, shortened recovery time and cosmesis (5). Nevertheless, the disadvantages could not be ignored. Though surgical instruments have been adapted, interference of instruments could not been avoided completed. Operators and assistants are more liable to get tired in uniportal VATS than in three-portal VATS or four-portal VATS.
Most surgeons perform uniportal lobectomy in lateral decubitus position. No surgeon has reported semiprone position for uniportal lobectomy before 2014, while semiprone position has been adopted for minimally invasive esophagectomy over the last few years (6). We reported the first case of uniportal lobectomy for lung cancer in semiprone position in 2014 (7), and reported the first case of uniportal lobectomy for pulmonary sequestration in semiprone position in 2015 (8). The advantages are good exposure of posterior mediastinum, relieving fatigue of operators and assistants, and reducing traction of lung. We have used semiprone position for uniportal VATS since last year. The objective of this study is to investigate the feasibility and safety of uniportal VATS in semiprone position.
Patients and methods
Patients
From May 28, 2014 to October 19, 2015, we attempted uniportal VATS lobectomy in semiprone position in 105 cases. Forty-five patients were male, and 60 patients were female. Average age was 57.1±10.6 years (24–76 years). All patients received preoperative examinations including electrocardiogram, chest computed tomography, pulmonary function, bronchoscope, brain magnetic resonance imaging, and bone scan if necessary. The indication criteria and exclusion criteria were described in the previous report of our center (9).
Surgical technique
Patient was intubated with a dual lumen endotracheal tube, and the operated lung was deflated. Patient was positioned in semiprone position. Upper arm was raised on arm rest, and body was immobilized. Both the surgeon and the assistant stood on the ventral side of patient. The assistant stood at the footstool to lower his upper arm. The layout was illustrated in Figure 1. A single 3–5 cm incision was made in the 5th intercostal space on the midaxillary line. We protected the incision with a plastic wound retractor. The assistant held a 30-degree 10 mm camera at the posterior part of the incision with one hand, and held a piece of gauze with articulated oval forceps or endoscopic grasping forceps to push lung for exposure. The operator held curved suction with the left hand, and harmonic scalpel (Ethicon Endo-Surgery Inc., Cincinnati, OH, USA) with the right hand. The curved suction and articulated forceps were specially designed for our center. Arteries and veins were dissociated and transected with endoscopic linear staplers (Ethicon Endo-Surgery Inc., Cincinnati, OH, USA). Slender arteries or veins were ligated with vascular clips (Weck Surgical, Teleflex, Limerick, USA) and then transected.
Figure 1.
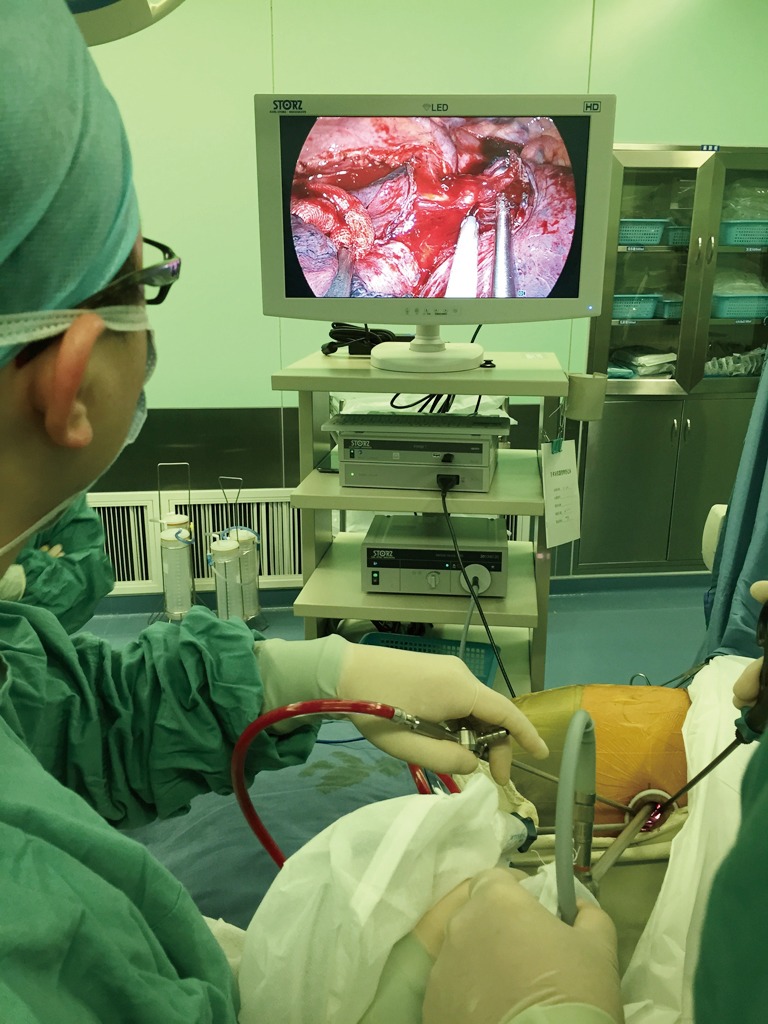
The operation room layout of uniportal video-assisted thoracic surgery lobectomy in semiprone position.
For tumors in right upper lobe, dissection might be performed from posterior mediastinum to anterior mediastinum (posterior approach) or from anterior mediastinum to posterior mediastinum (anterior approach). Posterior approach is preferred in the latter period and was described below (Figure 2). If the fissure was complete and arteries could be exposed easily, the fissure was dissected firstly. The upper lobe was pushed forward, and bronchus and arteries were transected. Vein was the last structure to be transected. If the fissure was poorly developed and it was difficult to expose interlobar pulmonary arteries, the dissection order was bronchus, artery, vein and fissure.
Figure 2.
Uniportal video-assisted thoracic surgery right upper lobectomy in semiprone position (10). Available online: http://www.asvide.com/articles/744
For tumors in left upper lobe, dissection might also be performed in posterior approach or in anterior approach. In posterior approach, artery was the first structure to be transected (Figure 3). No matter whether the fissure was well developed or not, the branches of left upper lobe arteries could always be dissociated and transected posteriorly firstly.
Figure 3.
Uniportal video-assisted thoracic surgery left upper lobectomy in semiprone position (11). Available online: http://www.asvide.com/articles/745
For tumors in lower lobes, if the fissure was complete, pulmonary artery branches were the first to be transected, and the vein and bronchus was followed (Figure 4). If the fissure was incomplete, the fissure was the last to be dissected (Figure 5).
Figure 4.
Uniportal video-assisted thoracic surgery right lower lobectomy in semiprone position (12). Available online: http://www.asvide.com/articles/746
Figure 5.
Uniportal video-assisted thoracic surgery left lower lobectomy in semiprone position (13). Available online: http://www.asvide.com/articles/747
The specimen was taken out in the specimen bag.
If malignancy was confirmed before or during operation, non-grasping mediastinal lymph node dissection was performed (14). For right paratracheal lymph node dissection, we opened the pleura inferior to the azygos vein with harmonic scalpel, lifting the azygos vein with curved suction device. We opened the pleura superior to the azygos vein then, and pushed the lower paratracheal lymph nodes with the suction device to cross over this vein. Lower and upper paratracheal lymph nodes were resected en-bloc. For subcarinal lymph node dissection, we opened the pleura anterior to vagus nerve, and separated esophagus from subcarinal lymph node. The esophagus was lifted by suction device, and subcarinal lymph node was resected en-bloc with harmonic scalpel. As the anatomic structures in the thoracic cavity were asymmetrical, lymph nodes dissections for right and left sides were different (Figure 6: lymph node dissection for right side with uniportal VATS; Figure 7: lymph node dissection for left side with uniportal VATS).
Figure 6.

Uniportal video-assisted thoracic surgery right mediastinal lymph node dissection in semiprone position (15). Available online: http://www.asvide.com/articles/748
Figure 7.

Uniportal video-assisted thoracic surgery left mediastinal lymph node dissection in semiprone position (16). Available online: http://www.asvide.com/articles/749
At the end of the operation, a 28-Fr chest tube was inserted in the posterior part of the incision.
Statistical analysis
The quantitative variables were expressed as mean ± standard deviation and rang. Qualitative variables were expressed as frequencies and percentages. Statistical analysis was conducted using Statistical Package for Social Sciences (SPSS) 20.0 software (SPSS Inc., Chicago, IL, USA).
Results
Out of 105 cases attempted, 99 patients received uniportal VATS in semiprone position without conversion to multiple incisions or thoracotomy. There were two conversions to three-port lobectomy, one conversion to double-port lobectomy, and three conversion to thoracotomy. The reasons of conversions were listed in order in Table 1. The first four conversions were mainly due to lack of experience, while the last two conversions were caused by calcified lymph nodes. Among the patients who received uniportal VATS in semiprone position, mean operation duration was 137.4±47.8 minutes. Operation duration was greater than or equal to 240 minutes in seven cases, as a result of severe pleural adhesion. Mean estimated blood loss was 60.7±102.7 mL. Mean time of drainage was 3.0±2.1 days, and postoperative length of stay averaged 4.9±2.3 days. Pathological findings of all the patients were listed in Table 2. In the cases of primary lung cancer, the mean number of nodal stations explored was 7.2±1.3, with a mean of 20.8±6.3 lymph nodes resected. As to the mediastinal lymph node specifically, a mean of 4.4±1.0 nodal stations were explored, and the number of resected mediastinal lymph nodes averaged 12.8±5.1. Of the 97 malignant tumors, there were five cases of N1 metastasis and five cases of N2 metastasis.
Table 1. Reasons of conversions.
| Diagnosis | Reasons | Converted to |
|---|---|---|
| Right upper lung cancer | Bleeding caused by traction of lung | Thoracotomy |
| Right upper lung cancer | Lymph nodes attached to arteries tightly | Three-portal VATS |
| Left upper lung cancer | Lymph nodes attached to arteries tightly | Three-portal VATS |
| Intralobar sequestration | Poor exposure caused by adhesion | Two-portal VATS |
| Bronchiectasis | Severe adhesion and calcified lymph nodes attached to arteries | Thoracotomy |
| Left lower lung cancer | Calcified lymph nodes attached to arteries | Thoracotomy |
VATS, video-assisted thoracic surgery.
Table 2. Pathology of all cases.
| Pathology | N=105 |
|---|---|
| Invasive adenocarcinoma | 82 |
| Minimally invasive adenocarcinoma | 3 |
| Squamous cell carcinoma | 5 |
| Adenosquamous cell carcinoma | 3 |
| Mucinous adenocarcinoma | 2 |
| Large cell carcinoma | 1 |
| Atelectasis of middle lobe | 1 |
| Sequestration | 2 |
| Atypical carcinoid | 1 |
| Organized pneumonia | 2 |
| Bronchiectasis | 1 |
| Sclerosing hemangioma | 1 |
| Hamartoma | 1 |
No perioperative death or major complication occurred. Hemorrhage was observed on day 2 after operation in two cases. After the administration of low molecular heparin was suspended, the bleeding mitigated without any other intervention. Chyle leakage occurred in one patient, and was cured with fat-free diet. The patient was discharged 5 days after operation. Four patients developed prolonged air leakage and one patient developed pneumonia. Incision infection occurred in one case.
Discussion
VATS lobectomy was first reported in 1992 (17). Most of VATS lobectomies have been undergone with three or four ports since then. Gonzalaz Rivas and his colleagues reported uniportal VATS lobectomy in 2011 (1), and proved the safety and feasibility of this technique. Uniportal VATS segmentectomy (18), sleeve lobectomy (3), and pneumonectomy (19) were then performed successfully in the next few years.
One of the advantages of uniportal VATS is that the approach to lesion is similar to the approach that surgeons would use in open surgery (20). Besides, the advantage of uniportal VATS lobectomy on postoperative pain has been demonstrated by surgeons, but there is still room for improvement. As a result of the small incision, interference of instruments, as well as the limitation for placing endo linear staplers, cannot be avoided. Moreover, fatigue of operator and assistant cannot be ignored. The first 10 attempts of uniportal VATS lobectomy were performed in lateral decubitus position, which were not included in the series. Operator and assistant were forced to raise upper armed in most of the operation time, which contributed to fatigue of surgeons. Concerning the disadvantages, we attempted uniportal VATS lobectomy in semiprone position after the 10 cases.
There are several common positions for thoracic surgery, such as lateral decubitus position, prone position, supine position, and semiprone position. Lateral decubitus position is most commonly used in VATS for the good exposure of most parts of thoracic cavity and easy conversion to thoracotomy. Whereas, the exposure of posterior mediastinum is not good in lateral decubitus position and the dissection of subcarinal lymph nodes is limited (21). Prone position provides excellent exposure for posterior mediastinum because the lung falls away under gravity (22), but this position is unpopular for several disadvantages. In prone position, the ports must be inserted through thick muscles in the posterior axillary line, and chest tube is placed in the posterior axillary line as a result. Moreover, conversion to thoracotomy is difficult in prone position. Semiprone position has the advantages of both lateral decubitus position and prone position. It provides the exposure of posterior mediastinum similar with prone position, and can be easily converted to lateral decubitus position for thoracotomy if necessary. Semiprone position is widely adopted in minimally invasive esophagectomy for the mobilization of esophagus and dissection of lymph nodes (6). The semiprone position has rarely been reported in VATS lobectomy, and has only been described in mediastinal lymph node dissection for lung cancer before 2014 (21).
The exposure for posterior mediastinum is rather excellent in semiprone position, while the exposure for anterior mediastinum is not so good. The posterior approach could take advantage of the better exposure and avoid disadvantage. The posterior approach could be performed no matter whether the fissure was complete or not. The task for the assistant was not complex which was pushing the lung with gauze, and the upper lobe was in the surgeon’s control totally. The posterior approach minimized the requirement for assistant, and the operation was not interrupted. If the fissure was developed well, the fissure was dissected firstly so that the assistant could manipulate lower lobe better.
The operation duration averaged 137.4±47.8 minutes, which was not significantly longer than that of previous three-port VATS lobectomy. During mediastinal lymph node dissection, the lymph nodes were suctioned or pushed with suction device, preventing from being crushed by forceps. The mean number of dissected mediastinal lymph nodes was 12.8±5.1, and the mean number of dissected mediastinal lymph node groups was 4.4±1.0, which met the requirement for lymph node dissection. The number of dissected lymph nodes was similar with the data reported by other surgeons who operated with three-port VATS (23) or uniportal VATS (24,25).
In the first 10 cases of uniportal VATS lobectomy which were performed in lateral decubitus position, two cases occurred postoperative hemoptysis. We reviewed the operations and speculated that traction of lung for exposure might have caused the hemoptysis. In the circumstance of single incision, the tension of traction was difficult to be controlled, which would cause the injury of lung parenchyma. In the subsequent cases, we pushed lung with a piece of gauze held by endoscopic grasping forceps for exposure, and no hemoptysis occurred afterwards. The lungs could be pushed ventrally or dorsally with no difficulty.
Fatigue was a big problem for surgeon in uniportal VATS, while the semiprone position might resolve this. In semiprone position, the thoracoscope, as well as operating instruments, was horizontal most of the operation time. Hence, the surgeon and the assistant did not have to lift their upper arms, which provided better ergonomic gesture. In a case of lung cancer with severe pleural adhesion, we spent more than 5 hours to complete the uniportal VATS lobectomy in semiprone position with no obvious fatigue.
One conversion to thoracotomy was the first case of right upper lobe resection in this series. There was a tiny branch of artery adjacent to the ascending artery of upper lobe. Traction caused bleeding of the tiny branch and we determined to extend the incision to 8 cm for the lack of experience. Whereas, the bleeding stopped spontaneously then. In the 19th case, we encountered similar situation, and stopped the bleeding without conversion. In two cases, the lymph nodes attached to arteries tightly, and we converted to three-portal VATS for the lack of experience, and concerning safety as well. The patients were changed to lateral decubitus position by tilting the operation table, and the surgeon stood on the dorsal side of the patients. In a case of pulmonary sequestration, the pleural adhesion hampered the exposure of abnormal artery, so we converted to two-portal VATS in semi-prone position. The operation was completed successfully even though the surgeon had not performed two-portal VATS ever before. After the first 15 cases, there were only two conversions of the 90 cases. One was bronchiectasis, and the other was lung cancer. In both cases, the lymph nodes were calcified and attached to vessels too tightly to be separated. Even with three ports, the operation could hardly be completed. Therefore, we converted to thoracotomy directly.
Conclusions
Uniportal VATS lobectomy in semiprone position is feasible and safe. Semiprone position can be easily converted to lateral decubitus position. Semiprone position provides better ergonomic gesture for surgeon and assistant.
Acknowledgements
Funding: This work was supported by the National Natural Science Foundation of China (Grant No. 81572295).
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. [DOI] [PubMed] [Google Scholar]
- 2.Kamiyoshihara M, Igai H, Ibe T, et al. A 3.5-cm Single-Incision VATS Anatomical Segmentectomy for Lung Cancer. Ann Thorac Cardiovasc Surg 2015;21:178-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gonzalez-Rivas D, Delgado M, Fieira E, et al. Left lower sleeve lobectomy by uniportal video-assisted thoracoscopic approach. Interact Cardiovasc Thorac Surg 2014;18:237-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gonzalez-Rivas D, Fieira E, Delgado M, et al. Is uniportal thoracoscopic surgery a feasible approach for advanced stages of non-small cell lung cancer? J Thorac Dis 2014;6:641-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [DOI] [PubMed] [Google Scholar]
- 6.Lin J, Kang M, Chen C, et al. Thoracoscopic oesophageal mobilization during thoracolaparoscopy three-stage oesophagectomy: a comparison of lateral decubitus versus semiprone positions. Interact Cardiovasc Thorac Surg 2013;17:829-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin Z, Xu S, Wang Q. Uniportal video-assisted thoracoscopic surgery right upper lobectomy with systematic lymphadenectomy in a semiprone position. J Thorac Dis 2014;6:1840-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin ZW, Xu ST, Wang Q. Uniportal video-assisted thoracic lobectomy in a semiprone position for the treatment of a large intralobar pulmonary sequestration. Interact Cardiovasc Thorac Surg 2015;21:542-4. [DOI] [PubMed] [Google Scholar]
- 9.Feng M, Shen Y, Wang H, et al. Uniportal video assisted thoracoscopic lobectomy: primary experience from an Eastern center. J Thorac Dis 2014;6:1751-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lin Z, Xi J, Xu S, et al. Uniportal video-assisted thoracic surgery right upper lobectomy in semiprone position. Asvide 2015;2:166. Available online: http://www.asvide.com/articles/744
- 11.Lin Z, Xi J, Xu S, et al. Uniportal video-assisted thoracic surgery left upper lobectomy in semiprone position. Asvide 2015;2:167. Available online: http://www.asvide.com/articles/745
- 12.Lin Z, Xi J, Xu S, et al. Uniportal video-assisted thoracic surgery right lower lobectomy in semiprone position. Asvide 2015;2:168. Available online: http://www.asvide.com/articles/746
- 13.Lin Z, Xi J, Xu S, et al. Uniportal video-assisted thoracic surgery left lower lobectomy in semiprone position. Asvide 2015;2:169. Available online: http://www.asvide.com/articles/747
- 14.Liu C, Pu Q, Guo C, et al. Non-grasping en bloc mediastinal lymph node dissection for video-assisted thoracoscopic lung cancer surgery. BMC Surg 2015;15:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lin Z, Xi J, Xu S, et al. Uniportal video-assisted thoracic surgery right mediastinal lymph node dissection in semiprone position. Asvide 2015;2:170. Available online: http://www.asvide.com/articles/748
- 16.Lin Z, Xi J, Xu S, et al. Uniportal video-assisted thoracic surgery left mediastinal lymph node dissection in semiprone position. Asvide 2015;2:171. Available online: http://www.asvide.com/articles/749
- 17.Lewis RJ, Caccavale RJ, Sisler GE, et al. Video-assisted thoracic surgical resection of malignant lung tumors. J Thorac Cardiovasc Surg 1992;104:1679-85; discussion 1685-7. [PubMed]
- 18.Gonzalez-Rivas D, Fieira E, Mendez L, et al. Single-port video-assisted thoracoscopic anatomic segmentectomy and right upper lobectomy. Eur J Cardiothorac Surg 2012;42:e169-71. [DOI] [PubMed] [Google Scholar]
- 19.Gonzalez-Rivas D, de la Torre M, Fernandez R, et al. Video: Single-incision video-assisted thoracoscopic right pneumonectomy. Surg Endosc 2012;26:2078-9. [DOI] [PubMed] [Google Scholar]
- 20.Bertolaccini L, Rocco G, Viti A, et al. Geometrical characteristics of uniportal VATS. J Thorac Dis 2013;5 Suppl 3:S214-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Agasthian T. Revisiting the prone position in video-assisted thoracoscopic surgery. Asian Cardiovasc Thorac Ann 2010;18:364-7. [DOI] [PubMed] [Google Scholar]
- 22.Palanivelu C, Prakash A, Senthilkumar R, et al. Minimally invasive esophagectomy: thoracoscopic mobilization of the esophagus and mediastinal lymphadenectomy in prone position--experience of 130 patients. J Am Coll Surg 2006;203:7-16. [DOI] [PubMed] [Google Scholar]
- 23.D'Amico TA, Niland J, Mamet R, et al. Efficacy of mediastinal lymph node dissection during lobectomy for lung cancer by thoracoscopy and thoracotomy. Ann Thorac Surg 2011;92:226-31; discussion 231-2. [DOI] [PubMed] [Google Scholar]
- 24.Gonzalez D, de la Torre M, Paradela M, et al. Video-assisted thoracic surgery lobectomy: 3-year initial experience with 200 cases. Eur J Cardiothorac Surg 2011;40:e21-8. [DOI] [PubMed] [Google Scholar]
- 25.Wang BY, Tu CC, Liu CY, et al. Single-incision thoracoscopic lobectomy and segmentectomy with radical lymph node dissection. Ann Thorac Surg 2013;96:977-82. [DOI] [PubMed] [Google Scholar]


