Abstract
The number of outpatient orthopedic surgeries performed within North America continues to increase. The impact of this change in services on patient outcomes is largely unknown. The objective of this review is to compare patient outcomes and associated costs for outpatient orthopedic surgeries traditionally performed in hospital to inpatient surgeries, as well as to summarize the eligibility and preoperative education requirements for outpatient orthopedic surgery in North America. We performed a systematic review of Medline, Pubmed and Embase databases for articles comparing the clinical and economic impact of outpatient orthopedic surgical procedures versus inpatient procedures in North America. We reported on requirements for inpatient versus outpatient care, preoperative education requirements, complications and patient outcomes, patient satisfaction, and when available total mean costs. Nine studies met the inclusion criteria for this review. Eligibility requirements for outpatient orthopedic surgery within the included studies varied, but generally included: patient consent, a caregiver at home following surgery, close proximity to an outpatient center, and no history of serious medical problems. Preoperative education programs were not always compulsory and practices varied between outpatient centers. All of the reviewed studies reported that outpatient surgeries had similar or improved level of pain and rates of nausea. Outpatients reported increased satisfaction with the care they received. As expected, outpatient procedures were less expensive than inpatient procedures. This review found that outpatient procedures in North America appear to be less expensive and safe alternatives to inpatient care for patients who are at lower risk for complications and procedures that do not necessarily require close hospital level care monitoring following same day surgery.
Key words: Orthopedic surgery, cost implication, inpatient, outpatient;
Introduction
The number of outpatient surgical procedures has continued to increase in the United States since the early 1980s, yet little research has been conducted to evaluate the impact of this surgical option on patient health. Outpatient (also known as ambulatory) surgeries are performed in an outpatient setting that does not require an overnight stay in a medical facility or hospital.1 The rise in outpatient surgical procedures is thought to be driven by the response of the Medicare program to escalating health care costs by expanding coverage to include ambulatory surgery centers.2 According to the 2006 National Survey of Ambulatory Surgery, an estimated 53.3 million outpatient procedures were performed that year in the United States.2 In 2011, over 60% of all surgeries performed in the United States were performed on an outpatient basis.3
Some patients are more likely to elect for outpatient surgery than others: females and adults aged 45 to 64 years are demographically the biggest users of outpatient care services.2 Common diagnoses addressed at outpatient surgery centers include diseases of the esophagus, diverticula of the intestine, cataracts, benign and malignant neoplasms, and the corresponding outpatient procedures include endoscopy of the small intestine, endoscopy of the colon, lens extraction, insertion of prosthetic lens, and injection of agent into spinal canal.2 However, higher risk orthopedic procedures historically performed exclusively as inpatient procedures are now being performed on an outpatient basis.1 These include routine arthroscopic procedures including anterior cruciate ligament reconstruction and more recently total joint arthroplasty surgery at the hip, knee and shoulder.4
There are several advantages with respect to outpatient procedures over in-hospital procedures, including: fewer scheduling delays, more autonomy for physicians, and cost savings.5 However, outpatient surgery is not a universal best choice solution because it is more complicated to monitor the recovery process following surgery since patients do not stay overnight in a supervised hospital setting. We performed a systematic review of the published literature to compare patient outcomes and costs for outpatient orthopedic surgeries in North America traditionally performed in hospital to inpatient surgeries, and to summarize the eligibility and rehabilitative requirements for these surgeries.
Materials and Methods
Literature search
We performed a systematic review of the Medline, Pubmed and Embase databases for all English articles published in North America addressing the clinical and economic impact of outpatient orthopedic surgical procedures relative to inpatient procedures. The search was performed on January 7, 2015 and the search strategy is shown in Table 1.
Table 1.
Search strategy.
| Medline and Embase | PubMed |
|---|---|
| 1. Inpatient.ab,ti. | 1. Inpatient[Title/Abstract] |
| 2. Outpatient.ab,ti. | 2. Outpatient[Title/Abstract] |
| 3. Ambulatory.ab,ti. | 3. Ambulatory[Title/Abstract] |
| 4. 2 OR 3 | 4. 2 OR 3 |
| 5. 1 AND 4 | 5. 1 AND 4 |
| 6. Orthop$.ab,ti. | 6. Orthopedic[Title/Abstract] |
| 7. Arthroplast$.ab,ti. | 7. Orthopaedic[Title/Abstract] |
| 8. Reconstruction.ab,ti. | 8. Arthroplasty[Title/Abstract] |
| 9. Repair.ab,ti. | 9. Reconstruction[Title/Abstract] |
| 10. Fracture.ab,ti. | 10. Repair[Title/Abstract] |
| 11. 6 OR 7 | 11. Fracture[Title/Abstract] |
| 12. 8 OR 9 OR 10 | 12. 6 OR 7 OR 8 |
| 13. 11 OR 12 | 13. 9 OR 10 OR 11 |
| 14. 5 AND 13 | 14. 12 OR 13 |
| 15. 5 AND 14 |
Eligibility criteria
Randomized controlled trials, prospective comparative studies, retrospective comparative studies, and case-control studies comparing outpatient and inpatient orthopedic surgical procedural outcomes and costs available in English were eligible for inclusion. We excluded case series, case studies, and expert opinion pieces since these do not include between group comparisons. In cases of multiple publications from the same data set, only the most recent study was included.
Data abstraction
The following data was abstracted from the included studies: author, country of publication, year, investigated procedure, sample size, eligibility requirements for outpatient surgery, operative rehabilitative practices, complications and patient outcomes, patient satisfaction and cost.
Data reporting
We listed eligibility requirements for outpatient surgery, operative rehabilitation requirements, complications and patient outcomes and patient satisfaction. Cost data were reported for each study as mean total costs when available. If mean total costs were not available, we listed the outcome that was reported by the study.
Data analysis
We reported means and standard deviations when possible. When means could not be reported we reported data descriptively. Data were not pooled across studies.
Results
We identified 3412 potentially relevant studies from our Medline, Pubmed and Embase search. Of the 3412 potentially eligible papers, 365 were excluded because they were duplicates, 383 were non-English, 2606 did not include both outpatient and inpatient groups, 46 did not address orthopedic surgical procedures, and six did not include comparative analyses. There were no cases of multiple publications from the same dataset. We found an additional three studies by checking study references and related articles. Therefore, nine studies met the eligibility criteria for our systematic review. A detailed summary of the screening process is provided in Figure 1.
Figure 1.
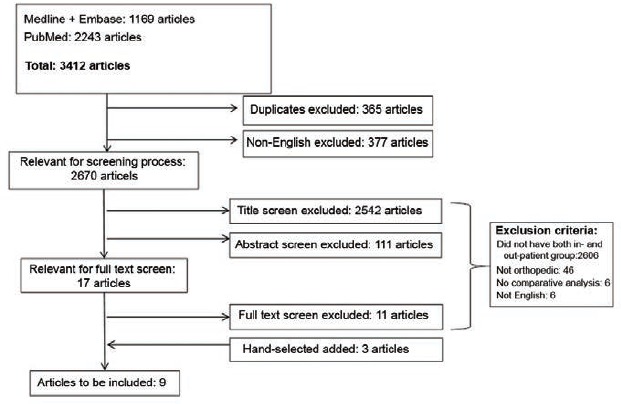
Flow chart of articles identified, included and excluded.
Study characteristics
Of the nine included studies, eight were conducted in the United States and one was conducted in Canada (Table 2).5-13 There were six prospective comparative studies, two retrospective cost analysis studies, and one case control study included. The mean sample size across the eight studies was 11,482±34,200 patients, with a range of 20 patients to 102,684 patients. Investigated surgical procedures included reconstruction of the anterior cruciate ligament (four studies), total hip arthroplasty (two studies), total knee arthroplasty (two studies) and volar plating for closed distal radius fractures (1 study). Three studies provided details on the eligibility criteria for outpatient versus inpatient orthopedic surgery, five studies described the rehabilitation protocols, five studies reported on complications and patient outcomes, one study evaluated patient satisfaction and seven studies provided cost data.
Table 2.
Study characteristics.
| Authors (Country, year) | Study design | Sample size | Investigated procedure | Listed eligibility criteria for outpatient surgery (Y/N) | Reported on operative rehabilitation (Y/N) | Reported on complications and patient outcomes (Y/N) | Reported on patient satisfaction (Y/N) | Included cost comparison (Y/N) |
|---|---|---|---|---|---|---|---|---|
| Kao (USA, 1995)5 | Prospective comparative | 25 outpatient, 12 inpatient | Reconstruction of the anterior cruciate ligament | N | Y | Y | N | Y |
| Novak (USA, 1996)10 | Prospective comparative | 45 outpatient, 29 inpatient | Reconstruction of the anterior cruciate ligament | N | N | Y | N | Y |
| Aronowitz (USA, 1998)9 | Prospective comparative | 34 outpatient, 1 inpatient | Reconstruction of the anterior cruciate ligament | N | Y | N | N | Y |
| Bertin (USA, 2005)6 | Prospective comparative | 10 inpatient, 10 outpatient | Total hip arthroplasty | Y | Y | N | N | Y |
| Krywulak (Canada, 2005)7 | Prospective comparative | 21 inpatient, 19 outpatient | Reconstruction of the anterior cruciate ligament | Y | Y | Y | Y | N |
| Kolisek (USA, 2009)8 | Prospective comparative | 64 inpatient, 64 outpatient | Total knee arthroplasty | Y | Y | Y | N | N |
| Mather (USA, 2011)12 | Retrospective cost-identification | 93 ASC, 37 inpatient | Volar plating for closed distal radius fractures | N | N | N | N | Y |
| Lovald (USA, 2014)11 | Retrospective cost-analysis 5+day | 71,341 3-4 day inpatient, 23,134 inpatient, 7755 1-2 day inpatient, 454 outpatient | Total knee arthroplasty | N | N | Y | N | Y |
| Aynardi (USA, 2014)13 | Case-control | 119 outpatient, 78 inpatient | Total hip arthroplasty | N | N | N | N | Y |
ASC, ambulatory surgery center.
Eligibility requirements for outpatient surgery
There were three studies that included their eligibility requirements for outpatient procedures including total hip arthroplasty, reconstruction of the anterior cruciate ligament, and total knee arthroplasty (Table 3).6-8 In order for patients to undergo outpatient surgery they had to provide consent; have stable cardiovascular, respiratory, and renal systems; have a caregiver at home following surgery; and live within close proximity of outpatient center.6-8 Studies differed in requirements with respect to age and time from injury.6-8 Bertin and colleagues (2005) did not include age or time from injury requirements in order for a patient to be eligible for outpatient surgery.6 Kolisek and colleagues (2009) also did not set an age criterion; however, they required that surgery be within 90 days of the injury.8 Krywulak and colleagues (2005) required that patients be between 15 and 50 years of age and surgery at least six hours after injury.7
Table 3.
Eligibility requirements for outpatient surgery.
| Author (Country, year) | Sample size | Investigated procedure | Inclusion criteria | Exclusion criteria |
|---|---|---|---|---|
| Bertin (USA, 2005)6 | 10 inpatient, 10 outpatient | Total hip arthroplasty | Consent; Stable cardiovascular, respiratory, and renal systems; Preoperatively master physical therapy instructions such as dislocation precautions; Caregiver in home following surgery | Patients with diabetes/history of prostatic hypertrophy initially excluded then considered on an individual basis |
| Krywulak (Canada, 2005)7 | 21 inpatient, 19 outpatient | Reconstruction of the anterior cruciate ligament | 15-50 years of age; >6 hours from injury; Live <1 hour from hospital; A caregiver for the first 48 hours after surgery; Perceived psychological ability to cope at home after surgery | Previous anterior cruciate ligament reconstruction; Serious health condition requiring in-hospital supervision after the operation; Hypersensitivity to ASA/NSAIDs; Known bleeding disorder or active peptic ulcer disease |
| Kolisek (USA, 2009)8 | 64 inpatient, 64 outpatient | Total knee arthroplasty | Lived within 1 hour from the office; An adult caregiver at home following surgery | History of diabetes, myocardial infarction, stroke, congestive heart failure, venous thromboembolism, cardiac arrhythmia, respiratory failure, or chronic pain requiring regular opioid medications |
Preoperative education requirements
Five studies described the preoperative education programs for both in- and outpatient surgery patients which included physical therapy instructions and nurse- and physiotherapist-led seminars.5-9 Two studies evaluating outpatient reconstruction of the anterior cruciate ligament gave crutch training, range of motion exercise demonstrations, and instruction in the use of a continuous passive motion device.5,9 Krywulak and colleagues (2005) did not make specific mention of the material covered in their program, but they chose to reinforce their presented material by providing handouts to patients.7 Bertin and colleagues (2005) included dislocation precautions in their physical therapy instructions.5 Kolisek and colleagues (2009) made at-home physiotherapy compulsory.8
Complications and patient outcomes
Kao and colleagues (1995) observed that two of the 25 outpatients were re-admitted for postanesthetic complications: one outpatient was re-admitted for vomiting unresponsive to antiemetics, and one outpatient was re-admitted for transient urinary retention.5 Novak and colleagues (1996) did not find any readmissions for pain or postanesthetic complications in either the outpatient or inpatient surgery group, although one inpatient later required re-operation for knee flexion contracture.10 Krywulak and colleagues (2005) found that patients who underwent outpatient reconstruction of the anterior cruciate ligament reported similar 24 hour-postoperative pain and nausea scores when compared to patients who underwent inpatient reconstructive surgery (P=0.79, P=0.26 respectively).7 Kolisek and colleagues (2009) evaluated the complication rate one-year following outpatient total knee arthroplasty procedures and found that there were no TKA-related complications.8 Lovald and colleagues (2014) compared complication rates following total knee arthroplasty among outpatient, 1-2 days in-hospital, 3-4 days in-hospital, and 5+ days in hospital groups.11 They found that the rate of joint pain 90 days post-surgery was lowest in the outpatient group but that there were no other statistically significant differences between groups.11
Patient satisfaction
Krywulak and colleagues (2005) surveyed patient satisfaction following in- and outpatient surgery of reconstruction of the anterior cruciate ligament using a patient satisfaction outcome questionnaire and found that the outpatient group was on average more satisfied in 19 of the 20 total questions in comparison to the inpatient group.7
Cost
There were seven cost studies which estimated an average cost savings of 17.6% to 57.6% for outpatient procedures relative to similar procedures performed in hospital (Table 4).5,6,9-13 Novak and colleagues (1996) reported that there was a significant difference in cost between the outpatient and inpatient surgery groups ($3225, P<0.001), but that among the inpatient surgery group the cost difference between an overnight stay and a two-day stay was not significant ($1463, P=0.07).6 Aronowitz and colleagues (1998) performed a cost analysis to account for the difference in cost between the outpatient and inpatient procedures and found that operating room charges made up 47% of the cost difference, overnight admission contributed 28% of the cost difference, and floor charges made up the remainder of the cost difference.9 Bertin and colleagues (2005) found that the outpatient total hip arthroplasty group required, on average $78,83 less for radiographs, $277,46 less for medication costs, $341,99 less for laboratory tests, $1002,87 for room costs, $2424,84 less for nursing costs and $472,04 less for therapy costs.6 Mather and colleagues (2011) found that the difference in cost of in-and outpatient operative repair of distal radius fracture using a volar plate was unaffected by ASA status, bone graft, carpal tunnel release, gender, age, surgeon experience, or fracture severity.12 Lovald and colleagues (2014) found that the incremental payments for osteoarthritis attributable costs at 2 years were lowest for the outpatient group and increased for in-hospital stays (of 1 day or longer).11 Aynardi and colleagues (2014) found that patients who underwent outpatient surgery reported more complications (although this did not reach statistical significance and included post-operative desaturations, intraoperative EKG changes and intra-operative non-displaced cal-car femorale fractures) but incurred significantly less final cost than the inpatient cohort.13
Table 4.
Procedural costs.
| Authors (Country, year) | Sample size | Investigated procedure | Results |
|---|---|---|---|
| Kao (USA, 1995)5 | 25 outpatient, 12 inpatient | Reconstruction of the anterior cruciate ligament | Mean total cost was $3905 at the outpatient center versus $9220 at the inpatient center |
| Novak (USA, 1996)10 | 45 outpatient, 29 inpatient | Reconstruction of the anterior cruciate ligament | Mean total cost was $8815 at the outpatient center versus $12,040 for an overnight stay at the inpatient center |
| Aronowitz (USA, 1998)9 | 34 outpatient, 1 inpatient | Reconstruction of the anterior cruciate ligament | Mean total cost was $3706 at the outpatient center versus $8406 at the inpatient center |
| Bertin (USA, 2005)6 | 10 inpatient, 10 outpatient | Total hip arthroplasty | Mean total cost was $19,021.24 at the outpatient center versus $23,087.38 at the inpatient hospital |
| Mather (USA, 2011)12 | 93 ASC, 37 inpatient | Volar plating for closed distal radius fractures | Mean total cost was $5220 at the ASC1 versus $7640 at the inpatient hospital |
| Lovald (USA, 2014)11 | 71,341 3-4 day inpatient, 23,134 5+day inpatient, 7755 1-2 day inpatient, 454 outpatient | Total knee arthroplasty | The 3-4 day group was the reference group and the incremental payments for osteoarthritis attributable costs at 2 years were -$8527 (lower) for the outpatient group,-$1967 (lower) for the 1-2 day group, and +$1159 (higher) for the 5+ day group |
| Aynardi (USA, 2014)13 | 119 outpatient, 78 inpatient | Total hip arthroplasty | Mean total cost was $24,529 at the outpatient center |
Discussion
Our paper provides a summary of the published literature in North America evaluating outpatient orthopedic surgery on cost and patient outcomes. This review included nine studies, and reported on eligibility requirements for inpatient versus outpatient care, operative rehabilitative practices, complications and patient outcomes, patient satisfaction, and when available total mean costs.
We found that the eligibility requirements for outpatient surgery varied but generally included patient consent, no history of significant medical problems, a caregiver at home following surgery and close proximity to outpatient center. Studies varied with respect to placing restrictions on patient age and time from injury to surgery. These criteria are in place to ensure that patients who are selected for outpatient surgery are not at increased risk of complications following surgery, will have an equally good or better chance of full recovery with minimal supervision following outpatient surgery and as well do not contradict the minimal exclusion criteria set forth by CMS for ambulatory surgery.14
We also found that preoperative education programs were not always prescribed and practices varied between hospitals and outpatient centers. Preoperative training informs the patient about the procedure and expected outcomes and addresses any anxiety or fear the patient may be experiencing.15 Additionally, preoperative education has been found to reduce requests for postoperative pain medication and increase patient satisfaction.15 This may be of particular importance to outpatients, since the most commonly reported postoperative complication of outpatient anesthesia is pain.15 Because of these benefits, it is important for hospitals and outpatient centers to establish preoperative education programs that are well-designed and include an effective protocol.15
The studies included in our review reported that outpatient surgeries had similar or improved rates of pain and nausea. Other studies have likewise reported that major morbidity and mortality following ambulatory procedures including anesthesia is extremely rare.16 This trend can likely be explained by the selection of healthier patients for outpatient surgery, as well as the monitoring practices and governmental regulations which concern outpatient surgical facilities.14
Patients who undergo outpatient orthopedic surgeries have been found to experience similar or increased satisfaction as inpatients. This has been observed in other countries outside of North America as well. Mira and colleagues (2009) performed a survey in 24 public Spanish hospitals and found that more patients in the outpatient group were satisfied with their procedure than patients in the inpatient group (88.3%, 77.0%, P<0.0001).16 There were surprisingly no comparative studies evaluating differences in patient outcomes or cost of outpatient versus inpatient orthopedic surgery outside of North America, and we speculate that reasons for this could include inaccessibility of cost data to researchers or international differences in reimbursement schemes that make a study of outpatient care meaningless or impractical (i.e. health care insurance mandates a fixed length of stay following injury, etc.).
Finally, we found that outpatient procedures were associated with greater cost savings (up to 60% in mean total cost) than inpatient procedures. Contributors to cost reductions were identified as operating room charges, overnight admission charges, and floor charges; and more specifically as costs associated with radiographs, medication, laboratory tests, room, nursing and therapy.6,9 Novak et al. (1996) and Lovald et al. (2014) found that cost savings in outpatient centers extended beyond length of stay.10,11 However, shorter stays remain a significant cause of cost savings as confirmed by Marla and Stallard (2009) which compared the cost of breast cancer day surgery versus 2-3 day stay performed in hospital found cost savings of 40% or 237 more.17
Conclusions
The current review demonstrates the lack of high quality evidence that directly compares outpatient and inpatient orthopedic procedures. Few studies have compared the outcomes and indications for outpatient procedures despite their growing popularity.3 Our review is strengthened by the large patient populations within the included studies, providing more accurate comparisons of outpatient versus inpatient orthopedic procedures. We found several areas where outpatient orthopedic surgical procedures have potential benefits over inpatient procedures, including patient satisfaction and cost. The results of our review suggest that patients who underwent outpatient orthopedic surgeries did not have to trade quality of care for cost savings.
In conclusion, we found that a representative group of select orthopedic surgeries increasingly performed as outpatient procedures appears to be cost-effective and safe alternative to inpatient care for patients considered low risk for immediate post-operative complications. As new technology emerges providing for safer surgery, an expansion of the procedures eligible for ambulatory surgery may depend on better defining patient eligibility characteristics and processes to prepare for out-patient recovery. This, rather than simply using the traditional approach of designating any one surgical procedure as exclusively requiring in-patient care. In this manner, a broader spectrum of procedures may become eligible for the safe and effective option of ambulatory surgery, avoiding the historical requirements and costs of overnight hospital-ization and monitoring.
Funding Statement
Funding: the work was supported by a grant from Moximed Inc.
References
- 1.Ambulatory surgery centers: a positive trend in health care. Ambulatory Surgery Center Association. Available from: http://www.ascassociation.org/Resources/ViewDocument/?DocumentKey=7d8441a1-82dd-47b9-b626-8563dc31930c. Accessed November 27, 2014
- 2.Cullen KA, Hall MJ, Golosinskiy A. Ambulatory Surgery in the United States, 2006. National health statistics reports; no 11. Revised. Hyattsville, MD: National Center for Health Statistics; 2009. [PubMed] [Google Scholar]
- 3.Kim S, Bosque J, Meehan J P, et al. Increase in outpatient knee arthroscopy in the United States: a comparison of National Surveys of Ambulatory Surgery, 1996 and 2006. J Bone Joint Surg Am 2011;93:994-1000. [DOI] [PubMed] [Google Scholar]
- 4.Wier LM (Truven Health Analytics), Steiner CA (AHRQ), Owens PL (AHRQ) Surgeries in Hospital-Owned Outpatient Facilities, 2012. HCUP Statistical Brief #188. February 2015. Agency for Healthcare Research and Quality, Rockville, MD. Available at: http://www.hcup-us.ahrq.gov/reports/stat-briefs/sb188-Surgeries-HospitalOutpatient-Facilities-2012.pdf.
- 5.Kao JT, Giangarra CE, Singer G, Martin S. A comparison of outpatient and inpatient 277 anterior cruciate ligament reconstruction surgery. Arthroscopy 1995;11:151-6. [DOI] [PubMed] [Google Scholar]
- 6.Bertin KC. Minimally invasive outpatient total hip arthroplasty: a financial analysis. Clin Orthop Relat Res 2005;435:154-63. [DOI] [PubMed] [Google Scholar]
- 7.Krywulak SA, Mohtadi NG, Russell ML, Sasyniuk TM. Patient satisfaction with inpatient versus outpatient reconstruction of the anterior cruciate ligament: a randomized clinical trial. Can J Surg 2005;48: 201-6. [PMC free article] [PubMed] [Google Scholar]
- 8.Kolisek FR, McGrath MS, Jessup NM, et al. Comparison of outpatient versus inpatient total knee arthroplasty. Clin Orthop Relat Res 2009;467:1438-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aronowitz ER, Kleinbart FA. Outpatient ACL reconstruction using intraoperative local 287 analgesia and oral postoperative pain medication. Orthopedics 1998;21:781-4. [DOI] [PubMed] [Google Scholar]
- 10.Novak PJ, Bach BR Jr, Bush-Joseph CA, Badrinath S. Cost containment: a charge comparison of anterior cruciate ligament reconstruction. Arthroscopy 1996;12:160-4. [DOI] [PubMed] [Google Scholar]
- 11.Lovald ST, Ong KL, Malkani AL, et al. Complications, mortality, and costs for outpatient and short-stay total knee arthro-plasty patients in comparison to standard-stay patients. J Arthroplasty 2014;29:510-5. [DOI] [PubMed] [Google Scholar]
- 12.Mather RC 3rd, Wysocki RW, Mack Aldridge J, 3rd, et al. Effect of facility on the operative costs of distal radius fractures. J Hand Surg Am 2011;36:1142-8. [DOI] [PubMed] [Google Scholar]
- 13.Aynardi M, Post Z, Ong A, et al. Outpatient surgery as a means of cost reduction in total hip arthroplasty: a case-control study. HSS J 2014;10:252-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Code of Federal Regulations. Covered Surgical Procedures, 42 C.F.R. § 411.16. Available from: http://www.ecfr.gov/cgibin/textidx?rgn=div5&node=42:3.0.1.1.3#se42.3.416_1166.
- 15.Kruzik N. Benefits of preoperative education for adult elective surgery patients. AORN J 2009;90:381-7. [DOI] [PubMed] [Google Scholar]
- 16.Marshall SI, Chung F. Discharge criteria and complications after ambulatory surgery. Anesth Analg 1999;88:508-17. [DOI] [PubMed] [Google Scholar]
- 17.Mira JJ, Tomás O, Virtudes-Pérez M, et al. Predictors of patient satisfaction in surgery. Surgery 2009;145:536-41. [DOI] [PubMed] [Google Scholar]


