Summary
Background
Patient misidentification, as a major patient safety issue, occurs in any healthcare setting and leads to inappropriate medical procedures, diagnosis or treatment, with serious outcomes.
Objectives
The study aimed to investigate the effectiveness of wristband bar-code medication scanning to reduce medical errors (ME).
Methods
A meta-analysis study was conducted. The relevant studies were searched in PubMed, Embase, Cochrane Library, Web of Science and Scopus from 1990 to March 2015. Thereafter, the studies retrieved were screened based on predefined inclusion and exclusion criteria. Data were extracted, and the quality of the included studies was evaluated using the STROBE checklist.
Results
In total, 14 articles involving 483 cases were included. The meta-analysis indicated that the use of wristband bar-code medication scanning can reduce the ME around 57.5% (OR=0.425, 95% CI: 0.28-0.65, P<0.001). The study results showed a marked heterogeneity in the subgroup analysis (I-squared=98%). This was I2=70.35, P-value=0.018 for the type of samples and I2=99%, P-value<0.001 for years and countries.
Conclusion
Wristband bar-code medication scanning can decrease the ME in hospital setting. Since the patient’s safety is the main goal of the World Health Organization, it is recommended that a unique patient identification barcode should be used with name, medical record number, and bar-coded financial number.
Key words: Patient wristband, electronic barcode, medical error
1. Background
Preventable medical errors (MEs) are a leading cause of medical injuries worldwide [1]. Patient misidentification can lead to inappropriate medical procedures, diagnosis or treatment, with serious outcomes [2]. Misidentification, as a major patient safety issue [3], can occur in any healthcare setting, such as hospital wards, outpatient clinics, laboratory, and radiology and even in primary healthcare settings [2]. A study showed that more than 160 000 adverse medical events may occur in the United States (US) each year because of misidentified laboratory specimens [4]. Patient identification is the first goal of 16 National Patient Safety Goals (NPSG) determined by the Joint Commission (JC) hospital authorization program [2]. Accurate identification of patients, their specimens and laboratory test results is critically important in order to provide effective and appropriate healthcare [5]. It is crucial to ensure accurate patient identification to prevent ME [6].
The goal of error reduction and substantially increased productivity and accuracy can be achieved through a system-focused approach that reduces reliance on human data entry and human double-checking through increased use of computer technology [7]. Information technology improves the quality, safety, and efficiency of health care and hospital processes. Reducing medication errors, including drug mistake and dosage error can be due to the use of information technology in hospital processes [8]. One potential way to reduce such errors is through the use of wristband bar-code medication scanning technology [9]. In the US, approximately 24% of the hospitals have implemented this technology to verify patient identification [1, 10] and it has been steadily increasing. Wristband bar-code medication scanning noticeably reduces medication errors (unauthorized drug, wrong form, wrong dose, wrong route, extra dose, and omission) [11], length of hospitalization and additional costs [9]. Wristband bar-code medication scanning is effective in the process of physician ordering, pharmacy dispensary and medication administration by nurses [12]. Moreover, this technology ensures the patient’s safety in laboratory [6], and assists nurses in confirming the patients’ identification [10].
Some studies have confirmed that that bar code-based computerized tracking system reduced the proportion of rejected blood samples and increased the patient’s safety [1, 11, 13, 14]. However, Murphy et al. showed a simple intervention in the form of a barrier warning label on blood bags reminding the staff to check the patient’s wristband failed to improve bedside transfusion practice [15].
2. Objective
To date, few studies have compared the relative effectiveness of wristband bar-code medication scanning on reduction of ME that have controversial results [12, 16–19]. Therefore, the meta-analysis study was conducted to investigate on the effectiveness of wristband bar-code medication scanning in the process of patient identification. It can be useful to improve the usability of patient wristband in hospital.
3. Methods
A meta-analysis study was conducted and the random effect model was used because of the differences in the effect size indices in different studies (the main assumption of random effect model). The studies were collected from databases, including PubMed, Scopus, Embase, Web of science and Cochrane library from 1990 to 2015. The researchers concurrently searched the studies with the title of effectiveness of wristband in preventing MEs using English keywords, such as patient wristband, patient bracelet, patient identification labels and patient wristlet. Using STROBE checklist to investigate the quality of articles [20], 14 articles were eligible to be used for the study. The names of the authors and journals were concealed and two researchers of the research group checked the including and excluding criteria. Disagreements were judged by the third researcher.
The inclusion criteria were
application of wristband in hospital, and
effect of wristband bar-code medication scanning on ME.
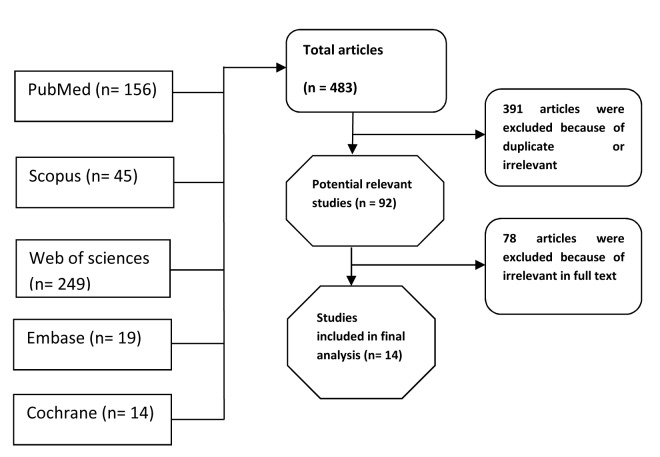
Besides, the studies which did not report the effect of patient wristband on ME were excluded. The steps of selecting articles are shown in ►Figure 1. The papers that were expressed in the result section with their characterization are shown in ►Table 1.
Fig. 1.
Flow diagram of the studies reviewed for this meta-analysis.
Table 1.
Characteristics of the studies included in the meta-analysis.
| Studies | Country | Year | Sample size | Before intervention | After intervention | Sample type |
|---|---|---|---|---|---|---|
| Morrison | USA | 2010 | 184 043 | 0.054% | 0.032% | patient specimen |
| Porcena | USA | 2005 | 8 824 | 1.82% | 0.17% | blood sample |
| Helmons | USA | 2009 | 654 | 11.65% | 10.75% | blood sample |
| DeYoung | USA | 2009 | 47 | 19.70% | 8.70% | patient |
| Askeland | USA | 2009 | 34 000 | 1.82% | 0.17% | blood products |
| Poon | USA | 2010 | 35 | 10.43% | 6.86% | patient |
| Mayo | USA | 1994 | 27 | 30.00% | 41% | patient |
| Morriss | USA | 2009 | 483 | 8.21% | 4.14% | patient |
| Murphy | UK, USA | 2007 | 242 | 32.7% | 34.12% | medication error |
| Bologna | Ridgewood | 2002 | 59 490 | 0.017% | 0.007% | blood specimen |
| Brown | Columbia | 2010 | 458 461 | 0.0226% | 0.0017% | blood specimen |
| Hayden | USA | 2009 | 37 040 | 0.032% | 0.005% | blood specimen |
| Hill | USA | 2010 | 334 039 | 0.42% | 0.11% | patient specimen |
| Kileen | USA | 2005 | 22 574 | 0.256% | 0.049% | patient specimen |
In the classification process of articles based on the inclusion criteria and the STROBE checklist, 14 relevant articles were identified. Data were analyzed and the results reported using a random-effects model with 95% confidence interval (CI) via CMA (Comprehensive Meta-Analysis) software. The heterogeneity was determined through Q, T2 and I2 indexes.
It is noteworthy that when the information was not reported in the studies, needed data were provided by contact with the corresponding authors. The Q index was used to estimate the significance of heterogeneity effect; also, T2 and I indexes were used to estimate its rate. Inverse method was used to estimate variances and weighting of the studies (1/ variance within studies + variance between studies).
4. Results
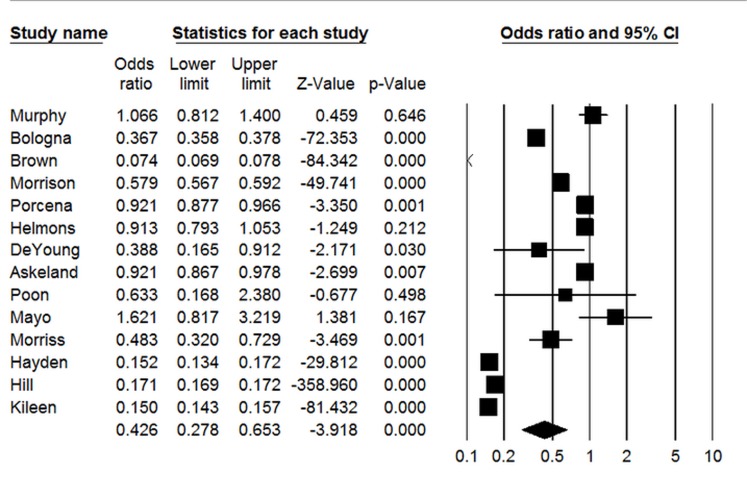
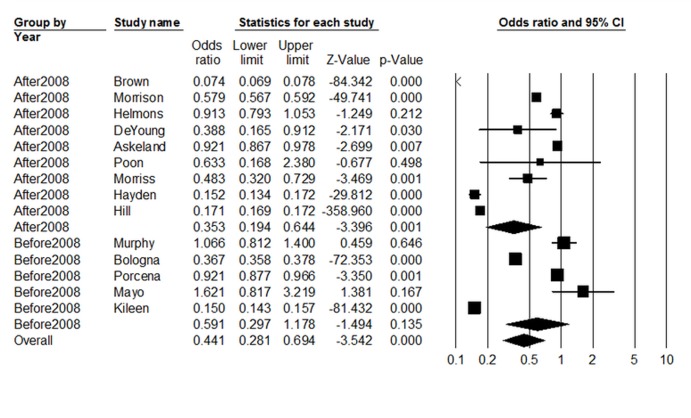
The results of the analysis showed that the pooled effect size of studies was equal to OR=0.426 (95% CI: 0.273–0.653), It indicated that wristband bar-code medication scanning can reduce some MEs about to 57.4% in the hospital. Also, the results of Chi-square test showed that there was a significant difference among the studies’ results (P-value=0.001). Furthermore, the finding of Tau-squared showed a significant difference among the studies’ results (T2=0.619). In addition, the I-squared result indicated that more than 98% of the total difference among the studies’ results was due to true variance (►Figure 2).
Fig. 2.
The forest plots for association between patient wristband and ME with using random effects model.
The indices related to heterogeneity included Chi-squared=288.59 (d.f.=13) P=0.001, estimation of between-study variance was Tau-squared=0.001, I-squared=98% and Z=–3.918, P=0.001, which showed that the heterogeneity among the studies is real; showing effects of other variables on the pooled effect size. Therefore, for determining of these variables on heterogeneity, sub-group analysis was applied. The finding of sub-group analysis is shown in ►Figures 3 to 5.
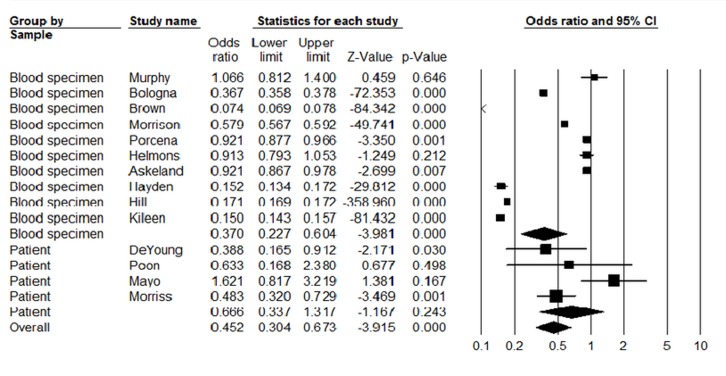
Fig. 3.
Subgroup analysis of the association between patient wristband and ME based on the type of samples.
According to ►Figure 3, the pooled effect size of studies conducted on blood specimen samples was OR=0.370 (95% CI: 0.227–0.604) and in the patients it was OR=0.666 (95% CI: 0.337–1.317). It showed that effectiveness of wristband bar-code medication scanning in the blood specimen samples is more than the patient samples. Also, the results related to heterogeneity for ►Figure 3 are shown in ►Table 2.
Table 2.
Heterogeneity between the sample type of the patient wristband and ME.
| Groups | Effect size and 95% Interval | Test of null (Two-Tail) | Heterogeneity | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Group | Number of Studies | Point estimate | Lower limit | Upper limit | Z-value | P-value | Q-value | df (Q) | P-value | I-squared |
| Fixed effect analysis | ||||||||||
| blood | 10 | 0.229 | 0.227 | 0.231 | -363.196 | 0.000 | 19 303.546 | 9 | 0.000 | 99.953 |
| patient | 4 | 0.616 | 0.449 | 0.846 | -2.999 | 0.003 | 10.120 | 3 | 0.018 | 70.355 |
| Random effects analysis | ||||||||||
| blood | 10 | 0.370 | 0.227 | 0.604 | -3.981 | 0.000 | ||||
| patient | 4 | 0.666 | 0.337 | 1.317 | -1.167 | 0.243 | ||||
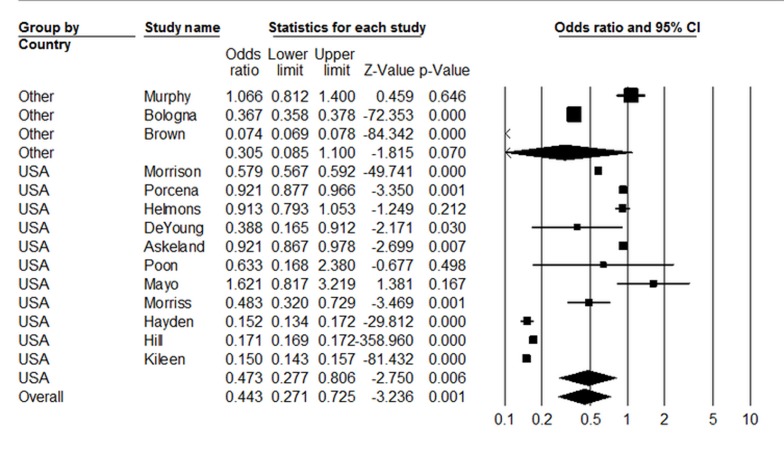
As shown in ►Table 2, the heterogeneity between studies was remained following the sub-group analysis based on the samples type. According to ►Figure 4, the pooled effect size of studies conducted in USA was OR=0.473 (95% CI: 0.277–0.806) and in other countries it was OR=0.305 (95% CI: 0.085–1.10); indicating the reducing effect of wristband bar-code medication scanning on ME. Also, the results related to heterogeneity of ►Figure 4 are shown in ►Table 3. As shown in ►Table 3, the heterogeneity between studies was sustained. The role of years of the studies on the heterogeneity is revealed in ►Figure 5. It shows that the pooled effect size of studies conducted in year 2008 and after that was OR=0.423 (95% CI: 0.23–0.775) and in the years of before 2008 it was OR=0.422 (95% CI: 0.224–0.793). The effect size in this section was same between the studies based on the years of studies. Also, the results related to heterogeneity of ►Figure 5 are shown in ►Table 4. In a ddition, the heterogeneity between the studies remained after subgroup analysis by the years of studies.
Fig. 4.
Subgroup analysis of association between patient wristband and ME based on the countries.
Table 3.
Heterogeneity between countries of the patient and ME.
| Groups | Effect size and 95% Interval | Test of null (Two-Tail) | Heterogeneity | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Group | Number of Studies | Point estimate | Lower limit | Upper limit | Z-value | P-value | Q-value | df (Q) | P-value | I-squared |
| Fixed effect analysis | ||||||||||
| Other | 3 | 0.284 | 0.277 | 0.291 | -100.034 | 0.000 | 2342.020 | 2 | 0.000 | 99.915 |
| USA | 11 | 0.224 | 0.222 | 0.226 | -249.570 | 0.000 | 16 686.310 | 10 | 0.000 | 99.940 |
| Total within | 19 028.330 | 12 | 0.000 | |||||||
| Total between | 322.750 | 1 | 0.000 | |||||||
| Overall | 14 | 0.229 | 0.228 | 0.231 | -363.157 | 0.000 | 19 351.080 | 13 | 0.000 | 99.933 |
Fig. 5.
Subgroup analysis of the association between patient wristband and ME based on years of studies conduction.
Table 4.
Heterogeneity between years of the studies on the patient wristband and ME.
| Groups | Effect size and 95% Interval | Test of null (Two-Tail) | Heterogeneity | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Group | Number of Studies | Point estimate | Lower limit | Upper limit | Z-value | P-value | Q-value | df (Q) | P-value | I-squared |
| Fixed effect analysis | ||||||||||
| <2008 | 5 | 0.292 | 0.285 | 0.298 | -103.687 | 0.000 | 1 122.177 | 4 | 0.000 | 99.644 |
| >2008 | 9 | 0.222 | 0.220 | 0.224 | -348.701 | 0.000 | 17 768.603 | 8 | 0.000 | 99.955 |
| Total within | 18 890.780 | 12 | 0.000 | |||||||
| Total between | 460.300 | 1 | 0.000 | |||||||
| Overall | 14 | 0.229 | 0.228 | 0.231 | -363.157 | 0.000 | 19 351.080 | 13 | 0.000 | 99.933 |
5. Discussion
Several studies conducted around the world have emphasized significance of wristband bar-code medication scanning on ME. The present meta-analysis sought to estimate the effectiveness of patient wristband bar-code scanning on prevention of MEs.
The results of the study indicated that the use of wristband in the hospital can reduce the incidence of ME around 57.5% (OR=0.425, 95% CI: 0.28–0.65). It is in accordance with the findings supporting the use of barcode to reduce ME in hospitals; Hayden reported that mislabeled specimens reduced from 0.032% to 0.005% [9]. Also, this technology reduced the medication error rate by 56% [1] and by 47% in neonatal intensive care units [14]. Other studies showed the effectiveness of this technology on reduction of ME [6–8, 11, 13]. The medical errors such as dosages and drugs errors can decrease in hospitals due to implementation of barcode technology.
According to implementation of this technology, medication administration errors decreased in medical units [11]. Askeland indicated that the blood sample rejection rate decreased from 1.82% to 0.17% after implementation of bar code–based tracking system [13]. Health managers should pay attention to proper use of this in the hospital to improve patients’ safety. However, Mayo found that the incidence of falls from bed cannot be significantly reduced in the patients who used wristband bar-code medication scanning in the hospital [21]. Although it is necessary to indicate that wristband is effective in identification of patients and related error, patient falls are not so related to identification by wristbands. Moreover, Murphy indicated that barcodes had no effect on the ME [15]. The sample size of her study was limited, as the results of the mentioned studies could be affected due to small sample size. Besides, checking with direct observation of practice was one of the difficulties in her study.
In total, wristband bar-code medication scanning, as a new technology, can prevent ME in more settings and it can be developed and distributed in hospitals for the improvement of patients’ safety. It leads to a decrease in hospital costs, improved quality and higher patient satisfaction. Since compliance with the bar code system has been very high with a low frequency of failure and it is accepted by the staff [13], it can be used in hospitals for improving the quality of services. Also, it is very likely to be safer than the prior manual system [12]. Therefore, it is recommended that an international guideline should be developed to use bar-codes for the patients’ identification in hospitals.
Besides, the use of bar codes is applicable in operation rooms [22] and it is suitable for all wards of hospital, especially in critical care wards. This technology has little errors [10] and it can be useful in health systems for increasing the patients’ safety. On the other hand, the implementation of wristband bar-code medication scanning not only reduce incidence of medication administration errors, but also has important implications for nursing workflow. Moreover, wristband bar-code medication scanning can decrease around 25% of nursing work time spent on medication-related activities [23]. According to benefits of this technology; therefore, it is recommended that hospital managers and policy makers should pay more attention to proper use of it in hospitals.
The study results showed a marked heterogeneity for samples, years and countries of the studies. As, the studies conducted in the USA had a heterogeneity and it shows that the same country could not be a main factor in homogeneity. There was heterogeneity between the studies before and after 2008. It may be perhaps due to the sample size of the studies, because the sample sizes ranged from 27 to 458 461 samples in the studies [21, 24]. On the other hand, studies done in different wards of the hospital showed that it may be due to the heterogeneity. The setting of the studies was different and some studies were conducted in only one or two general care centers such as medical-surgical and cardiac telemetry units [12, 17] or in neonatal intensive care unit [14]. The results differ since implementing barcode technology decreased medication administration errors in medical-surgical units more than intensive care units [11]. Also, checking wristband period was different between studies lasting for less than four weeks and in some studies it was over one year [9]. Moreover, in some studies the wristbands were checked by specimen bar code and in others only patient wristbands were checked. It can be one of the reasons of heterogeneity.
It is notable that in some studies more than five persons performed the observation and data gathering [11] and in other studies fewer people were involved [1].The software used in the studies were different, so Helmons used Stata for analysis [11] and some used SPSS.
Also, in the studies different error-detection methods were used (i.e. direct observation versus voluntary reporting or medical chart review), it can make different results in the studies.
Moreover, in some studies there was a Hawthorne effect [1, 11]. Besides, some studies showed that this technology can reduce some ME such as medication error [11]. In this regard, DeYoung found that wrong administration time errors decreased more than 50% post- implementation and there were no significant differences in other error types [1]. In addition, some studies focused on the medication errors especially [1] and others assessed all ME; therefore, it can lead to heterogeneity.
6. Conclusion
Wristband bar-code scanning can decrease the ME in hospital processes. Since the patient’s safety is a main goal of the World Health Organization, it is recommended that unique patient identification wristbands should be used with name, medical record number, and bar-coded financial number. Also, it should be determined if bar-coded wristband will reduce errors in each hospital and within each setting within hospitals. A procedure should be defined for immediate application of a wristband when a wristband is absent and there is a need for guest services to ensure that all patients are wearing a wristband. Moreover, it is recommended that the heterogeneity reasons should be taken into account in future studies.
Acknowledgement
The authors would like to acknowledge all the participants who helped us do this research with their supports and cooperation’s. Hereby, the authors would like to thank Dr. N. Shokrpour at Research and Consultation Center of Shiraz University of Medical Sciences for improving the use of English in the manuscript.
Footnotes
- Wristband barcode scanning decreases the ME in hospital processes.
- This technology is useful in health system; however, few studies have been conducted in this field.
Conflict of Interest
The researchers declared no conflicts of interest in relation to this article.
Human Subject Protections
No human subjects were engaged in the completion of this work, and no identified personal health information was used in the analyses reported.
References
- 1.DeYoung JL, Vanderkooi ME, Barletta JF. Effect of bar-code-assisted medication administration on medication error rates in an adult medical intensive care unit. Am J Health Syst Pharm 2009; 66(12):1110–1115. [DOI] [PubMed] [Google Scholar]
- 2.Dhatt GS, Damir HA, Matarelli S, Sankaranarayanan K, James DM. Patient safety: patient identification wristband errors. Clin Chem Lab Med 2011; 49(5):927–929. [DOI] [PubMed] [Google Scholar]
- 3.Zarbo RJ, Tuthill JM, D’Angelo R, Varney R, Mahar B, Neuman C, Ormsby A. The Henry Ford Production System Reduction of Surgical Pathology In-Process Misidentification Defects by Bar Code-Specified Work Process Standardization. Am J Clin Pathol 2009; 131(4):468–477. [DOI] [PubMed] [Google Scholar]
- 4.Valenstein PN, Raab SS, Walsh MK. Identification errors involving clinical laboratories. Arch Pathol Lab Med 2006; 130(8):1106–1113. [DOI] [PubMed] [Google Scholar]
- 5.Snyder SR, Favoretto AM, Derzon JH, Christenson RH, Kahn SE, Shaw CS, Baetz RA, Mass D, Fantz CR, Raab SS, Tanasijevic MJ, Liebow EB. Effectiveness of barcoding for reducing patient specimen and laboratory testing identification errors: a Laboratory Medicine Best Practices systematic review and meta-analysis. Clin Biochem 2012; 45(13):988–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morrison AP, Tanasijevic MJ, Goonan EM, Lobo MM, Bates MM, Lipsitz SR, Bates DW, Melanson SE. Reduction in specimen labeling errors after implementation of a positive patient identification system in phlebotomy. Am J Clin Pathol 2010; 133(6):870–877. [DOI] [PubMed] [Google Scholar]
- 7.Porcella A, Walker K. Patient safety with blood products administration using wireless and bar-code technology. AMIA Annu Symp Proc 2005: 614–618. [PMC free article] [PubMed] [Google Scholar]
- 8.Poon EG, Keohane CA, Yoon CS, Ditmore M, Bane A, Levtzion-Korach O, Moniz T, Rothschild JM, Kachalia AB, Hayes J, Churchill WW, Lipsitz S, Whittemore AD, Bates DW, Gandhi TK. Effect of bar-code technology on the safety of medication administration. N Engl J Med 2010; 362(18):1698–1707. [DOI] [PubMed] [Google Scholar]
- 9.Hayden RT, Patterson DJ, Jay DW, Cross C, Dotson P, Possel RE, Srivastava DK, Mirro J, Shenep JL. Computer-assisted bar-coding system significantly reduces clinical laboratory specimen identification errors in a pediatric oncology hospital. J Pediatr 2008; 152(2):219–224. [DOI] [PubMed] [Google Scholar]
- 10.Howanitz PJ, Renner SW, Walsh MK. Continuous wristband monitoring over 2 years decreases identification errors: a College of American Pathologists Q-Tracks Study. Arch Pathol Lab Med 2002; 126(7):809–815. [DOI] [PubMed] [Google Scholar]
- 11.Helmons PJ, Wargel LN, Daniels CE. Effect of bar-code-assisted medication administration on medication administration errors and accuracy in multiple patient care areas. Am J Health Syst Pharm 2009; 66(13):1202–1210. [DOI] [PubMed] [Google Scholar]
- 12.Poon EG, Keohane C, Featherstone E, Hays B, Dervan A, Woolf S, Hayes J, Bane A, Newmark L, Gandhi TK. Impact of barcode medication administration technology on how nurses spend their time on clinical care. AMIA Annu Symp Proc 2006: 1065. [PMC free article] [PubMed] [Google Scholar]
- 13.Askeland RW, McGrane SP, Reifert DR, Kemp JD. Enhancing transfusion safety with an innovative bar-code-based tracking system. Healthc Q 2008; 12: 85–89. [DOI] [PubMed] [Google Scholar]
- 14.Morriss FH, Abramowitz PW, Nelson SP, Milavetz G, Michael SL, Gordon SN, Pendergast JF, Cook EF. Effectiveness of a barcode medication administration system in reducing preventable adverse drug events in a neonatal intensive care unit: a prospective cohort study. J Pediatr 2009; 154(3):363–368. [DOI] [PubMed] [Google Scholar]
- 15.Murphy MF, Casbard AC, Ballard S, Shulman IA, Heddle N, Aubuchon JP, Wendel S, Thomson A, Hervig T, Downes K, Carey PM, Dzik WH. Prevention of bedside errors in transfusion medicine (PROBE-TM) study: a cluster***/randomized, matched***paired clinical areas trial of a simple intervention to reduce errors in the pretransfusion bedside check. Transfusion 2007; 47(5):771–780. [DOI] [PubMed] [Google Scholar]
- 16.Paoletti RD, Suess TM, Lesko MG, Feroli AA, Kennel JA, Mahler JM, Sauders T. Using bar-code technology and medication observation methodology for safer medication administration. Am J Health Syst Pharm 2007; 64(5): 536-543. [DOI] [PubMed] [Google Scholar]
- 17.Franklin BD, O’Grady K, Donyai P, Jacklin A, Barber N. The impact of a closed-loop electronic prescribing and administration system on prescribing errors, administration errors and staff time: a before-and-after study. Qual Saf Health Care 2007; 16(4): 279-284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sakowski J, Leonard T, Colburn S, Michaelsen B, Schiro T, Schneider J, Newman JM. Using a bar-coded medication administration system to prevent medication errors in a community hospital network. Am J Health Syst Pharm 2005; 62(24): 2619-2625. [DOI] [PubMed] [Google Scholar]
- 19.Johnson CL, Carlson RA, Tucker C, Willette C. Using BCMA software to improve patient safety in Veterans Administration Medical Centers. JHIM 2001; 16(1):46–51. [PubMed] [Google Scholar]
- 20.Stevanovic A, Coburn M, Rossaint R. Minimum requirements for high quality reporting of medical research results: CONSORT, STROBE and PRISMA statements. Anaesthesist 2015; DOI10.1007/s00101–015–0085–8 /?/ [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 21.Mayo NE, Gloutney L, Levy AR. A randomized trial of identification bracelets to prevent falls among patients in a rehabilitation hospital. Arch Phys Med Rehabil 1994; 75(12):1302–1308. [PubMed] [Google Scholar]
- 22.Ohsaka A, Furuta Y, Ohsawa T, Kobayashi M, Abe K, Inada E. Bar code-based pre-transfusion check in pre-operative autologous blood donation. Transfus Apher Sci 2010; 43(2):183–188. [DOI] [PubMed] [Google Scholar]
- 23.Keohane CA, Bane AD, Featherstone E, Hayes J, Woolf S, Hurley A, Bates DW, Gandhi TK, Poon EG. Quantifying nursing workflow in medication administration. J Nurs Adm 2008; 38(1):19–26. [DOI] [PubMed] [Google Scholar]
- 24.Brown JE, Smith N, Sherfy BR. Decreasing mislabeled laboratory specimens using barcode technology and bedside printers. J Nurs Care Qual 2011; 26(1):13–21. [DOI] [PubMed] [Google Scholar]