Abstract
American Indian women have lower cancer survival rates compared to non-Hispanic White women. Increased cancer screening fostered by culturally sensitive education and community programs may help decrease this disparity. This study assesses the effectiveness of Hopi Cancer Support Services (HCSS) in maintaining high rates of breast and cervical cancer screening among Hopi women and evaluates the impact of participation in HCSS programs on colorectal cancer (CRC) screening. A population-based survey was conducted on the Hopi reservation in 2012 (n = 252 women). Frequency of breast, cervical, and colorectal cancer screenings, participation in HCSS programs and barriers to screening were evaluated. Unconditional multiple logistic regression estimated the independent effect of the HCSS program on CRC screening. Approximately 88 % of Hopi women 40+ reported ever having had a mammogram; 71 % did so within the past 2 years. Approximately 66 % of women 50+ were ever screened for colorectal cancer (FOBT and/or colonoscopy). Women who had their last mammogram through HCSS were 2.81 (95 % CI 1.12, 7.07) times more likely to have been screened for CRC. Breast and cervical cancer screening continues at a high rate among Hopi women and is substantially greater than that reported prior to the inception of HCSS. Furthermore, participation in programs offered by HCSS is strongly associated with increased colorectal cancer screening. This tribal health program (HCSS) has strongly influenced cancer screening among Hopi women and is a model of a tribally run cancer prevention program.
Keywords: Cancer screening, Cancer, Screening, Reservation, Tribal health, Rural, Community health
Background
American Indian women have lower cancer survival rates compared to non-Hispanic White women [1]. Factors contributing to this disparity include lack of knowledge regarding screening and early detection [2, 3] and negative attitudes about cancer treatment [3]. The development of culturally sensitive cancer screening education for tribal groups may help decrease these disparities [4, 5]. American Indian women have shown that their use of both traditional and western medicine can promote well-being for themselves and their families [6, 7]. Several programs have demonstrated the effectiveness of personal navigators and/or Community Health Representatives (CHRs) in providing education and increasing cancer screening [8].
In 1996, the Hopi Tribe, upon the award of CDC Breast and Cervical Cancer Screening Program (BCCP) [9], began a comprehensive women’s cancer screening program entitled the Hopi Women’s Health Program (HWWP) [9]. HWHP was renamed Hopi Cancer Support Services (HCSS) in 2010 since its responsibilities expanded beyond women’s health. HCSS is part of the Hopi Tribe’s Department of Health and Human Services and has primary responsibility for increasing cancer screening, cancer knowledge, cancer awareness and cancer support for all residents living on the Hopi reservation. HCSS is located on the Hopi reservation in northern Arizona and is staffed by local tribal members.
In 2004, researchers from the University of Arizona and Northern Arizona University entered a partnership with HWHP to focus on cancer concerns of the Hopi Tribe. The partnership conducted a cross-sectional population based survey of women’s knowledge, attitudes, beliefs and behaviors about breast and cervical cancer and utilized data from the Hopi BCCP to determine the effectiveness of the HWHP. Researchers found that 2-year breast cancer screening rates increased among Hopi women age 40+ from less than 30 % in 1993 [10] to 69 % in 2005 [11]. This large increase was seen as a direct result of the HWHP programs.
In 2012, a population-based survey of 500 randomly selected Hopi tribal members age 18 and older, living on the reservation, was conducted by the partnership team. Using these data, we sought to determine whether current breast and cervical cancer screening behaviors remain consistent with the high rates observed in 2006, to identify current colorectal cancer (CRC) screening practices and to ascertain whether the HCSS program has positively influenced CRC screening behavior among Hopi women.
Methods
Data were from the 252 women participants in the 2012 population-based survey. This survey included questions about breast, cervical and colorectal cancer (CRC) screening practices, reasons for screening, barriers to screening, and location of the most recent screening. The research project was approved by Hopi Tribal Council and the University of Arizona Institutional Review Board.
Breast and cervical cancer screening behaviors were assessed by identifying whether Hopi women (n = 252) had ever been screened for cervical cancer and whether women age 40+ (n = 155) were ever screened for breast cancer. We examined how frequently women were being screened, where they were last screened and, if never screened, the reasons why not. These 2012 results were compared to results from the 2006 survey [11].
CRC screening was evaluated by creating a variable which reflected whether an age eligible woman (age 50+) ever had a fecal occult blood test (FOBT) and/or a colonoscopy. Frequency and motivation for these specific tests were first evaluated. Age-eligible women who had any CRC screening test were then compared to those who had no CRC testing on the following personal characteristics: socio-demographics, screening history, cancer experience, health status, attitudes toward cancer and information related to the Hopi culture (the use of traditional medicine, length of time living on the reservation and residency off the reservation).
To assess the influence of the HCSS program on ever having had any CRC screening, responses to all questions showing some participant interface with HCSS were individually analyzed in bivariate analyses. These questions were (1) attendance at cancer prevention programs presented by HCSS (Cancer101, HPV, Breast cancer, CRC, and Tobacco), (2) mammogram screening at the HCSS facility (3) screening at the recommendation of HCSS, (4) obtaining information about cancer from HCSS, (5) obtaining financial assistance from HCSS via the Hopi Cancer Assistance Fund, and (6) obtaining support in completing a Radiation Exposure Compensation Education Program (RECEP) application.
Unconditional multiple logistic regression was used to evaluate the independent effect of the HCSS program on having had any CRC screening. Prevalence odds ratios (OR) and 95 % confidence intervals (CI) were calculated as the measure of effect in both the bivariate and multivariate analyses. The initial full model included those variables which were statistically significantly associated at the 0.05 level with overall colorectal cancer screening in the bivariate analyses. Since many of the variables were collinear, decisions were made to exclude some variables. Factors included in the initial full model were: age, education, thinks health is better than most, been to a dentist, exercised, and the strong belief that getting screened for cancer helps find cancer earlier. The influence of the HCSS program was evaluated through the variable: having latest mammogram screening at HCSS. This variable was forced into all the models as the primary factor of interest. A parsimonious model for the remaining variables was created by sequentially removing non-statistically significant variables using a likelihood ratio test, until all remaining variables had a statistically significant effect. The final model included the following variables: age, education, having latest mammogram screening at HCSS, having been to a dentist (a surrogate for healthy behaviors) and the strong belief that getting screened for cancer helps find cancer earlier.
Results
Of the women interviewed, all (n = 252) were eligible for cervical cancer screening, 62 % (n = 155) were age 40+ and eligible for breast cancer screening and 48 % (n = 122) were age 50+ and eligible for CRC screening. These age criteria are consistent with those utilized by the CDC for the BCCP sites [9]. Table 1 provides a utilization profile of each cancer screening test.
Table 1.
Profile of cancer screenings among Hopi women, 2012 survey by type of screening test
| Pap | Mammogram | FOBT | Colonoscopy | |||||
|---|---|---|---|---|---|---|---|---|
| Age | 18+ | 40+ | 50+ | 50+ | ||||
| # Eligible | 252 | 155 | 122 | 122 | ||||
|
| ||||||||
| N | (%) | N | (%) | N | (%) | N | (%) | |
|
| ||||||||
| Screened | 216 | (86) | 138 | (88) | 63 | (52) | 55 | (45) |
| Length of time since last screening (% of those screened) | ||||||||
| <12 months ago | 66 | (31) | 66 | (48) | 21 | (33) | 7 | (13) |
| 1—<2 years ago | 60 | (28) | 44 | (32) | 10 | (16) | 5 | (9) |
| 2—<3 years ago | 31 | (14) | 12 | (9) | 8 | (13) | 7 | (13) |
| 3—<5 years ago | 18 | (8) | 7 | (5) | 11 | (17) | 11 | (20) |
| 5—<10 years ago | 17 | (8) | <5 | 8 | (13) | 18 | (33) | |
| 10 years ago | 9 | (4) | <5 | <5 | <5 | |||
| [10 years ago | 12 | (6) | <5 | <5 | <5 | |||
| Main reason for most recent test (% of those screened) | ||||||||
| Health provider | 17 | (8) | 9 | (7) | 11 | (17) | 11 | (20) |
| Part of routine exam | 177 | (82) | 121 | (88) | 38 | (60) | 29 | (53) |
| A specific problem | <5 | <5 | <5 | 8 | (15) | |||
Breast and Cervical Cancer Screening
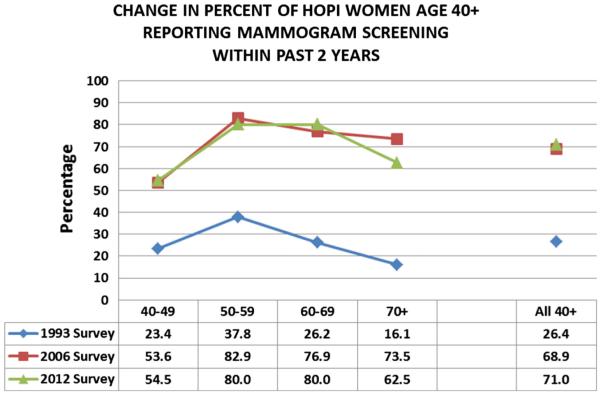
Approximately 86 % (n = 216) of women reported ever having a Pap test. Of those age-eligible, 73 % (n = 157) reported ever having a mammogram while 80 % (n = 110) of those screened did so no longer than 2 years ago. Most (70 %: n = 96) mammograms were done through HCSS. At least 90 % of age eligible women had their Pap test or mammogram as part of a routine exam or because a health professional recommended it. Reasons for not being screened included fear of the test or the results, lack of transportation or time, and not being told to do so. These reasons were reported with equal frequency. The 2012 mammogram screening results for all age groups are consistent with that found in 2006 and remain much higher than those reported in 1993 (Fig. 1).
Fig. 1.
Percent of Hopi women, age 40+ years, who reported receiving a mammogram within past 2 years by age group and by time period
Colorectal Cancer Screening
Of the age eligible women, approximately 52 % (n = 63) ever had a FOBT test and 45 % (n = 55) ever had a colonoscopy. Of those tested, 49 % (n = 31) had a FOBT within the past 2 years, and almost all had a colonoscopy within the past 10 years. At least 73 % had FOBTs or colonoscopies as part of a routine exam or because a health professional recommended it while 15 % (n = 8) had a colonoscopy because of a specific problem. Summarizing for any type of CRC screening, 66 % (n = 80) of the 122 age-eligible Hopi women reported having any type of CRC screening (FOBT and/or a colonoscopy); 31 % (n = 38) reported having had both a FOBT and a colonoscopy.
Multiple reasons were reported for not being screened for CRC. Approximately 31 % (n = 18) of those who did not have a FOBT and 39 % (n = 33) of those who did not have a colonoscopy indicated they were not told to have the test. Less than 5 persons who had no FOBT and 8 (12 %) who had no colonoscopy indicated they knew nothing about or never heard about the test.
A comparison of personal characteristics and behaviors stratified by ever/never being screened for CRC is found in Table 2. A smaller percentage of screened women was younger than age 65 (53 vs. 74 %), while a higher percentage was educated beyond high school (55 vs. 31 %), have a home landline (73 vs. 62 %) have lived off the Hopi reservation for at least 3 consecutive months (75 vs. 62 %) have had Pap testing (94 vs. 83 %), mammogram testing (99 vs. 86 %) and engage in healthy behaviors such as seeing a dentist in past year (81 vs. 60 %) or exercising (73 vs. 50 %). Also, a higher percentage of screened women perceived their health to be better than most (71 vs. 41 %), strongly believed in the efficacy of testing to find cancers early (94 vs. 79 %), attended at least one HCSS cancer education program (73 vs. 31 %) and had their latest mammogram done at HCSS (75 vs. 55 %).
Table 2.
Characteristics of Hopi women age 50+ ever screened and not ever screened for colorectal cancer
| Not screened (n = 42) |
Screened (n = 80) |
|||
|---|---|---|---|---|
| N | (%) | N | (%) | |
| Socio-demographic | ||||
| Age | ||||
| 50–64 years | 31 | (73.8) | 42 | (52.5) |
| 65–74 years | 5 | (11.9) | 25 | (31.3) |
| 75+ years | 6 | (14.3) | 13 | (16.3) |
| Education | ||||
| Less than 8th grade | <5 | <5 | ||
| 8–12 Grade but did not graduate | 11 | (26.2) | 10 | (12.5) |
| High school graduate/GED | 16 | (38.1) | 22 | (27.5) |
| Trade, technical or vocational school after HS | – | – | 8 | (10.0) |
| Some college but no degree | 8 | (19.0) | 15 | (18.8) |
| 2 Year college graduate or greater | 5 | (11.9) | 21 | (26.4) |
| Marital status | ||||
| Single | 10 | (23.8) | 16 | (20.0) |
| Married | 18 | (42.9) | 30 | (37.5) |
| Widowed | 9 | (21.4) | 19 | (23.8) |
| Separated/divorced | 5 | (11.9) | 15 | (18.8) |
| Employment | ||||
| Full-time or part time | 13 | (30.9) | 26 | (32.5) |
| Disabled/retired/not working | 29 | (69.0) | 54 | (67.5) |
| Household income | ||||
| Less than 10,000 | 18 | (42.9) | 33 | (41.3) |
| $10,000–$24,999 | 7 | (16.7) | 22 | (27.5) |
| $25,000–$34,999 | 5 | (11.9) | 12 | (15.0) |
| $35,000–$49,999 | 5 | (11.9) | 7 | (8.8) |
| $50,000–$74,999 | 7 | (16.7) | 6 | (7.6) |
| Transportation | ||||
| Has reliable source | 32 | (76.2) | 67 | (83.8) |
| Communication | ||||
| Has telephone landline | 26 | (61.9) | 58 | (72.5) |
| Has cell phone for personal use | 33 | (78.6) | 59 | (73.8) |
| Has home computer | 10 | (23.8) | 24 | (30.0) |
| Uses the internet | 14 | (33.3) | 26 | (32.5) |
| Hopi Culture | ||||
| Primary language spoken at home | ||||
| HOPI | 16 | (38.1) | 31 | (38.8) |
| Use of traditional medicine | ||||
| No times | 15 | (35.7) | 33 | (41.3) |
| 1–5 times | 19 | (45.2) | 38 | (47.5) |
| 6 time or more | 8 | (19.0) | 9 | (11.3) |
| Has lived off the Hopi reservation for at least 3 consecutive months | 26 | (61.9) | 60 | (75.0) |
| Average time living at current address (sd) | 38.7 (26.1) | 36.9 (22.4) | ||
| Average time living on the Hopi reservation (sd) | 46.2 (23.3) | 47.1 (22.3 | ||
| Screening history | ||||
| Ever had a Pap test | 35 | (83.3) | 75 | (93.8) |
| Ever had a mammogram | 36 | (85.7) | 79 | (98.8) |
| Cancer experience | ||||
| Has/had cancer | <5 | 11 | (13.8) | |
| Has a family history of cancer | 23 | (54.8) | 46 | (57.5) |
| Is a caregiver | 10 | (23.8) | 16 | (20.0) |
| Sought cancer information for self | 20 | (47.6) | 35 | (43.8) |
| Sought cancer information for a family member | 9 | (21.4) | 17 | (21.3) |
| Applied for radiation exposure compensation program | <5 | 6 | (7.5) | |
| Health status | ||||
| Has disabilities | 9 | (21.4) | 15 | (18.8) |
| Has diabetes | 18 | (42.9) | 39 | (48.8) |
| Is overweight or obese | 32 | (76.2) | 64 | (80.0) |
| Currently smokes cigarettes | <5 | <5 | ||
| Never smoked cigarettes | 35 | (83.3) | 70 | (87.5) |
| Thinks his/her health is better than most | 19 | (45.2) | 57 | (71.3) |
| Relationship with HCSS | ||||
| Attended at least 1 HCSS presentation | 13 | (31.0) | 57 | (71.3) |
| Screened at HCSS (mammogram only) | 23 | (54.8) | 60 | (75.0) |
| Healthy behaviors | ||||
| Has ever been to a dentist | 25 | (59.5) | 65 | (81.3) |
| Has had teeth cleaned | 21 | (50.0) | 55 | (68.8) |
| Exercised at least once in past 30 days | 21 | (50.0) | 58 | (72.5) |
| Always uses sunscreen | <5 | 14 | (17.5) | |
| Cancer attitudes: strongly agrees that | ||||
| Cancer is often caused by a person’s behavior or lifestyle | <5 | 9 | (11.3) | |
| Cancer is almost always fatal | 21 | (50.0) | 32 | (40.0) |
| Getting screened for cancer helps find cancer earlier | 33 | (78.6) | 75 | (93.8) |
Table 3 shows the association between ever screened for CRC and selected variables, unadjusted and unadjusted for other covariates. Unadjusted for other covariates, women who had received a screening mammogram through HCSS were 2.5 times more likely to also have been screened for CRC [OR 2.48 (1.12–5.46)] compared to women who either never had a mammogram or whose last mammogram was not at HCSS. Other factors showing statistically significant unadjusted associations with CRC screening included age (50–64 vs. 65+) [OR 0.39 (0.17–0.89)], education beyond High School [OR 2.59 (1.18–5.70)], ever having had a mammogram [OR 13.17 (1.53–113.42)], healthy behaviors such as seeing a dentist [OR 2.95 (1.28–6.78)], getting teeth cleaned [OR 2.20 (1.02–4.74)] and exercising [OR 2.64 (1.21–5.74)] and attendance at an HCSS educational program [OR 5.53 (2.45–12.48)]. Perceiving one’s health to be better than most [OR 3.00 (1.38–6.52)] and belief in the value of cancer testing [OR 4.09 (1.27–13.15)] were also associated with CRC screening.
Table 3.
Unadjusted and adjusted associations for ever having a colorectal cancer screening, Hopi women age 50+ (n = 122), odds ratios and 95 % confidence intervals
| Characteristic | Unadjusted OR (95 % CI)b |
Adjusteda
OR (95 % CI)b |
|---|---|---|
| Socio-demographics | ||
| Age: under age 65 | 0.39 (0.17–0.89)* | 0.19 (0.06–0.53)* |
| Education: educated beyond high school | 2.59 (1.18–5.70)* | 3.46 (1.38–8.70)* |
| Marital status: married | 0.80 (0.37–1.71) | |
| Income: household income under 35,000 | 2.06 (0.84–5.05) | |
| Transportation: has reliable transportation | 1.61 (0.64–4.06) | |
| Hopi Culture | ||
| Primary language spoken at home: Hopi | 1.03 (0.48–2.22) | |
| Used traditional medicine at least once in past 5 years | 1.10 (0.52–2.32) | |
| Screening history | ||
| Ever had a Pap test | 3.00 (0.89–10.12) | |
| Ever had a mammogram | 13.17 (1.53–113.42)* | |
| Cancer experience | ||
| Has/had cancer | 6.54 (0.81–52.49) | |
| Has a family history of cancer | 1.12 (0.53–2.37) | |
| Is a caregiver | 0.80 (0.33–1.96) | |
| Sought cancer information for self | 0.86 (0.40–1.81) | |
| Sought cancer information for a family member | 0.99 (0.40–2.46) | |
| Applied for RECP | 2.76 (0.87–8.76) | |
| Health status | ||
| Has disabilities | 0.85 (0.34–2.14) | |
| Has diabetes | 1.27 (0.60–2.69) | |
| Is overweight or obese | 1.25 (0.51–3.06) | |
| Currently smokes cigarettes | 0.51 (0.10–2.63) | |
| Never Smoked cigarettes | 1.40 (0.49–3.99) | |
| Thinks his/her health is better than most | 3.00 (1.38–6.52)* | |
| Relationship with HCSS | ||
| Attended at least 1 HCSS presentation | 5.53 (2.45–12.48)* | |
| Screened at HCSS (mammogram only) | 2.48 (1.12–5.46)* | 2.81 (1.12–7.07)* |
| Obtained information from HCSS | 1.06 (0.30–3.73) | |
| Obtained Support from HCSS | 1.74 (0.63–4.79) | |
| Healthy behaviors | ||
| Has been to a dentist | 2.95 (1.28–6.78)* | 3.10 (1.18–8.15)* |
| Has had teeth cleaned | 2.20 (1.02–4.74)* | |
| Exercised at least once in past 30 days | 2.64 (1.21–5.74)* | |
| Always uses sunscreen | 2.76 (0.75–10.20) | |
| Attitudes about cancer-strongly agrees that | ||
| Cancer is almost always fatal | 0.67 (0.31–1.41) | |
| Cancer is often caused by a person’s behavior or lifestyle | 1.20 (0.35–4.17) | |
| Getting screened for cancer helps find cancer earlier | 4.09 (1.27–13.15)* | 5.00 (1.22–20.44)* |
Statistically significant at the .05 level
Final model adjusted for other covariates in list
OR (95 %CI) = odds ratios and 95 % confidence intervals
Healthy behaviors such as seeing a dentist [OR 2.95 (1.28–6.78)] and getting teeth cleaned [OR 2.20 (1.02–4.74)] were highly correlated; the former was retained in the pool of explanatory variables since it had the largest effect size. Being screened at HCSS and ever having had a mammogram were also highly correlated. Since the former was the primary factor of interest, the latter was dropped from the pool of potential explanatory variables.
Adjusted for other covariates, women whose last mammogram was at HCSS were almost 3 times more likely to have been screened for CRC [OR 2.81 (1.12, 7.07)] compared to women who never had a mammogram or whose last mammogram was not at HCSS. Other factors positively associated with colorectal screening were having a strong belief that getting screened for cancer helps find cancer earlier [OR 5.00 (1.22–20.44)], engaging in healthy behaviors such as having been to the dentist [OR 3.10 (1.18–8.15)], and having a post-high school education [OR 3.46 (1.38–8.70)]. Younger age-eligible women (age 50–64) were also less likely to be screened for CRC than women age 65+ [OR 0.19 (0.06–0.53)].
Discussion
The natural experiment which occurred in 1996 with the creation of the HWHP Program clearly demonstrates the positive effect HCSS (HWHP’s successor) has had on breast and cervical cancer screening among Hopi women. In 1993, only 26 % [10] of Hopi women age 40+ had a mammogram within the past 2 years. By 2006, this percentage increased to 69 % [11] and further increased to 71 % in 2012. This conclusion is further supported when comparing these results to the screening percentages reported in the 2010 Arizona Behavioral Risk Factor Surveillance Survey (BRFSS). The latter reported that only 55.3 % of Arizona American Indians (AI) and 94.1 % of non-Hispanic Whites (NHW) ever had a mammogram [14] while approximately 88 % of Hopi women ever did so.
The current survey also indicates that the percentage of women over age 50 screened for CRC is higher among Hopi women compared to other AI in Arizona and that this percentage closely approximates that of NHW in Arizona. The EARTH study, conducted 2004–2007, reported that only 11.7 % of AI in the Southwest was screened for CRC via colonoscopy [15] and data from the 2010 Arizona BRFSS [14] showed differences between AI and NHW of almost 30 percentage points in FOBT testing (14.2 vs. 43.1 %) and almost 50 percentage points in sigmoidoscopy or colonoscopy testing (19.7 vs. 64.2 %). In contrast, the percentage of age eligible Hopi women who have had FOBT testing (52 %) was 11 percentage points higher than NHW and the gap in colonoscopy screening was smaller—approximately 20 % (45 vs. 64 %). Moreover, it is possible that the latter difference is an overestimate since the Hopi survey did not specifically capture information on sigmoidoscopy.
These analyses also demonstrate the considerable impact HCSS has had on CRC screening among Hopi women. Attendance at HCSS educational programs, interfacing with HCSS for information or support, and prior mammogram screening at HCSS are all associated with being screened for CRC. After adjusting for other covariates, women whose last mammogram was at HCSS were almost 3 times more likely to have been screened for CRC than those who were never screened or those who were screened elsewhere.
Both this study and the EARTH study found that age, education and prior cancer screening were associated with CRC screening; however we did not find an association with family history, smoking status, or presence of other medical conditions [15]. We did identify a significant association between perceived general health and CRC screening, but that was not observed in the EARTH study.
The most frequently chosen reason for not being screened for CRC was lack of provider input. Almost 33 % of women who had no FOBT testing and 50 % of those who never had a colonoscopy indicated that no one told them to have the test. Fear of a CRC test, fear of the results, embarrassment and lack of transportation were never or rarely indicated as possible barriers. These results appear inconsistent with the results from a nationwide web-based survey of Indian Health Service and tribal providers in which 88 % of providers indicated that they recommended FOBTs and that educational brochures were provided to their patients [16]. While recall bias may account for some of this discrepancy, it is possible that communication patterns between patient and provider are problematic.
There are several possible limitations with this current study, specifically selection bias and recall bias and insufficient statistical power. However, the women interviewed were randomly selected and represented all villages across the Hopi reservation and the response rate among women was high (74 %). Moreover, the findings for mammography and Pap testing were similar to those found 5 years earlier. All interviewers were local residents and were trained in proper interviewing methods. Finally, due to small cell sizes, we may not have had sufficient statistical power to detect effect size differences smaller than 2.8. This may have limited our ability to identify other factors statistically significantly associated with CRC screening. Therefore, our multivariate results should be interpreted as evidence of associations, not predictions.
Conclusion
This study clearly demonstrates that a tribally run cancer prevention program can significantly influence the prevalence of cancer screening in a tribal community and that HCSS is a thriving model of such a program.
Acknowledgments
This project was supported by [1] the Comprehensive Minority Institute/Cancer Center Partnership of the National Cancer Institute funded through the University of Arizona-Northern Arizona University Comprehensive [NAU/AZCC Partnership for Native American Cancer Prevention (NACP) 1U54CA143925-04] and [2] Arizona Department of Health Services, Arizona Biomedical Research Commission [Contract to UA: ADHS 13-031255/Brown (PI)].
Footnotes
Conflict of interest All authors confirm no conflicts of interest.
References
- 1.Dignan MB, Burhansstipanov L, Hariton J, Harjo L, Rattler T, Lee R, et al. A comparison of two Native American Navigator formats: Face-to-face and telephone. Cancer Control: Journal of the Moffitt Cancer Center. 2005;12(Suppl 2):28–33. doi: 10.1177/1073274805012004S05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Banner RO, Gotay CC, Enos R, Matsunaga DS, Hed-lund N, Issell BF, DeCambra H. Effects of a culturally tailored intervention to increase breast and cervical cancer screening in Native Hawaiians. National Institutes of Health, National Cancer Institute; Bethesda, MD: 1999. pp. 45–55. [Google Scholar]
- 3.Guadagnolo BA, Cina K, Helbig P, Molloy K, Reiner M, Cook EF, et al. Assessing cancer stage and screening disparities among Native American cancer patients. Public Health Reports. 2009;124(1):79–89. doi: 10.1177/003335490912400111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sanderson PR, Teufel-Shone NI, Baldwin JA, Sandoval N, Robinson F. Breast cancer education for Navajo women: A pilot study evaluating a culturally relevant video. Journal of Cancer Education: The Official Journal of the American Association for Cancer Education. 2010;25(2):217–223. doi: 10.1007/s13187-009-0036-7. doi:10.1007/s13187-009-0036-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Robinson F, Sandoval N, Baldwin J, Sanderson PR. Breast cancer education for Native American women: Creating culturally relevant communications. Clinical Journal of Oncology Nursing. 2005;9(6):689–692. doi: 10.1188/05.CJON.689-692. doi:10.1188/05.CJON.689-692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Canales M. Taking care of self: Health care decision making of American Indian women. Health Care for Women International. 2004;25(5):411–435. doi: 10.1080/07399330490438323. doi:10.1080/07399330490438323. [DOI] [PubMed] [Google Scholar]
- 7.Giuliano A, Papenfuss M, Guernsey De Zapien J, Tilousi S, Nuvayestewa L. Prevalence of chronic disease risk and protective behaviors among American Indian women living on the Hopi reservation. Annals of Epidemiology. 1998;8(3):160–167. doi: 10.1016/s1047-2797(97)00200-7. [DOI] [PubMed] [Google Scholar]
- 8.Petersen WO, Trapp MA, Sellers TA, Nicometo AM, Kaur JS. Evaluation of a training program to prepare community health representatives to promote breast and cervix cancer screening among Native American women. Journal of Cancer Education: The Official Journal of the American Association for Cancer Education. 2004;19(4):237–243. doi: 10.1207/s15430154jce1904_12. doi:10.1207/ s15430154jce1904_12. [DOI] [PubMed] [Google Scholar]
- 9.Control. CfD National Breast and Cervical Cancer Early Detection Program (NBCCEDP) 2013 http://www.cdc.gov/cancer/nbccedp/
- 10.Giuliano A, Papenfuss M, Guernsey de Zapien J, Tilousi S, Nuvayestewa L. Breast cancer screening among southwest American Indian women living on-reservation. Preventive Medicine. 1998;27(1):135–143. doi: 10.1006/pmed.1997.0258. doi:10.1006/pmed.1997.0258. [DOI] [PubMed] [Google Scholar]
- 11.Brown SR, Nuno T, Joshweseoma L, Begay RC, Good-luck C, Harris RB. Impact of a community-based breast cancer screening program on Hopi women. Preventive Medicine. 2011;52(5):390–393. doi: 10.1016/j.ypmed.2011.02.012. doi:10.1016/j.ypmed.2011.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.SAS . SAS Institute Inc; Cary, NC: [Google Scholar]
- 13.StataCorp . Stata statistical software: Release 13. StataCorp LP; College Station, TX: 2013. [Google Scholar]
- 14.Prevention. CfDCa . Behavioral risk factor surveillance system survey questionnaire. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; Altanta, GA: 2009. http://www.cdc.gov/brfss/ [Google Scholar]
- 15.Schumacher MC, Slattery ML, Lanier AP, Ma KN, Edwards S, Ferucci ED, et al. Prevalence and predictors of cancer screening among American Indian and Alaska native people: The EARTH study. Cancer Causes and Control. 2008;19(7):725–737. doi: 10.1007/s10552-008-9135-8. doi:10.1007/s10552-008-9135-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haverkamp D, Perdue DG, Espey D, Cobb N. A survey of Indian Health Service and tribal health providers’ colorectal cancer screening knowledge, perceptions, and practices. Journal of Health Care for the Poor and Underserved. 2011;22(1):243–257. doi: 10.1353/hpu.2011.0014. doi:10.1353/hpu.2011.0014. [DOI] [PubMed] [Google Scholar]