Abstract
Background
This study examined the association between self-reported levels of household disaster preparedness and a range of physical and mental health quality of life outcomes.
Methods
Data collected from 14 states participating in a large state-based telephone survey were analyzed (n 5 104 654). Household disaster-preparedness items included having a 3-day supply of food, water, and prescription medications; a working battery-powered radio and flashlight; an evacuation plan; and a willingness to evacuate when instructed to do so. Quality-of-life items were categorized into 2 domains: physical health (general health, unhealthy physical days, and activity-limited days) and mental health (unhealthy mental days, social and emotional support, and life satisfaction).
Results
Persons with self-reported impaired mental health were generally less likely to report being prepared for a disaster than those who did not report impairment in each domain. Persons with low life satisfaction were among the least likely to be prepared, followed by those with inadequate social and emotional support, and then by those with frequent mental distress. Persons reporting physical impairments also reported deficits in many of the preparedness items. However, after adjusting for sociodemographic characteristics, some of the associations were attenuated and no longer significant
Conclusion
Persons reporting impaired quality of life are vulnerable to increased mental and physical distress during a disaster, and their vulnerability is compounded if they are ill-prepared. Therefore, persons reporting impaired quality of life should be included in the list of vulnerable populations that need disaster preparedness and response outreach.
Keywords: Quality of life, Public health preparedness, General health status, BRFSS
Natural and manmade disasters are an inevitable part of human existence. In fact, global trends have shown an increase in the incidence and severity of disasters in the past decade.1 Fortunately, many of the physical and mental effects of disasters can be mitigated by personal disaster preparedness.1 In spite of this, only 25% of US households currently adhere to the minimum American Red Cross, Federal Emergency Management Agency, and Department of Homeland Security preparedness guidelines (ie, an established disaster plan and at least a 3-day supply of food, water, and prescription medications for each member of a household).2 According to Citizen Corp, a national service program under the Department of Homeland Security, the largest barriers to preparedness are a perceived lack of importance and time.3
Research conducted thus far has focused on identifying obstacles to disaster preparedness. For example, social, economic, and demographic characteristics (eg, income, age, health status, community support, self-efficacy, knowledge, motivation, resources) influence the likelihood that an individual or their household has prepared for a disaster.1,4 Other studies have noted that medical vulnerabilities such as disabilities and chronic medical conditions correlate with disparities between those who prepare for disasters and those who do not.1,5 Notably, very few, if any, studies have examined factors that influence the desire to prepare for disasters. Such factors include quality of life, a broad, subjective, nonclinical, and multidimensional concept that usually includes self-reported measures of physical and mental health as well as physical and mental health perceptions and their correlates (eg, health risks and conditions, functional status, social support, socioeconomic status).6,7
Studies that have examined the association between quality of life and disaster preparedness have concentrated primarily on individual perception of general health. In a 2006-2008 Behavioral Risk Factor Surveillance System (BRFSS) study conducted by Bethel et al,5 persons with fair or poor general health as compared with persons reporting excellent, very good, and good health, were less likely to report all 4 preparedness items (food, water, radio, and flashlight). They were, however, more likely to report a 3-day supply of prescription medications.5 In a random digit-dial telephone survey of Los Angeles County residents conducted by Eisenman et al,8 people reporting fair or poor general health were less likely to report having disaster supplies and an emergency plan than their healthier counterparts. Finally, in a group of adults with rheumatoid arthritis in Japan, those with poorer perceived health were less likely than those with more favorable perceived health to carry medications and prescription and treatment records.9
It is notable that a variety of impaired physical and mental quality of life outcomes have been associated with detrimental behaviors of omission. In a study of older adults with hypertension in a managed care organization conducted by Holt et al,10 people with low mental or physical quality of life scores were less likely than those with higher scores to take prescribed antihypertensive medication. Moreover, persons reporting frequent mental distress and inadequate social and emotional support were 1.6 and 1.8 times less likely, respectively, than their counterparts to engage in physical activity.11,12 We hypothesized that many of these quality of life outcomes may also affect level of household preparedness.
METHODS
The BRFSS is a state-based surveillance system, operated by state health departments in collaboration with the Centers for Disease Control and Prevention. The objective of the BRFSS is to collect uniform, state-specific data on preventive health practices and risk behaviors that are linked to chronic diseases, injuries, and preventable infectious diseases in the adult population.13 Trained interviewers collect data from a standardized questionnaire on a monthly basis using an independent probability sample of households with landline telephones in the noninstitutionalized US adult population. The BRFSS questionnaire consists of 3 parts: (1) core questions asked in all 50 states, the District of Columbia (DC), Puerto Rico, Guam, and the US Virgin Islands; (2) supplemental modules, which are a series of questions on specific topics (eg, adult asthma history, intimate partner violence, mental health) that a state can choose to include in their survey; and (3) questions added by the states individually. All BRFSS questionnaires, data, and reports are available at http://www.cdc.gov/brfss/.
General Preparedness Module Questions
The general preparedness module was included in the BRFSS in select states from 2006 to 2010. Preparedness data were available for Connecticut, Montana, Nevada, and Tennessee in 2006; Delaware, Louisiana, Maryland, Nebraska, and New Hampshire in 2007; Georgia, Montana, Nebraska, New York, and Pennsylvania in 2008; Mississippi in 2009; and Montana and North Carolina in 2010. Overall household disaster preparedness, as defined by the BRFSS questionnaire, included the following 7 criteria: having a 3-day supply of food, water, and prescription medications, a working battery-powered radio and flashlight, an evacuation plan, and an expressed willingness to evacuate when instructed to do so (Figure 1).
FIGURE 1.
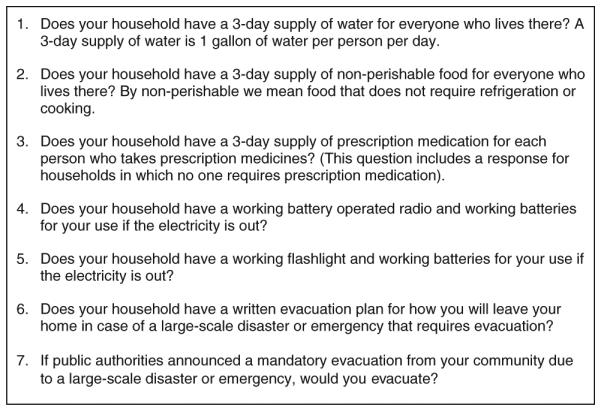
Selected Questions From the Behavioral Risk Factor Surveillance System (BRFSS) Disaster Preparedness Module
Quality of Life
The quality of life questions were available in the core questionnaire from 2006 to 2010. The health status section contained 1 question regarding general health: “Would you say that in general your health is excellent, very good, good, fair, or poor?” Responses were dichotomized into (1) excellent, very good, or good, versus (2) fair or poor.
Three questions constituted the Healthy Days—Health-Related Quality of Life section: physically unhealthy days, mentally unhealthy days, and activity limiting days. The physically unhealthy days question was assessed by asking the respondent, “Now thinking about your physical health, which includes physical illness and injury, for how many days during the past 30 days was your physical health not good?” Respondents reporting 14 or more days were identified as having frequent physical distress (FPD). The mentally unhealthy days question was assessed by asking the respondent, “Now thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good?” Respondents reporting 14 or more days were identified as having frequent mental distress (FMD). A similar question was asked for activity limitations: “During the past 30 days, for about how many days did poor physical or mental health keep you from doing your usual activities, such as self-care, work, or recreation?” Respondents reporting 14 or more days were identified as having frequent activity limitations (FAL).
The social and emotional support section contained 2 questions. Social and emotional support was assessed by asking respondents, “How often do you get the social and emotional support you need? (Always, Usually, Sometimes, Rarely, Never).” Reponses were dichotomized into (1) always or usually, versus (2) sometimes, rarely, or never. Finally, life satisfaction was assessed by asking respondents, “In general, how satisfied are you with your life? (Very satisfied, Satisfied, Dissatisfied, Very dissatisfied).” The responses were dichotomized into (1) very satisfied or satisfied, versus (2) dissatisfied or very dissatisfied.
For purposes of this study, quality of life items were categorized into a physical health domain and a mental health domain. The physical domain includes items assessing general health, physically unhealthy days, and activity-limited days. The mental domain includes items assessing unhealthy mental days, social and emotional support, and life satisfaction.
Statistical Analysis
We conducted a univariate analysis to explore the characteristics of the entire sample, including sociodemographics, preparedness, and quality of life. A bivariate analysis was used to explore the relationships between each of the sociodemographic variables and quality of life; a second bivariate analysis was then carried out to explore the relationship between quality of life and self-reported level of general household disaster preparedness. Significance was assessed using a χ2 test. Finally, the association between quality of life and household disaster preparedness was adjusted for a set of covariates using logistic regression.
Covariates included in the adjusted models were age in years (18-24, 25-34, 35-44, 45-54, ≥55), gender, race/ethnicity (white non-Hispanics, black non-Hispanics, Hispanics, other non-Hispanics), education (less than high school, high school graduate, greater than high school), marital status (currently married, previously married, never married), and employment status (currently employed, unemployed, retired, unable to work, homemaker/student). All analyses were weighted to reflect the complex survey design, resulting in weighted percentages, confidence intervals, and adjusted odds ratios. The unweighted and weighted sample size, response rate, and cooperation rate for each state in each year is reported in Table 1.
TABLE 1.
States Participating in the General Preparedness Module 2006-2010 by Year
| Year and State | Unweighted n | Weighted n | Response Ratea, % | Cooperation Rateb, % |
|---|---|---|---|---|
| 2006 | ||||
| Connecticutc | 4842 | 2 697 438 | 44.3 | 74.0 |
| Montana | 6059 | 727 026 | 54.8 | 72.5 |
| Nevada | 3591 | 1 825 459 | 50.1 | 80.2 |
| Tennessee | 4416 | 4 583 404 | 56.7 | 81.3 |
| 2007 | ||||
| Delaware | 3991 | 663 748 | 43.2 | 70.4 |
| Louisiana | 6684 | 3 249 264 | 41.0 | 60.1 |
| Maryland c | 4403 | 4 265 213 | 31.4 | 57.8 |
| Nebraskac | 5514 | 1 338 549 | 65.4 | 80.0 |
| New Hampshire | 5990 | 1 027 463 | 37.7 | 64.0 |
| 2008 | ||||
| Georgia | 5716 | 7 163 610 | 55.1 | 85.8 |
| Montana | 6846 | 738 769 | 48.3 | 69.4 |
| Nebraska c | 5373 | 13 333 476 | 65.5 | 80.2 |
| New York c | 3989 | 1 484 027 | 40.0 | 63.4 |
| Pennsylvania c | 6603 | 9 696 488 | 45.6 | 66.7 |
| 2009 | ||||
| Mississippi | 11 194 | 2 170 140 | 49.3 | 70.9 |
| 2010 | ||||
| Montana | 7304 | 760 685 | 65.4 | 80.6 |
| North Carolina | 12 139 | 7 174 410 | 41.1 | 64.5 |
The percentage of completed interviews of all eligible respondents.
The percentage of eligible respondents who were contacted and who completed the survey.
Split sample.
Significance was assessed using an alpha level of 0.05. All analyses were conducted using SAS callable SUDAAN (Research Triangle, release 9.2).
Data were available for 104 654 participants in the 14 states. For the purposes of this study, data were combined across all states and all years.
RESULTS
Respondent Characteristics
Approximately 21.4% (95% CI: 20.8%-22.0%) of respondents were aged 35 to 44 years, and 31.7% (95% CI: 31.2%-32.2%) were aged 55 years and older. Slightly more women than men responded to the survey (51.8%, 95% CI: 51.2%-52.5% vs 48.2%, 95% CI: 47.5%-48.8%). The majority of the respondents were white non-Hispanics (74.3%, 95% CI: 73.7%-75.0%), had a greater than high school education (60.6%, 95% CI: 60.0%-61.3%), were currently married %, 95% CI: 60.0%-61.3%), and were currently employed (61.1%, 95% CI: 60.4%-61.7%) (Table 2).
TABLE 2.
Characteristics of Respondents
| Characteristic | % (95% CI) |
|---|---|
| Demographic | |
| Sex | |
| Male | 48.2 (47.5-48.8) |
| Female | 51.8 (51.2-52.5) |
| Race | |
| White non-Hispanic | 74.3 (73.7-75.0) |
| Black non-Hispanic | 14.0 (13.5-14.4) |
| Hispanic | 6.5 (6.1-6.9) |
| Other non-Hispanica | 5.2 (4.9-5.5) |
| Age, y | |
| 18-24 | 9.9 (9.4-10.5) |
| 25-34 | 17.8 (17.2-18.4) |
| 35-44 | 21.4 (20.8-22.0) |
| 45-54 | 19.2 (18.8-19.7) |
| ≥55 | 31.7 (31.2-32.2) |
| Education | |
| Less than high school | 9.3 (8.9-9.7) |
| High school diploma | 30.1 (29.5-30.7) |
| Greater than high school | 60.6 (60.0-61.3) |
| Employment status | |
| Currently employed | 61.1 (60.4-61.7) |
| Unemployed | 5.8 (5.5-6.2) |
| Retired | 16.3 (15.9-16.6) |
| Unable to work | 5.6 (5.3-5.9) |
| Homemaker/student | 11.3 (10.9-11.8) |
| Marital status | |
| Currently married | 60.6 (60.0-61.3) |
| Previously marriedb | 17.7 (17.3-18.1) |
| Never marriedc | 21.7 (21.1-22.4) |
| Preparedness items | |
| 3-day supply of food | 82.9 (82.4-83.5) |
| 3-day supply of water | 53.6 (52.9-54.3) |
| 3-day supply of prescription medications | 89.7 (89.2-90.1) |
| Working radio and batteries | 77.7 (77.2-78.3) |
| Working flashlight and batteries | 94.8 (94.4-95.1) |
| Evacuation plan | 21.1 (20.6-21.7) |
| Leave if mandatory evacuation | 94.9 (94.6-95.2) |
| Quality of life | |
| Physical domain | |
| Frequent physical distress | 10.9 (10.5-11.3) |
| Fair or poor general health | 15.5 (15.1-16.0) |
| Frequent activity limitations | 6.9 (6.6-7.2) |
| Mental domain | |
| Frequent mental distress | 10.1 (9.7-10.6) |
| Dissatisfied or very dissatisfied with life | 5.4 (5.1-5.7) |
| Sometimes, rarely, or never receive social and emotional support |
20.1 (19.5-20.7) |
Asian, non-Hispanic; Native Hawaiian/Pacific Islander, non-Hispanic; American Indian/Alaska native, non-Hispanic; other race, non-Hispanic; multirace, non-Hispanic.
Previously married includes those divorced, widowed, or separated.
Never married includes those never married or member of unmarried couple.
An estimated 82.9% (95% CI: 82.4%-83.5%) of the respondents reported that they had a 3-day supply of food for each household member; 53.6% (95% CI: 52.9%-54.3%) had a 3-day supply of water for each household member; and 89.7% (95% CI: 89.2%-90.1%) had a 3-day supply of prescription medications for those in the household requiring them. More than three-quarters of respondents (77.7%, 95% CI: 77.2%-78.3%) reported having a working battery-operated radio; 94.8% (95% CI: 94.4%-95.1%) reported having a working battery-operated flashlight; 21.1% (95% CI: 20.6%-21.7%) reporting having a written evacuation plan; and 94.9% (94.6%-95.2%) reported that they would leave their community if public authorities issued a mandatory evacuation notice (Table 2).
One-quarter of all respondents (25.3%, 95% CI: 24.8%-25.9%) reported that their household was well-prepared to handle a large-scale disaster or emergency; 55.5% (95% CI: 54.9%-56.2%) felt somewhat prepared; and nearly one-fifth of those surveyed (19.1%, 95% CI: 18.6%-19.7%) did not feel that their household was at all prepared.
In the physical health domain, 10.9% (95% CI; 10.5%-11.3%) reported FPD; 15.5% (95% CI: 15.1%-16.0%) reported fair or poor general health; and 6.9% (95% CI: 6.6%-7.2%) reported FAL (Table 2). In the mental health domain, 10.1% (95% CI: 9.7%-10.6%) reported FMD; 5.4% (95% CI: 5.1%-5.7%) reported being dissatisfied or very dissatisfied with life; and 20.1% (95% CI: 19.5%-20.7%) reported sometimes, rarely, or never receiving social or emotional support. Sometimes, rarely, or never receive social and emotional support
Characteristics of Persons With Impaired Quality of Life
The prevalence of reported FPD, FAL, and fair/poor general health all increased with advancing age. The reported prevalence of FMD and life dissatisfaction was lowest for those 55 years and older, while the reported prevalence of inadequate social and emotional support was lowest for those in age groups 25 to 44 years and 55 years or older. Women were slightly more likely than men to report FMD, FPD, FAL, and fair/poor general health. Men, however, were more likely to report inadequate social and emotional support (Table 3). Race was significantly associated with reported FMD (P = 0.0040), fair/poor general health (P<0.0001), inadequate social and emotional support (P<0.0001), and dissatisfaction with life (P<0.0001). Black non-Hispanics were more likely to report FMD; white and other non-Hispanics were less likely to report fair/poor general health; and white non-Hispanics were less likely to report inadequate social and emotional support and dissatisfaction with life. The reported prevalence of FPD, FAL, and fair/poor general health increased as age increased.
TABLE 3.
Sociodemographic Characteristics of the Study Population by Impaired Quality of Life Status
| Physical domain |
Mental domain |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Demographic Characteristic |
Frequent Physical Distress |
Fair or Poor General Health |
Frequent Activity Limitations |
Frequent Mental Distress |
Dissatisfied or Very Dissatisfied With Life |
Sometimes, Rarely, or Never Has Social and Emotional Support |
||||||
| % (95% CI) | Sig | % (95% CI) | Sig | % (95% CI) | Sig | % (95% CI) | Sig | % (95% CI) | Sig | % (95% CI) | Sig | |
| Sex | ||||||||||||
| Male | 9.6 (9.1-10.2) | * | 14.5 (13.8-15.2) | * | 6.2 (5.7-6.7) | * | 8.2 (7.7-8.9) | * | 5.4 (4.9-6.0) | 21.1 (20.2-22.0) | * | |
| Female | 12.1 (11.6-12.6) | 16.5 (16.0-17.1) | 7.6 (7.3-8.0) | 11.9 (11.4-12.5) | 5.3 (5.0-5.7) | 19.2 (18.6-19.9) | ||||||
| Race | ||||||||||||
| White non-Hispanic | 10.9 (10.5-11.3) | 14.0 (13.5-14.4) | * | 6.7 (6.4-7.1) | 9.7 (9.3-10.2) | * | 4.7 (4.4-5.1) | * | 16.5 (15.9-17.0) | * | ||
| Black non-Hispanic | 10.8 (9.9-11.8) | 21.3 (19.9-22.7) | 7.6 (6.9-8.5) | 12.2 (11.0-13.5) | 7.8 (6.8-9.0) | 30.1 (28.4-31.9) | ||||||
| Hispanic | 9.8 (8.1-11.8) | 20.7 (18.3-23.3) | 6.1 (4.8-7.9) | 10.1 (8.3-12.2) | 6.3 (4.7-8.2) | 30.3 (27.2-33.6) | ||||||
| Other non-Hispanica | 12.2 (10.0-14.7) | 15.5 (13.5-17.7) | 8.6 (6.7-10.9) | 10.6 (8.8-12.6) | 7.3 (5.6-9.5) | 32.0 (28.8-35.4) | ||||||
| Age, y | ||||||||||||
| 18-24 | 4.3 (3.2-5.7) | * | 7.1 (5.8-8.7) | * | 3.3 (2.3-4.5) | * | 11.7 (10.0-13.7) | * | 5.4 (4.1-5.7) | * | 21.0 (18.5-23.7) | * |
| 25-34 | 6.0 (5.2-7.1) | 8.9 (7.8-10.1) | 4.2 (3.5-5.1) | 10.6 (9.5-211.8) | 5.3 (4.4-6.3) | 19.4 (17.8-21.0) | ||||||
| 35-44 | 8.0 (7.2-8.8) | 11.0 (10.0-11.9) | 5.3 (4.7-6.0) | 10.5 (9.6-11.4) | 5.6 (5.0-6.4) | 18.9 (17.7-20.2) | ||||||
| 45-54 | 12.3 (11.5-13.2) | 16.0 (15.1-17.0) | 8.3 (7.6-9.0) | 11.9 (11.1-12.7) | 6.6 (6.0-7.3) | 21.8 (20.7-22.9) | ||||||
| ≥55 | 16.9 (16.3-17.6) | 24.7 (24.0-25.4) | 9.9 (9.4-10.4) | 8.1 (7.7-8.6) | 4.5 (4.2-4.9) | 19.9 (19.3-20.6) | ||||||
| Education | ||||||||||||
| Less than high school | 24.0 (22.2-25.9) | * | 37.3 (35.3-39.3) | * | 16.3 (14.7-17.9) | * | 17.5 (15.9-19.2) | * | 9.5 (8.2-10.9) | * | 40.3 (38.1-42.5) | * |
| High school diploma | 13.1 (12.3-13.8) | 20.1 (19.2-21.0) | 8.4 (7.8-9.0) | 11.3 (10.6-12.1) | 6.3 (5.7-7.0) | 24.0 (23.0-25.1) | ||||||
| Greater than high school | 7.9 (7.5-8.3) | 10.0 (9.5-10.4) | 4.8 (4.5-5.2) | 8.5 (8.0-9.0) | 4.3 (4.0-4.7) | 15.2 (14.6-15.9) | ||||||
| Employment status | ||||||||||||
| Currently employed | 5.3 (4.9-5.7) | * | 8.20 (7.6-8.5) | * | 2.5 (2.2-2.8) | * | 8.0 (7.5-8.5) | * | 3.7 (3.4-4.1) | * | 17.7 (17.0-18.4) | * |
| Unemployed | 15.8 (13.8-18.1) | 22.4 (20.0-25.0) | 13.4 (11.6-15.4) | 20.2 (17.9-22.7) | 13.9 (12.0-16.2) | 31.1 (29.1-24.1) | ||||||
| Retired | 16.6 (15.8-17.5) | 26.0 (25.0-27.0) | 9.2 (8.5-9.9) | 6.2 (5.7-6.7) | 3.2 (2.9-3.7) | 19.9 (19.0-20.9) | ||||||
| Unable to work | 57.4 (54.8-59.9) | 68.7 (66.3-71.0) | 48.5 (45.9-51.0) | 36.5 (34.2-38.9) | 24.5 (22.4-26.8) | 42.3 (39.8-44.8) | ||||||
| Housewife/student | 8.6 (7.6-9.8) | 11.5 (10.4-12.7) | 4.7 (4.0-5.5) | 9.5 (8.4-10.8) | 3.8 (3.1-4.7) | 16.9 (15.4-18.6) | ||||||
| Marital status | ||||||||||||
| Currently married | 9.3 (8.9-9.8) | * | 12.9 (12.4-13.4) | * | 5.6 (5.3-6.0) | * | 7.9 (7.4-8.3) | * | 3.1 (2.8-3.5) | * | 15.3 (14.6-15.9) | * |
| Previously marriedb | 19.2 (18.3-20.1) | 27.9 (26.9-29.0) | 12.8 (12.0-13.6) | 15.1 (14.2-16.0) | 9.9 (9.2-10.7) | 29.6 (28.5-30.7) | ||||||
| Never marriedc | 8.6 (7.7-9.6) | 12.9 (11.9-14.1) | 5.9 (5.2-6.7) | 12.6 (11.5-13.8) | 8.0 (7.1-9.1) | 25.9 (24.3-27.5) | ||||||
Abbreviation: Sig, significance.
Asian, non-Hispanic; Native Hawaiian/Pacific Islander, non-Hispanic; American Indian/Alaska native, non-Hispanic; other race, non-Hispanic; multirace, non-Hispanic.
Previously married includes those divorced, widowed, or separated.
Never married includes those never married or member of unmarried couple.
Chi-square test, P<.05.
Persons with less than a high school education (vs a high school education or greater), those previously married (vs currently or never married), and those unable to work (vs working, retired, or a homemaker/student) were most likely to report impaired quality of life (FPD, FAL, FMD), fair/poor general health, inadequate social and emotional support, and life dissatisfaction.
Association Between Quality of Life and Level of Household Preparedness: Physical Health Domain
Frequent Physical Distress
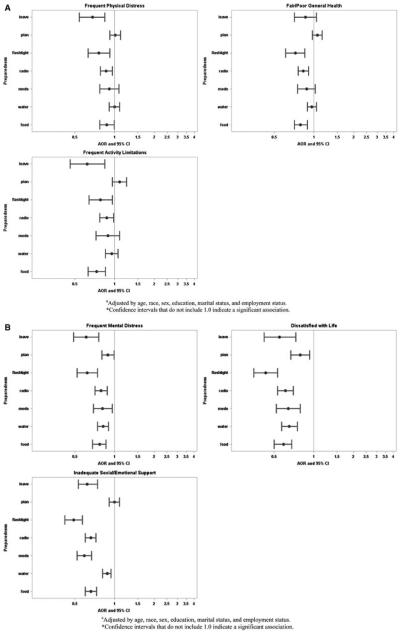
Persons with FPD were less likely to report having a radio or flashlight or to indicate a willingness to leave during a mandatory evacuation, but they were more likely to report having a 3-day supply of water and an evacuation plan than those without FPD, according to the unadjusted models (Table 4). The estimated differences in proportions between the groups for the significant preparedness items ranged from 2.9% (leave during mandatory evacuation) to 5.3% (working radio and batteries). After adjusting for other covariates, the odds of a person reporting FPD to report having a 3-day supply of food, a working battery-powered radio and flashlight, and a willingness to evacuate during a mandatory evacuation were significantly less than the odds of someone without FPD (Figure 2A).
TABLE 4.
Unadjusted Association Between Quality of Life and Preparedness Items
| Preparedness Variables in Physical Domain |
Physical Distress |
General Health |
Activity Limitations |
||||||
|---|---|---|---|---|---|---|---|---|---|
| No FPD | FPD | P | Excellent/ Very Good /Good |
Fair/ Poor | P | No FAL | FAL | P | |
| 3-day supply of food | 83.1 (82.5-83.7) | 81.6 (80.1-83.0) | .0679 | 83.4 (82.8-84.0) | 80.6 (79.3-81.9) | .0001 | 83.3 (82.7-83.9) | 78.4 (76.3-80.3) | ,.0001 |
| 3-day supply of water | 53.2 (52.4-53.9) | 56.4 (54.6-58.2) | .0015 | 53.1 (52.3-53.8) | 56.7 (55.1-58.2) | <.0001 | 53.5 (52.7-54.2) | 55.3 (52.9-57.6) | .1483 |
| 3-day supply of prescription medications | 89.6 (89.1-90.1) | 90.2 (89.0-91.3) | .3503 | 89.9 (89.3-90.4) | 88.9 (87.8-90.0) | .1291 | 89.7 (89.2-90.2) | 89.4 (87.7-90.9) | .7161 |
| Working radio and batteries | 78.4 (77.8-79.0) | 73.1 (71.4-74.7) | <.0001 | 78.8 (78.1-79.4) | 72.2 (70.8-73.6) | <.0001 | 78.2 (77.6-78.8) | 71.8 (70.0-73.8) | <.0001 |
| Working flashlight and batteries | 95.1 (94.8-95.5) | 92.1 (91.0-93.1) | <.0001 | 95.4 (95.0-95.7) | 91.6 (90.7-92.4) | <.0001 | 95.1 (94.7-95.4) | 91.4 (90.0-92.5) | <.0001 |
| Evacuation plan | 20.7 (20.2-21.3) | 24.2 (22.7-25.7) | <.0001 | 20.3 (19.8-20.9) | 25.5 (24.2-26.8) | <.0001 | 20.7 (20.2-21.3) | 25.8 (23.9-27.9) | <.0001 |
| Leave if mandatory evacuation | 95.2 (94.9-95.5) | 92.3 (91.1-93.4) | <.0001 | 95.1 (94.8-95.5) | 93.8 (92.9-94.5) | .0021 | 95.2 (94.8-95.5) | 91.6 (89.7-93.2) | .0001 |
|
Preparedness Variables in Mental
Health Domain |
Mental Distress
|
Life Satisfaction
|
Social and Emotional Support
|
||||||
| No FMD | FMD | P |
Very Satisfied
or Satisfied |
Dissatisfied or Very
Dissatisfied |
P |
Always or
Usually |
Sometimes, Rarely,
or Never |
P | |
| 3-day supply of food | 83.6 (83.0-84.1) | 77.7 (75.9-79.5) | <0.0001 | 83.6 (83.0-84.1) | 72.7 (69.9-75.3) | <0.0001 | 84.4 (83.8-85.0 | 77.0 (75.5-78.3) | <0.0001 |
| 3-day supply of water | 54.1 (53.4-54.8) | 49.2 (47.0-51.4) | <0.0001 | 54.1 (53.4-54.8) | 44.7 (41.7-47.7) | <0.0001 | 53.6 (52.8-54.3) | 53.1 (51.5-54.7) | 0.5968 |
| 3-day supply of prescription medications | 90.1 (89.5-90.6) | 86.3 (84.6-87.8) | <0.0001 | 90.1 (89.6-90.6) | 83.1 (80.3-85.5) | <0.0001 | 91.4 (90.9-91.9) | 83.1 (81.6-84.4) | <0.0001 |
| Working radio and batteries | 78.5 (77.9-79.2) | 71.4 (69.5-73.3) | <0.0001 | 78.5 (77.9-79.1) | 64.8 (61.9-67.6) | <0.0001 | 80.0 (79.3-80.6) | 69.2 (67.7-70.7) | <0.0001 |
| Working flashlight and batteries | 95.3 (94.9-95.6) | 90.4 (89.2-91.6) | <0.0001 | 95.3 (95.0-95.6) | 85.9 (83.7-87.9) | <0.0001 | 96.1 (95.8-96.4) | 89.4 (88.3-90.3) | <0.0001 |
| Evacuation plan | 21.1 (20.6-21.7) | 20.5 (18.9-22.1) | 0.4567 | 21.2 (20.7-21.7) | 20.1 (17.7-22.7) | 0.3898 | 20.6 (20.1-21.2) | 22.9 (21.7-24.3) | 0.0015 |
| Leave if mandatory evacuation | 95.2 (94.8-95.5) | 92.5 (91.2-93.6) | <0.0001 | 95.2 (94.9-95.5) | 90.8 (88.7-92.5) | <0.0001 | 95.6 (95.3-95.9) | 92.6 (91.6-93.5) | <0.0001 |
Abbreviations: FAL, frequent activity limitations; FMD, frequent mental distress; and FPD, frequent physical distress.
FIGURE 2.
Adjusteda Odds Ratios* of Respondents With Reported Impaired Quality of Life for Each Behavioral Risk Factor Surveillance System (BRFSS) Preparedness Item. A, Physical Health Domain; B, Mental Health Domain.
General Health
We found statistically significant unadjusted associations between reported general health and all general household disaster preparedness items, with the exception of having a 3-day supply of prescription medications (Table 4). Persons reporting fair or poor general health were significantly less likely than those reporting excellent, very good, or good general health to report having a 3-day supply of food and a working radio or flashlight, and were less likely to indicate a willingness to leave during an evacuation. However, they were more likely than persons reporting excellent, very good, or good general health to report having a 3-day supply of water and an evacuation plan. The range of the estimated significant differences between those reporting excellent, very good, or good general health (vs fair or poor general health) for reporting that they were prepared was 1.3% (leave during mandatory evacuation) to 6.6% (working radio and batteries). After adjusting for sociodemographic characteristics, the odds of having a 3-day supply of food and a working battery powered radio and flashlight for a person reporting fair or poor general health were significantly less than those for someone reporting excellent, very good, or good general health (Figure 2A).
Frequent Activity Limitations
Among those reporting FAL (vs not reporting FAL), we found significant unadjusted associations with all household disaster preparedness items except for having a 3-day supply of water and a 3-day supply of prescription medications. Estimated differences ranged from 3.6% (leave during mandatory evacuation) to 6.4% (working radio and batteries). Persons reporting FAL were more likely than those not reporting FAL to report having an evacuation plan (estimated difference 5.1%). After adjusting for sociodemographic characteristics, the odds of persons reporting FAL to report having a 3-day supply of food or a working battery-powered radio or flashlight were significantly less than for those not reporting FAL. The odds of reporting a willingness to leave during a mandatory evacuation was also significantly lower among those with FAL (Figure 2A).
Association Between Quality of Life and Level of Household Preparedness: Mental Health Domain
Frequent Mental Distress
Persons reporting FMD were significantly less likely than those reporting no FMD to report having a 3-day supply of food (P<0.0001), water (P<0.0001), or prescription medications (P<0.0001), and a working battery-powered radio (P<0.0001) or flashlight (P<0.0001), according to the unadjusted results (Table 4). Respondents reporting FMD were also less likely to report that they would leave the community in the event of a mandatory evacuation, as compared to those reporting no FMD (P<0.0001). The estimated differences in proportions between the groups for the significant preparedness items ranged from 2.7% (leave during a mandatory evacuation) to 7.1% (working radio and batteries). After adjusting for sociodemographic characteristics, the odds of reporting household disaster preparedness for all items among persons reporting FMD were significantly less than the odds for a person reporting no FMD (Figure 2B).
Life Satisfaction
Persons reporting that they were dissatisfied or very dissatisfied with life were significantly less likely than those who reported being satisfied or very satisfied with life to report all preparedness items except for having an evacuation plan (Table 4). When comparing across quality of life domains, in general, persons reporting that they were dissatisfied or very dissatisfied with life reported a lower percentage of general household preparedness compared to persons reporting all other impaired mental and physical health-related quality of life items. Moreover, the estimated difference in proportions between those who reported they were and were not satisfied with life was also greater for many of the preparedness items when comparing across the quality of life domains (range 4.4% for leaving during mandatory evacuation to 13.7% for having a working radio and batteries). The adjusted odds of someone who reported that they were dissatisfied or very dissatisfied with their life reporting each of the seven BRFSS general household disaster preparedness criteria were significantly less than the adjusted odds of someone who reported being very satisfied or satisfied with their lives reporting the same (Figure 2B).
Social and Emotional Support
Individuals reporting adequate social and emotional support were more likely to report having a 3-day supply of food, a 3-day supply of prescription medications, a working battery-powered radio, a working battery-powered flashlight, and an expressed willingness to evacuate when instructed to do so than those who reported inadequate social and emotional support (Table 4). The estimated differences in proportions ranged from 3.0% (leave during mandatory evacuation) to 10.8% (working radio and batteries), which was in many cases the second highest after life satisfaction. Conversely, persons reporting inadequate social and emotional support were more likely to report having an evacuation plan (estimated difference in proportion, 2.3%). After adjusting, all associations between reported social and emotional support and household preparedness except for having an evacuation plan remained significant (Figure 2B).
Association Between Quality of Life and Level of Household Preparedness: Summary
In the physical health domain, after adjusting for covariates, those reporting impaired physical health (whether measured as having FPD, poor general health, or FAL) were less likely to report having a battery-powered radio or flashlight or a 3-day supply of food. For 2 of the categories (FPD and FAL), respondents were also less likely to report being willing to leave their residence during a mandatory evacuation. No difference in preparedness was significant, with regards to reporting a 3-day supply of water, a 3-day supply of prescription medications, or an evacuation plan.
In the mental health domain, after adjusting for covariates, those reporting impaired mental health (whether captured as FMD, a dissatisfaction with life, or inadequate social or emotional support) were less likely to report having a 3-day supply of food, water, or medication, a battery-powered radio or flashlight, and a willingness to evacuate. Two groups (persons reporting FMD and persons reporting dissatisfaction with life) were also less likely to report having an evacuation plan.
DISCUSSION
To our knowledge, this is the first study to examine the association between a broad range of mental and physical quality of life items and disaster preparedness. Results of the study indicate that persons reporting mental health impairment tend to be the least likely to report being prepared for a major disaster. Among the mental and physical health-related quality of life domains, persons who reported being dissatisfied with life almost always had the lowest percentages for each preparedness item, followed by those reporting inadequate social and emotional support, and finally by those reporting FMD. Persons who reported impairments in the physical health-related quality of life domain also often had lower levels of household preparedness; however, after adjusting for sociodemographic characteristics, some of the associations were attenuated and no longer significant.
Regardless of whether the respondent reported impairment in the physical or mental health-related quality of life domains, those indicating a self-assessed impairment were generally less likely to have basic preparedness supplies such as a 3-day supply of food or a battery-powered radio or flashlight. Those reporting physical health impairment (as compared to those without physical health impairment), while often being more likely to have an evacuation plan, indicated that they would be less likely to leave their residence during a mandatory evacuation. This finding draws into question the feasibility of the evacuation plan, and may indicate a need to provide household-level notification and transportation in the event of a widespread disaster for this community. While it is encouraging that people reporting physical health impairments were not significantly different from those not reporting physical health impairments to have a 3-day supply of medication—given the increased reliance on medical services in this population and the potential for disruption in such services after a disaster—it is important to assure that the physically disabled population is more likely to have an adequate supply of prescription medication on hand. In general, those reporting mental health impairments were less likely to be prepared than those who did not report mental health impairments across almost all of the preparedness items. This finding may indicate a lack of desire to plan ahead and more of a focus on getting through daily responsibilities, suggesting the potential need for the availability of basic household preparedness supplies for communities with increased levels of mental impairment.
Research indicates that disasters can have an impact on quality of life by increasing emotional and physical problems and the risk of dysfunctional behavioral response.14-16 Given that people reporting FMD, FPD, FAL, fair or/poor general health, lack of social and emotional support, and dissatisfaction with life already experience impaired quality of life, they are a particularly vulnerable population. While emergency planning and response efforts have consistently focused on physical well-being,17 only recent attention has been given to incorporating mental illness into disaster preparedness and response.14,15,17,18 The need for inclusion of mental health in these efforts is evidenced in this report by the difference in preparedness between those who did and did not report impairments in the mental health quality of life domain.
Limitations
This study has several limitations. First, the BRFSS data are derived by sampling households with a landline telephone, Disaster Medicine and Public Health Preparedness thus excluding households with only cell phones. Second, only respondents who were physically and mentally capable of completing the survey were included; therefore, the actual association between impaired quality of life, social and emotional support, life satisfaction, and general preparedness may be attenuated in this study, as we may be missing from the study sample the subjects with the lowest levels of quality of life and preparedness. Third, the survey was limited to the questions contained in the BRFSS that addressed physical and mental health impairment. These questions may not capture the complexity of the physical or mental health impairment and may preclude the use of the results to suggest specific planning mechanisms. Fourth, it is possible that the associations reported between the quality of life, general health, social and emotional support, and life satisfaction indicators and preparedness are further diminished by assessing preparedness using items commonly found in the household (ie, these common items may not be indicative of disaster preparedness). Finally, the general preparedness module was only used in a total of 14 states between 2006 and 2010, with a few states using the module in any given year; therefore, the findings are not generalizable to the US population.
CONCLUSIONS
The findings in this report offer an important contribution to the study of potentially vulnerable populations as they relate to disasters and preparedness. Previous studies have shown that individuals with physical and mental limitations have increased vulnerability during a disaster.18,19 This study indicates that perception of one’s physical and mental health is also associated with vulnerability. As several researchers have suggested, public health entities should partner with community organizations and service providers to improve preparedness among individuals with physical and mental limitations.5,8 While this task appears daunting due to the heterogeneity of the population, we believe that persons with impaired quality of life should also be included in the list of vulnerable populations that need disaster preparedness and response outreach, particularly those with perceived impaired mental health.
Footnotes
Disclaimer
The findings and conclusions in this article are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Levac J, Toal-Sullivan D, O’Sullivan TL. Household emergency preparedness: a literature review. J Community Health. 2012;37(3):725–733. doi: 10.1007/s10900-011-9488-x. [DOI] [PubMed] [Google Scholar]
- 2.Clements BW. Disasters and Public Health: Planning and Response. 1st Butterworth-Heinenmann; Burlington, MA: 2009. [Google Scholar]
- 3.US Department of Homeland Security . Community Resilience Through Civic Responsibility and Self-Reliance. US Department of Homeland Security; Washington, DC: 2005. Citizens Corps Citizen Preparedness Review: Methodological Considerations and Key Findings in Preparedness Research. Issue 1. Summer. http://www.citizencorps.gov/downloads/pdf/ready/citizen_prep_review_ issue_1.pdf. Accessed June 22, 2012. [Google Scholar]
- 4.Ablah E, Konda J, Kelley CL. Factors predicting individual emergency preparedness: a multi-state analysis of 2006 BRFSS data. Biosecur Bioterror. 2009;7:317–330. doi: 10.1089/bsp.2009.0022. [DOI] [PubMed] [Google Scholar]
- 5.Bethel JW, Foreman AN, Burke SC. Disaster preparedness among medically vulnerable populations. Am J Prev Med. 2011;40(2):139–143. doi: 10.1016/j.amepre.2010.10.020. [DOI] [PubMed] [Google Scholar]
- 6.The World Health Organization Quality of Life Group The World Health Organization Quality of Life Assessment (WHOQOL). Development and psychometric properties. Soc Sci Med. 1998;46:1569–1585. doi: 10.1016/s0277-9536(98)00009-4. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention . Quality of life concepts. Centers for Disease Control and Prevention; Atlanta, GA: Mar 17, 2011. http://www.cdc.gov/hrqol/concept.htm. [Google Scholar]
- 8.Eisenman DP, Zhou Q, Ong M, et al. Variations in disaster preparedness by mental health, perceived general health, and disability status. Disaster Med Public Health Prep. 2009;3(1):33–41. doi: 10.1097/DMP.0b013e318193be89. [DOI] [PubMed] [Google Scholar]
- 9.Tomio J, Sato H, Muzumura H. Disparities in disaster preparedness among rheumatoid arthritis patients with various general health, functional, and disability conditions. Environ Health Prev Med. 2012;17(4):322–331. doi: 10.1007/s12199-011-0257-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holt EW, Muntner P, Joyce CJ, et al. Health-related quality of life and antihypertensive medication adherence among older adults. Age Ageing. 2010;39(4):481–487. doi: 10.1093/ageing/afq040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Strine TW, Balluz L, Chapman DP, et al. Risk behaviors and health care coverage among adults by frequent mental distress status, 2001. Am J Prev Med. 2004;26(3):213–216. doi: 10.1016/j.amepre.2003.11.002. [DOI] [PubMed] [Google Scholar]
- 12.Strine TW, Chapman DP, Balluz L, et al. Health-related quality of life and health behaviors by social and emotional support. Soc Psychiatry Psychiatr Epidemiol. 2008;43:151–159. doi: 10.1007/s00127-007-0277-x. [DOI] [PubMed] [Google Scholar]
- 13.Mokdad AH, Stroup DF, Giles WH. Behavioral Risk Factor Surveillance Team. Public health surveillance for behavioral risk factors in a changing environment: recommendations from the Behavioral Risk Factor Surveillance System. MMWR Recomm Rep. 2003;52(RR-9):1–12. [PubMed] [Google Scholar]
- 14.Pfefferbaum B, Flynn BW, Schonfeld D, et al. The integration of mental and behavioral health in disaster preparedness, response, and recovery. Disaster Med Public Health Prep. 2012;6(1):60–66. doi: 10.1001/dmp.2012.1. [DOI] [PubMed] [Google Scholar]
- 15.Pfefferbaum B, Schonfeld D, Flynn BW, et al. The H1N1 crisis: a case study of the integration of mental and behavioral health in public health crises. Disaster Med Public Health Prep. 2012;6:67–71. doi: 10.1001/dmp.2012.2. [DOI] [PubMed] [Google Scholar]
- 16.Van den Berg B, van der Velden PG, Yzermans J, et al. Health-related quality of life and mental health problems after a disaster: are chronically ill survivors more vulnerable to health problems? Qual Life Res. 2006;15:1571–1576. doi: 10.1007/s11136-006-0033-9. [DOI] [PubMed] [Google Scholar]
- 17.Wissow LS, Rutkow L, Kass NE, et al. Ethical issues raised in addressing the needs of people with serious mental disorders in complex emergencies. Disaster Med Public Health Prep. 2012;6:72–78. doi: 10.1001/dmp.2011.88. [DOI] [PubMed] [Google Scholar]
- 18.Compton MT, Kotwicki RJ, Kaslow NJ, et al. Incorporating mental health into bioterrorism response planning. Public Health Rep. 2005;120(suppl 1):16–19. doi: 10.1177/00333549051200S105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miller AC, Arquilla B. Chronic diseases and natural hazards: impact of disasters on diabetic, renal, and cardiac patients. Prehosp Disaster Med. 2008;23(2):185–194. doi: 10.1017/s1049023x00005835. [DOI] [PubMed] [Google Scholar]