In 2000, members of the Brain Attack Coalition published recommendations for the establishment of primary stroke centers (PSCs),1 and in 2005 they published recommendations for the establishment of comprehensive stroke centers (CSCs).2 To improve patient care and outcomes for stroke, the recommendations suggested that stroke centers should include acute stroke teams, written care protocols, emergency medical services integrated with the stroke center, rapid testing procedures, and continuous improvement processes. Since then, several certification programs have been developed to identify hospitals that have established a stroke center that meets specific criteria for the treatment of stroke.
The Joint Commission, DNV GL, and Healthcare Facilities Accreditation Program offer certification programs for PSCs and CSCs. PSC certification was designed to meet the Brain Attack Coalition’s recommendations for improved stroke care through access to dedicated, specialized personnel and procedures. CSCs must meet all of the requirements for certification as a PSC, plus additional requirements meant to help manage complex stroke cases. These include the requirements to meet specified volumes of patients and procedures, be capable of providing advanced imaging on-site at all times, provide after hospital care coordination for patients, have dedicated neurological intensive care unit beds for complex stroke cases, participate in stroke research, and collect standard performance measures.3
Several studies have analyzed the effectiveness of stroke centers in the care and management of patients with stroke. In New York state, patients with ischemic stroke admitted to a designated stroke center experienced a lower 30-day all-cause mortality rate and greater use of thrombolytic therapy.4 Also, among Medicare beneficiaries aged ≥65 years, hemorrhagic stroke patients treated at Joint Commission certified PSCs had lower 30-day mortality rates.5 PSCs and CSCs have shown improvements in stroke performance measures, the collection of which is required to maintain certification.3
The maps displayed here show the locations of Primary and Comprehensive Stroke Centers certified by The Joint Commission, DNV GL, and Healthcare Facilities Accreditation Program as of May 2015 overlaid on stroke hospitalization rates and discharge status by county among Medicare fee-for-service beneficiaries aged ≥65 in the United States (2010–2012). Rates are age standardized and spatially smoothed to enhance the stability of rates in counties with small populations. Counties with the highest stroke hospitalization rates (13.5–24.1 per 1000 total beneficiaries) were located primarily in the Southeast for both total beneficiaries and black beneficiaries (Figure 1). CSCs (n=113) are located in 32 states and the District of Columbia. Most are located in urban areas, and more than two thirds are located east of the Mississippi River. Concentrations of certified PSCs (n=1197) are located along the East and West coasts, Texas and near Chicago and Atlanta (Figure 2). The percentage of stroke hospitalizations in which Medicare beneficiaries died before discharge from the hospital was highest in counties in the Northeast and West. Many counties with high stroke hospitalization rates or high percentages of Medicare beneficiaries who died before discharge from the hospital do not have a stroke center located nearby.
Figure 1.
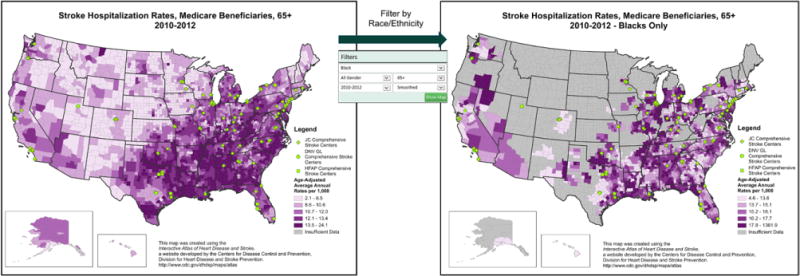
Comprehensive Stroke Centers 2015, with stroke hospitalization rates among Medicare beneficiaries and stroke hospitalization rates among black medicare beneficiaries only, 2010 to 2012.
Figure 2.
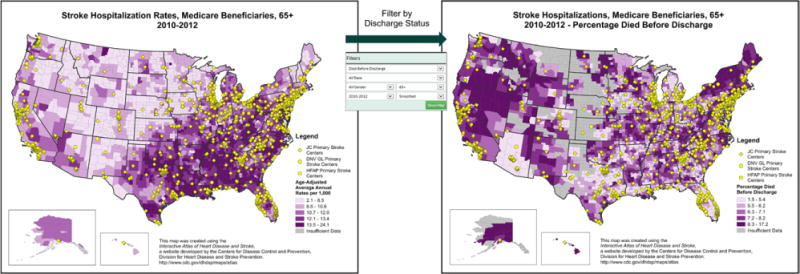
Primary Stroke Centers 2015, with stroke hospitalization rates among Medicare beneficiaries and percentage of stroke hospitalizations in which medicare beneficiaries died before discharge from the hospital, 2010 to 2012.
These maps were created using the Interactive Atlas of Heart Disease and Stroke—a web-based tool created by the Division for Heart Disease and Stroke Prevention within the Centers for Disease Control and Prevention and are the first ever to show stroke centers certified by all 3 organizations. The Atlas enables users to easily create and share county-level maps that display heart disease and stroke data by sex, race/ethnicity, and age group. Users can also create maps depicting an array of county-level social and economic data, including poverty, education, and urban/rural status. In addition, users can overlay locations of a variety of healthcare facilities and congressional boundaries on maps they create, view two maps at a time to compare indicators, and generate a report for a county or group of counties. The Interactive Atlas of Heart Disease and Stroke is a valuable tool for public health professionals, healthcare providers, researchers, community leaders, and others interested in monitoring trends, generating hypotheses, setting research priorities, and planning patient services. http://www.cdc.gov/dhdsp/maps/atlas
Footnotes
Disclosures
None.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.Alberts MJ, Hademenos G, Latchaw RE, Jagoda A, Marler JR, Mayberg MR, Starke RD, Todd HW, Viste KM, Girgus M, Shephard T, Emr M, Shwayder P, Walker MD. Recommendations for the establishment of primary stroke centers. Brain Attack Coalition. JAMA. 2000;283:3102–3109. doi: 10.1001/jama.283.23.3102. [DOI] [PubMed] [Google Scholar]
- 2.Alberts MJ, Latchaw RE, Selman WR, Shephard T, Hadley MN, Brass LM, Koroshetz W, Marler JR, Booss J, Zorowitz RD, Croft JB, Magnis E, Mulligan D, Jagoda A, O’Connor R, Cawley CM, Connors JJ, Rose-DeRenzy JA, Emr M, Warren M, Walker MD, Brain Attack Coalition Recommendations for comprehensive stroke centers: a consensus statement from the Brain Attack Coalition. Stroke. 2005;36:1597–1616. doi: 10.1161/01.STR.0000170622.07210.b4. [DOI] [PubMed] [Google Scholar]
- 3.Gorelick PB. Primary and comprehensive stroke centers: history, value and certification criteria. J Stroke. 2013;15:78–89. doi: 10.5853/jos.2013.15.2.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xian Y, Holloway RG, Chan PS, Noyes K, Shah MN, Ting HH, Chappel AR, Peterson ED, Friedman B. Association between stroke center hospitalization for acute ischemic stroke and mortality. JAMA. 2011;305:373–380. doi: 10.1001/jama.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lichtman JH, Jones SB, Leifheit-Limson EC, Wang Y, Goldstein LB. 30-day mortality and readmission after hemorrhagic stroke among Medicare beneficiaries in Joint Commission primary stroke center-certified and noncertified hospitals. Stroke. 2011;42:3387–3391. doi: 10.1161/STROKEAHA.111.622613. [DOI] [PMC free article] [PubMed] [Google Scholar]


