Abstract
Purpose
Because the occurrence of post-operative myocardial ischemia predicts subsequent cardiac morbidity and mortality, we determined the prevalence of and risk factors for myocardial ischemia in hip and knee arthroplasty patients.
Methods
High sensitivity cardiac troponin T (hs-cTnT) was measured on stored samples from post-operative day 2 in 394 hip and knee arthroplasty patients ≥ 65 years of age enrolled in the Genetics-InFormatics Trial (GIFT).
Results
Fifty-three (13.5%) participants had myocardial ischemia, of whom only three were diagnosed clinically during their hospitalization. The risk of myocardial ischemia increased with age (OR 3.52 per decade, 95% CI 2.00-6.19) and diabetes (OR 2.23, 95% CI 1.04-4.77). Myocardial ischemia was rarer with statins (OR 0.74, 95% CI 0.40-1.35) and more common with hypertension, coronary artery disease and tobacco use, although these were not statistically significant.
Conclusions
Subclinical myocardial ischemia occurs frequently after arthroplasty. Diabetic and elderly patients are at highest risk.
Keywords: Postoperative complication, myocardial ischemia, arthroplasty, risk factor, statin, troponin
INTRODUCTION
With the aging of the American population and the increased prevalence of obesity, over 1 million Americans undergo hip or knee arthroplasty each year for osteoarthritis [1]. Based on the National Hospital Discharge database, 1.1% of arthroplasty patients are diagnosed with cardiac complications in the 90 days after surgery [2]. However, most orthopedic surgery patients with myocardial ischemia do not complain of angina. For example, in a study of 200 hip fracture participants, 71 (35%) had an elevated troponin level but only 8% of them complained of chest pain [3]. Therefore the overall incidence of post-operative myocardial ischemia in orthopedic patients is likely much higher than 1.1%.
Understanding the true incidence and risk factors for post-operative myocardial ischemia in orthopedic patients is important for several reasons. First, the occurrence of even asymptomatic post-operative myocardial ischemia predicts subsequent cardiac morbidity and mortality [4-10]. Second, understanding the risk of postoperative myocardial ischemia can help patients make an informed decision about undergoing arthroplasty. Third, identifying patients at elevated cardiac risk can spur preemptive actions, such as giving cardioprotective medications peri-operatively to those that need them. For example, peri-operative beta-adrenergic receptor blockers decrease the risk of post-operative ischemia, although they increase the risk of postoperative ischemic stroke [11]. Likewise, peri-operative aspirin therapy may decrease the risk of post-operative myocardial infarction, cardiac arrest, severe arrhythmia, pulmonary embolism and cardiovascular death, but can cause major bleeding [12-14]. Three(3)-hydroxy-3-methylglutaryl coenzyme-A reductase inhibitors (“statins”) reduce the rate of myocardial infarction by 43%-53% after some non-cardiac surgeries, even when started only 1-30 days before surgery [15-17] but their benefit in orthopedic surgery patients is unknown.
This study was performed in order to quantify the incidence of and risk factors for post-operative myocardial ischemia in orthopedic patients. We conducted a cohort study nested within a multicenter trial of pharmacogenetic vs. clinical dosing of warfarin therapy in individuals undergoing elective hip or knee arthroplasty. We used a fourth generation high sensitivity cardiac troponin T (hs-cTnT) assay to detect post-operative myocardial ischemia.
MATERIALS & METHODS
Participants were recruited as an ancillary study to the Genetics InFormatics Trial (GIFT) of Warfarin Therapy to Prevent DVT. (NHLBI R01 HL097036). As previously described [18], GIFT is an ongoing multi-center randomized trial that utilizes web-based warfarin-dosing algorithms (www.WarfarinDosing.org) in individuals ≥ 65 years of age undergoing hip or knee arthroplasty.
Plasma samples were obtained from consenting GIFT study patients on postoperative day 2, frozen and stored. Batch testing for hs-cTnT was performed at a later date on deidentified samples. Measurement of hs-cTnT was accomplished in the General Core Laboratory of the Weill Cornell Medical College Clinical and Translational Science Center using a quantitative sandwich enzyme immunoassay kit from Meso Scale Discovery (MSD), Catalog Number K151EFC-1 (Gaithersburg, MD, USA), and processed on the MULTI-ARRAY Human Cardiac Troponin T MSD assay using the manufacturer’s instructions. The assay had a lower level of detection of 13 ng/L and a coefficient of variation of 7%. This assay has 100% cross-reactivity with Troponin. In this study, myocardial ischemia was defined as an hs-cTnT level ≥ 14ng/L, the published 99th percentile cutoff for this assay [9].
Deidentified patient demographics and medical history were obtained from the GIFT study database. Demographics were analyzed descriptively.
Statistical analysis
Logistic regression was performed to determine which factors were associated with higher risk myocardial ischemia. We offered the following variables in the backwards stepwise regression model: age, total hip vs. knee arthroplasty, bilateral vs. unilateral total knee arthroplasty, body mass index, coronary artery disease, creatinine clearance, diabetes, hypertension, race, sex, smoker status, use of a statin, and history of stroke. A p-value of 0.5 was used to retain variables in the model, and a two-sided p-value ≤ 0.05 was required to determine statistical significance.
To further quantify the odds ratio of myocardial ischemia in participants prescribed a statin, we used an inverse probability treatment of weighting propensity score (IPTW). The IPTW used the following covariates: age, sex, race, diabetes, coronary artery disease, smoker status, blood pressure, and bilateral arthroplasty (see appendix). A propensity score is the conditional probability of treatment assignment given the observed baseline characteristics. Propensity score conditioning results in unbiased estimates of the average treatment effect [19]. The Shapiro-Wilk test and normal probability plots were utilized to confirm normality. Chi-square goodness-of-fit test was utilized to compare unadjusted and IPTW-adjusted baseline characteristics. Hosmer and Lemeshow goodness-of-fit test determined model fit. The IPTW resulted in a c-statistic of 0.66.
Statistical data were calculated with SAS, version 9.2 (SAS Institute Inc., Cary, NC).
This study was performed in accordance with ethical standards and was approved by the local Institutional Review Board.
Results
Post-operative day 2 (POD2) plasma samples were available for hs-cTnT measurement from 394 hip or knee arthroplasty patients. Two hundred ninety-nine (76%) of these individuals underwent total knee arthroplasty, including 40 (10%) that underwent bilateral knee arthroplasty. The average (standard deviation) age of the patients was 71.8 (6.2) years (Table I).
Table I.
Patient characteristics
| Group Data | |||
|---|---|---|---|
| Characteristic | Total (N=394) |
TKA (N=299) |
THA (N=95) |
| Age - yr (mean ± sd) | 71.8 ± 6.16 | 71.8 ± 6.47 | 71.8 ± 5.19 |
| CAD (%) | 8.7 | 8.1 | 9.7 |
| DM (%) | 15.0 | 15.3 | 13.8 |
| HTN (%) | 16.3 | 15.3 | 18.3 |
| Male Sex (%) | 34.5 | 32.5 | 42.6 |
| Smoker (%) | 3.8 | 2.4 | 8.5 |
| African American (%) | 5.3 | 4.8 | 7.5 |
| Bilateral (%) | 10.2 | 13.2 | 1.1 |
TKA = total knee arthroplasty; THA=total hip arthroplasty; CAD = coronary artery disease; DM = diabetes; HTN = hypertension.
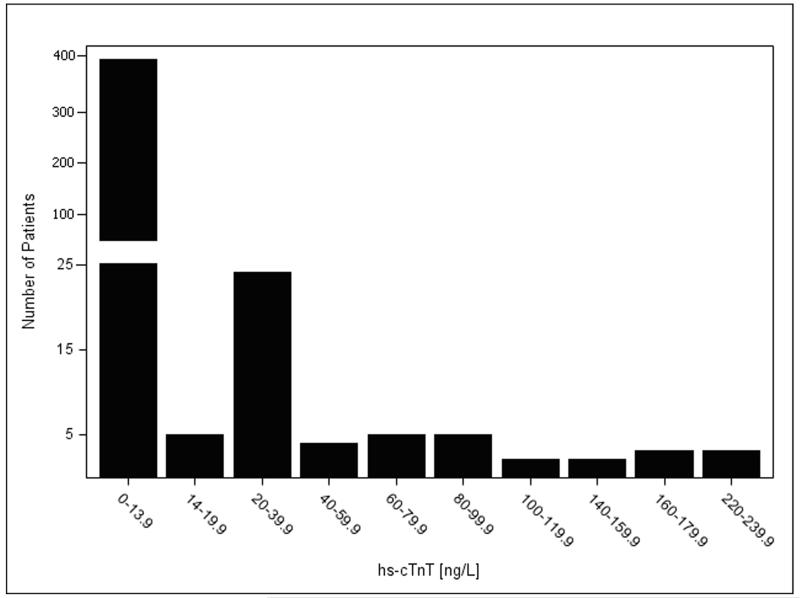
Fifty-three patients (13.5%) had myocardial ischemia postoperatively (hs-cTnT ≥ 14 ng/L) (Figure 1). The proportion of patients with myocardial ischemia did not differ by site. Only three participants (0.77%) were identified clinically as having myocardial ischemia during their hospital stay. These participants had POD2 hs-cTnT levels of 32.7, 34.1, and 35.6 respectively. The risk of myocardial ischemia increased with age (odds ratio (OR) 3.52 per decade, 95% confidence interval (CI) 2.00-6.19) and diabetes (OR 2.23, 95% CI 1.04-4.77). Myocardial ischemia was less common with a statin (OR 0.74, 95% CI 0.40-1.35) and more common with hypertension, coronary artery disease, and tobacco use, although these were not statistically significant.
Figure 1.
After using a propensity score to adjust for the likelihood of being on a statin and performing non-parsimonious stepwise regression, only age and diabetes mellitus were significant predictors of postoperative myocardial ischemia: the odds increased 3.5-fold per decade of life, and 2.2-fold in participants with diabetes mellitus (Table II). Although not statistically significant, the odds of myocardial ischemia were lower in participants on statin therapy and higher in participants with hypertension and coronary artery disease, smokers, and those undergoing bilateral knee arthroplasty (Table II).
Table II.
Risk Factors for Myocardial Ischemia after multivariate analysis with IPTW for statin use
| Risk Factor | OR (95% CI) | P value |
|---|---|---|
| Statin | 0.74 (0.40-1.35) | 0.326 |
| Age Per Decade | 3.52 (2.00-6.19) | < .0001 |
| Diabetes | 2.23 (1.04-4.77) | 0.038 |
| Hypertension | 1.78 (0.83-3.83) | 0.140 |
| CAD | 2.15 (0.84-5.46) | 0.109 |
| Smoker | 2.27 (0.51-10.07) | 0.280 |
| Bilateral TKA | 1.52 (0.55-4.21) | 0.420 |
| Male Sex | 1.19 (0.62-2.28) | 0.604 |
| Race1 | 1.32 (0.38-4.56) | 0.663 |
IPTW = inverse probability treatment of weighting propensity score; CAD = Coronary Artery Disease; TKA = Total Knee Arthroplasty.
Discussion
Over 1 million Americans undergo hip or knee arthroplasty each year [1], and 1%-2% are reported to experience arterial thrombotic complications such as acute stroke, MI or vascular death [2, 20-22]. Using a high sensitivity assay to measure cardiac troponin T (hs-cTnT), we found evidence of myocardial ischemia in 13.5% of patients after hip and knee arthroplasty. Of note, only 0.77% of patients were diagnosed clinically with myocardial ischemia (on the basis of symptoms and troponin measurement) during their hospital stay. The frequency of clinically apparent myocardial ischemia noted in our study was similar to the published 0.2-0.7% rate of post-arthroplasty myocardial infarction derived from administrative data [22-25]. The clinical detection of myocardial ischemia in the post-operative setting is difficult, because patients and clinicians are focused on musculoskeletal pain, and opiates used for orthopedic pain can mask angina. We found that many patients with undetected ischemia are discharged without potentially beneficial therapies such as beta antagonists, aspirin, ACE inhibitors, and/or statins.
Fourth generation hs-cTnT assays are highly specific for myocardial ischemia [26]. Although elevated levels can be seen in critically ill patients [9, 27], patients in this study were clinically well. Fourth generation hs-cTnT assays have greater sensitivity to detect myocardial ischemia than traditional assays [26, 28, 29]. In VISION, for example, a study of 15,133 patients over age 45 undergoing non-cardiac surgery, 11.6% of patients were found to have myocardial ischemia postoperatively. Even low levels of ischemia were clinically important in VISION: post-operative hs-cTnT values as low as 20 ng/L or 30 ng/L predicted 30-day mortality [10]. Nagele et al. also found that perioperative hs-cTnT elevations presaged mortality [9]. Hietala et al. demonstrated that perioperative troponin elevation in hip fracture patients was associated with both higher short-term (17% vs 4.7%, p=0.008) and long-term (61% vs 40%, p=0.005) mortality [30]. There were no deaths in our study, but this was most likely due to the small number of patients analyzed (n = 394).
The risk of myocardial ischemia in our study was higher with advancing age and in patients with diabetes, suggesting that these patients may benefit from cardiac monitoring and troponin testing post-operatively. Ischemia also tended to be more common among patients who had other risk factors for MI (hypertension, CAD, smoking, bilateral TKA, male sex, and African-American race).
Our finding that diabetes is a significant risk factor for silent ischemia confirms prior studies. For example, in a study of 579 individuals undergoing sestamibi stress tests, there was a higher incidence of silent ischemia among diabetic patients [31]. Similarly, in a study of nearly 2000 patients without a history of known myocardial infarction (MI) diagnosis, diabetes was an independent predictor of silent MI (OR 1.5, 95% CI 1.1-1.9, p=0.004) [32].
Our finding that silent ischemia is more common in the elderly also is supported by the literature. For example, in a population-based cohort study of 5888 participants ≥ 65 years of age without history of a MI diagnosis, 15.3% of participants had evidence of a MI by baseline ECG studies, 22.3% of which had been unrecognized [33]. Prior studies in orthopedic patients have also demonstrated an association between advanced age and myocardial ischemia. In a study of patients undergoing hip fracture surgery, 44.4% of those ≥ 90 years of age experienced troponin elevations compared with 12.5% of participants < 70 years of age (p<0.01) [3].
Our study was limited by insufficient sample size to quantify the effects of statin use on myocardial ischemia. In addition, because ECG testing was not routinely performed we do not know whether patients with elevated hs-cTnT levels had accompanying ECG changes. High sensitivity-cTnT levels were only available from POD2 plasma samples. Although troponin is known to be elevated for seven to ten days, we could not record hs-cTnT levels serially as many patients were discharged within the first three days and we also lacked funding. We also lacked baseline hs-cTnT levels which have also been shown to predict adverse outcomes [9]. These limitations are balanced by strengths, including complete follow-up for all 394 participants and standardized warfarin management (based on the GIFT study protocol).
In contemporary studies, postoperative myocardial infarction occurs at rates similar to those of pulmonary embolism following hip and knee arthroplasty [2, 23-25, 34, 35]. The results of our study suggest that patients at high risk for ischemia, such as diabetics and the elderly, may benefit from postoperative troponin testing. Safe new approaches to cardio-protection are also needed. Given that statin therapy has been shown to reduce the risk of adverse cardiovascular outcomes after a variety of high-risk surgeries [15-17, 36], we propose a randomized trial of statins vs. placebo in patients aged ≥ 65 years undergoing orthopedic surgery.
Acknowledgements
Funding for high sensitivity troponin T testing was provided by the Weill Cornell Clinical & Translational Science Center (UL1 TR000457-06). The Genetics InFormatics Trial (GIFT) of Warfarin Therapy to Prevent DVT is funded by the National Heart Lung Blood Institute (R01 HL097036).
Appendix
Table III. Patient characteristics before and after applying IPTW propensity score.
| Unadjusted Data | Data Adjusted with the Use of Inverse Probability Weighting |
|||||
|---|---|---|---|---|---|---|
| Characteristic | No Statin (N=339) |
Statin (N=53) |
P value | No Statin (N=339) |
Statin (N=53) |
P value |
| Age (yr) | 71.5 ± 7.3 | 72.1 ± 4.8 | 0.286 | 71.9 ± 6.8 | 71.9 ± 4.8 | 0.966 |
| Bilateral TKA (%) | 9.1 | 11.2 | 0.483 | 9.6 | 10.2 | 0.863 |
| CAD (%) | 4.0 | 13.3 | 0.001 | 8.7 | 8.7 | 0.983 |
| DM (%) | 10.1 | 19.9 | 0.006 | 15.0 | 14.9 | 0.988 |
| HTN (%) | 15.2 | 17.5 | 0.525 | 17.4 | 16.8 | 0.871 |
| Male Sex (%) | 25.8 | 43.4 | 0.0002 | 34.4 | 34.2 | 0.967 |
| Smoker (%) | 4.0 | 3.6 | 0.808 | 3.4 | 3.4 | 0.993 |
| Is Black (%) | 6.1 | 4.6 | 0.516 | 5.8 | 5.7 | 0.966 |
IPTW = Inverse probability treatment of weighting; TKA = total knee arthroplasty; BMI = body mass index; CAD = coronary artery disease; DM = diabetes; HTN = hypertension
Footnotes
Conflict of Interest
The authors have no conflicts of interest.
Contributor Information
Anne R. Bass, Division of Rheumatology, Department of Medicine, Hospital for Special Surgery, Weill Cornell Medical College, 535 E 70th Street, New York, NY 10021.
Tomás Rodriguez, Washington University School of Medicine in St. Louis, 660 S. Euclid Ave., St. Louis, MO 63110.
Gina Hyun, Washington University School of Medicine in St. Louis, 660 S. Euclid Ave., St. Louis, MO 63110.
Francisco G. Santiago, Clinical and Translational Science Center, Weill Cornell Medical College, 525 East 68th Street, Room A-150, New York, NY 10065
Jacqueline I. Kim, New York University School of Medicine, 550 1st Avenue, New York, NY 10016
Scott C. Woller, Intermountain Medical Center, University of Utah School of Medicine, PO Box 57700, Murray, UT 84157-7000.
Brian F. Gage, Washington University School of Medicine in St. Louis, 660 S. Euclid Ave., St. Louis, MO 63110.
References
- 1.CDC . FastStats: Inpatient surgery. 2013. [Google Scholar]
- 2.Memtsoudis SG, Gonzalez Della Valle A, Besculides MC, Gaber L, Sculco TP. In-hospital complications and mortality of unilateral, bilateral, and revision TKA: Based on an estimate of 4,159,661 discharges. Clin Orthop Relat Res. 2008;466:2617–2627. doi: 10.1007/s11999-008-0402-5. doi: 10.1007/s11999-008-0402-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hietala P, Strandberg M, Strandberg N, Gullichsen E, Airaksinen KE. Perioperative myocardial infarctions are common and often unrecognized in patients undergoing hip fracture surgery. J Trauma Acute Care Surg. 2013;74:1087–1091. doi: 10.1097/TA.0b013e3182827322. doi: 10.1097/TA.0b013e3182827322; 10.1097/TA.0b013e3182827322. [DOI] [PubMed] [Google Scholar]
- 4.Chong CP, van Gaal WJ, Savige J, Lim WK. Cardiac injury and troponin testing after orthopaedic surgery. Injury. 2011;42:855–863. doi: 10.1016/j.injury.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 5.Dawson-Bowling S, Chettiar K, Cottam H, Worth R, Forder J, Fitzgerald-O’Connor I, Walker D, Apthorp H. Troponin T as a predictive marker of morbidity in patients with fractured neck of femur. Injury. 2008;39:775–780. doi: 10.1016/j.injury.2008.01.025. doi: 10.1016/j.injury.2008.01.025; 10.1016/j.injury.2008.01.025. [DOI] [PubMed] [Google Scholar]
- 6.Sandhu A, Sanders S, Geraci SA. Prognostic value of cardiac troponins in elderly patients with hip fracture--a systematic review. Osteoporos Int. 2013;24:1145–1149. doi: 10.1007/s00198-012-2116-5. doi: 10.1007/s00198-012-2116-5; 10.1007/s00198-012-2116-5. [DOI] [PubMed] [Google Scholar]
- 7.Talsnes O, Hjelmstedt F, Dahl OE, Pripp AH, Reikeras O. Clinical and biochemical prediction of early fatal outcome following hip fracture in the elderly. Int Orthop. 2011;35:903–907. doi: 10.1007/s00264-010-1149-7. doi: 10.1007/s00264-010-1149-7; 10.1007/s00264-010-1149-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mangano DT, Browner WS, Hollenberg M, Li J, Tateo IM, study of perioperative ischemia research group Long-term cardiac prognosis following noncardiac surgery. JAMA. 1992;268:233–239. doi: 10.1001/jama.268.2.233. [DOI] [PubMed] [Google Scholar]
- 9.Nagele P, Brown F, Gage BF, Gibson DW, Miller JP, Jaffe AS, Apple FS, Scott MG. High-sensitivity cardiac troponin T in prediction and diagnosis of myocardial infarction and long-term mortality after noncardiac surgery. Am Heart J. 2013;166:325–332.e1. doi: 10.1016/j.ahj.2013.04.018. doi: 10.1016/j.ahj.2013.04.018; 10.1016/j.ahj.2013.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vascular Events In Noncardiac Surgery Patients Cohort Evaluation (VISION) Study Investigators. Devereaux PJ, Chan MT, Alonso-Coello P, Walsh M, et al. Association between postoperative troponin levels and 30-day mortality among patients undergoing noncardiac surgery. JAMA. 2012;307:2295–2304. doi: 10.1001/jama.2012.5502. doi: 10.1001/jama.2012.5502; 10.1001/jama.2012.5502. [DOI] [PubMed] [Google Scholar]
- 11.POISE Study Group. Devereaux PJ, Yang H, Yusuf S, Guyatt G, et al. Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): A randomised controlled trial. Lancet. 2008;371:1839–1847. doi: 10.1016/S0140-6736(08)60601-7. doi: 10.1016/S0140-6736(08)60601-7; 10.1016/S0140-6736(08)60601-7. [DOI] [PubMed] [Google Scholar]
- 12.PEP Prevention of pulmonary embolism and deep vein thrombosis with low dose aspirin: Pulmonary embolism prevention (PEP) trial. Lancet. 2000;355:1295–1302. [PubMed] [Google Scholar]
- 13.Oscarsson A, Gupta A, Fredrikson M, Jarhult J, Nystrom M, Pettersson E, Darvish B, Krook H, Swahn E, Eintrei C. To continue or discontinue aspirin in the perioperative period: A randomized, controlled clinical trial. Br J Anaesth. 2010;104:305–312. doi: 10.1093/bja/aeq003. doi: 10.1093/bja/aeq003; 10.1093/bja/aeq003. [DOI] [PubMed] [Google Scholar]
- 14.Devereaux PJ, Mrkobrada M, Sessler DI, Leslie K, Alonso-Coello P, et al. Aspirin in patients undergoing noncardiac surgery. N Engl J Med. 2014;370:1494–1503. doi: 10.1056/NEJMoa1401105. doi: 10.1056/NEJMoa1401105 [doi] [DOI] [PubMed] [Google Scholar]
- 15.Durazzo AE, Machado FS, Ikeoka DT, De Bernoche C, Monachini MC, Puech-Leao P, Caramelli B. Reduction in cardiovascular events after vascular surgery with atorvastatin: A randomized trial. J Vasc Surg. 2004;39:967–75. doi: 10.1016/j.jvs.2004.01.004. discussion 975-6. doi: 10.1016/j.jvs.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 16.Schouten O, Boersma E, Hoeks SE, Benner R, van Urk H, et al. Fluvastatin and perioperative events in patients undergoing vascular surgery. N Engl J Med. 2009;361:980–989. doi: 10.1056/NEJMoa0808207. doi: 10.1056/NEJMoa0808207; 10.1056/NEJMoa0808207. [DOI] [PubMed] [Google Scholar]
- 17.Winchester DE, Wen X, Xie L, Bavry AA. Evidence of pre-procedural statin therapy a meta-analysis of randomized trials. J Am Coll Cardiol. 2010;56:1099–1109. doi: 10.1016/j.jacc.2010.04.023. doi: 10.1016/j.jacc.2010.04.023; 10.1016/j.jacc.2010.04.023. [DOI] [PubMed] [Google Scholar]
- 18.Do EJ, Lenzini P, Eby CS, Bass AR, McMillin GA, et al. Genetics informatics trial (GIFT) of warfarin to prevent deep vein thrombosis (DVT): Rationale and study design. Pharmacogenomics J. 2011 doi: 10.1038/tpj.2011.18. doi: 10.1038/tpj.2011.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46:399–424. doi: 10.1080/00273171.2011.568786. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McMillin GA, Melis R, Wilson A, Strong MB, Wanner NA, Vinik RG, Peters CL, Pendleton RC. Gene-based warfarin dosing compared with standard of care practices in an orthopedic surgery population: A prospective, parallel cohort study. Ther Drug Monit. 2010;32:338–345. doi: 10.1097/FTD.0b013e3181d925bb. doi: 10.1097/FTD.0b013e3181d925bb. [DOI] [PubMed] [Google Scholar]
- 21.Singh JA, Jensen MR, Harmsen WS, Gabriel SE, Lewallen DG. Cardiac and thromboembolic complications and mortality in patients undergoing total hip and total knee arthroplasty. Ann Rheum Dis. 2011;70:2082–2088. doi: 10.1136/ard.2010.148726. doi: 10.1136/ard.2010.148726 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pedersen AB, Mehnert F, Sorensen HT, Emmeluth C, Overgaard S, Johnsen SP. The risk of venous thromboembolism, myocardial infarction, stroke, major bleeding and death in patients undergoing total hip and knee replacement: A 15-year retrospective cohort study of routine clinical practice. Bone Joint J. 2014;96-B:479–485. doi: 10.1302/0301-620X.96B4.33209. doi: 10.1302/0301-620X.96B4.33209 [doi] [DOI] [PubMed] [Google Scholar]
- 23.Hagen TP, Vaughan-Sarrazin MS, Cram P. Relation between hospital orthopaedic specialisation and outcomes in patients aged 65 and older: Retrospective analysis of US medicare data. BMJ. 2010;340:c165. doi: 10.1136/bmj.c165. doi: 10.1136/bmj.c165 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Menendez ME, Memtsoudis SG, Opperer M, Boettner F, Gonzalez Della Valle A. A nationwide analysis of risk factors for in-hospital myocardial infarction after total joint arthroplasty. Int Orthop. 2014 doi: 10.1007/s00264-014-2502-z. doi: 10.1007/s00264-014-2502-z [doi] [DOI] [PubMed] [Google Scholar]
- 25.Thornqvist C, Gislason GH, Kober L, Jensen PF, Torp-Pedersen C, Andersson C. Body mass index and risk of perioperative cardiovascular adverse events and mortality in 34,744 danish patients undergoing hip or knee replacement. Acta Orthop. 2014;85:456–462. doi: 10.3109/17453674.2014.934184. doi: 10.3109/17453674.2014.934184 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reichlin T, Hochholzer W, Bassetti S, Steuer S, Stelzig C, et al. Early diagnosis of myocardial infarction with sensitive cardiac troponin assays. N Engl J Med. 2009;361:858–867. doi: 10.1056/NEJMoa0900428. doi: 10.1056/NEJMoa0900428 [doi] [DOI] [PubMed] [Google Scholar]
- 27.Kawahara C, Tsutamoto T, Nishiyama K, Yamaji M, Sakai H, Fujii M, Yamamoto T, Horie M. Prognostic role of high-sensitivity cardiac troponin T in patients with nonischemic dilated cardiomyopathy. Circ J. 2011;75:656–661. doi: 10.1253/circj.cj-10-0837. doi: JST.JSTAGE/circj/CJ-10-0837 [pii] [DOI] [PubMed] [Google Scholar]
- 28.Lindahl B, Venge P, James S. The new high-sensitivity cardiac troponin T assay improves risk assessment in acute coronary syndromes. Am Heart J. 2010;160:224–229. doi: 10.1016/j.ahj.2010.05.023. doi: 10.1016/j.ahj.2010.05.023; 10.1016/j.ahj.2010.05.023. [DOI] [PubMed] [Google Scholar]
- 29.Urban MK, Jules-Elysee K, Loughlin C, Kelsey W, Flynn E. The one year incidence of postoperative myocardial infarction in an orthopedic population. HSS J. 2008;4:76–80. doi: 10.1007/s11420-007-9070-3. doi: 10.1007/s11420-007-9070-3; 10.1007/s11420-007-9070-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hietala P, Strandberg M, Kiviniemi T, Strandberg N, Airaksinen KE. Usefulness of troponin T to predict short-term and long-term mortality in patients after hip fracture. Am J Cardiol. 2014;114:193–197. doi: 10.1016/j.amjcard.2014.04.026. doi: 10.1016/j.amjcard.2014.04.026 [doi] [DOI] [PubMed] [Google Scholar]
- 31.DeLuca AJ, Kaplan S, Aronow WS, Sandhu R, Butt A, Akoybyan A, Weiss MB. Comparison of prevalence of unrecognized myocardial infarction and of silent myocardial ischemia detected by a treadmill exercise sestamibi stress test in patients with versus without diabetes mellitus. Am J Cardiol. 2006;98:1045–1046. doi: 10.1016/j.amjcard.2006.05.026. doi: 10.1016/j.amjcard.2006.05.026. [DOI] [PubMed] [Google Scholar]
- 32.Arenja N, Mueller C, Ehl NF, Brinkert M, Roost K, Reichlin T, Sou SM, Hochgruber T, Osswald S, Zellweger MJ. Prevalence, extent, and independent predictors of silent myocardial infarction. Am J Med. 2013;126:515–522. doi: 10.1016/j.amjmed.2012.11.028. doi: 10.1016/j.amjmed.2012.11.028; 10.1016/j.amjmed.2012.11.028. [DOI] [PubMed] [Google Scholar]
- 33.Sheifer SE, Gersh BJ, Yanez ND, 3rd, Ades PA, Burke GL, Manolio TA. Prevalence, predisposing factors, and prognosis of clinically unrecognized myocardial infarction in the elderly. J Am Coll Cardiol. 2000;35:119–126. doi: 10.1016/s0735-1097(99)00524-0. [DOI] [PubMed] [Google Scholar]
- 34.Bozic KJ, Bashyal RK, Anthony SG, Chiu V, Shulman B, Rubash HE. Is administratively coded comorbidity and complication data in total joint arthroplasty valid? Clin Orthop Relat Res. 2013;471:201–205. doi: 10.1007/s11999-012-2352-1. doi: 10.1007/s11999-012-2352-1 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wolf BR, Lu X, Li Y, Callaghan JJ, Cram P. Adverse outcomes in hip arthroplasty: Long-term trends. J Bone Joint Surg Am. 2012;94:e103. doi: 10.2106/JBJS.K.00011. doi: 10.2106/JBJS.K.00011 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Criner KT, Trionfo A. Impact of statins on postoperative venous thromboembolic events following total knee and hip replacements; AAOS Scientific Meeting Poster:Poster 204; 2014. [Google Scholar]