Abstract
Objectives
Children who are hard of hearing (CHH) have restricted access to acoustic and linguistic information. Increased audibility provided by hearing aids (HAs) influences language outcomes, but the advantages of appropriately-fit HAs can only be realized if children wear their devices on a consistent basis. The purpose of the current paper was to characterize long-term HA use in CHH, based on parent report measures, and identify factors that influence longitudinal trends in HA use.
Design
Participants were parents of 290 children with mild to severe hearing loss. At every visit, parents estimated the average amount of time the child used HAs per day during the week and on the weekends. Parent reports of daily HA use were analyzed to determine if different patterns of HA use were observed longitudinally during the study. Independent predictor variables were then related to longitudinal trends in HA use within three age groups (infant, preschool, school-age).
Results
On average across multiple visits, parents reported that their children wore their HAs for 10.63 hours per day (SD = 3.29). Data logging values were lower than parent report measures (M = 8.44, SD = 4.06), suggesting that parents overestimated daily HA use. The majority of children in each age group wore HAs at least 8 hours per day from their first research testing interval to their last, based on parent-report measures. Maternal education level predicted longitudinal trends in HA use for infants and school-age CHH. Degree of hearing loss was related to trends in school-age children only.
Conclusions
The current results indicated that the majority of CHH increased HA use over time, but a sizable minority demonstrated a low level of use or decreased use in the time period studied. Maternal education level influenced longitudinal trends in daily HA use. Degree of hearing loss influenced trends in school-age children only. Audiologists and early intervention service providers might aid in improving HA use by providing regular hands-on training with the HAs and individualized problem-based strategies to address the challenges families experience with attaining a high level of use. Families may also benefit from practical demonstrations of the benefits of consistent HA use, such as hearing loss simulations, examples of listening in noise with and without HAs, or listening to malfunctioning HAs.
INTRODUCTION
One of the goals of this monograph is to explore the concept that consistent access to the speech spectrum is a prerequisite for successful speech and language development. Children who are hard of hearing (CHH), by nature of their hearing loss, have restricted access to acoustic and linguistic information. Recent studies suggest that increased audibility provided by hearing aids (HAs) influences speech production, grammar and vocabulary outcomes (Koehlinger et al. 2013; Stiles et al. 2012; Tomblin et al. 2014). Presumably, however, the advantages of appropriately-fit HAs will only be realized if children wear their devices on a consistent basis. The ways in which amount of audibility and consistency of HA use accrue over time may reveal an effect of cumulative linguistic experience on speech and language development. The purpose of the current paper is to characterize long-term HA use in CHH, based on parent report, and determine what factors influence consistency of HA use over time. In subsequent articles in this monograph, we will seek to determine if amount of HA use influences auditory, speech, and language outcomes of CHH.
Most studies involving CHH have not addressed the contributions of aided audibility or amount of daily HA use on individual differences in speech perception, speech production, or language (Davis et al. 1986; Davis et al. 1981; Elfenbein et al. 1994; Fitzpatrick et al. 2011; Sininger et al. 2010). There is compelling evidence for a relationship between aided audibility and vocabulary skills (Stiles et al. 2012), as well as syntax (Koehlinger et al. 2013), articulation, and global language (Tomblin et al. 2014), but there is less research on how the amount of daily HA use might influence outcomes. Marnane and Ching (2015) examined HA use as a categorical variable and reported that the majority of 3 year olds were consistent users (i.e., more than 8 hours per day). They also found that children who wore HAs more frequently had higher scores on a parent-report scale of auditory skills, but there was no significant relationship between amount of HA use and functional outcomes after controlling for other demographic variables (maternal education level, additional disabilities). In contrast, other studies indicate that amount of HA use varies substantially across children who are hard of hearing (Fitzpatrick et al. 2010; Munoz et al. 2014; Walker et al. 2013; Munoz et al. 2015), when HA use is considered as a continuous variable as opposed to a categorical variable. Further research is needed to explore the influence of HA use (measured as a continuous variable) on auditory and language outcomes.
There is also evidence that the amount of HA use varies widely depending on the listening context, chronological age, and degree of hearing loss of the child, as well as socio-economic status of the family (Moeller et al. 2009; Walker et al. 2013; Munoz et al. 2015). Moeller and colleagues (2009) conducted longitudinal interviews with mothers of seven early-identified infants with mild to moderate hearing loss (age range = 11 to 28.5 months). Instead of asking mothers to estimate overall daily HA use, the researchers evaluated consistency of use with a Likert scale for different situations (e.g., in the car, book sharing, at the playground, etc.). Results showed that the infants were inconsistent HA users for most situations prior to two years of age. Only two out of the seven parents were able to establish early, consistent usage across all contexts. Over time, amount of HA use increased, although at the oldest age (28.5 months) there were still some situations that parents found problematic, such as riding in the car. Consistent with the findings of Moeller et al., Munoz and her colleagues (2014, 2015) have also found that HA management is difficult for families with younger children, particularly in specific contexts. Munoz et al. (2015) surveyed 37 families about parent-reported challenges with HA use. Munoz and colleagues noted wide variation in the amount of hours children wore their HAs, with 32% (n = 11) of parents reporting that their child wore HAs less than 5 hours per day. Similar to the results in Moeller et al. (2009), parents also reported that specific situations resulted in difficulty with HA compliance, including riding in the car, playing outside, or leaving the child in the care of alternate caregivers.
The findings by Moeller et al. (2009) and Munoz et al. (2015) suggest that there are individual differences in HA use time for young children as a result of the listening context, which could contribute to variation in speech and language outcomes in children with hearing loss. One limitation in both studies is that the researchers had to rely on parents as proxy reporters of HA use, because objective measures were not available at the time of data collection. Many current HA models now have data logging, a feature built into the HA which automatically records information about the HAs over time, including average hours of daily use. Jones and Launer (2011) utilized a database for pediatric HA fittings at participating clinics, and collected data logging information on approximately 5000 children, ages birth to 19 years. Consistent with the parent report measures in previous research (Moeller et al. 2009; Munoz et al. 2015) they found that the amount of HA use per day increased with age. Unlike the results in Moeller et al., the data logging results indicated that only 10% of children were full-time HA users, defined by Jones and Launer as more than 12 hours per day. Furthermore, 40% of children used their HAs for 4 hours or less per day. The average use time for the entire sample was 5.5 hours per day, although there was wide variation across children. Jones and Feilner (2013) reported on more recent data collected from the Phonak database. They separated use time based on the ages of the children, noting that infants and toddlers wore HAs an average of 5.5 hours and school-age children wore HAs an average of 7 hours per day. These results lend additional support to the premise that there is considerable variability in the amount of daily HA use in children with hearing loss. These daily use practices may interact with the level of aided audibility provided by the HAs, and together these two factors may influence developmental outcomes of CHH. However, further investigation is needed to support this hypothesis.
Because the data logging information in the Jones and Launer (2011) and Jones and Feilner (2013) studies were obtained through a confidential patient database, the authors were unable to describe the demographic characteristics of the children, and therefore, could not identify child- or family-specific factors that influenced individual differences in average daily HA use. Such information has clinical value, because it could help direct audiological and educational counseling practices. Marttila and Karikoski (2006) looked at HA use as a dichotomous variable (non-users versus users) and reported that chronological age, degree of hearing loss, and age at HA fitting influenced whether or not children wore HAs. Munoz et al. (2014) examined data logging results from a cross-sectional sample of 29 children. Based on descriptive statistics, they observed that HA use increased with chronological age and severity of hearing loss. Walker et al. (2013) examined predictive factors of average daily HA use within a cross-sectional, multi-center sample of 272 CHH, between the ages of 5 months to 7 years, 3 months. Results from a multiple regression analysis showed that longer daily HA use (based on parent report) was related to older age, poorer hearing, higher maternal education level, and recruitment site.
One drawback of Jones and Launer (2011), Munoz et al. (2015), and Walker et al. (2013) is that these studies used cross-sectional data to describe daily HA use. Moeller et al. (2009) collected longitudinal data on consistency of HA use across different contexts, but it was with a small number of children (n = 7). Given the trends seen in Moeller et al. (2009) and Munoz et al. (2014), as well as the significant predictor of age in the Walker et al. (2013) findings, it is likely that many children start off wearing HA only a few hours a day during infancy, but increase their amount of HA use during preschool. Alternative trends are also possible, however: some children may start off wearing their HAs for the majority of the day and maintain that level of HA use over time. Other children may start off using the HAs frequently but decrease use over time, perhaps due to the influence of degree of hearing loss. For example, children with mild degrees of HL may start to identify situations where they feel they can “get by” without amplification as they get older. All three trends are plausible, but more importantly, there are different implications for counseling depending on which pattern children tend to show.
There is limited clinical evidence regarding the influence of HA use on developmental outcomes. In order to examine the effects of amplification on outcomes, we first need to understand the longitudinal variations in HA use from infancy to the early school-age years, as well as the variables that predict trends in longitudinal HA use for individual children. These lines of research, when considered in combination with the influence of audibility (McCreery et al., this issue, pp. xxxx) and linguistic input (Ambrose et al., this issue, pp. xxxx), will allow clinicians and researchers to make more informed evidence-based decisions on appropriate interventions for families of young children with hearing loss.
The current study addresses the following research questions:
What are longitudinal trends in daily HA use among CHH? We predict that most children will increase HA use over time, based on parent report. We also anticipate that trends in longitudinal HA use will vary as a function of chronological age at baseline (i.e., most school-age children will display trends of high HA use over time, while most infants will display trends of low HA use initially, but increased HA use over time).
What factors predict trends in daily HA use over time? We predict that greater degree of hearing loss and higher maternal educational level will be predictive of greater daily HA use over time. Gender, age at HA fitting, and recruitment site will not.
MATERIALS AND METHODS
Participants
Participants were parents of 290 children (133 females) with hearing loss who wore HAs. At the initial testing visit, the children were between the ages of 5 months and 7 years, 1 month (M = 39.84 months; SD = 21.58 months). Two hundred and twenty children (75.9%) referred from their newborn hearing screen. The mean age at confirmation of hearing loss was 7.34 months (median = 3.0, SD = 12.11) and the mean age at fitting of HAs was 11.20 months (median = 5.75, SD = 14.47) for children who failed the newborn hearing screen.
Sixty-nine children were identified with hearing loss after the newborn period, due to passing the newborn hearing screen, not being screened, or lack of follow-up following the failed newborn hearing screen (one child’s newborn hearing screen status was unknown). Of those 69 participants, the mean age at confirmation of hearing loss was 28.48 months (median = 28, SD = 17.15) and the mean age at HA fitting was 31.68 months (median = 30.00, SD = 18.32). Based on a review of medical records and parent report, we were able to confirm that 30.4% of these later-identified children had a congenital hearing loss and 29% had a confirmed post-natal onset of hearing loss as a result of structural abnormalities (e.g., Enlarged Vestibular Aqueduct Syndrome) or acquired etiologies (e.g., ototoxicity, meningitis, assisted ventilation). We were unable to determine the onset of hearing loss for 40.6% of the group.
The mean better-ear pure-tone average (BEPTA) for the whole group at the baseline visit was 48.73 dB HL (SD = 13.48). Sixty-nine participants had a slight/mild hearing loss (16.25 to 39 dB HL), 150 had a moderate hearing loss (40 to 59 dB HL) and 64 had a moderately-severe/severe hearing loss (60 to 82.50 dB HL) at the baseline visit (7 did not have audiometric data at the baseline visit). Twelve percent (34/290) presented with a progressive hearing loss during the course of the study, as determined by more than a 10 dB HL increase in BEPTA (i.e., decline in thresholds) between the first and last visit. Two hundred eighty-three children were fitted with wide dynamic range compression HAs and 6 had bone conduction HAs. One child had wide dynamic range compression HAs at the first visit and bone conduction HAs at all subsequent visits. Ten children received cochlear implants subsequent to study enrollment. Only pre-implantation data are included in the current analysis.
Data collection
As previously described in this monograph (Tomblin et al., this issue, pp. XXX), children and their families participated in an initial baseline visit, followed by two visits a year for children under age 2 and one visit a year for children older than 2 years for up to four years, or until 9 years of age. The number of visits varied across children, depending on their age at enrollment and time of study completion. At the initial visit, parents completed an intake interview with an examiner. Intake questions documented demographic characteristics related to the child and family, including predictor variables incorporated in the present study (i.e., maternal education level, gender, and age at HA fitting). At every visit, parents participated in a face-to-face interview regarding HA use. To determine long-term trends in HA use, we included data from each visit for parents who completed the HA use questionnaire at more than one visit (number of observations = 915). Seventy parents reported on HA use for two visits, 86 for three visits, 100 for four visits, 21 for five visits, and 2 for six visits.
In addition to parent-report measures of HA use, audiologists obtained data logging information when possible. Families were unaware that the data logging feature was used throughout the data collection period, and the results were not shared with parents due to potentially biasing effects of intervention. In the current analysis, 232 children had at least one visit in which data logging and parent report measures could be compared. Eighty-four children had data logging collected at one visit, 107 children had data logging at two visits, 37 had data logging at three visits, and 4 had data logging at four visits.
Hearing aid use questionnaire
As part of each visit, an examiner conducted an interview with the caregiver pertaining to pediatric HA use (see Walker et al. 2013, for an example of the HA use questionnaire). Parents estimated the average amount of time the child used HAs per day during the week and on the weekends. To compare the parent report estimate to data logging, we calculated a weighted HA use measure in which parents’ estimates of weekday use was multiplied by 0.71 (5/7 days of the week) and weekend use was multiplied by 0.29 (2/7 days of the week). The two values were then added together. This weighted measure was used to represent HA use time in all statistical analyses.
Hearing aid datalogging
Audiologists collected values for average use time per day by connecting the HAs to a HiPro box and using the appropriate HA software to obtain data logging values. If the values were different between ears, the larger value was included in data analyses.
Statistical analyses
The experimental design for the two primary research questions in this study was longitudinal with multiple age cohorts (i.e., infant, preschool, school-age). For our first research question, investigating HA use over time, we analyzed clusters based on longitudinal trends in daily HA use. To determine how longitudinal trends tend to cluster, we examined parent report of HA use at the baseline visit in combination with the amount of change between the first and the last visit. Ward’s hierarchical clustering (Ward 1963) was used to determine cluster groupings in the longitudinal HA trends.
In our second research question, we examined which independent predictor variables were related to longitudinal trends in HA use. To investigate the relationships among the independent predictor variables and the dependent response variables, we used logistic regression models. Statistical analyses were conducted by separating children into three subgroups based on age at baseline visit: infants (6 months to 2 years, n = 80), preschool (2 years to 5 years, n = 134); and school-age (5 years to 7 years, n = 76). Due to low sample sizes and missing data, univariate analyses were performed within each age group. Logistic regression was conducted with the continuous independent variables, age at HA fitting and BEPTA (four-frequency PTA when it was available, three-frequency PTA when it was not). Fisher’s chi-square tests were conducted with the categorical variables: maternal education level, test site, and gender. Because the number of visits differed across children, we also used Fisher’s exact test to evaluate the effect of number of visits that each participant had within each of the clusters. We used Cohen’s (1988) criteria to determine effect sizes for the regression analyses (small = 1.49; medium = 3.45; large = 9).
The independent variables were gender, recruitment site (University of Iowa, Boys Town National Research Hospital, and University of North Carolina-Chapel Hill), maternal education level, BEPTA, age at HA fitting, and number of visits. Maternal education and BEPTA were obtained from the baseline visit. The dependent variables consisted of pre-determined dichotomous categories of longitudinal HA use, based on the results of the cluster analysis. Due to the large number of maternal education categories collected, arbitrary nominal levels were introduced in the data analysis. Table 1 displays descriptive statistics summarizing both the independent and dependent variables that were included in the regression analysis.
Table 1.
Summary of descriptive statistics and demographic characteristics for children with HAs at baseline visit (n = 290).
| Variable | Mean | Median | SD | Min | Max | n |
|---|---|---|---|---|---|---|
| Chronological age (months) | 39.84 | 38.00 | 21.58 | 5.00 | 87.00 | 290 |
| Better-ear PTA (dB HL) | 48.73 | 48.75 | 13.48 | 16.25a | 82.50b | 283 |
| Daily HA use: weighted (hours) |
10.04 | 11.00 | 3.41 | 0.00 | 17.00 | 290 |
| Age at HA fitting (months) | 16.08 | 7.00 | 17.75 | 1.00 | 72.00 | 290 |
| Maternal education level | % | n | ||||
| High school or less | 15.5 | 45 | ||||
| Vocational school/some collegec | 31.7 | 92 | ||||
| Collegec | 25.9 | 75 | ||||
| Graduate school | 27.0 | 78 | ||||
| Gender | ||||||
| Male | 54.1 | 157 | ||||
| Female | 45.9 | 133 | ||||
| Test site | ||||||
| Boys Town | 41.0 | 119 | ||||
| Iowa | 24.5 | 71 | ||||
| North Carolina | 34.5 | 100 | ||||
Note. HA = Hearing aid
Fourteen children’s PTAs fell outside the criterion range (25–75 dB HL). The research team made some exceptions at both ends of the range, due to unique audiological or medical circumstances (e.g., hearing loss in low or high frequencies only, fluctuation due to otitis media with effusion or enlarged vestibular aqueduct syndrome).
College refers to a four-year university setting.
RESULTS
Descriptive HA use data
On average, parents reported that their children wore their HAs for 10.78 hours per day during the week (SD = 3.26) and 10.24 hours per day during the weekends (SD = 3.68). The weighted sum of weekday and weekend use was 10.63 hours per day (SD = 3.29). Data logging indicated 8.44 hours per day (SD = 4.06). These values are longitudinal and include repeated measures, in that there are multiple data points for individual children across visits. Descriptively, the values are slightly higher than the data reported in Walker et al. (2013) (10.48 hours for weekday use, 9.96 hours for weekend use, and 8.2 hours for data logging), which may reflect the inclusion of later visits and an increase in data from older children in the current analysis. Figure 1 displays the distributions in the parent-report measure for HA use and data logging (with repeated measures for both parent-report and data logging measures). It is apparent from the figure that the median amounts of HA use increased with age, as reported on parent measures and through data logging measures. This trend supports our prediction that HA use will increase over time.
Figure 1.
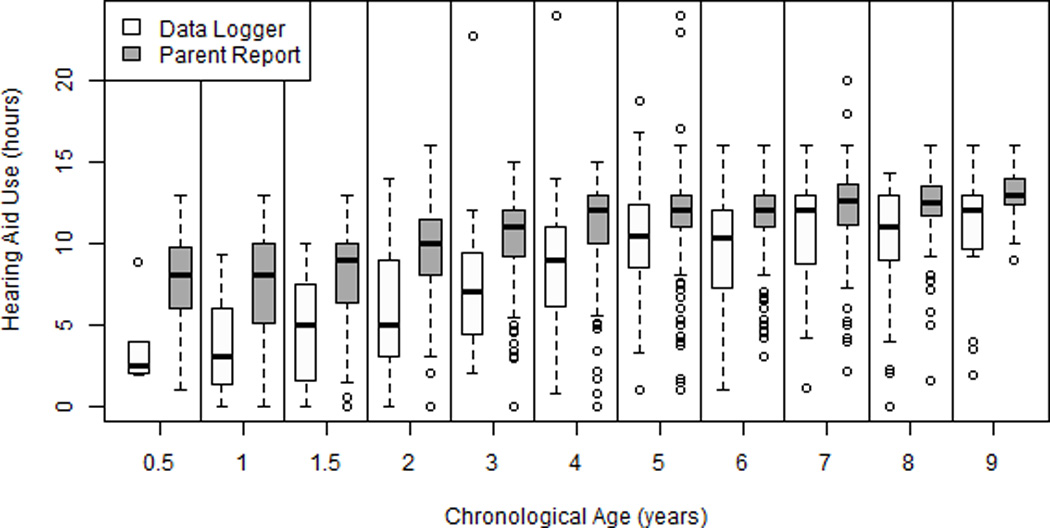
Box plot of amount of HA use based on data logging and parent report over time. The central lines represent the median values and the box limits are the 25th and 75th percentiles. The lower fence is from the 10 to 25th percentile and the upper fence is from the 75 to 90th percentile. The circles represent outliers at the upper and lower 10th percentiles.
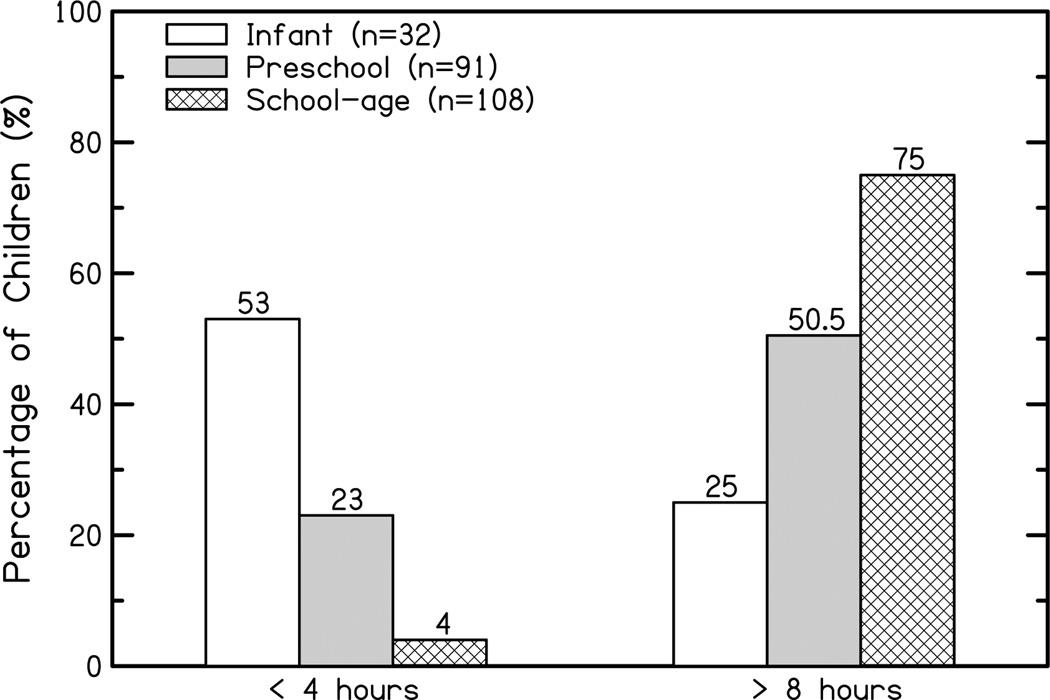
Figure 2 displays the mean and median values for hours of use, per age group, based on data logging values from the first visit in which data logging was obtained (i.e., no repeated measures). Data logging results indicated that infants (i.e., children with visits between 6 months and 2 years of age) wore HAs an average of 4.36 hours per day (SD = 3.17), preschoolers (i.e., children with visits between 2 and 4 years of age) wore HAs an average of 7.57 hours per day (SD = 4.32), and school-age children (i.e., children with visits between 5 and 9 years of age) wore HAs an average of 10.15 hours per day (SD = 3.33). Figure 3 displays the percentage of children who were routine HA users and limited HA users, based on data logging. We defined routine use as 8 hours or more per day, based on the fact that infants generally sleep an average of 14 hours, which decreases to an average of 10 hours for 9 year olds (Iglowstein et al. 2003). We also took into account times during the day when it is unlikely children would be wearing HAs (e.g., swimming, bath, getting dressed). We acknowledge that this value associated with “routine” is arbitrary and 8 hours per day should not be considered full-time or optimal use for children. We defined limited HA use as less than 4 hours per day, using the rationale that such low use is inconsistent with best practice recommendations for young children who use HAs.
Figure 2.
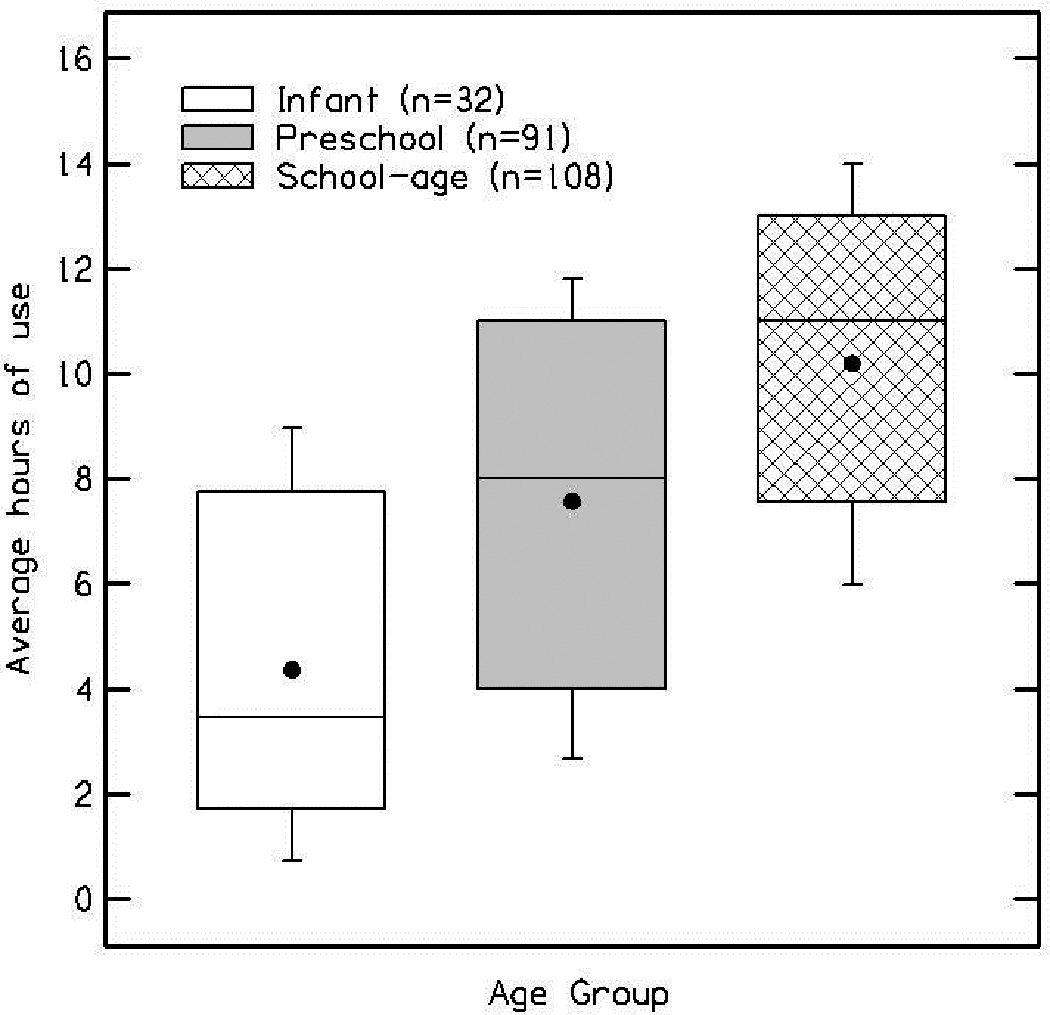
Box plot of data logging measures by age group. The central lines represent the median values, the black dots are the mean values, and the box limits are the 25th and 75th percentiles. The lower fence is from the 10 to 25th percentile and the upper fence is from the 75 to 90th percentile.
Figure 3.
Percentage of children who were limited HA users vs routine HA users based on data logging values, separated by age groups.
Relationships between parent report measures and data logging: cross-sectional analysis
To examine the relationship between parent report measures and data logging, we compared data from the first visit in which both measures were collected (n = 232). Thus, the analysis in this section is cross-sectional rather than longitudinal, to avoid having to account for multiple visits with individual participants. Using a Pearson correlation coefficient, there was a statistically significant correlation between parent report measures and data logging (r = 0.71, p < .001). This correlation was consistent with the relationship between parent-report measures and data logging described in Walker et al. (2013), in which parent report of HA use and data logging showed a significant correlation of 0.76. The correlation between parent report and data logging was generally consistent across age groups (infants: n = 34, r = 0.69, p < .001; preschool: n = 98, r = 0.62, p < .001; school-age: n = 100, r = 0.61, p = .001).
The mean difference between parent report measures and data logging was 2.34 hours (SD = 3.04) for all participants. When children were separated based on age, infants had a mean difference between parent report measures and data logging of 2.43 hours (SD = 2.45), preschoolers had a mean difference of 2.53 hours (SD = 3.36), and school-age children had a mean difference of 2.13 hours (SD = 2.90). In total, 81% of parents overestimated the amount of time their child wore their HAs, and 19% were accurate or underestimated HA use. Again, this is consistent with the cross-sectional findings in Walker et al. (2013), in which the average overestimation was 2.6 hours (n = 133, SD = 2.52) and 84% of parents overestimated daily HA use. Taken together, the correlational data and mean differences between data logging and parent report data suggest that the majority of parents overestimate HA use, but the relative difference between parents’ estimations and data logging is consistent across children.
To better understand differences between parent report measures and data logging, we examined 95% confidence intervals for data logging given increasing amounts of HA use reported by parents for the whole group. If a parent reported five hours of daily use, the model estimated data logged time was 3.60 hours with a 95% confidence interval between 2.87 and 4.32 hours. If a parent reported 10 hours of daily use, the estimated data logged time was 7.74 hours with a 95% confidence interval of 7.35 to 8.13 hours. If a parent reported fifteen hours of daily use, the estimated data logged time was 11.88 hours with a 95% confidence interval from 11.27 to 12.49 hours.
We conducted a multiple linear regression analysis to determine what factors predicted the amount of overestimation between parent report of HA use and data logging values. Independent variables included maternal education level, child’s chronological age, recruitment site, gender, and BEPTA. The dependent variable was the difference between parent report of HA use and data logging value at the first visit in which parent report and data logging were both available (n = 232). Only BEPTA was a significant predictor of overestimation (β = −.14, p = .03). Parents of children with better hearing were more likely to overestimate HA use compared to parents of children with poorer hearing. These results were inconsistent with results in Walker et al. (2013), in which chronological age was the only significant predictor of the amount of overestimation in parent report (i.e., parents of younger children tended to overestimate more than parents of older children). This discrepancy may be related to the addition of more children with mild hearing loss in the current data set (54 children, compared to 24 children in the mild hearing loss range in Walker et al. 2013). Parents of children with mild hearing loss may be less aware of how often their child is wearing HAs on a daily basis, perhaps because there are circumstances in which these children do not wear amplification consistently (e.g., after school, on the weekends).
Relationships between parent report measures and data logging over time: longitudinal
To determine whether or not trends in parent report hours of use would be consistent with trends in data logging, we examined results for 38 children (16 infant, 14 preschool, 8 school-age) who had data logging and parent report measures at both their first baseline visit and last visit. We conducted a two-sample paired t-test to assess the differences between parent report and data logging for their baseline scores and change scores (difference between baseline and last visit). There was a significant difference between the baseline scores for parent report and data logging hours (p < .001), which is expected given the mean differences presented in the descriptive data for the whole group of children. Paired t-tests did not indicate a significant difference in the change values over time (p = .15). In other words, the difference between hours of use at the baseline visit compared to the final visit was similar between parent report measures and data logging. Thus, parent report data showed the same relative trends as data logging over time.
Research question 1: What are longitudinal trends in HA use?
For the current longitudinal cluster analysis (question 1) and the subsequent logistic regression analysis (question 2), we relied on parent report measures rather than data logging. Although objective data logging measures may have been preferable, such an analysis would have been limited due to the lower number of repeated measures for data logging, particularly for children with three or more visits (41 children had data logging at three or more visits, compared to 209 children with parent report data). Furthermore, the correlation between data logging and parent report was strong and the relative trends were similar over time. Given the much larger number of participants with long-term parent report data compared to data logging, parent report of HA use allowed us to examine long-term trends with sufficient power to conduct regression analyses.
For question 1, we predicted that longitudinal trends in HA use might vary as a function of chronological age at baseline. To further investigate that prediction, children were separated into three groups by age at the baseline visit: infant, preschool, and school-age. Data from each age group were clustered based on the amount of HA use at the initial visit (high, low) and direction of growth between the initial and final visit (increasing, decreasing, no change). Because participants varied in the number of visits, final visits did cross into the older age groups for some participants (i.e., a child might start the study at 2 years of age and be followed over four visits so that their final visit was at 6 years of age). In these cases, the age cohort was based on the child’s age at the start of the study. We arbitrarily divided higher and lower amounts of HA use at 8 hours, using the rationale stated earlier in this manuscript.
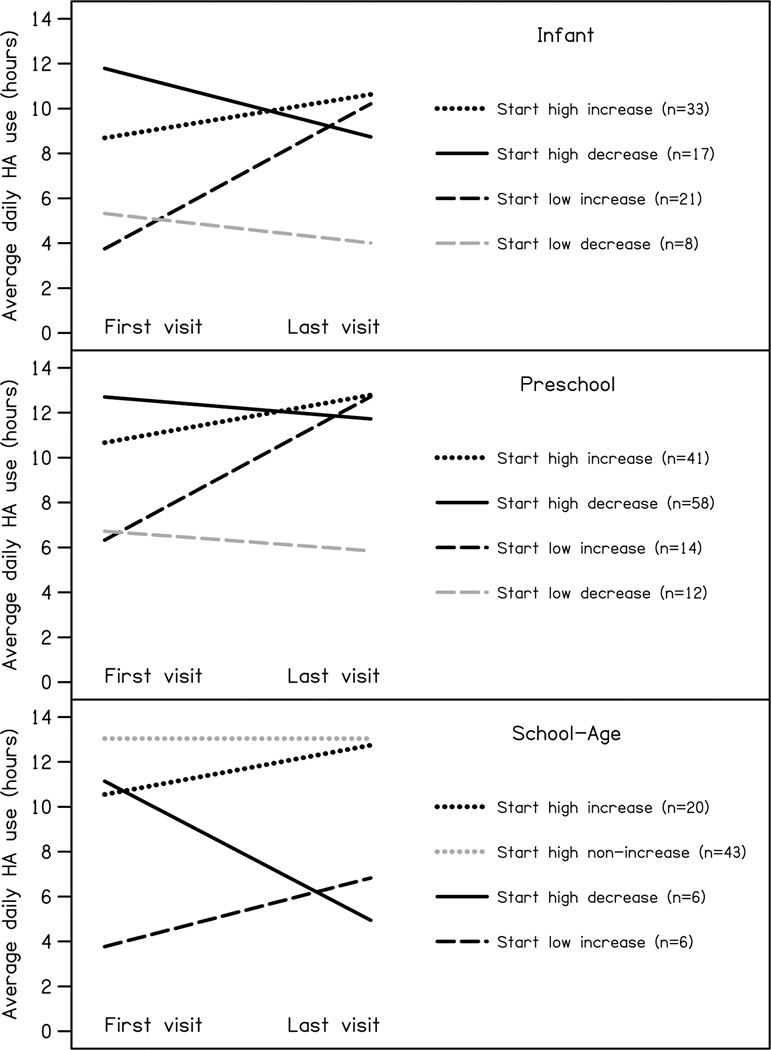
For longitudinal HA use, infants were clustered into categories of 1) high daily use increasing over time, 2) high daily use decreasing over time, 3) low daily HA use increasing over time and 4) low daily use decreasing over time (see Table 2 and Figure 4). Children in the first group (high-increase) made up 42% of the group, whereas 22% showed the high-decreasing trend. Both of these groups showed an early pattern of high HA use, even though they showed different trajectories in HA use over time. These two groups were combined for the statistical analysis, because of their similar amounts of long-term HA use. There was a subgroup of infants who were low HA users, but increased their use with time (27%). Finally, there was a group of infants (10%) who showed low amounts of HA use at baseline, and remained low users over time. The latter two groups were analyzed separately, because they demonstrated different patterns of use over time.
Table 2.
Infant, preschool, and school-age groups: Means (SDs) of initial hours of HA use and change in HA use between first and last visit (based on parent report measures), categorized by clusters over time.
| Infant Cluster | Initial Mean (SD) | Change Mean (SD) | n | % |
| Start High Increase | 8.69 (1.23) | 1.94 (1.4) | 33 | 64% |
| Start High Decrease | 11.79 (1.09) | −3.05 (2.69) | 17 | |
| Start Low Increase | 3.75 (2.15) | 6.46 (2.22) | 21 | 27% |
| Start Low Decrease | 5.32 (0.95) | −1.31 (2.34) | 8 | 10% |
| Preschool Cluster | Initial Mean (SD) | Change Mean (SD) | n | |
| Start High Increase | 10.67 (1.14) | 2.12 (0.94) | 41 | 79% |
| Start High Decrease | 12.7 (1.1) | −0.97 (1.71) | 58 | |
| Start Low Increase | 6.33 (3.18) | 6.39 (2.54) | 14 | 11% |
| Start Low Decrease | 6.72 (2.65) | −0.87 (1.89) | 12 | 10% |
| School age Cluster | Initial Mean (SD) | Change Mean (SD) | n | |
| Start High Increase | 10.55 (1.6) | 2.19 (2.03) | 20 | 84% |
| Start High Non Increase | 13.04 (1.18) | 0 (1.16) | 43 | |
| Start High Decrease | 11.14 (2.94) | −6.2 (2.12) | 6 | 16% |
| Start Low Increase | 3.77 (1.75) | 3.06 (3.98) | 6 | |
Figure 4.
Average trend plots of four clusters from first to last visit, based on parent report of daily HA use within the three age cohorts (infant, preschool, school-age).
Preschoolers were clustered into groups that were similar to the infants: 1) high daily use increasing over time, 2) high daily use decreasing over time, 3) low daily use increasing over time, and 4) low daily use decreasing over time (see Table 2 and Figure 4). When the high-increase and high-decrease clusters are combined, 79% of the preschool-age children could be viewed as wearing their HAs more than 8 hours per day over time. Again, these two groups were combined for the logistic regression, because both trends represented high HA use from the baseline to the final visit. Eleven percent wore HAs at low levels at the first visit, but increased use time by their last visit, while 10% demonstrated low amounts of HA use over time. Like the infants, the latter two groups were analyzed separately.
Data for school-age children clustered into slightly different longitudinal trends compared to the infants and preschoolers. One trend included children who demonstrated high daily HA use initially, which increased over time, while another trend included children with high daily HA use and no change over time (see Table 2 and Figure 4). These two groups were combined, because both trends represented high HA use from the baseline to the final visit. Together, these groups made up 84% of the school-age children. Six children displayed high HA use initially, but decreased daily use over time. Another six children displayed low HA use initially, and increased use by the final visit, but still not to a level that would be considered high level of HA use based on the average amount of daily use for school-age children (M = 11.49). These two groups were also combined, because both trends represented low usage over time. Together, these two groups made up 16% of the school-age children.
By examining parent-report of HA use as a function of age, the majority of children in each age group wore HAs more than 8 hours per day from their first OCHL study visit to their last. As predicted, the percentage of children in this particular cluster increased with age, from 64% of the infants to 84% of the school-age group. Interestingly, even though there was no overlap in participants across the three groups, the percentage of children who demonstrated low HA use over time was fairly constant across the three age groups (10% in the infant and preschool groups; 16% in the school-age group). These data suggest that there is a fairly constant percentage of children who maintain low HA use as they get older.
Research Question 2: What factors predict trends in longitudinal HA use?
Because chronological age did appear to influence longitudinal HA patterns, both in the trends that were displayed and the percent of children who fell into those clusters, we used regression analyses within each age group, as opposed to combining the entire group. This allowed us to identify the factors that predict which children fell into the longitudinal cluster groups, as a function of age.
Infants
The first analysis of infants combined the start high-increasing group with the start high-decreasing group (based on the rationale that both groups showed a trend of more than 8 hours of HA use over time). This combined start high group was compared to the start low-increasing group. Pairwise comparisons for maternal education levels revealed significant differences between levels, with large effect sizes (i.e., odds ratios). The odds of being in the start low-increasing group instead of the start high group were 9 times higher for mothers with a high school diploma compared to mothers with some college education or mothers with a post-graduate degree (OR = 8.99, p = 0.03; OR = 9.01, p = 0.04, respectively), and 18 times higher for mothers with a high school degree compared to mothers with a bachelor’s degree (OR = 18.15, p = 0.01). Table 3 displays a summary of significant variables and odds ratios for the infant cohort. There were no other significant pairwise comparisons in maternal education level (p > 0.05). Recruitment site, age at HA fitting, gender, BEPTA, and number of visits were not significant predictors of cluster groups (all p-values > 0.18).
Table 3.
Summary of significant results in logistic regression analyses.
| Infant | School-age | ||
|---|---|---|---|
| Predictor Variables | Odds ratio (p value) | Odds ratio (p value) | |
| Maternal education level | |||
| HS vs some collegea | 8.99 (.03) | ||
| HS vs post-graduatea | 9.01 (.04) | ||
| HS vs bachelor’s degreea | 18.15 (.01) | ||
| Some college vs bachelor’s degreeb | 13.89 (.04) | ||
| Some college vs post-graduateb | 19.96 (.02) | ||
| BEPTA | |||
| Better hearing vs poorer hearingb | 1.10 (.02) | ||
Note: HS = high school degree or less; BEPTA = better-ear pure-tone average;
Pairwise comparison of infants in the start low-increasing cluster to infants in the consistent HA use cluster, with infants in the start low-increasing group more likely to be have mothers with less education;
Pairwise comparison of school-age children in the inconsistent HA cluster to school-age children in the consistent HA cluster, with inconsistent users more likely to have better hearing and mothers with less education.
The second analysis of infants compared the start low-increasing group to the start low-decreasing group. No factors predicted which children fell into these groups, possibly due to small sample sizes (n = 8 for children in the start low-decrease group and n = 19 for children in the start low-increase group).
Preschool
The first analysis of the preschool group combined the start high-increasing cluster with the start high-decreasing cluster, following the same rationale used with the infants. This combined start high group was compared to the start low-increasing cluster. None of the predictor variables were significant (all p-values > 0.07).
The second analysis compared the start low-increasing group with the start low-decreasing group. There were no significant predictors of group membership between these two comparisons, except for the number of visits (p < 0.01). The low decreasing group had fewer overall visits than the low increasing group. All of the preschool children in the low decreasing group had two or three visits while the majority of the low increasing group had four visits. This resulted in a greater proportion of children who were 5 years or older (79%) in the low increasing group at the last visit compared to the low decreasing group (33%). Thus, it is possible that if we had been able to continue following the children in the low decreasing group, the trends may have reversed upon school entry.
School-age
For school-age children, we combined the start high-increasing group with the start high-no change group. This group represented routine HA users who wore HAs more than 8 hours per day over time. We also combined the start low-increasing group with the start high-decreasing group. This group represented low HA users over time. These two groups were then compared to one another. Maternal education level was a significant predictor of group (p = 0.05), with large effect sizes. Children whose mothers had a bachelor’s degree were approximately 14 times more likely to be routine users, compared to mothers who had some college education (OR = 13.89, p = 0.04). Children whose mothers had a post-graduate degree were 20 times more likely to be in routine users, compared to mothers with some college education (OR = 19.96, p = 0.02). No other pairwise comparisons were significant for maternal education level. BEPTA was also a significant predictor of cluster group (OR = 1.10, p = 0.02), with small effect sizes. In other words, children with better hearing were more likely to use HAs less frequently over time, while children with poorer hearing were more likely to be in clusters using HAs 8 hours or more over time. Age at HA fitting, recruitment site, gender, and number of visits were not significant predictors of cluster group (all p values > 0.36). Table 3 summarizes the significant results from the regression analyses.
In summary, the results of the regression analysis indicate that maternal education level is a significant predictor of longitudinal trends in HA use for infants and school-age CHH. None of the variables were significant predictors for preschool-age children, but the present findings appear to have been influenced by the number of visits per cluster for the preschoolers. Degree of HL was a significant predictor of longitudinal HA use trends for elementary school-age children only.
DISCUSSION
The primary goals of the current study were to describe longitudinal trends in HA use and examine the factors that influenced longitudinal trends. Results showed that CHH vary in the amount of time they wear HAs, which is consistent with previous findings from the OCHL cohort and others (Moeller et al. 2009; Munoz et al. 2014; Munoz et al. 2015; Walker et al. 2013). Specific factors appeared to influence long-term trends in HA use, but interestingly, these predictors differed depending on the age range in question.
Research question #1: What are longitudinal trends in daily HA use?
The results for our first research question were consistent with our predictions. We expected to see most of the children show a pattern of increasing HA use over time and the results supported this hypothesis. Many of the children within each of the three age cohorts were routine HA users who wore HAs 8 hours per day or more to start with and maintained that level of use over time. It should be acknowledged that these data may be an overestimation of the percentage of children who might be considered routine HA users, because it was based on parent report data rather than data logging. An important future direction for this line of research will be to investigate longitudinal trends in HA use using data logging as an objective measure of use time.
Not surprisingly, the infant group demonstrated the smallest percentage of children who wore HAs more than 8 hours per day over time (64%). Although this still represents a majority of the infants, a substantial minority (36%) of parents reported very limited HA use, at least initially. It is encouraging to note, however, that 27% of the infants showed a trend of moving from limited to more routine HA use with age. This cluster within the infant age group is important to recognize, because it shows families that it is possible to overcome challenges to HA use for CHH during the infant and toddler years. These findings highlight a need for continued support for families who are dealing with HA compliance issues in young children. In our previous work, parents recounted child-related challenges as causes for less-than-optimal hearing aid use consistency, although the report of these challenges decreases by age 2 years (Walker et al. 2013). Munoz et al. (2014) investigated the issue of child-related challenges in more detail, and reported that parents had concerns about losing the HAs in public places or when the child was in the care of others. Furthermore, because individual differences in language abilities are greater for younger children than older children (Fenson et al. 2000), parents of infants may not see the benefit of wearing HAs as readily as parents of children who are older. Nevertheless, it is important for service providers to remind parents of infants of the cumulative nature of the benefit of HA use. Parents who report that they are confident in their ability to manage their child’s HAs also perceive that their child wears their device more often and feel that they are more involved in their child’s development of speech and language, compared to parents who report feelings of low self-efficacy with regards to HA management (Desjardin 2005). Audiologists and early intervention service providers might aid in improving HA use consistency, especially for families with low socioeconomic status, by providing regular hands-on training with the HAs or providing a parent-parent mentor. Families may also benefit from practical demonstrations of the benefits of consistent HA use, such as hearing loss simulations, examples of listening in noise with and without HAs, or listening with malfunctioning HAs. To date, however, there is no evidence-based research to indicate what strategies are most effective for improving HA compliance in young children. Future research might explore the efficiency of different counseling practices in improving HA compliance in infants, for audiologists, speech-language pathologists, and early interventionists.
The current findings also indicate that a fairly stable percentage of infant, preschool and school-age children maintained lower HA use over time (10 to 16% across the age cohorts), even though the participants in these age cohorts did not overlap. This may be an underestimation of the proportion of children with low levels of HA use over the long term, as the analyses were performed with parent report data compared to data logging, and parent report has been found to regularly overestimate data logging values. Bearing this in mind, these results indicate a need for support and continued counseling by service providers regarding the importance of consistent device use, even after children have worn HAs for several years. In this context, a discussion of the results of data logging (currently available in most HA models) with parents and children could play a role in counseling efforts during regular intervention visits. It is also likely to be helpful to continue to discuss context-specific barriers to HA use with parents. For example, as children enter late-elementary and middle school, they may be less inclined to wear HAs in social settings. Children may encounter challenges when they are in situations where they must wear a helmet (e.g., bike riding, sports). The current data set only includes children in the early elementary school years; therefore, it is unclear what potential barriers may arise as children get older. We are continuing to follow this cohort of children into later elementary grades to explore this issue in a renewal of the original OCHL grant.
Research question #2: What factors predict trends in daily HA use over time?
We hypothesized that two factors – poorer hearing and higher maternal education level – would predict more consistent HA use over time. We based the first two predictions on findings from our previous research (Walker et al. 2013), in which BEPTA and maternal education level were significant predictors of amount of daily HA use.
Our predictions were correct, in that degree of HL and maternal education level both influenced parent-reported trends in HA use over time. We did not predict that these variables would have a different effect depending on the age of the child, although this finding is not surprising. Maternal education level was a significant predictor for the youngest age group and the oldest age group: infants and school-age children whose mothers had more education were more likely to start off wearing the HAs more than 8 hours per day, and maintain that level of use over time, while children whose mothers had less education tended to fall into a pattern of low initial HA use, increasing with time. Within the preschool group, however, maternal education level did not influence trends in HA use. This may be due to the fact that by this age, parents and children, regardless of socioeconomic status, have had sufficient time to appreciate the level of benefit the child receives from amplification, or be more cognizant of lack of progress in speech and language skills. At this stage in development, family-specific factors such as maternal education level may start to play less of a role in the amount of daily HA use (Walker et al. 2013), although it is not clear from the present analysis if child-specific factors play more of a role.
With school-age children, both maternal education level and severity of hearing loss appeared to play a role in higher versus lower levels of HA use. This shift in influential factors over time is practical information for service providers because it highlights a change in emphasis of counseling, depending on the age of the child. It is also important to note that the school-age children with more severe degrees of hearing loss tended to be more routine HA users, whereas children with milder degrees of hearing loss tended to show less regular HA use. The influence of degree of hearing loss is consistent with our previous findings (Walker et al. 2013). In that study, children with BEPTAs of more than 50 dB HL wore HAs more often than children with BEPTA of less than 50 dB HL, based on ratings of consistency of use both in public and at school. Fitzpatrick et al. (2010) also reported decreased HA use in children with mild hearing loss. They examined a population-based, retrospective chart review of 255 children with mild or unilateral hearing loss and found that less than two-thirds of those children wore amplification on a regular basis. An older study by Vesterager and Parving (1995) also found more frequent HA use (>8 hours per day) in children with severe hearing loss compared to mild hearing loss. In the present study, trends in HA use were not influenced by degree of hearing loss in the preschool-age group, whereas the school-age cohort did show such an effect. It is possible that there is less oversight for HA use as children with mild hearing loss enter elementary grades. It is also possible that school-age children with mild hearing loss (and their parents) may begin to identify situations in which they feel they do not need amplification, such as on the weekends, after school, or in social settings. It is unclear what effect limited HA use has on functional outcomes for school-age children with mild hearing loss or unilateral loss, given their significant amount of residual hearing. Future directions should address this gap in the research literature.
Limitations and Future Directions
Although this is the first paper to examine longitudinal trends in HA use in a large sample of CHH, there are several limitations that should be highlighted. Potentially, progression of hearing loss could be a factor that contributes to increased HA use, given the finding that poorer hearing relates to increased HA use (Munoz et al. 2014; Walker et al. 2013). We did not examine progression of hearing loss as a predictor of trends in HA use, however, due to the low number of children who demonstrated a significant decline in thresholds from the first to last visit. Dividing the low number of children with progressive hearing loss into age groups would further decrease statistical power and limit interpretability of results. Future studies could include a closer examination of children with progressive hearing loss, to determine trends in HA use within this specific population.
Another limitation is that the cluster analysis and logistic regression relied on parent report measures of HA use, rather than the objective information supplied by data logging, because the sample had an insufficient amount of data logging across all visits. This paper clearly demonstrates that most parents overestimate the amount of time their child wears HAs compared to data logging. Objective data logging measures would appear to be preferable when recording amount of daily HA use. Future research should incorporate data logging measures in investigations of longitudinal HA use, and whenever possible, audiologists and related professionals should rely on data logging as a measure of daily HA use.
A third limitation is that we are unable to ascertain the effects of intervention (e.g., audiology, speech-language pathology, early intervention) on HA use. We collected online surveys from the children’s managing audiologists, speech-language pathologists, and teachers of the deaf/hard of hearing, but we did not query the service providers about their general strategies with regards to HA compliance. We also did not contact children’s educational audiologists, who may have been able to provide additional information regarding HA compliance issues. Thus, we were unable to determine how intervention influences daily HA use, or how specific service providers may influence HA compliance in the pediatric population. Future research should address intervention strategies for counseling parents about HA use, particularly those families who are struggling with HA compliance.
Finally, a fourth limitation is that families in the OCHL study volunteered to participate in this longitudinal project. Like many longitudinal samples, this sample tended to be biased towards higher socioeconomic status and was not representative of income or educational status of the US population as a whole. This suggests the possibility that our findings of a strong effect of maternal education levels on longitudinal HA use actually underestimate these influences in the greater population. There remains a need for more research on alternative counseling and support strategies for families of diverse economic backgrounds, as the present findings suggest that current approaches may not be working well for less-advantaged families.
Summary
In 2007, the Joint Committee on Infant Hearing (2007) advocated for more research directed towards improving the effectiveness of intervention for children with hearing loss. One logical area of research is to identify malleable factors that may influence developmental outcomes. Malleable factors include any family- or child-specific variables that are amenable to change as part of intervention. In many previous studies, researchers focused on factors such as age at identification, age at amplification, or type of intervention. In this article, we focused on HA use time as a malleable factor, an issue that has received little attention in past research. Results indicated that the majority of CHH increase HA use over time, but a sizable minority remain limited users and some actually decrease usage over time. Family-specific variables influenced trends in longitudinal HA use in younger children (i.e., maternal education level) and child-specific variables influenced trends in longitudinal HA use in school-age children (i.e., degree of hearing loss). Another article in this monograph examines the influence of longitudinal HA use on language outcomes. As shown in this subsequent article (Tomblin et al. this issue, pp. xxxx), children with greater amounts of HA use achieve better developmental outcomes, due to enhanced cumulative linguistic experience.
Supplementary Material
Acknowledgments
Source of Funding: This research was supported by the following grants from the NIH-NIDCD: R01DC009560 and R01DC013591. The authors had full editorial control of this work and manuscript.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
See Supplemental Digital Content, Appendix A List of Acronyms used throughout Outcomes in Children with Hearing Loss Study.
References
- Ambrose SE, Walker EA, Berry LMU, Oleson JJ, Moeller MP. Quantity and Quality of Caregivers’ Linguistic Input to 18-month and 3-year-old Children who are Hard of Hearing. Ear and Hearing. doi: 10.1097/AUD.0000000000000209. in submission. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson KL, Goldstein H. Speech perception benefits of FM and infrared devices to children with hearing aids in a typical classroom. Language, Speech, and Hearing Services in Schools. 2004;35:169–184. doi: 10.1044/0161-1461(2004/017). [DOI] [PubMed] [Google Scholar]
- Benoit R. Home use of FM amplification systems during the early childhood years. Hearing Instruments. 1989;40:8–12. [Google Scholar]
- Ching TY, Dillon H, Marnane V, et al. Outcomes of Early-and Late-Identified Children at 3 Years of Age: Findings From a Prospective Population-Based Study. Ear and Hearing. 2013;34:535–552. doi: 10.1097/AUD.0b013e3182857718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Psychology Press; 1988. [Google Scholar]
- Crandell C. Noise effects on the speech recognition of children with minimal hearing loss. Ear and Hearing. 1993;7:210–217. doi: 10.1097/00003446-199306000-00008. [DOI] [PubMed] [Google Scholar]
- Davies MG, Yellon L, Purdy SC. Speech-in-noise perception of children using cochlear implants and FM systems. Australian and New Zealand Journal of Audiology. 2001;23:52–62. [Google Scholar]
- Davis J, Elfenbein JL, Schum RL, et al. Effects of mild and moderate hearing impairments on language, educational, and psychosocial behavior of children. Journal of Speech and Hearing Disorders. 1986;51:53–62. doi: 10.1044/jshd.5101.53. [DOI] [PubMed] [Google Scholar]
- Davis J, Shepard N, Stelmachowicz P, et al. Characteristics of hearing-impaired children in the public schools: part II--psychoeducational data. Journal of Speech and Hearing Disorders. 1981;46:130–137. doi: 10.1044/jshd.4602.130. [DOI] [PubMed] [Google Scholar]
- Desjardin JL. Maternal perceptions of self-efficacy and involvement in the auditory development of young children with prelingual deafness. Journal of Early Intervention. 2005;27:193–209. [Google Scholar]
- Eisenberg ME, Olson RE, Neumark-Sztainer D, et al. Correlations between family meals and psychosocial well-being among adolescents. Archives of Pediatrics & Adolescent Medicine. 2004;158:792–796. doi: 10.1001/archpedi.158.8.792. [DOI] [PubMed] [Google Scholar]
- Elfenbein JL, Hardin-Jones MA, Davis J. Oral communication skills of children who are hard of hearing. Journal of Speech, Language and Hearing Research. 1994;37:216–226. doi: 10.1044/jshr.3701.216. [DOI] [PubMed] [Google Scholar]
- Fenson L, Bates E, Dale P, Goodman J, Reznick JS, Thal D. Reply: Measuring variability in early child language: Don’t shoot the messenger. Child Development. 2000;71(2):323–328. doi: 10.1111/1467-8624.00147. [DOI] [PubMed] [Google Scholar]
- Finitzo-Hieber T, Tillman TW. Room acoustics effects on monosyllabic word discrimination ability for normal and hearing-impaired children. Journal of Speech, Language, and Hearing Research. 1978;21:440–458. doi: 10.1044/jshr.2103.440. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick EM, Crawford L, Ni A, et al. A descriptive analysis of language and speech skills in 4-to 5-yr-old children with hearing loss. Ear and Hearing. 2011;32:605–616. doi: 10.1097/AUD.0b013e31821348ae. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick EM, Durieux-Smith A, Whittingham J. Clinical practice for children with mild bilateral and unilateral hearing loss. Ear and Hearing. 2010;31(3):392–400. doi: 10.1097/AUD.0b013e3181cdb2b9. [DOI] [PubMed] [Google Scholar]
- Flexer C. Individual and Sound-Field FM Systems: Rationale, Description, and Use. Volta Review. 1997;99:133–162. [Google Scholar]
- Joint Committee on Infant Hearing. Year 2007 position statement: principles and guidelines for early hearing detection and intervention programs. Pediatrics. 2007;120:898–921. doi: 10.1542/peds.2007-2333. [DOI] [PubMed] [Google Scholar]
- Iglowstein I, Jenni OG, Molinari L, et al. Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics. 2003;111:302–307. doi: 10.1542/peds.111.2.302. [DOI] [PubMed] [Google Scholar]
- Jones C, Launer S. Pediatric fittings in 2010: The Sound Foundations Cuper project. In: Seewald RC, Bamford JM, editors. A Sound Foundation through Early Amplification: Proceedings of the 2010 International Conference. Chicago, IL: Phonak AG; 2011. pp. 187–192. [Google Scholar]
- Jones C, Feilner M. A Sound Foundation through Early Amplification: Proceedings of the 2013 International Conference. Chicago, IL: Phonak AG; 2013. What do we know about the fitting and daily life usage of hearing instruments in pediatrics? pp. 97–103. [Google Scholar]
- Koehlinger KM, Van Horne AJO, Moeller MP. Grammatical outcomes of 3-and 6-year-old children who are hard of hearing. Journal of Speech, Language, and Hearing Research. 2013;56:1701–1714. doi: 10.1044/1092-4388(2013/12-0188). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marnane V, Ching TY. Hearing aid and cochlear implant use in children with hearing loss at three years of age: Predictors of use and predictors of changes in use. International Journal of Audiology. 2015;(0):1–8. doi: 10.3109/14992027.2015.1017660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marttila TI, Karikoski JO. Hearing aid use in Finnish children—impact of hearing loss variables and detection delay. International Journal of Pediatric Otorhinolaryngology. 2006;70(3):475–480. doi: 10.1016/j.ijporl.2005.07.028. [DOI] [PubMed] [Google Scholar]
- McCreery RW, Bentler RA, Roush PA. Characteristics of hearing aid fittings in infants and young children. Ear and Hearing. 2012;34(6):701–710. doi: 10.1097/AUD.0b013e31828f1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCreery RW, Walker E, Spratford M, et al. Longitudinal predictors of aided speech audibility in infants and children. Ear and Hearing. doi: 10.1097/AUD.0000000000000211. in submission. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moeller MP, Donaghy KF, Beauchaine KL, et al. Longitudinal study of FM system use in nonacademic settings: Effects on language development. Ear and Hearing. 1996;17:28–41. doi: 10.1097/00003446-199602000-00004. [DOI] [PubMed] [Google Scholar]
- Moeller MP, Hoover B, Peterson B, et al. Consistency of hearing aid use in infants with early-identified hearing loss. American Journal of Audiology. 2009;18:14–23. doi: 10.1044/1059-0889(2008/08-0010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz K, Olson WA, Twohig MP, Preston E, Blaiser K, White KR. Pediatric Hearing Aid Use: Parent-Reported Challenges. Ear and Hearing. 2015;36:279–287. doi: 10.1097/AUD.0000000000000111. [DOI] [PubMed] [Google Scholar]
- Munoz K, Preston E, Hicken S. Pediatric hearing aid use: How can audiologists support parents to increase consistency? Journal of the American Academy of Audiology. 2014;25(4):380–387. doi: 10.3766/jaaa.25.4.9. [DOI] [PubMed] [Google Scholar]
- Nábělek AK, Pickett J. Reception of consonants in a classroom as affected by monaural and binaural listening, noise, reverberation, and hearing aids. The Journal of the Acoustical Society of America. 2005;56:628–639. doi: 10.1121/1.1903301. [DOI] [PubMed] [Google Scholar]
- Schafer EC, Thibodeau LM. Speech recognition in noise in children with cochlear implants while listening in bilateral, bimodal, and FM-system arrangements. American Journal of Audiology. 2006;15:114–126. doi: 10.1044/1059-0889(2006/015). [DOI] [PubMed] [Google Scholar]
- Sininger YS, Grimes A, Christensen E. Auditory development in early amplified children: Factors influencing auditory-based communication outcomes in children with hearing loss. Ear and Hearing. 2010;31:166–185. doi: 10.1097/AUD.0b013e3181c8e7b6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stiles DJ, Bentler RA, McGregor KK. The speech intelligibility index and the pure-tone average as predictors of lexical ability in children fit with hearing aids. Journal of Speech, Language, and Hearing Research. 2012;55:764–778. doi: 10.1044/1092-4388(2011/10-0264). [DOI] [PubMed] [Google Scholar]
- Tomblin JB, Harrison M, Ambrose SE, Walker EA, Oleson JJ, Moeller MP. Language outcomes in young children with mild to severe hearing loss. Ear and Hearing. doi: 10.1097/AUD.0000000000000219. in submission. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomblin JB, Walker EA, McCreery RW, Arenas RM, Harrison M, Moeller MP. Outcomes of children with hearing loss: Data collection and methods. Ear and Hearing. doi: 10.1097/AUD.0000000000000212. this volume, XXXX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomblin JB, Oleson JJ, Ambrose SE, et al. The Influence of Hearing Aids on the Speech and Language Development of Children with Hearing Loss. JAMA Otolaryngology - Head & Neck Surgery. 2014;140:43–49. doi: 10.1001/jamaoto.2014.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vesterager V, Parving A. Rehabilitation of hearing-impaired children: Intervention and outcome. International Journal of Audiology. 1995;34(4):207–217. doi: 10.3109/00206099509071913. [DOI] [PubMed] [Google Scholar]
- Walker EA, Spratford M, Moeller MP, et al. Predictors of hearing aid use time in children with mild-to-severe hearing loss. Language, Speech, and Hearing Services in Schools. 2013;44:73–88. doi: 10.1044/0161-1461(2012/12-0005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward JH., Jr Hierarchical grouping to optimize an objective function. Journal of the American Statistical Association. 1963;58:236–244. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.