Abstract
Primary mediastinal liposarcomas are extremely rare. They are primarily diseases of adults; however, they may be encountered in children. They are characterized by their large size and variable histologic subtypes, which correlate with clinical behavior and prognosis. Although the overall prognosis is poor, it is dependent upon the histologic subtype and completeness of surgical excision. Herein we present a case of a primary mediastinal pleomorphic liposarcoma in a 49-year-old male who received an en-bloc resection and superior vena cava replacement with Gortex graft. The patient has been disease-free after surgery for over 14 months.
Keywords: Primary mediastinal liposarcoma, superior vena cava graft, superior vena cava syndrome
Introduction
Primary mediastinal liposarcomas are extremely rare. The clinical manifestations are usually nonspecific at the early stage; however, the tumors are prone to rapid growth and can cause related symptoms by directly invading or compressing surrounding tissues and organs. We present a case of a primary mediastinal pleomorphic liposarcoma in a 49-year-old male who received an en-bloc resection and superior vena cava replacement with Gortex graft.
Case report
A 49-year-old Chinese male was admitted to our hospital with the chief complaints of an irritating dry cough and dyspnea. A large mediastinal mass was found on computed tomography (CT). No other symptoms were present, such as chest pain, fever, wheezing, hemoptysis, or superior vena cava syndrome. He had no smoking history and no family history of cancer. A review of systems was non-contributory and physical examination was unremarkable. On admission, peripheral blood count, serum chemistry, and urinalysis were normal.
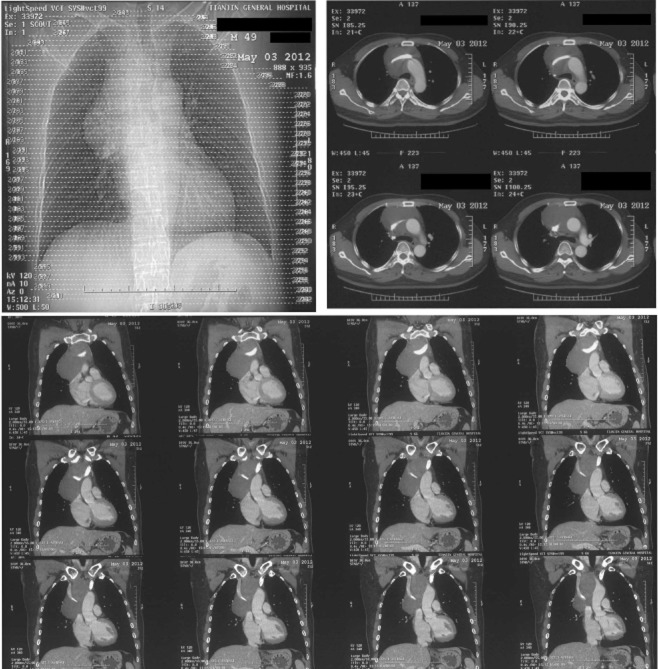
An enhanced chest CT scan revealed a huge mass in the superior mediastinum involving the superior vena cava, and its density was compatible with fat. Three-dimensional reconstruction of chest enhanced CT showed encroachment on the superior vena cava, as well as the left and right innominate veins (Fig. 1). Abdominal enhanced CT, brain enhanced magnetic resonance imaging (MRI) scan and bronchoscopy were all normal.
Figure 1.
Enhanced chest computed tomography scan revealed a huge fatty mass in the superior mediastinum involving the superior vena cava. Three-dimensional reconstruction showed encroachment on the superior vena cava, as well as the left and right innominate veins.
Surgical removal of the mass was planned on 16 May 2012. After establishment of a venous bypass between the right internal jugular vein and the right femoral vein, surgical exploration was performed through a standard median sternotomy under general anesthesia in order to better expose the mass and giant mediastinal veins. There was a huge tumor (10 × 8 × 7 cm3) located in the superior mediastinum encompassing the superior vena cava, as well as the left and right innominate veins. The right phrenic nerve was also invaded by the tumor. The tumor was removed en-bloc together with the superior vena cava, the left and right innominate veins, and mediastinal lymph nodes. Reconstructions of the left innominate vein up to the right auricle and the right innominate vein up to superior vena cava with Gortex grafts were performed.
Within the soft, irregular resected specimen, two nodules were found, measuring 5.5 × 4 × 2.5 cm3and 6.3 × 5.5 × 5 cm3. The cut surface of the tumor showed a multilobular and encapsulated yellow and gray appearance; the final histological diagnosis was pleomorphic liposarcoma (Fig. 2).
Figure 2.
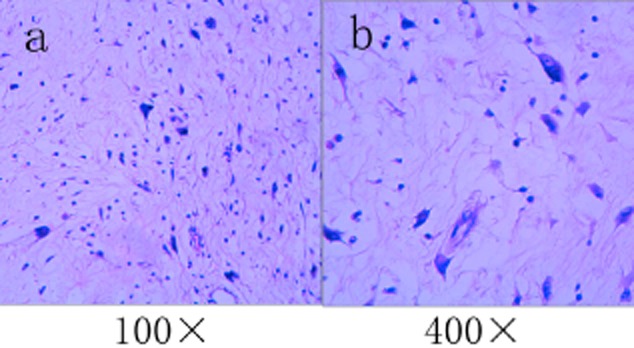
Hematoxylin and eosin stained slides show a pleomorphic liposarcoma with a variable number of pleomorphic lipoblasts and a lack of a low-grade precursor.
The postoperative course was uneventful and warfarin was prescribed for anticoagulation. A total of 60 Gy mediastinal dose was given as adjuvant therapy three months postoperatively. The patient is now over 14 months postoperative and he has no evidence of local recurrence or distal metastases.
Discussion
Primary mediastinal liposarcomas, first mentioned in the literature in 1939, are extremely rare, with less than 200 cases reported worldwide to date.1–4Liposarcomas usually arise in the lower extremities or retroperitoneum, and two thirds of these discovered in the mediastinum are secondary involvement as a result of metastases or direct extension from retroperitoneal tumors.4–6The time interval between the first presentation and mediastinal metastases is reported to range from seven to 25 years.7Primary mediastinal liposarcomas account for only 1–2% of all liposarcomas.4,8,9Although liposarcomas are the most common subtypes of sarcoma in the mediastinum, particularly in the anterior mediastinum, they comprise less than 1% of all mediastinal tumors.10,11
Primary mediastinal liposarcomas are hypothesized to arise within the adipose tissue of the adult thymus. Hahn et al.10found an admixture of liposarcomas and thymic tissue or an attenuated rim of thymic tissue around the tumor mass in hematoxylin and eosin (H&E) slides, which were suggestive of a thymic origin of these tumors. From operative and microscopic findings, other authors also support this hypothesis.12–14However, this location, which is based on speculation, is subject to controversy because almost half of the primary mediastinal liposarcomas locate in the posterior mediastinum.15,16In addition, in some cases they were assumed to originate from the pericardium.17–20Therefore, rather than originating from adipose tissue of the thymus, these tumors may originate from primitive mesenchymal cells, which have the property of lipogenesis, anywhere in the mediastinum.18,21
Similar to liposarcomas of the extremities and retroperitoneum, the age range of patients at the time of diagnosis ranges between 20 and 70 years, with a peak in the fifth decade.10,22Although mediastinal liposarcoma is primarily a disease of adults, it may also occur in young adults and children.23–25Hahn and Fletcher10reported a case in a three-year-old child. In our case, the patient was 49 years of age at diagnosis.
The clinical manifestations of mediastinal liposarcomas are usually nonspecific. The main manifestations include asthenia, cough, chest pain, and weight loss. Furthermore, 15% of them are asymptomatic and are discovered on routine chest radiography.16They can grow quite rapidly and reach a considerable size in a relatively short time. One patient was reported to have a giant mediastinal liposarcoma that measured 21.0 cm × 17.0 cm × 15.0 cm and weighed 2430 g. However, he was asymptomatic until three weeks before surgery and his CT scan was negative six months earlier.7By directly invading or compressing surrounding structures, such as the heart, trachea, and esophagus, the tumor can produce symptoms, such as arrhythmia, dyspnea, tachypnea, and dysphagia. When the superior vena cava is invaded, patients may present with signs of superior vena cava obstruction.26In our case, the patient presented with some nonspecific symptoms, such as cough and mild dyspnea. Although the superior vena cava was engulfed in tumor and narrowed, he had no signs of a superior vena cava syndrome.
The predominant finding of mediastinal liposarcomas on conventional chest radiography is a widened mediastinum. On enhanced CT scan, liposarcomas appear as nonhomogeneous fatty masses that vary in appearance depending on the amount of soft tissue and fibrous bands in the tumor. More solid components may be present and enhance with contrast material injection. Surrounding structures may be infiltrated or displaced.26MRI T1-weighted images show fatty tissue with high signal intensity, whereas the signal intensity diminishes in T2-weighted images. An enhanced MRI is better than an enhanced CT scan in its capacity to differentiate tumor subtypes and rule out invasion of vessels in the mediastinum and thoracic inlet.18,27,28A CT-guided fine-needle aspiration biopsy permits a preoperative determination of the histologic type of the tumor.29–31The identification of lipoblasts in the biopsy specimen is the key to the correct diagnosis.32
The World Health Organization classification of soft tissue tumors recognizes five categories of liposarcomas: (i) well-differentiated liposarcoma/atypical lipomatous tumor; (ii) dedifferentiated liposarcoma; (iii) myxoid liposarcoma; (iv) pleomorphic liposarcoma; and (v) mixed-type liposarcoma. Well-differentiated liposarcomas and dedifferentiated liposarcomas share the same cytogenetic and molecular genetic alterations, including a supernumerary ring and giant marker chromosomes containing amplified sequences of chromosome region 12q13-15, including genes such as MDM2, CDK4 and CPM.33–36Conventional and high-grade myxoid liposarcomas are characterized genetically in approximately 95% of cases by t(12;16)(q13;p11), resulting in the formation of the FUS-DDIT3 (CHOP) fusion gene, with roughly 5% of cases showing the variant t(12;22)(q13;q12), forming an EWSR1-DDIT3 fusion gene.37,38Pleomorphic liposarcoma, the least common liposarcoma subtype, is a high-grade, pleomorphic sarcoma containing a variable number of pleomorphic lipoblasts and lacking a low-grade precursor.9,39Pleomorphic liposarcomas contain complex numerical and structural chromosomal abnormalities, similar to other high-grade pleomorphic sarcomas.40Based on these advances in molecular genetics, liposarcomas can be classified into three main histogenetic subtypes: well-differentiated/dedifferentiated liposarcomas, myxoid liposarcomas, and pleomorphic liposarcomas.
Histopathologic characteristics are the main prognostic factor. The survival in patients with myxoid or pleomorphic liposarcomas is significantly shorter than that of patients with dedifferentiated or well-differentiated liposarcomas. Boland et al.4re-reviewed all available prior reports and found that death from the disease was reported in 11 of 39 (28%) and seven of 23 (30%) patients with well-differentiated and dedifferentiated liposarcomas, respectively, in contrast to 16 of 28 (57%) and 17 of 25 (68%) patients with myxoid liposarcomas and pleomorphic liposarcomas, respectively. Hirai et al.21reviewed the Japanese literature for surgical cases of primary liposarcoma of the mediastinum and found 15 cases. All eight patients (100%) with the well-differentiated type were alive after a mean interval of 35 months, including two of eight patients (25%) that had local recurrence. Conversely, two of five patients (40%) with the myxoid type were alive after a mean interval of 13 months and three of five patients (60%) died after a mean interval of 26 months. Pleomorphic liposarcomas were not found in this series. In Hahn et al.'s series of 24 cases, four pleomorphic liposarcomas were reported and disease recurrence was quite rapid, with a mean interval of three months.10
Surgical removal is considered to be the gold standard in the treatment of primary mediastinal liposarcomas, as well as other sites.16,41A standard median sternotomy and posterolateral thoracotomy are the most common surgical approach. A hemi-clamshell incision and percutaneous cardiopulmonary support may be needed in some cases.42,43A thoracoscopic approach has also been used recently for exploration and surgical excision of large mediastinal liposarcomas.17The difficulty in achieving complete and curative removal of the tumor lies in its relationship to neighboring structures. In order to obtain a complete removal of the tumor, adjacent organs, such as the superior vena cava and phrenic nerve, must be removed, as in our patient. If the entire tumor cannot be resected, surgical debulking often results in symptomatic relief.44Radiation therapy is often added as an adjunct to partial resection and may result in long-term survival of five years.45However, liposarcoma appears to have a very low sensitivity to radiotherapy and chemotherapy.44,46Intraoperative radiofrequency ablation is also tested in patients who are not well suited to undergo a further surgical resection; this procedure has proven to be safe and effective.47
The overall prognosis for patients with mediastinal liposarcomas is poor because of late tumor detection, involvement of vital structures, and inability to achieve complete resection.4Kiyama et al.48reviewed 21 cases in the Japanese literature and reported that the overall five-year survival rate was 38.1%. Approximately 40% of mediastinal liposarcomas recur after surgery and multiple successive recurrences are common.10However these patients can benefit from repeated resection of recurrent tumors, and surgery should always be considered as the appropriate management for these patients.19,20,49,50In our case, because the final pathologic diagnosis was a pleomorphic liposarcoma, which is a high grade sarcoma that has a tendency to recur and metastasize, the patient was recommended to receive a routine dose radiotherapy (200 cGy × 30) three months after hospital discharge to enhance therapeutic effects and diminish the possibility of tumor recurrence. The patient is now almost 14 months postoperative and no evidence of tumor recurrence or metastasis is present. Because there may be an interval of several years between resection and recurrence, close and long-term follow-up is strongly recommended in these patients with mediastinal liposarcomas.50
Acknowledgments
The patient granted written informed consent for publication of this manuscript and the accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal. This work was supported in part by grants by the Science and Technology Support Key Program of Tianjin (12ZCDZSY16100) and the Ministry of Education for New Century Excellent Talents (NCET-10-0956). Funding sources had no role in study design, data collection, and analysis; in decision to publish; or in preparation of the manuscript.
Disclosure
No authors report any conflict of interest.
Reference
- Kozonis MC, Wiggers RF, Golden HM. Primary liposarcoma of the mediastinum. Ann Intern Med. 1951;35:703–710. doi: 10.7326/0003-4819-35-3-703. [DOI] [PubMed] [Google Scholar]
- Raghavan R, Raghuram P, Parekh PV, Kurien JM. Posterior mediastinal liposarcoma simulating a lung mass: an unusual case report. Cancer Imaging. 2007;7:141–144. doi: 10.1102/1470-7330.2007.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu LG, Wei X, Pan TC. A giant primary myxoid liposarcoma of the posterior mediastinum. Chin Med J. 2010;123:1818–1820. [PubMed] [Google Scholar]
- Boland JM, Colby TV, Folpe AL. Liposarcomas of the mediastinum and thorax: a clinicopathologic and molecular cytogenetic study of 24 cases, emphasizing unusual and diverse histologic features. Am J Surg Pathol. 2012;36:1395–1403. doi: 10.1097/PAS.0b013e3182562bc1. [DOI] [PubMed] [Google Scholar]
- McLean TR, Almassi GH, Hackbarth DA, Janjan NA, Potish RA. Mediastinal involvement by myxoid liposarcoma. Ann Thorac Surg. 1989;47:920–921. doi: 10.1016/0003-4975(89)90038-6. [DOI] [PubMed] [Google Scholar]
- Alho A, Eeg Larsen T. A case of multifocal liposarcoma? Acta Orthop Scand. 1992;63:98–99. doi: 10.3109/17453679209154860. [DOI] [PubMed] [Google Scholar]
- Di Giammarco G, Di Mauro M, Pano M, et al. Giant metastatic myxoid liposarcoma of the mediastinum: a case report. J Thorac Cardiovasc Surg. 2005;129:1440–1442. doi: 10.1016/j.jtcvs.2005.01.010. [DOI] [PubMed] [Google Scholar]
- Burt M, Ihde JK, Hajdu SI, et al. Primary sarcomas of the mediastinum: results of therapy. J Thorac Cardiovasc Surg. 1998;115:671–680. doi: 10.1016/S0022-5223(98)70333-2. [DOI] [PubMed] [Google Scholar]
- Weiss SW, Goldblum JR. Enzinger and Weiss's Soft Tissue Tumors, 5th. Philadelphia, PA: Mosby/Elsevier; 2008. edition. [Google Scholar]
- Hahn HP, Fletcher CD. Primary mediastinal liposarcoma: clinicopathologic analysis of 24 cases. Am J Surg Pathol. 2007;31:1868–1874. doi: 10.1097/PAS.0b013e318093f925. [DOI] [PubMed] [Google Scholar]
- Marulli G, Rea F, Feltracco P, et al. Successful resection of a giant primary liposarcoma of the posterior mediastinum. J Thorac Oncol. 2007;2:453–455. doi: 10.1097/01.JTO.0000268681.10367.cf. [DOI] [PubMed] [Google Scholar]
- Sekine Y, Hamaguchi K, Miyahara Y, et al. Thymus-related liposarcoma: report of a case and review of the literature. Surg Today. 1996;26:203–207. doi: 10.1007/BF00311509. [DOI] [PubMed] [Google Scholar]
- Kashu Y, Yukumi S, Tsunooka N, et al. Successful resection of a massive mediastinal liposarcoma that rapidly extended into the entire left thoracic cavity: report of a case. Surg Today. 2012;42:68–71. doi: 10.1007/s00595-011-0013-8. [DOI] [PubMed] [Google Scholar]
- Klimstra DS, Moran CA, Perino G, Koss MN, Rosai J. Liposarcoma of the anterior mediastinum and thymus. A clinicopathologic study of 28 cases. Am J Surg Pathol. 1995;19:782–791. doi: 10.1097/00000478-199507000-00006. [DOI] [PubMed] [Google Scholar]
- Cicciarelli FE, Soule EH, McGoon DC. Lipoma and liposarcoma of the mediastinum: a report of 14 tumors including one lipoma of the thymus. J Thorac Cardiovasc Surg. 1964;47:411–429. [PubMed] [Google Scholar]
- Schweitzer DL, Aguam AS. Primary liposarcoma of the mediastinum. Report of a case and review of the literature. J Thorac Cardiovasc Surg. 1977;74:83–97. [PubMed] [Google Scholar]
- Decker JR, de Hoyos AL, Decamp MM. Successful thoracoscopic resection of a large mediastinal liposarcoma. Ann Thorac Surg. 2011;92:1499–1501. doi: 10.1016/j.athoracsur.2011.02.051. [DOI] [PubMed] [Google Scholar]
- Punpale A, Pramesh CS, Jambhekar N, Kadota E, Goto S, Kato M. Giant mediastinal liposarcoma: a case report. Ann Thorac Cardiovasc Surg. 2006;12:425–427. [PubMed] [Google Scholar]
- Noji T, Morikawa T, Kaji M, Ohtake S, Katoh H. Successful resection of a recurrent mediastinal liposarcoma invading the pericardium: report of a case. Surg Today. 2004;34:450–452. doi: 10.1007/s00595-003-2719-8. [DOI] [PubMed] [Google Scholar]
- Kendall SW, Williams EA, Hunt JB, Petch MC, Wells FC, Milstein BB. Recurrent primary liposarcoma of the pericardium: management by repeated resections. Ann Thorac Surg. 1993;56:560–562. doi: 10.1016/0003-4975(93)90900-3. [DOI] [PubMed] [Google Scholar]
- Hirai S, Hamanaka Y, Mitsui N, Uegami S, Matsuura Y. Surgical resection of primary liposarcoma of the anterior mediastinum. Ann Thorac Cardiovasc Surg. 2008;14:38–41. [PubMed] [Google Scholar]
- Enzinger FM, Winslow DJ. Liposarcoma. A study of 103 cases. Virchows Arch Pathol Anat Physiol Klin Med. 1962;335:367–388. [PubMed] [Google Scholar]
- Chiyo M, Fujisawa T, Yasukawa T, et al. Successful resection of a primary liposarcoma in the anterior mediastinum in a child: report of a case. Surg Today. 2001;31:230–232. doi: 10.1007/s005950170174. [DOI] [PubMed] [Google Scholar]
- Mikkilineni RS, Bhat S, Cheng AW, Prevosti LG. Liposarcoma of the posterior mediastinum in a child. Chest. 1994;106:1288–1289. doi: 10.1378/chest.106.4.1288. [DOI] [PubMed] [Google Scholar]
- Anand Rajan KD, Subbarao KC, Agarwala S, Gupta SD. Mediastinal liposarcoma of mixed type in childhood: a report of a case with unusual histologic features. Indian J Pathol Microbiol. 2010;53:525–528. doi: 10.4103/0377-4929.68297. [DOI] [PubMed] [Google Scholar]
- Munden RF, Nesbitt JC, Kemp BL, Chasen MH, Whitman GJ. Primary liposarcoma of the mediastinum. AJR Am J Roentgenol. 2000;175:1340. doi: 10.2214/ajr.175.5.1751340. [DOI] [PubMed] [Google Scholar]
- Jung JI, Kim H, Kang SW, Park SH. Radiological findings in myxoid liposarcoma of the anterior mediastinum. Br J Radiol. 1998;71:975–976. doi: 10.1259/bjr.71.849.10195015. [DOI] [PubMed] [Google Scholar]
- Jelinek JS, Kransdorf MJ, Shmookler BM, Aboulafia AJ, Malawer MM. Liposarcoma of the extremities: MR and CT findings in the histologic subtypes. Radiology. 1993;186:455–459. doi: 10.1148/radiology.186.2.8421750. [DOI] [PubMed] [Google Scholar]
- Attal H, Jensen J, Reyes CV. Myxoid liposarcoma of the anterior mediastinum. Diagnosis by fine needle aspiration biopsy. Acta Cytol. 1995;39:511–513. [PubMed] [Google Scholar]
- Alvarez-Sala R, Casadevall J, Caballero P, Prados C, Ortega B. Long-term survival in a surgically treated non-encapsulated mediastinal primary liposarcoma. Diagnostic utility of core-needle biopsy for mediastinal tumors. J Cardiovasc Surg (Torino) 1995;36:199–200. [PubMed] [Google Scholar]
- Munjal K, Pancholi V, Rege J, Munjal S, Bhandari V, Nahar R. Fine needle aspiration cytology in mediastinal myxoid liposarcoma: a case report. Acta Cytol. 2007;51:456–458. doi: 10.1159/000325766. [DOI] [PubMed] [Google Scholar]
- Romero-Guadarrama MB, Jiménez-Becerra S, Durán-Padilla MA, Santiago-Prieto AC, Cruz-Ortiz H, Novelo-Retana V. Mediastinal pleomorphic liposarcoma diagnosed by fine needle aspiration biopsy: a case report. Acta Cytol. 2007;51:440–442. doi: 10.1159/000325763. [DOI] [PubMed] [Google Scholar]
- Fletcher CD, Akerman M, Dal Cin P, et al. Correlation between clinicopathological features and karyotype in lipomatous tumors. A report of 178 cases from the Chromosomes and Morphology (CHAMP) Collaborative Study Group. Am J Pathol. 1996;148:623–630. [PMC free article] [PubMed] [Google Scholar]
- Mandahl N, Höglund M, Mertens F, et al. Cytogenetic aberrations in 188 benign and borderline adipose tissue tumors. Genes Chromosomes Cancer. 1994;9:207–215. doi: 10.1002/gcc.2870090309. [DOI] [PubMed] [Google Scholar]
- Pedeutour F, Forus A, Coindre JM, et al. Structure of the supernumerary ring and giant rod chromosomes in adipose tissue tumors. Genes Chromosomes Cancer. 1999;24:30–41. [PubMed] [Google Scholar]
- Pedeutour F, Suijkerbuijk RF, Van Gaal J, et al. Chromosome 12 origin in rings and giant markers in well-differentiated liposarcoma. Cancer Genet Cytogenet. 1993;66:133–134. doi: 10.1016/0165-4608(93)90245-h. [DOI] [PubMed] [Google Scholar]
- Turc-Carel C, Limon J, Dal Cin P, Rao U, Karakousis C, Sandberg AA. Cytogenetic studies of adipose tissue tumors. II. Recurrent reciprocal translocation t(12;16)(q13;p11) in myxoid liposarcomas. Cancer Genet Cytogenet. 1986;23:291–299. doi: 10.1016/0165-4608(86)90011-7. [DOI] [PubMed] [Google Scholar]
- Crozat A, Aman P, Mandahl N, Ron D. Fusion of CHOP to a novel RNA-binding protein in human myxoid liposarcoma. Nature. 1993;363:640–644. doi: 10.1038/363640a0. [DOI] [PubMed] [Google Scholar]
- Fletcher CD, Unni KK, Mertens F, editors. Pathology and Genetics of Tumors of Soft Tissue and Bone. Lyon: IARC Press; 2002. . eds. [Google Scholar]
- Idbaih A, Coindre JM, Derré J, et al. Myxoid malignant fibrous histiocytoma and pleomorphic liposarcoma share very similar genomic imbalances. Lab Invest. 2005;85:176–181. doi: 10.1038/labinvest.3700202. [DOI] [PubMed] [Google Scholar]
- Paquette M, Truong PT, Hart J, et al. Primary sarcoma of the mediastinum: a report of 16 cases referred to the British Columbia Cancer Agency. J Thorac Oncol. 2010;5:898–906. doi: 10.1097/jto.0b013e3181d8fe80. [DOI] [PubMed] [Google Scholar]
- Matsuo T, Takamori S, Hayabuchi N, et al. Giant liposarcoma occupying most of the hemi-thorax and resected in the supine position: report of a rare case. Kurume Med J. 2011;58:63–65. doi: 10.2739/kurumemedj.58.63. [DOI] [PubMed] [Google Scholar]
- Okuno M, Kawashima M, Miura K, Kadota E, Goto S, Kato M. Resection of giant mediastinal liposarcoma using the hemiclamshell incision. Gen Thorac Cardiovasc Surg. 2010;58:654–656. doi: 10.1007/s11748-010-0584-0. [DOI] [PubMed] [Google Scholar]
- Standerfer RJ, Armistead SH, Paneth M. Liposarcoma of the mediastinum: report of two cases and review of the literature. Thorax. 1981;36:693–694. doi: 10.1136/thx.36.9.693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grewal RG, Prager K, Austin JH, Rotterdam H. Long term survival in non-encapsulated primary liposarcoma of the mediastinum. Thorax. 1993;48:1276–1277. doi: 10.1136/thx.48.12.1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greif J, Marmor S, Merimsky O, Kovner F, Inbar M. Primary liposarcoma of the mediastinum. Sarcoma. 1998;2:205–207. doi: 10.1080/13577149877993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shoji F, Taketomi A, Yano T, Maehara Y. Intraoperative radiofrequency ablation in an open thoracotomy setting for the new treatment of mediastinal liposarcoma: report of a case. Surg Today. 2011;41:992–994. doi: 10.1007/s00595-010-4380-3. [DOI] [PubMed] [Google Scholar]
- Kiyama H, Tanabe S, Nagasawa S, Irie Y, Ohshima N, Yamada T. [A case of primary anterior mediastinal liposarcoma with a heterotopic mass in the pericardium of the same histology] Nihon Kyobu Geka Gakkai Zasshi. 1996;44:2191–2195. . (In Japanese.) [PubMed] [Google Scholar]
- Coulibaly B, Bouvier C, Payan MJ, Thomas P. Recurrent dedifferentiated liposarcoma of mediastinum involving lung and pleura. Interact Cardiovasc Thorac Surg. 2009;9:741–742. doi: 10.1510/icvts.2009.209494. [DOI] [PubMed] [Google Scholar]
- Chung C, Lu CC, Chang SC, Hsu WH, Perng RP. Mediastinal liposarcoma with local recurrence: a case report. Zhonghua Yi Xue Za Zhi (Taipei) 1996;57:70–73. [PubMed] [Google Scholar]