Abstract
Background
The National Central Cancer Registry of China (NCCR) is responsible for cancer surveillance. Local cancer registries in each province submit data for annual publication.. The incidence and mortality of esophageal cancer in China in 2010 by age, gender, and area is reported in this article.
Methods
There were data from 145 out of 219 qualified cancer registries. Esophageal cancer cases and deaths (ICD 10 code as C15) were stratified by location, gender, age, and cancer site. The 2000 Chinese census and Segi's population were used for age-standardized incidence/mortality rates. The rank in all cancer types and cumulative rate were also calculated.
Results
It was estimated that 287 632 new cases were diagnosed and 208 473 patients died from esophageal cancer in 2010 in China. Esophageal cancer incidence ranked fifth of all cancer types with a rate of 21.88/100 000. Age-standardized rates by Chinese population (CASR) and World population (WASR) for incidence and mortality were 16.71/100 000 and 16.97/100 000, respectively. The mortality of esophageal cancer ranked fourth in all cancer types with a rate of 15.85/100 000. The CASR and WASR for mortality were 11.95/100 000 and 12.02/100 000, respectively. For both incidence and mortality, the rates of esophageal cancer were much higher in men than that in women, in rural areas than in urban areas, and peaked at age 80–84.
Conclusions
Esophageal cancer is still a major cancer type in rural areas of China. Effective prevention and control should be emphasized, including health education, chemoprevention, and early detection in high-risk groups.
Keywords: Cancer registry, China, esophageal cancer, incidence, mortality
Introduction
Esophageal cancer is a major worldwide health problem with high rates of incidence and death, as well as considerable morbidity and the burden of treatment.1–10 In the developed world, the incidence of esophageal adenocarcinoma (EAC) has increased dramatically over the last 30 years and now outnumbers esophageal squamous cell cancer (ESC) in some countries. Esophageal cancer was the fifth most common cancer and the fourth leading cause of cancer death in all cancer types in China in 2010.11 Based on the population of cancer registration data from the National Central Cancer Registry of China, the incidence of esophageal cancer has been decreasing since the 1990s in both urban and rural areas in China. In 2009, esophageal cancer incidence was 22.14/100 000 and mortality was 16.77/100 000 in cancer registration areas, which covered 72 registries and 85.47 million of the population. In 2010, as a result of the National Program of Cancer Registration, the number of registries more than doubled compared to the previous year.
In this study, esophageal cancer data were retrieved from the national database and analysed, particularly the updated statistics on incidence rates and mortalities.
Material and methods
Data source
The National Central Cancer Registry (NCCR) of China collected cancer registration data from local cancer registries. All new cancer cases diagnosed in 2010 were reported to the cancer registries from hospitals, community health centers and medical insurance. The number of cancer deaths was obtained from vital statistics. Population information was collected from local statistic bureaus or household register departments in local public security bureaus.
Two hundred and nineteen cancer registries covering 31 provinces submitted cancer registration data to NCCR. The overall population coverage was 205.83 million, accounting for 15.5% of the national population of China. Data classified under invasive esophageal cancer (C15) by the International Classification of Diseases (ICD) for Oncology third edition, were retrieved from the overall cancer database and analyzed. After evaluation, there were 145 cancer registries that were qualified for inclusion in the study, including 63 cities and 82 counties covering 158 403 248 of the population, and accounting for 11.86% of the national population of China.
Quality control
Based on the Guideline of Chinese Cancer Registration and the standard of data inclusion in Cancer Incidence in Five Continents Volume IX, cancer registration data were evaluated by the quality indicators of proportion of morphological verification (MV%), percentage of cancer cases identified with death certification only (DCO%), and mortality to incidence ratio (M/I).12–14As the criteria of reception, an overall MV% of more than 55%, DCO% less than 20%, and M/I between 0.55–0.95 were considered reliable and acceptable.
The indicators of MV%, DCO%, and M/I ratio of 145 registries' pooled data for esophageal cancer were 76.68%, 2.31%, and 0.58 in all areas, respectively. The MV% was higher in rural areas than that in urban areas, but the MI ratio was lower in urban areas (Table 1).
Table 1.
Quality control index of esophageal cancer for 145 selected registries in China, in 2010
| Areas | Gender | M/I | MV% | DOC% | UB% |
|---|---|---|---|---|---|
| ALL | Both | 0.74 | 76.68 | 2.31 | 0.58 |
| Male | 0.74 | 76.88 | 2.45 | 0.56 | |
| Female | 0.75 | 76.21 | 1.97 | 0.65 | |
| Urban areas | Both | 0.76 | 74.65 | 2.11 | 0.89 |
| Male | 0.76 | 75.69 | 2.16 | 0.79 | |
| Female | 0.77 | 71.80 | 1.98 | 1.19 | |
| Rural areas | Both | 0.73 | 78.03 | 2.44 | 0.38 |
| Male | 0.72 | 77.73 | 2.66 | 0.39 | |
| Female | 0.74 | 78.65 | 1.96 | 0.35 | |
| Eastern areas | Both | 0.76 | 77.36 | 1.94 | 0.48 |
| Male | 0.75 | 77.77 | 1.94 | 0.46 | |
| Female | 0.78 | 76.36 | 1.93 | 0.52 | |
| Middle areas | Both | 0.69 | 78.11 | 2.75 | 0.45 |
| Male | 0.68 | 78.37 | 3.19 | 0.47 | |
| Female | 0.70 | 77.57 | 1.83 | 0.42 | |
| Western areas | Both | 0.74 | 68.33 | 3.70 | 1.64 |
| Male | 0.76 | 67.49 | 4.06 | 1.39 | |
| Female | 0.67 | 70.68 | 2.68 | 2.34 |
Statistical analysis
Incident cases and deaths of esophageal cancer from every cancer registry were pooled and stratified by urban/rural, area (Eastern, Middle, and Western in China), gender, and for 19 age groups (0-, 1–4, 5–9, …80–84, 85 + years). The age specific rate in each group and the national population in 2010 were used for the estimates of incidences and deaths. The 2000 China census and Segi's world population were applied for age-standardized rates. The cumulative risk of developing or dying from cancer before 75 years (in the absence of competing causes of death) was calculated and presented as a percentage. Software including MS-FoxPro, MS-Excel, IARCcrgTools issued by the International Agency for Research on Cancer were used for data checking. SAS software was used to sort and calculate.
Results
Incidence
It was estimated that 287 632 new cases were diagnosed as esophageal cancer in 2010 with an incidence rate of 21.88/100 000, accounting for 9.30% of overall new cancer cases in China. It ranked the fifth most common cancer, following cancers of the lung, stomach, female breast, and liver. The age-standardized incidence rates by China (CASIR) population and by World population (WASIR) were 16.71/100 000 and 16.97/100 000, respectively. Among the patients aged 0–74, the cumulative incidence rate was 2.15%.
The incident rate among men (204 449 new cases with an incidence rate of 30.38/100 000) remarkably higher than that in women (83 183 cases with 12.96/100 000). Urban areas had a lower incidence rate (109 683 and 16.55/100 000) than that in rural areas (177 949 and 27.29/100 000). Among the three regions, the Eastern region had the most new cases with the least in the Western region, however, the incidence rates were similar (Table 2).
Table 2.
Estimated esophageal cancer incidence by gender and area in China, 2010
| Areas | Gender | No. of cases | Crude rate (1/105) | Ratio (%) | ASRcn (1/105) | ASRwld (1/105) | Cumulative rate 0–74 (%) | TASR 35–64 (1/105) | Rank |
|---|---|---|---|---|---|---|---|---|---|
| ALL | Both | 287 632 | 21.88 | 9.30 | 16.71 | 16.97 | 2.15 | 26.62 | 5 |
| Male | 204 449 | 30.38 | 11.31 | 24.05 | 24.42 | 3.07 | 39.35 | 4 | |
| Female | 83 183 | 12.96 | 6.47 | 9.46 | 9.60 | 1.21 | 13.46 | 6 | |
| Urban areas | Both | 109 683 | 16.55 | 6.45 | 11.50 | 11.68 | 1.46 | 17.45 | 6 |
| Male | 81 167 | 23.92 | 8.32 | 17.31 | 17.58 | 2.18 | 27.45 | 5 | |
| Female | 28 516 | 8.81 | 3.94 | 5.76 | 5.83 | 0.72 | 7.03 | 7 | |
| Rural areas | Both | 177 949 | 27.29 | 12.77 | 23.10 | 23.49 | 3.01 | 37.39 | 4 |
| Male | 123 282 | 36.95 | 14.81 | 32.40 | 32.96 | 4.21 | 53.47 | 4 | |
| Female | 54 667 | 17.17 | 9.74 | 13.97 | 14.21 | 1.82 | 20.96 | 4 | |
| Eastern areas | Both | 116 152 | 21.12 | 9.04 | 15.93 | 16.19 | 2.07 | 24.59 | 6 |
| Male | 81 942 | 29.11 | 11.23 | 22.94 | 23.36 | 2.96 | 37.11 | 4 | |
| Female | 34 210 | 12.74 | 6.16 | 9.05 | 9.15 | 1.17 | 11.68 | 5 | |
| Middle areas | Both | 93 298 | 22.08 | 9.26 | 16.94 | 17.17 | 2.18 | 26.65 | 5 |
| Male | 64 502 | 29.92 | 11.08 | 23.66 | 23.96 | 3.02 | 37.57 | 4 | |
| Female | 28 796 | 13.92 | 6.77 | 10.32 | 10.45 | 1.32 | 15.38 | 7 | |
| Western areas | Both | 78 182 | 22.83 | 9.77 | 17.70 | 18.01 | 2.26 | 29.99 | 5 |
| Male | 58 005 | 32.97 | 11.69 | 26.35 | 26.74 | 3.33 | 45.36 | 4 | |
| Female | 20 177 | 12.12 | 6.63 | 9.03 | 9.26 | 1.17 | 13.95 | 6 |
ASRcn, Age-standardised rate (China standard population, 2000); ASRwld, Age-standardised rate (World standard population); TASR, Truncated age-standardised rate (World standard population).
Age-specific incidence rates of esophageal cancer were relatively low in subjects under 55 years of age and dramatically increased after 55 years of age, reaching a peak for subjects 80–84 years old (143.65/100 000). This trend was observed in men, however, in women the highest incidence rate occurred in the age group 75–79 years. In general, age specific incidence rates were significantly higher in men than that in women and lower in urban than that in rural areas (Table 3, Fig 1).
Table 3.
Age-specific incidence rates of esophageal cancer in China, 2010 (1/105)
| Age group | All areas | Urban | Rural | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Both | Male | Female | Both | Male | Female | Both | Male | Female | |
| All | 21.88 | 30.38 | 12.96 | 16.55 | 23.92 | 8.81 | 27.29 | 36.95 | 17.17 |
| 0– | 0.04 | 0.08 | 0.00 | 0.07 | 0.13 | 0.00 | 0.00 | 0.00 | 0.00 |
| 1– | 0.01 | 0.02 | 0.00 | 0.02 | 0.03 | 0.00 | 0.00 | 0.00 | 0.00 |
| 5– | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 10– | 0.03 | 0.05 | 0.00 | 0.00 | 0.00 | 0.00 | 0.06 | 0.11 | 0.00 |
| 15– | 0.02 | 0.04 | 0.00 | 0.00 | 0.00 | 0.00 | 0.03 | 0.07 | 0.00 |
| 20– | 0.05 | 0.02 | 0.08 | 0.07 | 0.00 | 0.15 | 0.03 | 0.03 | 0.03 |
| 25– | 0.20 | 0.30 | 0.10 | 0.18 | 0.35 | 0.00 | 0.22 | 0.26 | 0.18 |
| 30– | 0.35 | 0.37 | 0.33 | 0.28 | 0.26 | 0.30 | 0.41 | 0.46 | 0.35 |
| 35– | 1.41 | 2.16 | 0.63 | 0.85 | 1.36 | 0.32 | 1.88 | 2.82 | 0.89 |
| 40– | 5.01 | 7.38 | 2.54 | 3.15 | 4.63 | 1.63 | 6.83 | 10.03 | 3.45 |
| 45– | 12.34 | 19.39 | 5.04 | 8.33 | 14.03 | 2.60 | 16.33 | 24.56 | 7.53 |
| 50– | 28.30 | 42.92 | 12.94 | 18.19 | 30.39 | 5.42 | 38.76 | 55.84 | 20.75 |
| 55– | 53.96 | 80.02 | 27.37 | 34.34 | 54.01 | 13.98 | 77.48 | 111.69 | 43.16 |
| 60– | 88.86 | 127.89 | 48.48 | 59.67 | 90.68 | 26.89 | 126.31 | 176.81 | 75.50 |
| 65– | 109.88 | 153.88 | 65.04 | 77.19 | 110.72 | 42.00 | 153.37 | 213.32 | 94.65 |
| 70– | 130.10 | 180.36 | 80.40 | 90.26 | 129.11 | 50.86 | 180.39 | 246.90 | 116.65 |
| 75– | 142.29 | 197.55 | 92.79 | 102.74 | 149.33 | 61.80 | 193.32 | 258.33 | 133.61 |
| 80– | 143.65 | 212.41 | 89.19 | 110.57 | 166.25 | 69.03 | 188.03 | 269.76 | 117.97 |
| 85– | 125.21 | 180.61 | 92.05 | 105.19 | 158.19 | 75.38 | 152.20 | 208.23 | 115.77 |
Figure 1.
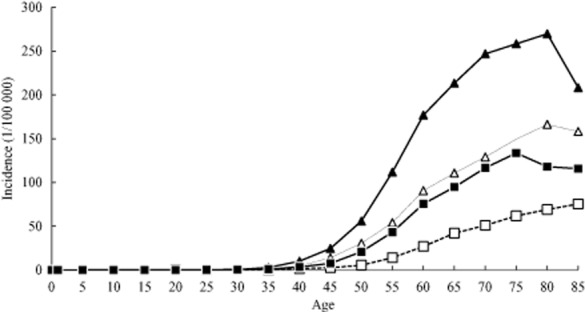
Age-specific incidence rate of esophageal cancer in China, 2010 (1/105).  , urban male;
, urban male;  , urban female;
, urban female;  , rural male;
, rural male;  , rural female.
, rural female.
Mortality
Nearly 208 473 patients died of esophageal cancer in 2010 in China with a mortality rate of 15.85/100 000, accounting for 10.65% of overall cancer deaths. It ranked the fourth most fatal cancer following cancers of the lung, liver, and stomach. The age-standardized mortality rates by China (CASMR) population and by World population (WASMR) were 11.95/100 000 and 12.02/100 000, respectively. Among the patients aged 0–74, the cumulative mortality rate was 1.44%.
As with the incidence rate, esophageal cancer deaths were much higher in men (148 865 deaths with mortality of 22.12/100 000) than that in women (59 608 deaths and 9.29/100 000). Urban areas experienced lower mortality (80 798 and 12.19/100 000) than that of rural areas (127 675 and 19.58/100 000). Among the three regions, the Eastern had the most deaths, with the least in Western region, however, the Western region had the highest mortality (Table 4).
Table 4.
Estimated esophageal cancer mortality by gender and area in China, 2010
| Areas | Gender | No. of cases | Crude rate (1/105) | Ratio (%) | ASRcn (1/105) | ASRwld (1/105) | Cumulative rate 0–74 (%) | TASR 35–64 (1/105) | Rank |
|---|---|---|---|---|---|---|---|---|---|
| ALL | Both | 208 473 | 15.85 | 10.65 | 11.95 | 12.02 | 1.44 | 15.31 | 4 |
| Male | 148 865 | 22.12 | 11.87 | 17.54 | 17.69 | 2.11 | 23.61 | 4 | |
| Female | 59 608 | 9.29 | 8.49 | 6.52 | 6.53 | 0.75 | 6.74 | 4 | |
| Urban areas | Both | 80 798 | 12.19 | 7.81 | 8.35 | 8.44 | 1.01 | 10.27 | 5 |
| Male | 60 544 | 17.84 | 9.27 | 12.90 | 13.10 | 1.57 | 17.01 | 4 | |
| Female | 20 254 | 6.26 | 5.31 | 3.90 | 3.90 | 0.44 | 3.25 | 6 | |
| Rural areas | Both | 127 675 | 19.58 | 13.85 | 16.43 | 16.48 | 1.96 | 21.23 | 4 |
| Male | 88 321 | 26.47 | 14.70 | 23.30 | 23.41 | 2.80 | 31.43 | 4 | |
| Female | 39 354 | 12.36 | 12.27 | 9.79 | 9.81 | 1.13 | 10.81 | 4 | |
| Eastern areas | Both | 86 549 | 15.74 | 10.59 | 11.62 | 11.67 | 1.40 | 14.20 | 4 |
| Male | 60 538 | 21.51 | 11.75 | 16.90 | 17.01 | 2.03 | 22.19 | 4 | |
| Female | 26 011 | 9.69 | 8.60 | 6.56 | 6.55 | 0.76 | 5.96 | 4 | |
| Middle areas | Both | 63 549 | 15.04 | 10.34 | 11.43 | 11.42 | 1.30 | 13.75 | 4 |
| Male | 43 932 | 20.38 | 11.15 | 16.26 | 16.31 | 1.86 | 20.20 | 4 | |
| Female | 19 617 | 9.48 | 8.90 | 6.77 | 6.73 | 0.74 | 7.11 | 4 | |
| Western areas | Both | 58 375 | 17.05 | 11.13 | 13.12 | 13.33 | 1.66 | 19.18 | 4 |
| Male | 44 395 | 25.24 | 12.86 | 20.14 | 20.46 | 2.54 | 30.31 | 4 | |
| Female | 13 980 | 8.40 | 7.80 | 6.13 | 6.23 | 0.76 | 7.58 | 6 |
ASRcn, Age-standardised rate (China standard population, 2000); ASRwld, Age-standardised rate (World standard population); TASR, Truncated age-standardised rate (World standard population).
Age-specific mortalities of esophageal cancer were relatively low in subjects under 50 years of age and dramatically increased after 50 years of age, reaching a peak for subjects in the oldest age group (85 years and over) in all areas, urban and rural women. However, the highest mortalities were observed in the age group of 80–84 in rural both genders, and rural men. Age specific mortalities were significantly higher in men than that in women and lower in urban than that in rural areas (Table 5, Fig 2).
Table 5.
Age-specific mortality of esophageal cancer in China, 2010 (1/105)
| Age group | All areas | Urban | Rural | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Both | Male | Female | Both | Male | Female | Both | Male | Female | |
| All | 15.85 | 22.12 | 9.29 | 12.19 | 17.84 | 6.26 | 19.58 | 26.47 | 12.36 |
| 0– | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 1– | 0.01 | 0.00 | 0.03 | 0.00 | 0.00 | 0.00 | 0.03 | 0.00 | 0.07 |
| 5– | 0.04 | 0.00 | 0.08 | 0.00 | 0.00 | 0.00 | 0.09 | 0.00 | 0.19 |
| 10– | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 15– | 0.01 | 0.02 | 0.00 | 0.00 | 0.00 | 0.00 | 0.02 | 0.03 | 0.00 |
| 20– | 0.01 | 0.02 | 0.00 | 0.01 | 0.01 | 0.00 | 0.02 | 0.03 | 0.00 |
| 25– | 0.14 | 0.20 | 0.07 | 0.18 | 0.29 | 0.07 | 0.10 | 0.13 | 0.07 |
| 30– | 0.27 | 0.29 | 0.26 | 0.20 | 0.25 | 0.14 | 0.33 | 0.32 | 0.35 |
| 35– | 0.97 | 1.53 | 0.39 | 0.55 | 0.80 | 0.30 | 1.32 | 2.14 | 0.47 |
| 40– | 2.43 | 3.78 | 1.01 | 1.45 | 2.49 | 0.39 | 3.38 | 5.03 | 1.64 |
| 45– | 6.99 | 11.66 | 2.15 | 4.52 | 8.12 | 0.90 | 9.45 | 15.09 | 3.43 |
| 50– | 15.53 | 24.60 | 6.00 | 10.27 | 18.21 | 1.96 | 20.97 | 31.19 | 10.20 |
| 55– | 31.60 | 49.23 | 13.60 | 21.63 | 35.91 | 6.84 | 43.55 | 65.45 | 21.57 |
| 60– | 52.08 | 77.50 | 25.77 | 35.34 | 56.00 | 13.50 | 73.56 | 105.77 | 41.14 |
| 65– | 75.48 | 111.04 | 39.25 | 59.88 | 91.13 | 27.08 | 96.24 | 138.45 | 54.89 |
| 70– | 101.75 | 142.04 | 61.89 | 68.85 | 100.15 | 37.10 | 143.27 | 196.44 | 92.31 |
| 75– | 132.58 | 184.00 | 86.52 | 87.82 | 127.91 | 52.59 | 190.33 | 254.68 | 131.22 |
| 80– | 160.84 | 227.27 | 108.23 | 111.83 | 160.43 | 75.56 | 226.60 | 310.31 | 154.84 |
| 85– | 162.44 | 237.23 | 117.67 | 124.12 | 194.81 | 84.37 | 214.09 | 289.47 | 165.08 |
Figure 2.
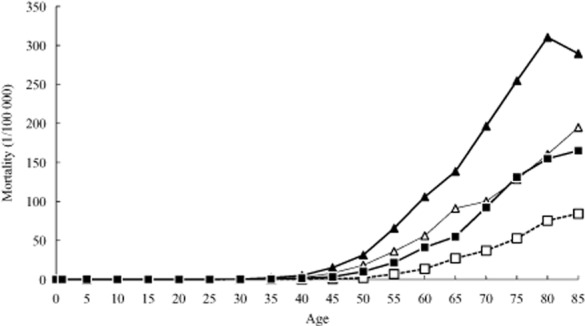
Age-specific mortality of esophageal cancer in China, 2010 (1/105).  , urban male;
, urban male;  , urban female;
, urban female;  , rural male;
, rural male;  , rural female.
, rural female.
Discussion
NCCR has published cancer statistics in cancer registration areas in China since 2005.15–17 In 2010, 219 registries submitted cancer registration data to NCCR under the requirement of the National Program. This data coverage was the highest to date in China. When the International Agency for Research on Cancer/International Association of Cancer Registry (IARC/IACR) called for data collection from all over the world, China submitted population based cancer registration data from 26 registries for the publication of Cancer Incidence in Five Continents, Volume 10. Finally, 12 registries' data were qualified based on the criteria from IACR and contributed to the publication (http://ci5.iarc.fr/CI5-X/ci5-X.htm). Recently, the national program pushed this work forward both in the increase of coverage and the improvement in data quality.
The results showed that the estimated incidences of esophageal cancer were 287.6 thousand (incidence rate of 21.88/100 000) and deaths were 208.5 thousand (mortality of 15.85/100 000) in 2010. It still ranked the fifth in incidence and fourth in mortality of all cancer types. Compared to the 2009 data, both incidence and mortality were slightly lower;4 however, the coverage of registries dramatically changed in this time. Recently, the establishment of registries has focused on rural areas because of the unbalanced distribution between urban and rural areas; rural populations accounted for a small percentage in the data compared to the reality. We used regional stratification in this study. Finally, national estimates of incidence and mortality were calculated using the age specific rate in each group and the national population in 2010.
This time trend analysis has shown that the incidence of esophageal cancer has continued to decrease after adjusted by age since the late 1990s.18 However, as the ageing population increases, the number of new cases of esophageal cancer is also predicted to increase.18
Conclusion
The prevention and control of esophageal cancer was identified as a priority as a result of its status as a major type of cancer in China, particularly in rural areas. A focus on early detection and treatment comparable to other major cancer types, including stomach, cervical, breast, and liver cancer, has led to a breakthrough of the cancer screening program in China, especially in rural areas. Program sites of esophageal cancer have spread to more than 100 and nearly half a million people considered high-risk are screened every year, undoubtedly contributing to the decreasing rate of esophageal cancer mortality in China.
Acknowledgments
We would like to express our appreciation to all of the staff from local cancer registries that have made a great contribution by providing their cancer registration databases.
Disclosure
No authors report any conflict of interest.
References
- Castro C, Bosetti C, Malvezzi M, et al. Patterns and trends in esophageal cancer mortality and incidence in Europe (1980–2011) and predictions to 2015. Ann Oncol. 2014;25:283–290. doi: 10.1093/annonc/mdt486. [DOI] [PubMed] [Google Scholar]
- Beales ILP, Hensley A, Loke Y. Reduced esophageal cancer incidence in statin users, particularly with cyclo-oxygenase inhibition. World J Gastrointest Pharmacol Ther. 2013;4:69–79. doi: 10.4292/wjgpt.v4.i3.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pohl H, Welch HG. The role of overdiagnosis and reclassification in the marked increase of esophageal adenocarcinoma incidence. J Natl Cancer Inst. 2005;97:142–146. doi: 10.1093/jnci/dji024. [DOI] [PubMed] [Google Scholar]
- Brown LM, Devesa SS, Chow WH. Incidence of adenocarcinoma of the esophagus among white Americans by sex, stage, and age. J Natl Cancer Inst. 2008;100:1184–1187. doi: 10.1093/jnci/djn211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–2917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- Bosetti C, Levi F, Ferlay J, et al. Trends in oesophageal cancer incidence and mortality in Europe. Int J Cancer. 2008;122:1118–1129. doi: 10.1002/ijc.23232. [DOI] [PubMed] [Google Scholar]
- Sikkema M, de Jonge PJ, Steyerberg EW, Kuipers EJ. Risk of esophageal adenocarcinoma and mortality in patients with Barrett's esophagus: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2010;8:235–244. doi: 10.1016/j.cgh.2009.10.010. [DOI] [PubMed] [Google Scholar]
- Das D, Chilton AP, Jankowski JA. Chemoprevention of oesophageal cancer and the AspECT trial. Recent Results Cancer Res. 2009;181:161–169. doi: 10.1007/978-3-540-69297-3_15. [DOI] [PubMed] [Google Scholar]
- Alexandre L, Broughton T, Loke Y, Beales IL. Meta-analysis: risk of esophageal adenocarcinoma with medications which relax the lower esophageal sphincter. Dis Esophagus. 2012;25:535–544. doi: 10.1111/j.1442-2050.2011.01285.x. [DOI] [PubMed] [Google Scholar]
- Sun X, Chen W, Chen Z, Wen D, Zhao D, He Y. Population-based case-control study on risk factors for esophageal cancer in five high-risk areas in China. Asian Pac J Cancer Prev. 2010;11:1631–1636. [PubMed] [Google Scholar]
- Chen W, He Y, Zheng R, et al. Esophageal cancer incidence and mortality in China, 2009. J Thorac Dis. 2013;5:19–26. doi: 10.3978/j.issn.2072-1439.2013.01.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Office for Cancer Prevention and Control, China. The Guideline of Cancer Registration of China. Beijing: Peking Union Medical College Press; 2004. [Google Scholar]
- Curado M, Edwards B, Shin H. Storm H. Ferlay J. Heanue M. Boyle . Cancer Incidence in Five Continents. IX. Lyon: International Agency for Research on Cancer; 2008. [Google Scholar]
- Parkin DM, Bray F. Evaluation of data quality in the cancer registry: principles and methods Part II. Completeness. Eur J Cancer. 2009;45:756–764. doi: 10.1016/j.ejca.2008.11.033. [DOI] [PubMed] [Google Scholar]
- National Office for Cancer Prevention and Control, National Center for Cancer Registry, Disease Prevnetion and Control Bureau, MOH. Chinese Cancer Registry Annual Report (2008) Beijing: Military Medical Science Press; 2009. p. 9. [Google Scholar]
- National Office for Cancer Prevention and Control, National Center for CancerRegistry, Disease Prevnetion and Control Bureau, MOH. Chinese Cancer Registry Annual Report (2009) Beijing: Military Medical Science Press; 2010. p. 6. [Google Scholar]
- National Office for Cancer Prevention and Control, National Center for Cancer Registry, Disease Prevnetion and Control Bureau, MOH. Chinese Cancer Registry Annual Report (2010) Beijing: Military Medical Science Press; 2011. p. 2. [Google Scholar]
- Zeng HM, Zheng RS, Zhang SW, et al. Analysis and prediction of esophageal cancer incidence trend in China. Zhonghua Yu Fang Yi Xue Za Zhi. 2012;46(7):593–597. (In Chinese.) [PubMed] [Google Scholar]


