Abstract
Background
In recent decades, low-level laser therapy (LLLT) has been widely used to relieve pain caused by different musculoskeletal disorders. Though widely used, its reported therapeutic outcomes are varied and conflicting. Results similarly conflict regarding its usage in patients with nonspecific chronic low back pain (NSCLBP). This study investigated the efficacy of low-level laser therapy (LLLT) for the treatment of NSCLBP by a systematic literature search with meta-analyses on selected studies.
Method
MEDLINE, EMBASE, ISI Web of Science and Cochrane Library were systematically searched from January 2000 to November 2014. Included studies were randomized controlled trials (RCTs) written in English that compared LLLT with placebo treatment in NSCLBP patients. The efficacy effect size was estimated by the weighted mean difference (WMD). Standard random-effects meta-analysis was used, and inconsistency was evaluated by the I-squared index (I2).
Results
Of 221 studies, seven RCTs (one triple-blind, four double-blind, one single-blind, one not mentioning blinding, totaling 394 patients) met the criteria for inclusion. Based on five studies, the WMD in visual analog scale (VAS) pain outcome score after treatment was significantly lower in the LLLT group compared with placebo (WMD = -13.57 [95 % CI = -17.42, -9.72], I2 = 0 %). No significant treatment effect was identified for disability scores or spinal range of motion outcomes.
Conclusions
Our findings indicate that LLLT is an effective method for relieving pain in NSCLBP patients. However, there is still a lack of evidence supporting its effect on function.
Keywords: LLLT, Low-level laser therapy, Nonspecific chronic low back pain, NSCLBP, Pain relief
Background
Low back pain (LBP) is one of the most common musculoskeletal disorders [1, 2] and the leading cause of disability worldwide [3]. It affects more than two-thirds of the population during their lifetime and one in four people seek medical help for LBP in a 6-month period [4]. Musculoskeletal disorders account for 6–8 % of total disability-adjusted life years (DALYs) and of this large total, low back pain accounts for nearly half [5]. The majority of the symptoms resolve spontaneously within 1–3 months. However, 3–10 % of patients develop chronic symptoms lasting more than 6 weeks [6]. The underlying etiology of most low back pain is currently unclear. Thus, the one term, nonspecific chronic low back pain (NSCLBP), is used to refer to this condition [7]. Annually, $91 billion in medical expenses are spent for back pain with an additional $50 billion indirect costs incurred due to loss in productivity and disability benefit payments [8, 9].
The main goal of NSCLBP therapy is rarely the complete eradication of pain. Different strategies are currently utilized including surgery and drug therapy, exercise therapy, manipulation, acupuncture, electrical treatments, and cognitive-behavioral interventions.
In recent decades, low-level laser therapy (LLLT) has been widely used to relieve pain caused by different musculoskeletal disorders [10, 11]. Though widely used, its reported therapeutic outcomes are varied and conflicting. Results similarly conflict regarding its usage in patients with NSCLBP [12, 13]. There has been a recent increase in the number of RCTs evaluating the effectiveness of LLLT in patients with NSCLBP [12–18]. Therefore, the aim of this study was to examine the totality of evidence to evaluate the effectiveness of LLLT on symptoms and function in patients with NSCLBP through a systematic review and meta-analysis.
Methods
Search strategy and study selection
We conducted a systematic review and meta-analysis, using the approach recommended by the PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analyses) guidelines for meta-analyses of interventional studies [19]. The following bibliographic databases were searched up to 20 December 2014: Medline via PubMed from 1990, EMBASE via OVID from 1990, Web of Science from 1990 as well as the Cochrane Central Register of Controlled Trials. The search strategy was as follows: back pain OR low back pain OR backache OR lumbar adjacent pain OR chronic low back pain OR nonspecific chronic low back pain OR NSCLBP AND low-level laser therapy OR low-intensity laser therapy OR low-energy laser therapy OR LLLT OR LILT OR LELT OR infrared laser OR IR laser OR diode laser.
Two reviewers independently identified titles and abstracts relevant to LLLT for patients suffering from NSCLBP. Full texts of the published articles were analyzed and included. The reference list of the full-text articles was also reviewed. To be included in this analysis, studies had to meet the following criteria: (1) be randomized controlled trials; (2) involve patients suffering from NSCLBP; (3) compare LLLT and placebo treatment (no treatment or sham laser); (4) report pain and/or functional outcomes of patients; (5) attain a PEDro score (an 11-point scale, which is the one most often employed for physical treatments) [20] of >5 and (6) be written in English. Trials with an unbalanced additional modality between groups were excluded.
Data extraction
Study data were extracted by two reviewers and checked for accuracy by a third reviewer including the intervention description, inclusion/exclusion criteria, baseline, demographics, and values for all outcomes at baseline and after treatment. The primary outcomes of interest were the visual analog pain (VAS) pain score and disability measured by the Oswestry disability index (ODI) [21] after treatment. The secondary outcomes of interest were change in VAS pain score (defined as the mean difference between treatment arms from baseline to follow-up) and range of motion (ROM). If the data were not presented in the study as mean and standard deviation, or were presented in a form that prevented calculation of mean and standard deviation, the original authors were contacted.
Statistical analysis
All the primary and secondary outcomes were continuous data, permitting means and standard deviations to be used to calculate a weighted mean difference (WMD) and 95 % confidence interval (CI) in the meta-analysis. Data were presented as a forest plot. All results were checked for clinical and statistical heterogeneity. Heterogeneity was evaluated by a test for heterogeneity (I2 statistic): significant heterogeneity was defined as I2 ≤ 0.10; substantial heterogeneity was defined as I2 > 50 %. Data were pooled using a random-effects model. All analyses were conducted using Stata software, version 11.0 (Stata Inc., College Station, TX, USA).
Results
Study selection and characteristics
Figure 1 illustrates the selection process for including studies in the meta-analysis. In total, 221 potential studies were found. Based on the title and abstract content, 202 of these studies were excluded. The full texts of the remaining 19 studies were read, and a further 12 studies were excluded, resulting in seven studies [12–18] retained in the qualitative and quantitative synthesis of this review. A total of 394 patients were included: 202 patients in the LLLT group and 192 patients in the placebo group. Among the total of seven studies, three [16–18] included exercise as an additional treatment method in both study and control groups, while the other four did not. The characteristics of the included studies are listed in Table 1. Six of the seven studies achieved a high-quality PEDro score (≥7) (Table 2). Two otherwise relevant trials were excluded due to PEDro scores < =5. All outcomes with appropriately reported data were extracted and included in the meta-analysis. Outcome measures were grouped according to their construct and design (Table 3).
Fig. 1.
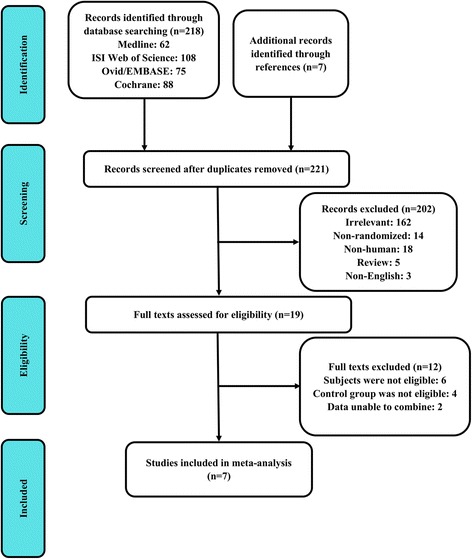
CONSORT diagram showing screening process and search results for the meta-analysis of LLLT for chronic nonspecific low back pain. LLLT low-level laser therapy
Table 1.
General information on low-level laser therapy (LLLT) included in the meta-analysis
| Study | Type of studies | Sample size | Age (SD) years | Gender (M/F) | Dropouts (n) | VAS pain (SD) | Intervention |
|---|---|---|---|---|---|---|---|
| Klein and Eek 1990 [13] | TB-RCT | Study group (n = 10) | 44.1 (7.9) | 2/8 | 0 | 30 (12) | LLLT vs. Placebo |
| Control group (n = 10) | 41.3 (10.7) | 3/8 | 0 | 33 (11) | |||
| Soriano and Rios 1998 [14] | DB-RCT | Study group (n = 38) | 63.2 | 16/22 | 0 | 79 | LLLT vs. Placebo |
| Control group (n = 33) | 64.33 | 18/20 | 0 | 81 | |||
| Basford et al. 1999 [15] | DB-RCT | Study group (n = 27) | 47.8 (48.0) | 18/12 | 3 | 35.2 (29.0) | LLLT vs. Placebo |
| Control group (n = 29) | 48.2 (49) | 13/16 | 0 | 37.4 (36.0) | |||
| Gur et al. 2003 [16] | SB-RCT | Study group (n = 25) | 35.2 (10.51) | 7/18 | 0 | 62 (21) | LLLT + Ex vs. Placebo + Ex |
| Control group (n = 25) | 36.4 (9.83) | 8/17 | 0 | 65 (16) | |||
| Djavid et al. 2007 [17] | DB-RCT | Study group (n = 19) | 38 (7) | 12/7 | 0 | 62 (16) | LLLT + Ex vs. Placebo + Ex |
| Control group (n = 18) | 36 (10) | 15/3 | 0 | 63 (20) | |||
| Vallone et al. 2014 [18] | RCT | Study group (n = 50) | 68 (24-89) | 43/57 | 0 | 66.4 (17.7) | LLLT + Ex vs. Placebo + Ex |
| Control group (n = 50) | 0 | 63.6 (15.2) | |||||
| Hsieh et al. 2014 [12] | DB-RCT | Study group (n = 33) | 60.1 (14.2) | 14/19 | 0 | 78 (24) | LLLT vs. Placebo |
| Control group (n = 27) | 58.5 (10.6) | 8/19 | 0 | 79 (17) |
Mean (standard deviation) are provided above for age (years) and VAS pain (VAS visual analog scale)
TB-RCT triple blind-randomized controlled trial, DB-RCT double-blind randomized controlled trial, SB-RCT single-bind randomized controlled trial, M male, F female, Ex exercise
Table 2.
Summary of methodological quality based on PEDro classification scale
| Study | Item | Total | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | ||
| Klein and Eek 1990 [13] | ✓ | ✓ | x | ✓ | ✓ | ✓ | ✓ | ✓ | x | ✓ | ✓ | 9 |
| Soriano and Rios 1998 [14] | ✓ | ✓ | x | ✓ | x | x | x | ✓ | x | ✓ | ✓ | 6 |
| Basford et al. 1999 [15] | ✓ | ✓ | x | ✓ | ✓ | ✓ | x | ✓ | x | ✓ | ✓ | 8 |
| Gur et al. 2003 [16] | ✓ | ✓ | x | ✓ | ✓ | x | x | ✓ | x | ✓ | ✓ | 7 |
| Djavid et al. 2007 [17] | ✓ | ✓ | x | ✓ | ✓ | ✓ | x | ✓ | x | ✓ | ✓ | 8 |
| Vallone et al. 2014 [18] | ✓ | ✓ | ✓ | ✓ | x | x | x | ✓ | x | ✓ | ✓ | 7 |
| Hsieh et al. 2014 [12] | ✓ | ✓ | ✓ | ✓ | ✓ | x | ✓ | ✓ | x | ✓ | ✓ | 9 |
Items: 1-eligibility criteria specified, 2-random allocation, 3-concealed allocation, 4-groups similar at baseline, 5-subject blinding, 6-therapist blinding, 7-assessor blinding, 8-less than 15 % dropouts, 9-intention-to-treat analysis, 10-between-group statistical comparisons, 11-point measures and variability data; ✓yes, x no
Table 3.
Technical features of laser use in the studies included for meta-analysis
| Study | Laser type | Laser model (Manufacturer) | Treatment time/Number of total sessions/Number of sessions per week | Laser continuous output | Energy density (J/cm2) | Energy per point (J/point per session) |
|---|---|---|---|---|---|---|
| Klein and Eek 1990 [13] | GaAs 904 nm | Omniprobe | 20 m/12/3 | 20 W | 1.3 | 1.3 |
| Soriano and Rios 1998 [14] | GaAs 904 nm | NA | NA/10/5 | 40 mW | 4 | 6*10-6 |
| Basford et al. 1999 [15] | Nd: YAG 1060 nm | NA | 12 m/12/3 | 542 mW | 239.3 | 48.78 |
| Gur et al. 2003 [16] | GaAs 904 nm | Class IIIb Laser Product | 30 m/20/5 | 4.2 mW | 1 | 1 |
| Djavid et al. 2007 [17] | GaAlAs 810 nm | NA | 20 m/12/2 | 50 mW | 27 | 5.9697 |
| Vallone et al. 2014 [18] | GaAlAs 980 nm | LEONARDO BIO | 6 m/9/3 | 20 W | 37.5 | 1200 |
| Hsieh et al. 2014 [12] | GaAlAs 890 nm | Anodyne | 40 m/6/3 | 780 mW | 10.4 | NA |
NA not available
Meta-analysis
Pain relief
The mean VAS pain score after treatment was lower in the LLLT compared with the placebo group (WMD = -13.57 [95 % CI = -17.42, -9.72], I2 = 0 %). Subgroup analysis showed that exercise as an additional treatment did not change the results (Fig. 2). Three [12, 17, 18] of the included studies provided data on change in short-term VAS pain (follow-up minus baseline). The meta-analysis revealed significantly greater decline in VAS pain in response to LLLT compared with placebo treatment (WMD = -12.00 [95 % CI = -2.02, -21.98] I2 = 77.6 %) (Table 4).
Fig. 2.

Forest plot analysis of the VAS pain score after LLLT treatment. WMD weighted mean difference, LLLT low-level laser therapy, VAS visual analog scale; weight % stands for the portion of the total sample contributed by each study
Table 4.
Meta-analyses of weighted mean differences in various continuous parameters between the LLLT and placebo groups
| Outcome parameters* | Number of patients | Weighted mean difference (95 % CI) | p value | I2 | |
|---|---|---|---|---|---|
| LLLT group (n) | Placebo group (n) | ||||
| Change in VAS pain score after treatment (from baseline to after treatment) 12,17,18 | 102 | 95 | -12.00 [-2.02, -21.98] | 0.012 | 77.6 % |
| Anterior-posterior flexion (degree)13,17 | 29 | 28 | 3.20 [-2.54, 8.93] | 0.961 | 0 % |
| Anterior-posterior flexion (cm)15,16 | 35 | 35 | -.2.84 [-5.44, 0.02] | 0.480 | 0 % |
| Extension (degree)13,17 | 29 | 28 | 0.08 [-2.39, 2.54] | 0.973 | 0 % |
LLLT low-level laser therapy, VAS visual analog scale
*Study references provided by superscripts
Disability score
Disability data measured by ODI after treatment were provided by four studies [13, 15–17]. The ODI measures intensity of pain, lifting and activities such as ability to care for oneself, ability to walk, ability to sit, sexual function, ability to stand, social life, sleep quality and ability to travel. The combined results showed no significant difference between LLLT and placebo groups (WMD = -2.89 [95 % CI = -7.88, 2.29], I2 = 88 %) (Fig. 3).
Fig. 3.
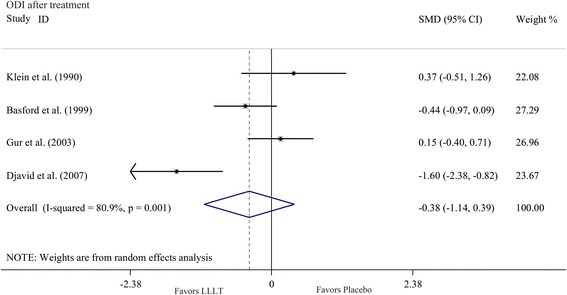
Forest plot analysis of disability outcomes after LLLT treatment measured by Oswestry disability index (ODI). LLLT low-level laser therapy
ROM
Data on ROM after treatment were provided by three studies and included flexion (angle measured in degrees), anterior-posterior flexion (measured in centimeters) and extension (angle measured in degrees). The combined data in terms of these three parameters demonstrated no statistical difference between the treatment groups (Table 4).
Discussion
NSCLBP is defined as pain of the lumbosacral area of the spine lasting more than 12 weeks. NSCLBP is a complex and multifactorial condition that may or may not have the characteristic of limiting the patient’s ROM [6]. Though various treatments options have been proposed, the management is still controversial. Most patients with NSCLBP who require medication for pain relief are likely to be middle-aged or older, and are at high risk for both adverse gastrointestinal and cardiovascular side effects [22]. Also the long-term surgical outcomes are no better than medical management [23]. Since first introduced by Mester et al. in 1968 [24], clinical application of LLLT has become more and more popular. Several experimental and clinical studies [25, 26] demonstrated its effectiveness for relief of chronic pain. Thus, many patients seek LLLT because it has no accompanying detrimental effects on systemic cardiovascular health or other adverse effects. Recently, several high-quality RCTs have emerged to assess the effectiveness of LLLT in patients with NSCLBP. We performed the current analysis, including seven RCTs with 394 patients, to gain a better understanding of the overall effect of LLLT for NSCLBP based on the higher-quality studies in a field full of seemingly conflicting results. Overall the analysis suggests that: (1) LLLT can relieve NSCLBP in a manner superior to placebo treatment; (2) LLLT is not superior to placebo treatment with respect to disability or ROM outcomes.
The mechanisms for LLLT-mediated pain relief are not fully understood. Several possible mechanisms are believed to account for the effects of LLLT, such as the following: (a) increased endogenous opioid neurotransmitter production [27]; (b) raised threshold to thermal pain and enhanced local blood circulation [28]; (c) increased oxygen consumption by accelerating the redox reaction rate of the electron respiratory chain of mitochondria [29]; (d) increased adenosine triphosphate (ATP) production at the cellular level [30]; (e) increased production of anti-inflammatory cytokines [12].
Multiple variables affect the clinical therapeutic effects of laser therapy, such as wavelength, energy density, the number of treatment sessions and their duration [31, 32]. Wavelength is also considered an essential parameter for beneficial outcomes of LLLT; it determines the ability of a laser to penetrate tissue. Wavelengths in a range of 700–1000 nm are most often used to treat deep tissues because of their superior penetration [33]. The recommended LLLT wavelengths per World Association of Laser Therapy (WALT) guidelines are 780–860 nm [34] and 904 nm [35] depending upon the condition being treated. Previous studies [36, 37] have also reported better therapeutic effects of LLLT with higher energy density, number of sessions and frequency of application. All the included studies used a wavelength within the recommended range.
It is well recognized that the effects of phototherapy are time-dependent [38]. We also observed this phenomenon as demonstrated in this meta-analysis by significant short-term but not moderate-term benefit. In contrast to pain outcomes, we did not find any significant improvement in disability or ROM due to LLLT. There might be several reasons for this. For one, the cause of NSCLBP is still unclear. Usually it is hard to determine the precise etiology of the pain. Some theories suggest that NSCLBP is linked to a reflex response of the back extensor muscles, resulting in a loss of flexion relaxation of the back muscles and a reduction of spinal flexion with secondary increased tissue strain [39]. LLLT may relieve the pain by increasing oxygen consumption and blood supply to the muscles [40]. With respect to duration, the effect is comparable to other interventions (e.g., antidepressants and traction), which are effective in the short term [41]. A primary effect on muscle may explain why we did not find any significant effect of LLLT on knee osteoarthritis (OA) pain [42], in which the sources of pain are diverse. Moreover, NSCLPB is likely a heterogeneous group of diseases, which have different etiologies but share similar symptoms. Thus, some of them might react well to LLLT while others not. Only two studies provided data on ROM. For this outcome, negative results might relate to inadequate study power that could be overcome with more high-quality investigations with ROM. Finally, like other LBP interventions, effects on pain appear to be stronger than effects on function [43].
Seven years ago, Yousefi-Nooraie et al. [44] conducted a meta-analysis of LLLT for nonspecific low back pain (NLBP); it contained seven studies of both acute and chronic NLBP [13–17, 45, 46]. The authors concluded that data were insufficient to confirm the clinical effectiveness of LLLT for NLBP. Our study is more specific, focusing on NCLBP, and is an update on this topic now demonstrating the likelihood of a beneficial effect of LLLT on low back pain. The difference in conclusions can likely be attributed to several strengths of our study. First, we focused on chronic LBP studies. The separation of chronic from acute NLBP is likely to decrease the heterogeneity. Second, the power of the current meta-analysis was substantially increased due to the inclusion of two additional studies corresponding to an appreciable increase in the numbers of subjects (sample size increased two times) over the prior meta-analysis. What is more, two low-quality studies were excluded due to PEDro scores <5 [44, 45]. Even if we included the results of theses two trials, the pooled results were still consistent with results of analyses of the trials of higher quality. Third, this meta-analysis was performed on the basis of the Cochrane Collaboration’s principle and designed to be rigorous in its search strategy. Fourth, narrow CIs around the point estimates due to the availability of higher-quality trials resulted in more precise estimates of treatment effects.
Some limitations of the current meta-analysis warrant discussion. First and foremost, we were limited by the outcome reporting of the included studies; for instance, only two studies were available for pooling to evaluate ROM. Second, because of the relatively heterogeneous treatment protocols with respect to laser parameters and laser schedules, high heterogeneity was detected in several outcomes. To overcome this, a random-effects model was chosen. Third, three of the included studies used exercise as an additional treatment in both study and control groups, while the other four did not. This could contribute to high heterogeneity in pooled results. However, the subgroup analysis showed that the use of adjunctive exercise did not affect the results. Fourth, LLLT has been also extensively used and studied in Europe and Russia; by restricting to English language studies, we could have missed some trials. Fifth, due to our relatively small number of trials, we could not assess publication bias using funnel plots or statistical tests for small sample effects.
Conclusions
The results of our systematic review and meta-analysis have provided the best current evidence on LLLT for the treatment of NSCLBP. It suggests that LLLT is an effective method to relieve low back pain in patients who present with NSCLBP. However, there is still a lack of evidence supporting its effectiveness on functional outcomes. Further research is needed to identify the optimal LLLT parameters for achieving therapeutic efficacy, particularly for functional outcomes, and for understanding its mechanisms of action.
Acknowledgments
We wish to acknowledge funding in support of ZH by the China Health Ministry Program (201302007). We also wish to acknowledge support of VBK by the National Institutes of Health National Institute on Aging Older American Independence Centers (NIH/NIA OAIC) P30-AG-028716. This research was funded by the China Health Ministry Program (201302007). We recognize the support of the China Scholarship Council (CSC). These organizations had no involvement in the study design, collection, analysis or interpretation of data, in the writing of the manuscript, or in the decision to submit the manuscript for publication.
Abbreviations
- ATP
Adenosine triphosphate
- CI
Confidence interval
- DALYs
Disability-adjusted life years
- LBP
Low back pain
- LLLT
Low-level laser therapy
- NLBP
Nonspecific low back pain
- NSCLBP
Nonspecific chronic low back pain
- OA
Osteoarthritis
- ODI
Oswestry disability index
- RCTs
Randomized controlled trials
- ROM
range of motion
- VAS
Visual analog scale
- WALT
World Association of Laser Therapy
- WMD
Weighted mean difference
Footnotes
ZeYu Huang, Jun Ma and Jing Chen contributed equally to this work.
Competing interests
None of the authors have competing interests to disclose. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Authors’ contributions
ZH, BS, FP and VBK take responsibility for the integrity of the work as a whole. All authors had full access to all of the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis. ZH, BS, FP and VBK conceived and designed the study. ZH, JM and JC collected and assembled the data. All authors assisted with analysis and interpretation of the data. ZH and VBK drafted the manuscript. All authors assisted with manuscript revisions and read and approved the final manuscript.
Contributor Information
ZeYu Huang, Email: Zey.huang@gmail.com.
Jun Ma, Email: dr.majun@foxmail.com.
Jing Chen, Email: sallychen.jc@gmail.com.
Bin Shen, Email: 492385233@qq.com.
FuXing Pei, Phone: +86-18980601380, Email: peifuxing1951@163.com.
Virginia Byers Kraus, Phone: +1-919-681-6652, Email: vbk@duke.edu.
References
- 1.Papageorgiou AC, Croft PR, Ferry S, Jayson MI, Silman AJ. Estimating the prevalence of low back pain in the general population. Evidence from the South Manchester Back Pain Survey. Spine. 1995;20:1889–94. doi: 10.1097/00007632-199509000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Strine TW, Hootman JM. US national prevalence and correlates of low back and neck pain among adults. Arthritis Rheum. 2007;57:656–65. doi: 10.1002/art.22684. [DOI] [PubMed] [Google Scholar]
- 3.Hoy D, March L, Brooks P, Brooks P, Blyth F, Woolf A, et al. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73:968–74. doi: 10.1136/annrheumdis-2013-204428. [DOI] [PubMed] [Google Scholar]
- 4.Kent PM, Keating JL. The epidemiology of low back pain in primary care. Chiropr Osteopat. 2005;13:13. doi: 10.1186/1746-1340-13-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197–223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 6.Croft PR, Macfarlane GJ, Papageorgiou AC, Thomas E, Silman AJ. Outcome of low back pain in general practice: a prospective study. BMJ. 1998;316:1356–9. doi: 10.1136/bmj.316.7141.1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van Tulder MW, Koes BW, Metsemakers JF, Bouter LM. Chronic low back pain in primary care: a prospective study on the management and course. Fam Pract. 1998;15:126–32. doi: 10.1093/fampra/15.2.126. [DOI] [PubMed] [Google Scholar]
- 8.Furlan AD, Yazdi F, Tsertsvadze A, Gross A, Van Tulder M, Santaguida L, et al. A systematic review and meta-analysis of efficacy, cost-effectiveness, and safety of selected complementary and alternative medicine for neck and low-back pain. Evid Based Complement Alternat Med. 2012;2012:953139. doi: 10.1155/2012/953139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cherkin DC, Sherman KJ, Deyo RA, Shekelle PG. A review of the evidence for the effectiveness, safety, and cost of acupuncture, massage therapy, and spinal manipulation for back pain. Ann Intern Med. 2003;138:898–906. doi: 10.7326/0003-4819-138-11-200306030-00011. [DOI] [PubMed] [Google Scholar]
- 10.Chen J, Huang Z, Ge M, Gao M. Efficacy of low-level laser therapy in the treatment of TMDs: a meta-analysis of 14 randomised controlled trials. J Oral Rehabil. 2015;42:291–9. doi: 10.1111/joor.12258. [DOI] [PubMed] [Google Scholar]
- 11.Montes-Molina R, Prieto-Baquero A, Martinez-Rodriguez ME, Romojaro-Rodriguez AB, Gallego-Mendez V, Martinez-Ruiz F. Interferential laser therapy in the treatment of shoulder pain and disability from musculoskeletal pathologies: a randomised comparative study. Physiotherapy. 2012;98:143–50. doi: 10.1016/j.physio.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 12.Hsieh RL, Lee WC. Short-term therapeutic effects of 890-nanometer light therapy for chronic low back pain: a double-blind randomized placebo-controlled study. Lasers Med Sci. 2014;29:671–9. doi: 10.1007/s10103-013-1378-2. [DOI] [PubMed] [Google Scholar]
- 13.Klein RG, Eek BC. Low-energy laser treatment and exercise for chronic low back pain: double-blind controlled trial. Arch Phys Med Rehabil. 1990;71:34–7. [PubMed] [Google Scholar]
- 14.Soriano F, Rios R. Gallium Arsenide laser treatment of chronic low back pain: a prospective, randomized and double blind study. Laser Therapy. 1998;10:175–80. doi: 10.5978/islsm.10.175. [DOI] [Google Scholar]
- 15.Basford JR, Sheffield CG, Harmsen WS. Laser therapy: a randomized, controlled trial of the effects of low-intensity Nd:YAG laser irradiation on musculoskeletal back pain. Arch Phys Med Rehabil. 1999;80:647–52. doi: 10.1016/S0003-9993(99)90167-3. [DOI] [PubMed] [Google Scholar]
- 16.Gur A, Karakoc M, Cevik R, Nas K, Sarac AJ, Karakoc M. Efficacy of low power laser therapy and exercise on pain and functions in chronic low back pain. Lasers Surg Med. 2003;32:233–8. doi: 10.1002/lsm.10134. [DOI] [PubMed] [Google Scholar]
- 17.Djavid GE, Mehrdad R, Ghasemi M, Hasan-Zadeh H, Sotoodeh-Manesh A, Pouryaghoub G. In chronic low back pain, low level laser therapy combined with exercise is more beneficial than exercise alone in the long term: a randomised trial. Aust J Physiother. 2007;53:155–60. doi: 10.1016/S0004-9514(07)70022-3. [DOI] [PubMed] [Google Scholar]
- 18.Vallone F, Benedicenti S, Sorrenti E, Angiero F. Effect of diode laser in the treatment of patients with nonspecific chronic low back pain: a randomized controlled trial. Photomed Laser Surg. 2014;32:490–4. doi: 10.1089/pho.2014.3715. [DOI] [PubMed] [Google Scholar]
- 19.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sherrington C, Herbert RD, Maher CG, Moseley AM. PEDro. A database of randomized trials and systematic reviews in physiotherapy. Man Ther. 2000;5:223–6. doi: 10.1054/math.2000.0372. [DOI] [PubMed] [Google Scholar]
- 21.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine. 2000;25:2940–52. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 22.White WB. The potential role of nitric oxide in cardiovascular safety when treating osteoarthritis in patients with hypertension. Introduction. Am J Med. 2009;122(5 Suppl):S1–2. doi: 10.1016/j.amjmed.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 23.Holm I. Fusion surgery is slightly better than non-surgical treatment in patients with severe chronic non-specific low back pain. Aust J Physiother. 2002;48:133. doi: 10.1016/S0004-9514(14)60208-7. [DOI] [PubMed] [Google Scholar]
- 24.Mester E, Ludany G, Sellyei M, Szende B. On the biologic effect of laser rays. Bull Soc Int Chir. 1968;27:68–73. [PubMed] [Google Scholar]
- 25.Salmos-Brito JA, de Menezes RF, Teixeira CE, Gonzaga RK, Rodrigues BH, Braz R, et al. Evaluation of low-level laser therapy in patients with acute and chronic temporomandibular disorders. Lasers Med Sci. 2013;28:57–64. doi: 10.1007/s10103-012-1065-8. [DOI] [PubMed] [Google Scholar]
- 26.Masoumipoor M, Jameie SB, Janzadeh A, Nasirinezhad F, Soleimani M, Kerdary M. Effects of 660- and 980-nm low-level laser therapy on neuropathic pain relief following chronic constriction injury in rat sciatic nerve. Lasers Med Sci. 2014;29:1593–8. doi: 10.1007/s10103-014-1552-1. [DOI] [PubMed] [Google Scholar]
- 27.Hagiwara S, Iwasaka H, Hasegawa A, Noguchi T. Pre-irradiation of blood by gallium aluminum arsenide (830 nm) low-level laser enhances peripheral endogenous opioid analgesia in rats. Anesth Analg. 2008;107:1058–63. doi: 10.1213/ane.0b013e31817ee43e. [DOI] [PubMed] [Google Scholar]
- 28.Schindl A, Schindl M, Schon H, Knobler R, Havelec L, Schindl L. Low-intensity laser irradiation improves skin circulation in patients with diabetic microangiopathy. Diabetes Care. 1998;21:580–4. doi: 10.2337/diacare.21.4.580. [DOI] [PubMed] [Google Scholar]
- 29.Yu W, Naim JO, McGowan M, Ippolito K, Lanzafame RJ. Photomodulation of oxidative metabolism and electron chain enzymes in rat liver mitochondria. Photochem Photobiol. 1997;66:866–71. doi: 10.1111/j.1751-1097.1997.tb03239.x. [DOI] [PubMed] [Google Scholar]
- 30.Benedicenti S, Pepe IM, Angiero F, Benedicenti A. Intracellular ATP level increases in lymphocytes irradiated with infrared laser light of wavelength 904 nm. Photomed Laser Surg. 2008;26:451–3. doi: 10.1089/pho.2007.2218. [DOI] [PubMed] [Google Scholar]
- 31.Fulop AM, Dhimmer S, Deluca JR, Johanson DD, Lenz RV, Patel KB, et al. A meta-analysis of the efficacy of laser phototherapy on pain relief. Clin J Pain. 2010;26:729–36. doi: 10.1097/AJP.0b013e3181f09713. [DOI] [PubMed] [Google Scholar]
- 32.Enwemeka CS, Parker JC, Dowdy DS, Harkness EE, Sanford LE, Woodruff LD. The efficacy of low-power lasers in tissue repair and pain control: a meta-analysis study. Photomed Laser Surg. 2004;22:323–9. doi: 10.1089/pho.2004.22.323. [DOI] [PubMed] [Google Scholar]
- 33.Kwon K, Son T, Lee KJ, Jung B. Enhancement of light propagation depth in skin: cross-validation of mathematical modeling methods. Lasers Med Sci. 2009;24:605–15. doi: 10.1007/s10103-008-0625-4. [DOI] [PubMed] [Google Scholar]
- 34.Therapy WWAoL. Dose table 780-860nm for Low Level Laser Therapy WALT 2010. Available from: http://waltza.co.za/wp-content/uploads/2012/08/Dose_table_780-860nm_for_Low_Level_Laser_Therapy_WALT-2010.pdf. 2010.
- 35.(WALT) WAoLT. Dose table 904 nm for Low Level Laser Therapy WALT 2010. Available from: http://waltza.co.za/wp-content/uploads/2012/08/Dose_table_904nm_for_Low_Level_Laser_Therapy_WALT-2010.pdf. 2010.
- 36.Alghadir A, Omar MT, Al-Askar AB, Al-Muteri NK. Effect of low-level laser therapy in patients with chronic knee osteoarthritis: a single-blinded randomized clinical study. Lasers Med Sci. 2014;29:749–55. doi: 10.1007/s10103-013-1393-3. [DOI] [PubMed] [Google Scholar]
- 37.Fukuda VO, Fukuda TY, Guimarães M, Shiwa S, de Lima BDC, Martin R, et al. Short-term efficacy of low-level laser therapy in patients with knee osteoarthritis: a randomized placebo-controlled, double-blind clinical trial. Rev Bras Ortop. 2011;46:526–33. doi: 10.1590/S0102-36162011000500008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Burke TJ. The effect of monochromatic infrared energy on sensation in subjects with diabetic peripheral neuropathy: a double-blind, placebo-controlled study: response to Clifft et al. Diabetes Care. 2006;29:1186–7. doi: 10.2337/dc06-0040. [DOI] [PubMed] [Google Scholar]
- 39.Burnett AF, Cornelius MW, Dankaerts W, O’sullivan PB. Spinal kinematics and trunk muscle activity in cyclists: a comparison between healthy controls and non-specific chronic low back pain subjects-a pilot investigation. Man Ther. 2004;9:211–9. doi: 10.1016/j.math.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 40.Hayworth CR, Rojas JC, Padilla E, Holmes GM, Sheridan EC, Gonzalez-Lima F. In vivo low-level light therapy increases cytochrome oxidase in skeletal muscle. Photochem Photobiol. 2010;86:673–80. doi: 10.1111/j.1751-1097.2010.00732.x. [DOI] [PubMed] [Google Scholar]
- 41.van Tulder M, Koes B, Bombardier C. Low back pain. Best Pract Res Clin Rheumatol. 2002;16:761–75. doi: 10.1053/berh.2002.0267. [DOI] [PubMed] [Google Scholar]
- 42.Huang Z, Chen J, Ma J, Shen B, Pei FX, Kraus VB. Effectiveness of low-level laser therapy in patients with knee osteoarthritis: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2015;23:1437–44. doi: 10.1016/j.joca.2015.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Walti P, Kool J, Luomajoki H. Short-term effect on pain and function of neurophysiological education and sensorimotor retraining compared to usual physiotherapy in patients with chronic or recurrent non-specific low back pain, a pilot randomized controlled trial. BMC Musculoskelet Disord. 2015;16:83. doi: 10.1186/s12891-015-0533-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yousefi-Nooraie R, Schonstein E, Heidari K, Rashidian A, Penneick V, Akbari-Kamrani M, et al. Low level laser therapy for nonspecific low-back pain. Cochrane Database Syst Rev. 2008:CD005107. [DOI] [PubMed]
- 45.Longo LTA, Monti A. Treatment with 904 nm and 10600 nm laser acute lumbago-double blind control-laser. J Eur Med Laser Ass. 1991;3:16–9. [Google Scholar]
- 46.Toya S, Motegi M, Inomata K, Ohshiro T, Maeda T. Report on a computer-randomized double blind clinical trial to determine the effectiveness of the GaAlAs (830 nm) diode laser for pain attenuation in selected pain groups. Laser Therapy. 1994;6:143–8. doi: 10.5978/islsm.94-OR-08. [DOI] [Google Scholar]


