Abstract
Objective
To examine baseline characteristics and biochemically verified 1-, 4-, and 6-month tobacco quit rates among college students enrolled in a Quit and Win cessation trial, comparing those who concurrently smoke both hookah and cigarettes with those who deny hookah use.
Methods
Analyses were conducted on data from 1,217 college students enrolled in a Quit and Win tobacco cessation randomized clinical trial from 2010–2012. Multivariable logistic regression (MLR) analyses examined group differences in baseline characteristics and cotinine verified 30-day abstinence at 1, 4, and 6-month follow-up, adjusting for baseline covariates.
Results
Participants smoked 11.5(±8.1) cigarettes per day on 28.5(±3.8) days/month, and 22% smoked hookah in the past 30 days. Hookah smokers (n=270) were more likely to be male (p<0.0001), younger (p<0.0001), report more binge drinking (p<0.0001) and score higher on impulsivity (p<0.001). MLR results indicate that hookah users, when compared to non-users, had a 36% decrease in odds of self-reported 30-day abstinence at 4-months (OR= 0.64, 95% CI=0.45–0.93, p=0.02) and a 63% decrease in odds in biochemically verified continuous abstinence at 6-months (OR = 0.37, CI=0.14–0.99, p=0.05).
Conclusion
College cigarette smokers who concurrently use hookah display several health risk factors and demonstrate lower short and long-term tobacco abstinence rates.
Keywords: cigarette smoking, hookah smoking, smoking cessation, awards and prizes, young adult, college students
Introduction
While cigarette smoking is on the decline overall in the U.S., use remains high among young adults. Compared with individuals ages 12–17 and 26 and older, those between the ages 18–25 have the highest prevalence of current smoking (31.8%) (Substance Abuse and Mental Health Services Administration, 2012). Although college students are less likely to smoke cigarettes than their peers not enrolled in college (46%) (Lenk et al., 2012), current smoking rates among college smokers continues to be high (21.3%) (Substance Abuse and Mental Health Services Administration, 2012). In addition, the use of other tobacco products is increasingly common among young adults. A national survey of students from 119 four-year colleges indicates that past 30-day use of cigars, smokeless tobacco and pipes were 8.5%, 3.7% and 1.2% respectively (Rigotti et al., 2000). The use of a waterpipe to smoke tobacco, commonly referred to as “hookah” or “shisha,” has also increased in popularity among college students. Lifetime or “ever use” of hookah among college students is approximately 40%, while the recent prevalence estimate of current use (use within the past 30 days) is approximately 16% (Griffith, Harmon & Gilly, 2011;Rahman, Chang, Hadgu, Salinas-Miranda & Corbin, 2014; Sutfin et al., 2011). This data suggests that after cigarettes, hookah smoking may currently be the most commonly used tobacco product used by college students.
Hookah smoking is often a social experience and socializing is often indicated as the most appealing aspect of this behavioral trend (Ahmed, Jacob, Allen & Benowitz, 2011). Hookah bars are frequently located around college campuses (Fielder, Carey & Carey, 2012; Sutfin et al., 2011). Further, hookah smoking may be gaining in popularity because of a widespread belief that it is not as harmful as smoking cigarettes or using other tobacco products and that it is less addictive (Primack et al., 2008; Sutfin et al., 2011). However, a hookah session has been associated with ingestion of greater carbon monoxide, tar and nicotine than smoking a single cigarette (Eissenberg and Shihadeh, 2009). Further, saliva and urine cotinine levels of hookah smokers are comparable with cigarette smokers (Aoun, Pascale, & Waled, 2007; Neergaard, Singh, Job & Montgomery, 2007). A systematic review of the literature on health effects of hookah indicate that smoking hookah more than doubles the risk of lung cancer, respiratory illness and low birth weight when used during pregnancy (Akl et al., 2010).
Recent interest in hookah smoking among college students has provided a picture of the general characteristics of a young adult hookah smoker. Hookah users are generally younger in age, more likely to be white and male (Eissenberg et al., 2008), report increased use of both alcohol and marijuana (Sutfin et al., 2011), and are more likely to be current cigarette smokers (Eissenberg et al., 2008; Sutfin et al., 2011). In fact, among a sample of current hookah users, 77.4% endorsed concurrent use of cigarettes (Lee et al., 2014).
Although research has provided insight on the typical college hookah user, few studies have examined the characteristics of college students who concurrently use both hookah and cigarettes or explored the impact of hookah use on cigarette smoking quit attempts. Secondary analyses of data gathered during a randomized clinical trial evaluating the impact of Quit and Win contests on college student tobacco abstinence rates (ClinicalTrials.Gov Registry #NCT01096108) was used to describe the demographic, tobacco-specific and psychosocial characteristics of college student smokers who concurrently smoked hookah, compared to those who did not. These data were also used to examine the potential impact of concurrent hookah use on biochemically verified tobacco cessation rates.
The purpose of this study is to build upon previous research to describe the demographic, tobacco-specific and psychosocial characteristics of college students who smoke cigarettes, compared to those who smoke both hookah and cigarettes. Further, to examine the potential impact of concurrent hookah use on biochemically verified tobacco cessation rates among a large sample of college students enrolled in a Quit and Win tobacco cessation research trial.
Methods
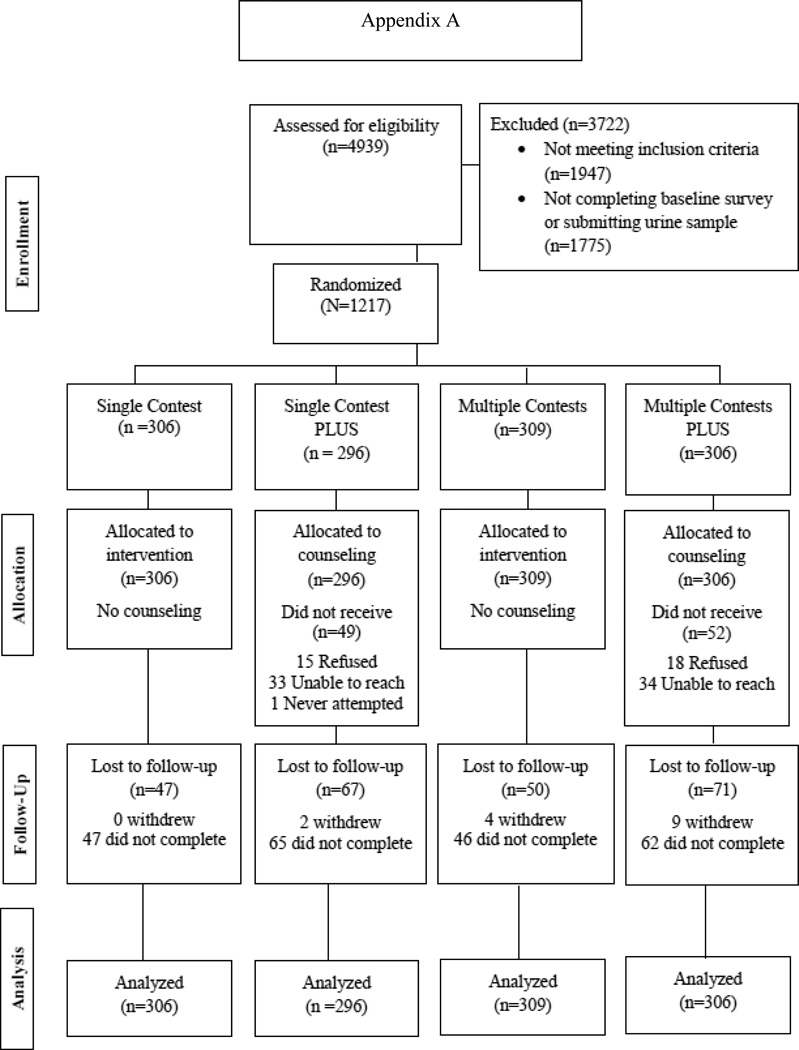
Data for this study comes from a two-by-two factorial randomized clinical trial with group allocation to four treatment arms to evaluate the efficacy of a single, lottery-incentivized cessation contest (i.e., 30-day period) vs. three, successive 30-day contests, with and without counseling, on tobacco cessation quit rates at 1, 4- and 6-months after study baseline (i.e., end of first contest period, end of treatment and end of study, retrospectively). Participants eligible for this study were students enrolled in one of 17 participating colleges who had smoked at least one cigarette per day on 10 or more days in the past month. Identification of hookah users was determined by asking the following question at eligibility: “In the past 30 days have you smoked tobacco from a waterpipe (hookah, shisha, nargile), even one or two puffs?” Participants who responded “yes” were considered hookah users while those who did not were considered to be non-users of hookah.
Procedures
During 2010–2012, a randomized clinical trial was implemented at 2- and 4-year colleges in 3 waves (N = 1,217). Participants were required to abstain from all tobacco products (including cigarette smoking and other forms of tobacco including smokeless tobacco, cigars, cigarettes, pipe and hookah) for 1-or 4-months for the chance to win lottery-based prizes. The primary outcome was biochemically verified confirmation of self-reported tobacco abstinence using urine cotinine (cutpoint 40ng/mL) at 6-months post enrollment. Regardless of hookah smoking status, at the beginning of each of the three recuiting years, all participants were randomized in blocks of 4, stratified by campus, by the study statistician. Participants were assigned to one of four study arms to compare the impact of a single Quit and Win contest, with and without Motivation and Problem-Solving Counseling (MAPS) to multiple, concurrent contests (i.e., 3-month long contests) with and without counseling. Assignment was not blinded to staff or participants. Specifically,, Single Contest (1-month contest only; n=306); Single PLUS (1-month contest, plus 6 counseling sessions, n=296); Multiple Contests (3 successive contests; n=309); and Multiple PLUS (3 successive contests, plus 6 counseling sessions, n=306) were compared. An on-line survey was completed at 1, 4 and 6 months post-enrollment. Urine cotinine was analyzed at baseline to verify positive smoking status and at all follow-up assessments to confirm self-reported abstinence from cigarettes and all tobacco products.
Measures
Baseline measures assessed participant demographic, psychosocial, and tobacco-related characteristics (i.e., age, gender, ethnicity, employment, marital status, year in school, and type of school [2-year vs 4-year]). Tobacco-related variables included days smoked cigarettes in the past 30, number of cigarettes smoked per day (CPD), number of 24-hour smoking quit attempts in the past year, age of first cigarette, menthol cigarette use, and use of smokeless tobacco, cigars, pipe and/or hookah in the past 30 days. Nicotine dependence was measured using “time to first cigarette” (≤ 30 minutes) (Heatherton et al., 1991). Craving was assessed using the craving subscale from the Wisconsin Smoking Withdrawal Scale (Welsch et al., 1999); alcohol use was assessed using questions from the AUDIT (# of days drank at least one drink, # of days drank five or more drinks [i.e., binge drinking episode]) (Saunders et al., 1993) and stress was measured using the 4-item Perceived Stress Scale (Cohen et al., 1983). Two subscales of the Wisconsin Inventory of Smoking Dependence Motives (WISDM) (Smith et al., 2010) were used (i.e., cue exposure and loss of control). Social influence was measured by asking how many of participant’s five closest friends smoked cigarettes (Centers for Disease Control and Prevention, 1999). Finally, we assessed impulsivity using the short form of the Barratt Impulsiveness Scale (Spinella, 2007).
Data Analysis
Sample size for the parent trial was determined using a closed testing procedure based on a logistic regression with main effects (30-day verified abstinence across standard vs. multiple contest and counseling vs. no counseling).
Demographic, smoking, and other characteristics were summarized by group (hookah users vs. non-users) using mean and standard deviation (SD) for continuous variables and frequency and percentage for categorical variables. Chi-square test and t test (or Wilcoxon rank sum test) were used for categorical and continuous variables, respectively, to compare hookah users vs. non-users in the univariate analysis. Multivariable logistic regression (MLR) analysis was performed to model the probability of self-reported quit and biochemically verified quit at 1, 4 and 6 months, adjusting for treatment group, and selected baseline demographics, and tobacco-use related variables. Continuous abstinence at 6-months was also examined. Missing smoking status was recoded as smoking.
Results
Participants
Demographic, tobacco-specific and psychosocial variables are presented in Table 1. The mean (±SD) age of participants was 26.3±7.7 years, 54.9% were women, and 85.1% identified as White. Two-thirds (67.7%) of participants attended a 4-year university. On average, participants smoked 11.5±8.1 cigarettes per day, smoked on 28.5±3.8 days per month, and 49% smoked their first cigarette within 30 minutes of waking (i.e., probable nicotine dependence).
Table 1.
Demographic, Psychosocial, and Tobacco-Related Characteristics (N=1217) of Participating Quit and Win College Students from the Midwest, 2010–2012
| Variable | Total (N=1,217) |
Hookah Users (n=270) |
Non-Hookah Users (n=947) |
P-value |
|---|---|---|---|---|
| Age, mean (SD) | 26.3 (7.7) | 21.5 (4.1) | 27.6 (7.9) | <0.0001 |
| Female, n (%) | 668 (54.9%) | 111 (41.1%) | 557 (58.8%) | <0.0001 |
| Ethnicity, White, n (%) | 1036 (85.1%) | 229 (84.8%) | 807 (85.2%) | 0.87 |
| Employment, Full time, n (%) | 212 (17.4%) | 21 (7.8%) | 191 (20.2%) | <0.0001 |
| Marital Status, Married/living with partner, n (%) | 404 (33.2%) | 31 (11.5%) | 373 (39.4%) | <0.0001 |
| Type of school, n (%) | <0.0001 | |||
| 2-year | 393 (32.3%) | 46 (17.0%) | 347 (36.6%) | |
| 4-year | 824 (67.7%) | 224 (83.0%) | 600 (63.4%) | |
| Cigarettes per day, mean (SD) | 11.5 (8.1) | 9.4 (7.7) | 12.1 (8.2) | <0.0001 |
| Days smoked, past 30 days, mean (SD) | 28.5 (3.8) | 28.0 (4.2) | 28.6 (3.6) | 0.03 |
| Quit attempts, past year, mean (SD) | 3.5 (8.1) | 4.6 (9.7) | 3.2 (7.6) | <0.0001 |
| Time to first cigarette, ≤ 30 minutes, n (%) | 598 (49.2%) | 112 (41.5%) | 486 (51.4%) | <0.01 |
| Other tobacco use, past 30 days, n (%) | ||||
| Smokeless | 148 (12.2%) | 54 (20.0%) | 94 (9.9%) | <0.0001 |
| Cigars/Pipes | 241 (19.8%) | 111 (41.1%) | 130 (13.7%) | <0.0001 |
| Smoke menthol cigarettes, n (%) | 375 (30.8%) | 103 (38.1%) | 272 (28.8%) | <0.01 |
| Age of first cigarette, mean (SD) | 15.6 (3.0) | 15.7 (2.4) | 15.6 (3.1) | 0.35 |
| Wisconsin Smoking Withdrawal Scale, Craving, mean (SD) | 6.4 (2.2) | 6.2 (2.2) | 6.4 (2.3) | 0.12 |
| Days of drinking, past 30, mean (SD) | 7.9 (7.3) | 9.5 (6.8) | 7.5 (7.3) | <0.0001 |
| Days of binge drinking, past 30, mean (SD) | 3.5 (4.4) | 5.1 (5.0) | 3.1 (4.1) | <0.0001 |
| Perceived Stress Scale, mean (SD) | 5.9 (2.9) | 6.4 (2.8) | 5.7 (2.9) | <0.001 |
| Dependence Motives (WISDM), mean (SD) | ||||
| Cue exposure | 5.0 (1.4) | 5.2 (1.4) | 4.9 (1.4) | <0.01 |
| Loss of control | 4.1 (1.6) | 3.9 (1.6) | 4.2 (1.6) | 0.01 |
| Five closest friends smoke, mean (SD) | 2.9 (1.4) | 3.1 (1.3) | 2.9 (1.4) | <0.01 |
| Barratt Impulsivity Scale, mean (SD) | ||||
| Motor Impulsivity | 11.2 (3.1) | 12.3 (3.3) | 10.9 (3.0) | <0.0001 |
| Attention Impulsivity | 11.0 (3.3) | 12.0 (3.4) | 10.7 (3.2) | <0.0001 |
| Non-Planning | 11.3 (3.2) | 12.0 (3.2) | 11.2 (3.2) | <0.001 |
| Total Score | 33.5 (7.1) | 36.2 (7.4) | 32.8 (6.8) | <0.0001 |
Chi-square test was used for categorical variables and t-test was used for continuous variables except for cigarettes per day, which was compared using Wilcoxon rank sum test because of its skewed distribution.
Approximately 22% (n=270) reported hookah use in the past 30 days. There were significant differences between participants who were hookah users and participants who were not. Hookah using smokers were significantly younger (21.5±4.1 years vs. 27.6±7.9 years, p<0.0001), more likely to be male (58.9% vs. 41.2%, p<0.0001), less likely to be employed full-time (7.8% vs. 20.2%, p<0.0001), and less likely to be married/living with a partner (11.5% vs. 39.4%, p<0.0001). Hookah users smoked fewer cigarettes per day (9.4±7.7 vs. 12.1± 8.2, p<0.0001) but had significantly more cigarette smoking quit attempts (4.6±9.7 vs. 3.2±7.6, p<0.0001). Hookah users were less nicotine dependent (41.5% vs. 51.4% smoked first cigarettes within 30 minutes of waking, p<0.01); reported more days of drinking (9.5±6.8 vs. 7.5±7.3, p<0.0001) and more days of binge drinking in the past month (5.1±5.0 vs. 3.1±4.1, p<0.0001); and were more likely to report current use of smokeless tobacco (20.0% vs. 9.9%, p<0.0001) and cigars or pipe (41.1% vs. 13.7%, p<0.0001). Hookah users also scored higher on the Wisconsin Inventory of Smoking Dependence Motives (WISDM) (Smith et al., 2010) subscales, cue exposure (5.2±1.4 vs. 4.9±1.4, p<0.01) and loss of control (3.9±1.6 vs. 4.2±1.6, p=0.01). Impulsivity was also higher among hookah smokers (36.2±7.4 vs. 32.8±6.8, p<0.0001).
Self-Report and Biochemically Verified Abstinence
Self-report and biochemically confirmed abstinence rates for hookah users and non-hookah-users at each assessment period were calculated. There were no significant differences in self-reported (39.3% vs. 43.4% p = 0.22) or cotinine verified quit rates at one month (27.4% vs Y, 31.7%), p = 0.17); however, hookah users when compared to non-users were significantly less likely to report abstinence at the 4- and 6-month follow-ups (20.0% vs. 29.7%, p<0.01 and 15.9% vs. 23.3%, p<0.01, respectively) and less likely to have biochemically verified abstinence at 6-month follow-up (8.2% vs. 13.9%, p=0.01). Rates of 6-month continuous abstinence were also significantly lower for hookah users compared to non-users for both self-reported abstinence (5.9% vs. 15.3%, p<0.0001) and verified abstinence (1.9% vs. 7.0%, p<0.01). Of note, there were no significant differences in self-report or biochemically verified missing status between the two groups at 1- or 6-month assessment periods.
Adjusted Multi-Variable Analyses
Results of a MLR, adjusting for treatment group, age, gender, ethnicity, marital status, type of school, number of 24-hour quit attempts in the past year, CPD, use of smokeless tobacco, and use of cigars and/or pipe in the past 30 days are shown in Table 2. Self-reported quit rates at 4-month remained significant. Hookah users had a 36% decreased odds of self-reported quit at end of treatment (i.e., 4-month assessment) than non-hookah users (odds ratio [OR] = 0.64, 95% confidence interval [CI], 0.45–0.93, p=0.02). Rates of 6-month continuous abstinence were also significantly different between hookah users and non-users of hookah for both self-report and biochemically verified quit rates. Compared to non-users, hookah users had a 55% decrease in odds of self-report continuous abstinence (OR = 0.45, 95% CI 0.25–0.81, p<0.01) and a 63% decrease in odds of biochemically verified continuous abstinence (OR = 0.37, CI 0.14–0.99, p=0.05).
Table 2.
Multivariable Logistic Regression Analysis of Abstinencea Comparing Participating Quit and Win College Students from the Midwest who Concurrently Smoke Hookah and Cigarettes with Non-hookah Users, 2010–2012
| Odd Ratio of Abstinence for Hookah Users vs. Non-Hookah Usersa |
95% Confidence Interval (CI) |
P-valueb | |||
|---|---|---|---|---|---|
| Quit at 1 month | |||||
| Self-report | 0.81 | 0.59 | 1.10 | 0.17 | |
| Verified | 0.81 | 0.58 | 1.15 | 0.24 | |
| Quit at 4 months | |||||
| Self-report | 0.64 | 0.45 | 0.93 | 0.02 | |
| Verified | 0.75 | 0.47 | 1.19 | 0.22 | |
| Quit at 6 months | |||||
| Self-report | 0.76 | 0.51 | 1.13 | 0.18 | |
| Verified | 0.71 | 0.42 | 1.20 | 0.20 | |
| Continuous at 6 months | |||||
| Self-report | 0.45 | 0.25 | 0.81 | <0.01 | |
| Verified | 0.37 | 0.14 | 0.99 | 0.05 | |
Adjusted for: treatment condition (counseling vs. no counseling and multiple vs. single contest), age, gender, ethnicity (white vs. non-white), marital status (married/living with partner vs. other), type of school (2- vs. 4-year school), number of 24-hour quit attempts in the past year, CPD, use of smokeless tobacco (Y/N) in the past 30 days, and use of cigars and/or pipe (Y/N) in the past 30 days.
Wald test p-values.
Discussion
In this sample of college students, current use of hookah was 22% and lifetime use was 62.1%. These findings are on the high-end of previous US-based surveys which report current hookah use at approximately 16% (Griffith, Harmon & Gilly, 2011; Rahman, Chang, Hadgu, Salinas-Miranda & Corbin, 2014; Sutfin et al., 2011). Lifetime use in our sample was also higher than the 20–50% reported in prior research (Barnett et al., 2013; Jarrett et al., 2012). Our sample was unique in that all participants were cigarette smokers and enrolled participants in a clinical trial testing the impact of Quit and Win contests on tobacco cessation. Because hookah use is more common among cigarette smokers than non-smokers (Barnett et al., 2013; Lee et al., 2014), it stands to reason that the number of hookah users, both current and lifetime, will be greater in this sample than in a general population of college students.
Baseline comparisons of hookah users and non-users resulted in a large number of significant differences across groups. First, hookah users in our sample were younger, with a mean age of 21.5. These findings support prior research documenting increased hookah use with decreased age. Each year in age decreased the odds that participants were dual users of hookah and cigarettes by approximately 20% (Jarrett et al., 2012). Previous research also supports our findings that males are more likely than females to be hookah and cigarette users (Cobb et al., 2012; Jarrett et al., 2012). Hookah users in our sample averaged more drinking days and were more likely to binge drink. They were also more likely to cite “drinking alcohol” and “smoking at parties” as reasons for relapse after a quit attempt. Previous research has found that students who used alcohol, marijuana, or other drugs had increased odds of being both hookah and cigarette users than being cigarette-only smokers (Jarrett et al., 2012). Hookah users also scored higher on impulsivity measures, indicating that they may be more likely to act without thinking (motor impulsiveness subscale), demonstrate less forethought (non-planning impulsiveness), and have a greater inability to concentrate (attentional impulsiveness). Further, hookah users had more social influence to smoke cigarettes when compared to cigarette only smokers. Cobb and colleagues found that hookah users were more likely to report being influenced by friends to smoke hookah and were more likely to perceive peers who smoked hookah as “cool” or “very cool” (Cobb et al., 2012).
When examining cigarette use, hookah users smoked fewer cigarettes per day on average than non-users and were less likely to be nicotine dependent. However, they were also significantly less likely to be abstinent at end of treatment (4 months) and less likely to achieve continuous abstinence at 6 months, indicating hookah users may have a more difficult time quitting and staying quit. Hookah users were also more likely to use other tobacco products, including smokeless tobacco and cigars/pipes and made more quit attempts on average than cigarette only smokers.
The reasons hookah users had a more difficult time quitting are not known, however it is possible that hookah smoking serves as a catalyst for cigarette smoking. Hookah users in our sample scored significantly higher on the “cue exposure” subscale of the Wisconsin Inventory of Smoking Dependence Motives (WISDM) (Smith et al., 2010), indicating that smoking hookah may act as a cue or reminder to smoke cigarettes.
Results of this study suggest that concurrent use of hookah may serve as a barrier to attempts to achieve cigarette smoking abstinence. Specialized cessation programs or modules may be needed to address the specific cessation needs of hookah smokers. Further, increased effort is needed to educate college students on the hazards of hookah use. The relatively young age of hookah users in our study and in previous research gives rise to the question of the trajectory of their path. To our knowledge, no prior research has yet determined whether hookah smoking is a passing “phase” among young people or if the habit will follow them into adulthood. Longitudinal research is needed to address this gap in knowledge.
Study Limitations and Strengths
A limitation of this study is that it is observational in nature and, therefore, any identified associations cannot be interpreted as causal. The trial was not designed apriori to examine the impact of hookah smoking on tobacco cessation rates. Further, the sample consisted of cigarette smokers attending colleges in the Midwest who enrolled in a Quit and Win contest to quit smoking. Participants in this trial represent a self-selected group who are motivated to quit smoking in exchange for the opportunity to win financial incentives. Students enrolled in this study were more likely to be daily smokers (i.e., average number of days smoked in the past 30 was 28). Recent studies demonstrate a high rate of non-daily smoking among college students, with one study finding that 70% of college students were non-daily smokers (Sutfin et al., 2012) and another reporting the percent of non-daily smokers at 66% (Berg et al., 2012). Because non-daily smokers are less likely to identify themselves as smokers, they may be less likely to attempt to quit smoking (Berg et al., 2009) and therefore, may have been less likely to enroll in this trial. Therefore, we may have missed a sizeable number of non-daily smokers who concurrently smoke hookah. Future Quit and Win interventions should develop recruitment methods to target this population.
Despite these limitations, the results of this study add to the knowledge base of the demographic, tobacco-specific and psychosocial characteristics of hookah users compared to cigarette only users. Further, to our knowledge, it is the first study to report on the impact of hookah use in a tobacco cessation attempt.
Conclusion
In 2012, an estimated 38.1% of young adults were current users of one or more tobacco products (CDC, 2014). The use of multiple tobacco products is a concerning issue due to the potential increased risks of nicotine dependence and failure in quit attempts, when compared to cigarette use alone (Tomar et al., 2010). Given the young age of hookah use and the increased difficulty maintaining long-term cessation, it is evident that interventions need to be developed targeting users of both hookah and cigarettes.
Supplementary Material
Figure 1.
Study Flowchart
Highlights.
Hookah smokers were less likely to report 30-day abstinence at 4-month follow-up.
Continuous abstinence at 6-months was significantly lower among hookah users.
Concurrent use of hookah may serve as a barrier to attempts to quit smoking.
Hookah smokers average more drinking days and are more likely to be binge-drinkers.
Acknowledgments
This study was funded by the National Heart, Lung, and Blood Institute (5R01-HL094183-05, Thomas, PI).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Statement
The authors declare that there are no conflicts of interest.
The parent trial is registered with ClinicalTrials.Gov, NCT01096108.
References
- Ahmed B, Peyton J, Allen F, Benowitz N. Attitudes and Practices of Hookah Smokers in the San Francisco Bay Area. Journal of Psychoactive Drugs. 2011;43(2):146–152. doi: 10.1080/02791072.2011.587707. [DOI] [PubMed] [Google Scholar]
- Akl EA, Gaddam S, Gunukula SK, Honeine R, Jaoude PA, Irani J. The effects of waterpipe tobacco smoking on health outcomes: a systematic review. Int J Epidemiol. 2010;39:834–857. doi: 10.1093/ije/dyq002. [DOI] [PubMed] [Google Scholar]
- Association ACH. American College Health Association National College Health Assessment II: Reference Group Executive Summary Spring 2013. Hanover, MD: 2013. [Google Scholar]
- Aoun BZ, Pascale S, Waked M. Saliva Cotinine and Exhaled Carbon Monoxide Levels in Natural Environment Waterpipe Smokers. Inhalation Toxicology. 2007;19(9):771–777. doi: 10.1080/08958370701401699. [DOI] [PubMed] [Google Scholar]
- Barnett TE, Smith T, He Y, Soule EK, Curbow BA, Tomar SL, McCarty C. Evidence of emerging hookah use among university students: a cross-sectional comparison between hookah and cigarette use. BMC Public Health. 2013;13:302. doi: 10.1186/1471-2458-13-302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg CJ, Lust KA, Sanem JR, Kirch MA, Rudie M, Ehlinger E, Ahluwalia JS, An LC. Smoker Self-Identification Versus Recent Smoking Among College Students. Am J Prev Med. 2009;36:333–336. doi: 10.1016/j.amepre.2008.11.010. [DOI] [PubMed] [Google Scholar]
- Berg CJ, Sutfin EL, Mendel J, Ahluwalia JS. Use of and interest in smoking cessation strategies among daily and nondaily college student smokers. J Am Coll Health. 2012;60:194–202. doi: 10.1080/07448481.2011.586388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. National Center for Chronic Disease Prevention and Health Promotion. National Youth Tobacco Survey (NYTS); 1999. [Google Scholar]
- Centers for Disease Control and Prevention (US) The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. 2014. [PubMed] [Google Scholar]
- Cobb CO, Khader Y, Nasim A, Eissenberg T. A multiyear survey of waterpipe and cigarette smoking on a US university campus. J Am Coll Health. 2012;60:521–527. doi: 10.1080/07448481.2012.692416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- Eissenberg T, Shihadeh A. Waterpipe tobacco and cigarette smoking: direct comparison of toxicant exposure. Am J Prev Med. 2009;37:518–523. doi: 10.1016/j.amepre.2009.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eissenberg T, Ward KD, Smith-Simone S, Maziak W. Waterpipe tobacco smoking on a U.S. College campus: prevalence and correlates. J Adolesc Health. 2008;42:526–529. doi: 10.1016/j.jadohealth.2007.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fielder R, Carey KB, Carey MP. Prevalence, frequency, and initiation of hookah tobacco smoking among first-year female college students: A one-year longitudinal study. Addictive Behaviors. 2012;37(2):221. doi: 10.1016/j.addbeh.2011.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths MA, Harmon TR, Gilly MC. Hubble bubble trouble: the need for education about and regulation of hookah smoking. J Public Policy and Marketing. 2011;30(1):119–132. [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. Br J Addict. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Jarrett T, Blosnich J, Tworek C, Horn K. Hookah use among U.S. college students: results from the National College Health Assessment II. Nic Tob Res. 2012;14:1145–1153. doi: 10.1093/ntr/nts003. [DOI] [PubMed] [Google Scholar]
- Lee YO, Bahreinifar S, Ling PM. Understanding tobacco-related attitudes among college and noncollege young adult hookah and cigarette users. J Am Coll Health. 2014;62:10–18. doi: 10.1080/07448481.2013.842171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenk K, Rode P, Fabian L, Bernat D, Klein E, Forster J. Cigarette use among young adults: comparisons between 2-year college students, 4-year college students, and those not in college. J Am Coll Health. 2012;60:303–308. doi: 10.1080/07448481.2011.607481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neergaard J, Singh P, Job J, Montgomery S. Waterpipe Smoking and Nicotine Exposure: A Review of the Current Evidence. Nicotine Tob Res. 2007;9(10):987–994. doi: 10.1080/14622200701591591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Primack BA, Sidani J, Agarwal AA, Shadel WG, Donny EC, Eissenberg TE. Prevalence of and associations with waterpipe tobacco smoking among U.S. university students. Ann Behav Med. 2008;36:81–86. doi: 10.1007/s12160-008-9047-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman S, Chang L, Hadgu S, Salinas-Miranda AA, Corvin J. Prevalence, Knowledge, and Practices of Hookah Smoking Among University Students, Florida. Prev Chronic Dis. 2014;11:14. doi: 10.5888/pcd11.140099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rigotti NA, Lee J, Wechsler H. US College Students; Use of Tobacco Products: Results of a National Survey. JAMA. 2000;284:699–705. doi: 10.1001/jama.284.6.699. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, Delafuente JR, Grant M. Development of the Alcohol-Use Disorders Identification Test (Audit) – WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol-Consumption. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Smith SS, Piper ME, Bolt DM, Fiore MC, Wetter DW, Cinciripini PM, Baker TB. Development of the Brief Wisconsin Inventory of Smoking Dependence Motives. Nic Tob Res. 2010;12:489–499. doi: 10.1093/ntr/ntq032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinella M. Normative data and a short form of the Barratt Impulsiveness Scale. The International journal of neuroscience. 2007;117:359–368. doi: 10.1080/00207450600588881. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2011 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-44, HHS. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012. [Google Scholar]
- Sutfin EL, McCoy TP, Berg CJ, Champion H, Helme DW, O'Brien MC, Wolfson M. Tobacco use by college students: a comparison of daily and nondaily smokers. Am J Health Behav. 2012;36:218–229. doi: 10.5993/AJHB.36.2.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutfin EL, McCoy TP, Reboussin BA, Wagoner KG, Spangler J, Wolfson M. Prevalence and correlates of waterpipe tobacco smoking by college students in North Carolina. Drug Alcohol Depend. 2011;115:131–136. doi: 10.1016/j.drugalcdep.2011.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomar SL, Alpert HR, Connolly GN. Patterns of dual use of cigarettes and smokeless tobacco among US males: findings from national surveys. Tob Control. 2010;19:104–109. doi: 10.1136/tc.2009.031070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welsch SK, Smith SS, Wetter DW, Jorenby DE, Fiore MC, Baker TB. Development and validation of the Wisconsin Smoking Withdrawal Scale. Exp Clin Psychopharmacol. 1999;7:354–361. doi: 10.1037//1064-1297.7.4.354. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.