Abstract
This study examines sources of referral for prescription opioid admission to substance use disorder treatment facilities and their relative completion success rates using secondary analysis of an existing data set (Treatment Episode Datasets – Discharge). Five years of data from public and private treatment facilities were extracted for client discharges with no prior treatment (N = 2,909,884). Healthcare professionals account for very few referrals to treatment (<10%). Prescription opioid clients referred into treatment had lower treatment success compared to other substance clients and when referred by healthcare providers had lower success rates (OR = 0.72, 95% CI 0.70 – 0.75) than clients from other referral sources. Fewer treatment referrals for prescription opioid misuse by healthcare providers and lower success rates are significant and timely findings due to the prevalence of prescription opioid misuse. Healthcare providers are well positioned to refer early for prescription opioid misuse and continue support of their patients during treatment.
Keywords: prescription opioid, healthcare referral, substance abuse, treatment outcomes
1. Introduction
Opioid use disorder is a complex public health problem that has created major human and societal costs. In 2013 in the United States, opioid use disorder associated with prescription opioids affected 1.8 million Americans, and opioid use disorder associated with heroin affected 517,000 (Substance Abuse and Mental Health Services Administration, 2014). Prescription opioid (PO) misuse results in significant morbidity and mortality often due to unintentional overdose (Dunn et al., 2010). Since 2004, emergency room visits related to POs increased 153%, or over 220,000 visits (Substance Abuse and Mental Health Services Administration, 2013), and the deaths from PO overdose out-numbered death from motor vehicle accidents (Centers for Disease Control and Prevention, 2011). The growth of this problem suggests a need to investigate PO admissions to treatment and successful treatment completions. Given the importance and increasing health care contacts with PO users, it is important to understand who is currently referring those presenting with PO as a problem substance. Furthermore, it is important to understand how referral sources are associated successful treatment completion.
Successful treatment completion is a clinically meaningful outcome measure predictive of long-term outcomes such as decreased criminal involvement, fewer treatment readmissions (Evans, Li, & Hser, 2009; Garnick, Lee, Horgan, & Acevedo, 2009; Zarkin, Dunlap, Bray, & Wechsberg, 2002), employment, and income one year following treatment (Arria et al., 2003). Furthermore, successful treatment completion data is useful in public health analyses (Alterman, 2001; Garnick et al., 2009). Referral source is associated with treatment success (Arndt, Acion, & White, 2013; Atkinson, Misra, Ryan, & Turner, 2003). For example, for all substances, employer and criminal justice referrals predict the highest percentage of successful completion rates, while self-referrals and healthcare referrals (HCR) predict the lowest percentage of success (Arndt et al., 2013; Evans et al., 2009; Friedmann, Lemon, Stein, & D’Aunno, 2003; Kelly, Finney, & Moos, 2005; Perron & Bright, 2008; Wild, Cunningham, & Ryan, 2006). Coercion may be a factor for completion success rate for treatment (Wild et al., 2006). For instance, criminal justice system referrals mandate treatment and keep clients in the treatment programs longer (Perron & Bright, 2008). Longer retention in a treatment program is generally associated with better post-treatment outcomes (National Institute on Drug Abuse, 2010; Perron & Bright, 2008). However, self-referral and HCR clients are associated with lower success in treatment completion (Arndt et al., 2013). The recent Federal initiative for screening, brief intervention, and referral to treatment (SBIRT) in primary healthcare for patients misusing alcohol and illicit drugs highlighted the relevance of this investigation as SBIRT aims to increase HCRs (Urada, Teruya, Gelberg, & Rawson, 2014). While there is an urgent need for screening and intervention of PO problems, referral and treatment outcomes for clients with PO admissions is relatively unexplored.
The purpose of this study was to explore PO admissions to treatment facilities and their associated successful treatment completions. We speculated that referral rates for treatment admissions for PO use disorder by healthcare professionals (HCP) would be lower compared with other referrals sources. In addition, successful treatment completion rates for PO admissions would be lower compared with other substances. In addition, we presented descriptive data on treatment admissions identifying with PO as the primary problem substance.
2. Material and Methods
2.1 Participants and Selection
This study was a secondary analysis of an existing data set from the Substance Abuse and Mental Health Services Administration. Admission and discharge information is requested from all public and private, urban and rural county addictions treatment facilities receiving public funding in the United States. These data were drawn from the Treatment Episode Datasets – Discharge (TEDS-D). TEDS consists of approximately 1.5 million annual admissions to licensed substance abuse treatment facilities making up a major proportion of all treatment admissions in the 50 states. Thus, results from TEDS are generalizable to those in licensed substance abuse treatment facilities. We used a concatenated 2006–2009 dataset (United States Department of Health and Human Services, 2009) and the 2010 dataset (United States Department of Health and Human Services, 2010) providing 5 years of discharge data (N = 8,096,795). TEDS-D data is collected on all admissions/discharges rather than each individual. We selected only those records where the client indicated no prior treatment (N = 3,014,422) to capture only first-time admission for analysis of individuals rather than multiple records for one person. Clients receiving medication assisted opioid therapy (e.g., methadone) were excluded resulting in our final analytic sample (N = 2,909,884). Medication assisted opioid therapy is viewed by some researchers (Bluthenthal, Jacobson, & Robinson, 2007; Guerrero et al., 2013) as an ongoing, indeterminate treatment that can misrepresent retention outcomes. Because these were secondary analyses of de-identified data, the University of Iowa Human Subjects Office, IRB exempted this study from review.
2.2 Measures
The main outcomes were successful substance abuse treatment completion status at discharge, and length of stay. TEDS data include demographic information and treatment characteristics collected on admission by agency staff. Continuous variables such as age were categorized due to confidentiality concerns. Participants were mostly male. Race/ethnic groups were determined by self-report and combined into White (non-Hispanic/Latino ethnicity), Black (Black/African American regardless of ethnicity), Hispanic (Puerto Rican, Mexican, Cuban, Central or South American or any other Spanish cultural origin), and Other (Native American, Asian, or other racial groups). Participants were categorized to either a POs group or Other Substance group (including heroin and alcohol). The PO group, our primary independent variable, consisted of admissions coded with “other opiates and synthetics” as their primary problem substance by TEDS. The “other opiates and synthetics” category include buprenorphine, codeine, Hydrocodone, hydromorphone, meperidine, morphine, opium, oxycodone, pentazocine, propoxyphene, tramadol, and any other drug with morphine-like effects. The PO group may consist of those misusing prescriptions or illegally obtained POs. Referral source was a major factor in our analyses. For one set of analyses, referral source was divided into HCR group (physician, psychiatrist, other licensed HCP, general hospital, psychiatric hospital, mental health program, or nursing home) or Other (individual/self, alcohol/drug abuse care providers, school/educational settings, employers/EAPs, courts/criminal justice agencies, and other community referrals).
The primary outcome variable of successful treatment completion was originally coded into several categories by treatment agency staff, and reduced to fewer subcategories by TEDS. We dichotomized successful treatment completion as “Treatment Completed” versus all other reasons (e.g., left against professional advice, terminated by facility, incarcerated, transferred, other). The secondary outcome of Length of stay was defined by month-long intervals. Due to varied ranges provided by TEDS, frequencies in this analysis are in 1-month intervals and include discharges throughout the interval. Discharges were categorized in between 1 and 30 days were categorized as 1 month. Discharges between 31 and 60 days were categorized as 2 months, and so on.
2.3 Statistical Analysis
Basic chi-square was used to analyze differences between categorical variables. Logistic regression and estimated marginal probabilities (expressed as percentages) for multivariate analyses, predicted PO admission or referral from HCPs and successful treatment completion. Effect sizes were calculated using the probabilistic index (PI) and odds ratios (OR). A PI of 0.5 is the base and indicates no effect whatsoever, a PI < 0.56 is small, < 0.64 medium, and 0.7 is large (Acion, Peterson, Temple, & Arndt, 2006). Small differences would be considered statistically significant using p < 0.05. Because of the very large sample size and number of tests, the threshold for significance was set to 0.0001 to avoid a type I error. Risk differences greater than 5 percentage points were considered clinically meaningful measures of effect as were odds ratios greater than 2.0. Previous research has followed this effect size threshold in analysis of TEDS data (Sahker, Toussaint, Ramirez, Ali, & Arndt, 2015).
3. Results
3.1 Demographic data
Clients with primary substance as PO were more likely female and white when compared to the “other substance” group. Among the other substances group, Blacks and Hispanic/Latinos were almost 5 and 4 times more likely, respectively. Nearly 44% of those admitted for POs were between the ages of 21 and 29 in contrast to those among the other substances group where only 27.65% were in this age interval. There were fewer younger and older clients in the PO group than in other substances group. While there was an overall significant difference in age (Mann-Whitney z = 7.73, p < 0.0001) the effect size was trivial (PI < 0.51). The people with PO admissions were more often unemployed, retired or disabled, living independently, currently married and less often supporting themselves from wages and salary in comparison to the other substance group.
3.2 Referral Sources
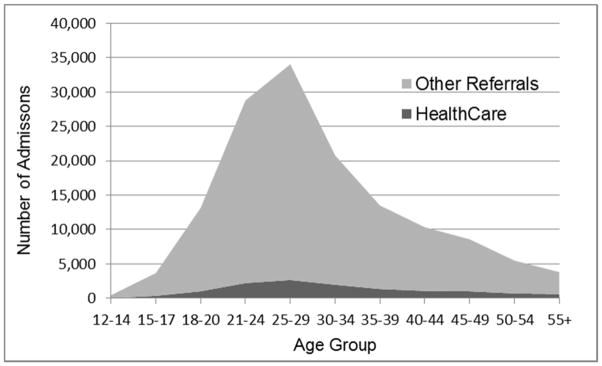
Substance use treatment information appears in Table 1 comparing the PO and other substance groups. The PO group had considerably more self-referrals and fewer criminal justice referrals compared to the other substances. While there were more HCR among the PO admissions (chi-square = 3,664.55, df = 1, p < 0.0001) the difference of 3.78 percentage points missed our criterion of 5.0 to be considered clinically meaningful. HCR were generally low in both groups (PO and other substances) and were only slightly less than 10% for the PO clients. Figure 1 shows the number of HCPs and other referral source admissions by age group where POs were the primary problem substance.
Table 1.
Treatment Characteristics of Prescription Opioid and Other Drug Discharges
| Other Substance % |
Prescription Opioids % |
|
|---|---|---|
| (n = 2,764,846) | (n = 145,038) | |
| Referral Source*** | ||
| Individual, Self | 24.91 | 47.00 |
| Alcohol/Drug Abuse | 6.29 | 11.71 |
| Healthcare Professional | 5.40 | 9.18 |
| School (Educational) | 2.27 | 0.37 |
| Employer/EAP | 0.86 | 0.87 |
| Other Community Referral | 12.83 | 10.90 |
| Criminal Justice | 47.43 | 19.96 |
| Service Setting*** | ||
| 24 Hour Detox Hospital | 0.72 | 2.05 |
| 24 Hour Detox Residential | 11.54 | 24.59 |
| Rehab Hospital | 0.31 | 0.55 |
| Rehab Short-Term | 9.39 | 16.87 |
| Rehab Long-Term | 7.05 | 6.28 |
| Intensive Outpatient | 13.41 | 12.77 |
| Non-Intensive Outpatient | 56.97 | 34.71 |
| Ambulatory Detoxification | 61 | 2.17 |
| Discharge Reason*** | ||
| Treatment Completed | 46.91 | 38.61 |
| Left Against Advice | 24.11 | 25.37 |
| Terminated by Facility | 6.49 | 6.28 |
| Transferred | 14.49 | 20.78 |
| Incarcerated | 1.69 | 1.16 |
| Death | 0.19 | 0.30 |
| Other | 6.12 | 7.49 |
| Length of Stay*** | ||
| Up to 30 Days | 37.70 | 62.76 |
| 31–60 Days | 15.93 | 12.33 |
| 61–90 Days | 11.39 | 7.05 |
| 91–120 Days | 9.63 | 5.13 |
| 120 or More Days | 25.35 | 12.73 |
| Length of Stay Successful Clients*** | ||
| (N=1,353,013) | (n = 1,297,017) |
(n = 55,996) |
| Up to 30 Days | 31.79 | 63.43 |
| 31–60 Days | 13.31 | 10.45 |
| 61–90 Days | 11.22 | 6.16 |
| 91–120 Days | 11.50 | 5.18 |
| 120 or More Days | 32.18 | 14.77 |
Note.
p<.0001, χ2 test for difference; Bold, clinically meaningful difference of 5% or greater
Fig. 1.
Number of opioid admissions by referral source and age group.
The HCR versus other referrals, for PO admissions were analyzed by age, race, gender, and employment status. Demographic differences between HCRs and other referral sources among the PO admissions (Table 2) showed marginally more females among the referrals coming from healthcare. HCRs were also somewhat older (Mann-Whitney z = −19.66, p < 0.0001). The racial make-up of the two referral groups, HCR or other referrals, were very similar although there were slightly more whites among the HCR (chi-square = 4772, df = 1, p < 0.0001). Moreover, while statistically significant, there were few differences in employment status. The largest differences occurred in the reasons the client was not in the labor force. For example, admissions from HCR more often included those who were retired, disabled, or not in the labor force due to other reasons. HCRs were less common for those reporting no income or were in dependent living situations compared to other referral sources. HCRs were more likely to occur for those living independently.
Table 2.
Prescription Opioid Group Referral Source and Demographic Discharge Characteristics
| Other Referral % |
Healthcare Referral % |
|
|---|---|---|
| (n = 131,951) | (n = 13,087) | |
| Gender*** | ||
| Male | 51.71 | 47.47 |
| Female | 48.29 | 52.53 |
| Age*** | ||
| 12–14 | 0.33 | 0.27 |
| 15–17 | 2.60 | 2.78 |
| 18–20 | 9.35 | 7.89 |
| 21–24 | 20.45 | 16.96 |
| 25–29 | 24.18 | 20.34 |
| 30–34 | 14.49 | 15.15 |
| 35–39 | 9.38 | 10.33 |
| 40–44 | 7.15 | 8.27 |
| 45–49 | 5.86 | 7.83 |
| 50–54 | 3.70 | 5.45 |
| 55 + | 2.50 | 4.72 |
| Race/Ethnicity*** | ||
| White | 86.04 | 88.22 |
| Black | 4.19 | 2.94 |
| Hispanic | 6.42 | 5.20 |
| Other | 3.34 | 3.64 |
| Employment Status*** | ||
| Full-Time | 17.28 | 17.95 |
| Part-Time | 7.17 | 7.91 |
| Unemployed | 41.51 | 43.06 |
| Not in Labor Force | 34.04 | 31.09 |
| Detail Not in Labor Force*** | ||
| Homemaker | 7.46 | 9.73 |
| Student | 11.35 | 13.18 |
| Retired/Disabled | 21.69 | 37.24 |
| Inmate of Institution | 6.77 | 0.67 |
| Other | 52.72 | 39.17 |
Note.
p<.0001, χ2 test for difference; Bold, clinically meaningful difference of 5% or greater
3.3 Treatment service setting
The most common setting for treatment services for all referral types and all substances was outpatient treatment, however, fewer clients from HCRs and PO admissions were referred there (Table 3). Compared to other referral sources, HCR clients were more often placed in short-term, long-term, or 24-hour residential detoxification settings. Compared to other substance clients, PO clients were more likely to be detoxified in a free standing, 24-hour detoxification setting, and more likely to be admitted to short-term residential treatment (<30 days).
Table 3.
Prescription Opioid Group Referral Source and Demographic Discharge Characteristics (continued)
| Other Referral % |
Healthcare Referral % |
|
|---|---|---|
| (n = 131,951) | (n = 13,087) | |
| Income/Support*** | ||
| Wages/Salary | 30.92 | 32.78 |
| Public Assistance | 4.09 | 5.99 |
| Retirement/Pension | 5.27 | 9.42 |
| Other | 25.28 | 23.79 |
| None | 34.44 | 28.02 |
| Living Arrangements*** | ||
| Homeless | 5.87 | 6.49 |
| Dependent Living | 17.93 | 11.74 |
| Independent Living | 76.21 | 81.77 |
| Marital Status*** | ||
| Never Married | 54.34 | 49.16 |
| Now Married | 23.00 | 26.75 |
| Separated | 5.87 | 7.05 |
| Divorced/Widowed | 16.79 | 17.05 |
| Age at First Use*** | ||
| 11 and Under | 1.36 | 1.92 |
| 12–14 | 6.55 | 6.32 |
| 15–17 | 18.62 | 16.85 |
| 18–20 | 21.15 | 18.24 |
| 21–24 | 17.67 | 15.62 |
| 25–29 | 14.05 | 14.07 |
| 30–34 | 7.97 | 9.24 |
| 35–39 | 5.20 | 6.21 |
| 40–44 | 3.62 | 4.96 |
| 45–49 | 2.17 | 3.46 |
| 50–54 | 1.05 | 1.97 |
| 55 + | 0.59 | 1.15 |
| Service Setting*** | ||
| 24 Hour Detox Hospital | 2.92 | 1.97 |
| 24 Hour Detox Residential | 21.92 | 24.86 |
| Rehab Hospital | 1.37 | 0.47 |
| Rehab Short-Term | 12.19 | 17.34 |
| Rehab Long-Term | 3.86 | 6.52 |
| Intensive Outpatient | 13.13 | 12.73 |
| Non-Intensive Outpatient | 42.53 | 33.94 |
| Ambulatory Detoxification | 2.07 | 2.18 |
Note.
p<.0001, χ2 test for difference; Bold, clinically meaningful difference of 5% or greater
3.4 Discharge status
Successful discharge from treatment indicates the client completed all the components of the program. There were important differences in 1) the success rates for PO admissions compared to other substances and 2) the success rates for HCRs compared to other referral sources.
Considerably fewer clients in the PO group were successfully discharged from treatment (chi-square = 3,815.43, df = 1, p < 0.0001) as compared to other substances. However, the relative increased number of clients transferred for additional treatment (e.g., after a detoxification program) may have contributed to this difference. Even so, there were lower treatment success rates for PO admissions compared to other substance clients in each service setting, as shown by stratified analyses. For example, among hospital detoxification clients, 63.9% of PO clients successfully completed compared to 74.4% of other clients. Among ambulatory, non-intensive outpatient treatment, 26.8% of PO clients successfully completed in contrast to 45.1% of those clients presenting with other substances. Thus, the PO clients had lower success rates across all treatment service settings.
PO clients referred into treatment by HCPs had lower success rates than clients from other referral sources. Table 4 shows discharge outcomes for PO admissions from HCR versus other sources. Using logistic regression, predicting successful completion from referral source showed a highly significant difference (OR = 0.72, 95% CI 0.70 – 0.75, Wald z = 16.6, p < 0.0001) with HCRs showing a lower success rate than the other referral sources. The estimated reduction in successful discharges from HCRs was a 7.43 percentage points (95% CI: 6.59 – 8.27). A follow-up logistic regression was done controlling for client sex, age, race/ethnicity, employment status, primary source of income, living arrangement, marital status, age of first use, geographical location of service (state), and service setting. HCRs continued to show a lower successful completion rate (OR = 0.84, 95% CI: 0.79 – 0.89, Wald z = 6.14, p < 0.0001) although the effect was attenuated. The covariate adjusted success rate for HCRs was 37.2% and for other referral sources was 41.4%, a difference of 4.17 percentage points (95% CI: 2.8 – 5.5).
Table 4.
Prescription Opioid Group Referral Source and Outcomes
| Other Referral % |
Healthcare Referral % |
|
|---|---|---|
| (n = 131,951) | (n = 13,087) | |
| Discharge Reason*** | ||
| Treatment Completed | 39.28 | 31.85 |
| Left Against Advice | 24.85 | 30.65 |
| Terminated by Facility | 6.32 | 5.92 |
| Transferred | 20.61 | 22.41 |
| Incarcerated | 1.21 | 0.68 |
| Death | 0.29 | 0.39 |
| Other | 7.43 | 8.10 |
| Length of Stay*** | ||
| Up to 30 Days | 62.67 | 63.61 |
| 31–60 Days | 12.20 | 13.69 |
| 61–90 Days | 7.09 | 6.64 |
| 91–120 Days | 5.17 | 4.71 |
| 120 or More Days | 12.87 | 11.35 |
Note.
p<.0001, χ2 test for difference; Bold, clinically meaningful difference of 5% or greater
Length of stay was also shorter for those referred by HCPs (Mann-Whitney z = 9.10, p < 0.0001) compared to all other sources, however, this comparison was complicated by the differences in service settings. Stratified analyses within each service setting produced significant differences in all situations. However, HCR admissions tended to stay longer in detoxification settings than clients referred from other sources. In all other settings, HCR clients stayed a shorter period.
4. Discussion
Analysis of admissions into treatment for problems with PO use provided important findings. These findings included (1) few referrals came from HCPs, (2) white and female clients had a higher percentage of admissions for PO use than other substances, (3) the completion success rates for PO admissions was lower than other substance admissions.
Less than 10% of PO treatment admissions came from HCRs, whereas the largest source was self-referrals (47%). The low percentage of HCR was consistent with findings from a study of older adults admitted for SUD treatment (Arndt, Clayton, & Schultz, 2011). Furthermore, the current study showed lower successful completion rates associated with HCRs, which may have been because HCR sources favored short-term detoxification settings rather than the more commonly directed outpatient treatment (See Table 2). The preference for shorter recovery programs by healthcare professionals may be potentially associated with the poorer outcomes observed in HCRs. Further research could investigate HCR to longer term, more intensive outpatient programs by and PO treatment services across referral sources. Overall, there is a general lack of understanding of SUD and its treatment throughout the healthcare system which may be the reason screening for SUD does not occur in a consistent manner (Lawrence, Rasinski, Yoon, & Curlin, 2013; Swenson-Britt, Carrougher, Martin, & Brackley, 2000). In a study of over 23,000 adults receiving health maintenance examinations, one in six patients reported HCPs spoke to them about alcohol use (Arndt, Schultz, Turvey, & Petersen, 2002). This small number of physician discussions for alcohol may mean even lower numbers for PO discussions. Future research on PO physician interventions and discussions would further improve the current understanding.
Criminal justice (19.9%) referral for PO use disorder was lower than for other substances (47.43%), however, illegal PO use is more difficult to determine (SAMHSA, 2013). Additionally, self-referral into treatment for misuse of POs was comparatively high (47%). High self-referrals and lower treatment completion supports existing research suggesting coercion increased treatment completion (Wild et al., 2006).
The demographics of those admitted into treatment for PO use disorder compared to other substances indicated they were predominantly White, in their late 20s, never married, and lived independently. The gender makeup for PO admissions to treatment was about 50/50 male/female compared to a 2-to-1 ratio for all other substances. The current gender makeup supports previous findings of PO dependence (Back, Lawson, Singleton, & Brady, 2011; Parsells Kelly et al., 2008). Furthermore, women were more likely than men to report their first exposure to PO (Back et al., 2011; Maremmani et al., 2010; McHugh et al., 2013), be prescribed PO (Campbell et al., 2010; McHugh et al., 2013; Pokela, Simon Bell, Lihavainen, Sulkava, & Hartikainen, 2010; Sadowski, Carrie, Grymonpre, Metge, & St John, 2009), and experienced PO overdose deaths (Centers for Disease Control and Prevention, 2013). These finding support the need for a greater focus on women and PO prescription, misuse, and now, treatment outcomes.
These data have limitations of note. First, some data were collected from self-report, this affects validity. For example, clients may have actually been referred by health care sources, but upon admission to a treatment facility, they reported self-referral. Unfortunately this cannot be accounted for in these data. Second, the present study measured successful treatment completion and length of stay as the outcome measures. Improved measures of treatment success as an outcome variable could investigate substance use and abstinence data beyond treatment. Future research should focus on longitudinal designs. Third, an interaction between successful treatment completion and referral source or secondary problem substances was not hypothesized a priori. Through exploring the data, an interesting association between HCR and PO admissions was found. Future research could investigate the moderating effects of referral source and other problem substances on PO treatment completion. Fourth, there is an important distinction between PO misuse arising from a legitimate prescription for a pain condition, versus abuse arising from street acquired PO pills. Unfortunately, this distinction cannot be drawn from the data and is needed to be investigated in future PO studies. Fifth, TEDS defines transfers as, “Client was transferred to another substance abuse treatment program, provider or facility within an episode of treatment.” This may include transfers to either greater or lesser levels of care. Ultimately, transfers are unclear and unstandardized, thus, including transfers in the successful category may misrepresent total successful completion. Those transferred out of a facility, are not counted as additional treatment episodes as the current study includes only first time episodes. Counting transfers as successful completions may misrepresent “success” across different states. Finally, some admissions in the TEDS database depended on external factors such as public fund availability. States might have used their funds to target specific groups such as pregnant women and adolescents. These admissions may not have captured all substance abuse treatment admissions. However, the TEDS database attempts to include all admissions to any provider that receives public funding. Another limitation involved individuals’ self-report for several of the variables, which may have affected the reliability and validity of the data.
5. Conclusions
The clinically meaningful findings of low HCP referral rates and low treatment success for those with PO use disorder identified a major gap in care and treatment delivery. Possible solutions include (1) HCPs universally and routinely screen for PO misuse, especially when prescribing opioids for pain, and early referral to treatment when objective findings through screening indicate high risk for misuse, (2) maintaining client, substance abuse treatment and healthcare team relationships once the client is in treatment.
Finally, HCPs can improve care by focusing on PO misuse among women. Given the sharp rise in deaths related to PO misuse in women (Centers for Disease Control and Prevention, 2013) and findings of HCPs prescribing PO more for women (Campbell et al., 2010; McHugh et al., 2013; Pokela et al., 2010; Sadowski et al., 2009), there is a need for thorough evaluations of pain symptoms and risks such as past year substance use of other drugs and serious mental health conditions (Tetrault et al., 2008). If POs are needed for the management of pain, monitoring through evidenced based screening and monitoring tools and frequent healthcare encounters, drug screenings, and medication management may result in safe and effective care.
Acknowledgments
Author contributions:
Dr. Arndt, and Mr. Sahker had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: All authors. Acquisition of data: Arndt, Sahker. Analysis and interpretation of data: All authors. Drafting of the manuscript: All authors. Editing of the manuscript prior to submission: All authors. Critical drafting and revisions: St. Marie. Administrative, technical, and material support: All Authors. Final approval of the version to be published: St. Marie. Accountability agreement: All authors.
Dr. St. Marie disclosures include Postdoctoral Pain and Associated Symptoms Training grant from NINR/NIH, T32 NR011147; had received funding for other research projects from the Nurse Practitioner Healthcare Foundation and the American Society for Pain Management Nursing. She serves on the Advisory Board for Risk Evaluation and Mitigation Strategies (REMS) through CORE.
Ethan Sahker has nothing to disclose.
Dr. Stephan Arndt has nothing to disclose.
References
- Acion L, Peterson JJ, Temple S, Arndt S. Probabilistic index: An intuitive non-parametric approach to measuring the size of treatment effects. Statistics in Medicine. 2006;25(4):591–602. doi: 10.1002/sim.2256. [DOI] [PubMed] [Google Scholar]
- Alterman AI, Langenbucher J, Morrison RL. State-level treatment outcome studies using administrative databases. Evaluation Review. 2001;25:162–183. doi: 10.1177/0193841X0102500203. [DOI] [PubMed] [Google Scholar]
- Arndt S, Acion L, White K. How the states stack up: Disparities in substance abuse outpatient treatment completion rates for minorities. Drug Alcohol Dependence. 2013;132(3):547–554. doi: 10.1016/j.drugalcdep.2013.03.015. [DOI] [PubMed] [Google Scholar]
- Arndt S, Clayton R, Schultz SK. Trends in substance abuse treatment 1998–2008: Increasing older adult first-time admissions for illicit drugs. The American Journal of Geriatric Psychiatry. 2011;19(8):704–711. doi: 10.1097/JGP.0b013e31820d942b. [DOI] [PubMed] [Google Scholar]
- Arndt S, Schultz SK, Turvey C, Petersen A. Screening for alcoholism in the primary care setting: Are we talking to the right people? Journal of Family Practice. 2002;51(1):41–50. [PubMed] [Google Scholar]
- Arria AM, Goldkang S, Rusinko W, Luongo PF, Hsu M, Lee A, Krause H. Drug treatment completion and post-discharge employment in the topps-ii interstate cooperative study. Journal of Substance Abuse Treatment. 2003;25(1):9–18. doi: 10.1016/s0740-5472(03)00050-3. [DOI] [PubMed] [Google Scholar]
- Atkinson RM, Misra S, Ryan SC, Turner JA. Referral paths, patient profiles and treatment adherence of older alcoholic men. Journal of Substance Abuse Treatment. 2003;25(1):29–35. doi: 10.1016/s0740-5472(03)00048-5. http://dx.doi.org/10.1016/S0740-5472(03)00048-5. [DOI] [PubMed] [Google Scholar]
- Back SE, Lawson KM, Singleton LM, Brady KT. Characteristics and correlates of men and women with prescription opioid dependence. Addictive Behaviors. 2011;36(8):829–834. doi: 10.1016/j.addbeh.2011.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluthenthal RN, Jacobson JO, Robinson PL. Are racial disparities in alcohol treatment completion associated with racial differences in treatment modality entry? Comparison of outpatient treatment and residential treatment in los angeles county, 1998 to 2000. Alcoholism: Clinical and Experimental Research. 2007;31(11):1920–1926. doi: 10.1111/j.1530-0277.2007.00515.x. [DOI] [PubMed] [Google Scholar]
- Campbell CI, Weisner C, LeResche L, Ray GT, Saunders K, Sullivan MD, Boudreau D. Age and gender trends in long-term opioid analgesic use for noncancer pain. American Journal of Public Health. 2010;100(12):2541–2547. doi: 10.2105/AJPH.2009.180646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Policy Impact: Prescription Painkiller Overdoses. 2011 Retrieved, from http://www.cdc.gov/homeandrecreationalsafety/pdf/policyimpact-prescriptionpainkillerod.pdf.
- Centers for Disease Control and Prevention. New CDC Vital Signs: Prescription Pain Killer Epidemic among Women. 2013 Retrieved, from http://www.cdc.gov/media/dpk/2013/dpk-Prescription%20drug%20overdose.html#graphics.
- Dunn KM, Saunders KW, Rutter CM, Banta-Green CJ, Merrill JO, Sullivan MD, Psaty BM. Opioid prescriptions for chronic pain and overdose: A cohort study. Annals of Internal Medicine. 2010;152(2):85–92. doi: 10.7326/0003-4819-152-2-201001190-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans E, Li L, Hser YI. Client and program factors associated with dropout from court mandated drug treatment. Evaluation and Program Planning. 2009;32(3):204–212. doi: 10.1016/j.evalprogplan.2008.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedmann PD, Lemon SC, Stein MD, D’Aunno TA. Community referral sources and entry of treatment-naive clients into outpatient addiction treatment. The American Journal of Drug and Alcohol Abuse. 2003;29(1):105–115. doi: 10.1081/ADA-120018841. [DOI] [PubMed] [Google Scholar]
- Garnick DW, Lee MT, Horgan CM, Acevedo A. Adapting washington circle performance measures for public sector substance abuse treatment systems. Journal of Substance Abuse Treatment. 2009;36(3):265–277. doi: 10.1016/j.jsat.2008.06.008. http://dx.doi.org/10.1016/j.jsat.2008.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerrero EG, Marsh JC, Duan L, Oh C, Perron B, Lee B. Disparities in completion of substance abuse treatment between and within racial and ethnic groups. Health Services Research. 2013;48(4):1450–1467. doi: 10.1111/1475-6773.12031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Finney JW, Moos R. Substance use disorder patients who are mandated to treatment: Characteristics, treatment process, and 1-and 5-year outcomes. Journal of Substance Abuse Treatment. 2005;28(3):213–223. doi: 10.1016/j.jsat.2004.10.014. [DOI] [PubMed] [Google Scholar]
- Lawrence RE, Rasinski KA, Yoon JD, Curlin FA. Physicians’ beliefs about the nature of addiction: A survey of primary care physicians and psychiatrists. The American Journal on Addictions. 2013;22(3):255–260. doi: 10.1111/j.1521-0391.2012.00332.x. [DOI] [PubMed] [Google Scholar]
- Maremmani I, Stefania C, Pacini M, Maremmani AGI, Carlini M, Golia F, Dell’Osso L. Differential substance abuse patterns distribute according to gender in heroin addicts. Journal of Psychoactive Drugs. 2010;42(1):89–95. doi: 10.1080/02791072.2010.10399789. [DOI] [PubMed] [Google Scholar]
- McHugh RK, DeVito EE, Dodd D, Carroll KM, Potter JS, Greenfield SF, Weiss RD. Gender differences in a clinical trial for prescription opioid dependence. Journal of Substance Abuse Treatment. 2013;45(1):38–43. doi: 10.1016/j.jsat.2012.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Drug Abuse. Drugs, Brains, and Behavior: The Science of Addiction. Bethesda, MD: National Institutes of Health, National Institute on Drug Abuse; 2010. [Google Scholar]
- Parsells KJ, Cook SF, Kaufman DW, Anderson T, Rosenberg L, Mitchell AA. Prevalence and characteristics of opioid use in the us adult population. PAIN. 2008;138(3):507–513. doi: 10.1016/j.pain.2008.01.027. http://dx.doi.org/10.1016/j.pain.2008.01.027. [DOI] [PubMed] [Google Scholar]
- Perron BE, Bright CL. The influence of legal coercion on dropout from substance abuse treatment: Results from a national survey. Drug and Alcohol Dependence. 2008;92(1–3):123–131. doi: 10.1016/j.drugalcdep.2007.07.011. http://dx.doi.org/10.1016/j.drugalcdep.2007.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pokela N, Simon Bell J, Lihavainen K, Sulkava R, Hartikainen S. Analgesic use among community-dwelling people aged 75 years and older: A population-based interview study. The American Journal of Geriatric Pharmacotherapy. 2010;8(3):233–244. doi: 10.1016/j.amjopharm.2010.05.001. http://dx.doi.org/10.1016/j.amjopharm.2010.05.001. [DOI] [PubMed] [Google Scholar]
- Sadowski CA, Carrie AG, Grymonpre RE, Metge CJ, St John P. Access and intensity of use of prescription analgesics among older manitobans. The Canadian Journal of Clinical Pharmacology. 2009;16(2):322–330. [PubMed] [Google Scholar]
- Sahker E, Toussaint MN, Ramirez M, Ali SR, Arndt S. Evaluating racial disparity in referral source and successful completion of substance abuse treatment. Addictive Behaviors. 2015;48:25–29. doi: 10.1016/j.addbeh.2015.04.006. http://dx.doi.org/10.1016/j.addbeh.2015.04.006. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Author; 2013. NSDUH Series H-46, HHS Publication No. (SMA) 13-4795. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Author; 2014. NSDUH series H-48, HHS publication no. (SMA) 14-4863. [PubMed] [Google Scholar]
- Swenson-Britt E, Carrougher G, Martin BW, Brackley M. Project hope: Changing care delivery for the substance abuse patient. Clinical Nurse Specialist. 2000;14(2):92–100. doi: 10.1097/00002800-200003000-00014. [DOI] [PubMed] [Google Scholar]
- Tetrault JM, Desai RA, Becker WC, Fiellin DA, Concato J, Sullivan LE. Gender and non-medical use of prescription opioids: Results from a national us survey. Addiction. 2008;103(2):258–268. doi: 10.1111/j.1360-0443.2007.02056.x. [DOI] [PubMed] [Google Scholar]
- United States Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Office of Applied Studies. Treatment Episode Data Set -- Discharges (TEDS-D), 2009. 2010 Retrieved from: http://doi.org/10.3886/ICPSR33621.v1.
- United States DeptDepartment of Health and Human Services, Substance Abuse and Mental Health Services Administration, Office of Applied Studies. Treatment Episode Data Set -- Discharges (TEDS-D) -- concatenated, 2006 to 2008. 2009 Retrieved from: http://doi.org/10.3886/ICPSR33621.v1.
- Urada D, Teruya C, Gelberg L, Rawson R. Integration of substance use disorder services with primary care: Health center surveys and qualitative interviews. Substance Abuse Treatment, Prevention, and Policy. 2014;9(1):15. doi: 10.1186/1747-597X-9-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wild TC, Cunningham JA, Ryan RM. Social pressure, coercion, and client engagement at treatment entry: A self-determination theory perspective. Addictive Behaviors. 2006;31(10):1858–1872. doi: 10.1016/j.addbeh.2006.01.002. http://dx.doi.org/10.1016/j.addbeh.2006.01.002. [DOI] [PubMed] [Google Scholar]
- Zarkin GA, Dunlap LJ, Bray JW, Wechsberg WM. The effect of treatment completion and length of stay on employment and crime in outpatient drug-free treatment. Journal of Substance Abuse Treatment. 2002;23(4):261–271. doi: 10.1016/s0740-5472(02)00273-8. http://dx.doi.org/10.1016/S0740-5472(02)00273-8. [DOI] [PubMed] [Google Scholar]