Abstract
Background & Aim
The ability of Staphylococcus aureus to successfully colonize (a)biotic surfaces may be explained by biofilm formation and the actions of virulence factors. The aim of the present study was to establish the presence of 52 proteins, including virulence factors such as alpha-toxin, during biofilm formation of five different (methicillin resistant) S. aureus strains on Leiden human epidermal models (LEMs) and polystyrene surfaces (PS) using a competitive Luminex-based assay.
Results
All five S. aureus strains formed biofilms on PS, whereas only three out of five strains formed biofilms on LEMs. Out of the 52 tested proteins, six functionally diverse proteins (ClfB, glucosaminidase, IsdA, IsaA, SACOL0688 and nuclease) were detected in biofilms of all strains on both PS and LEMs. At the same time, four toxins (alpha-toxin, gamma-hemolysin B and leukocidins D and E), two immune modulators (formyl peptide receptor-like inhibitory protein and Staphylococcal superantigen-like protein 1), and two other proteins (lipase and LytM) were detectable in biofilms by all five S. aureus strains on LEMs, but not on PS. In contrast, fibronectin-binding protein B (FnbpB) was detectable in biofilms by all S. aureus biofilms on PS, but not on LEMs. These data were largely confirmed by the results from proteomic and transcriptomic analyses and in case of alpha-toxin additionally by GFP-reporter technology.
Conclusion
Functionally diverse virulence factors of (methicillin-resistant) S. aureus are present during biofilm formation on LEMs and PS. These results could aid in identifying novel targets for future treatment strategies against biofilm-associated infections.
Introduction
Staphylococcus aureus (S. aureus) is the causative agent of a variety of infections with generally significant morbidity and mortality. The incidence of both hospital and community acquired infections caused by methicillin-resistant S. aureus (MRSA) has increased significantly in the last decades [1–3]. Unfortunately, the treatment of such infections is becoming increasingly complex as current antibiotics may be less effective due to resistance development and biofilm formation [4]. As the number of newly approved antimicrobial agents continues to decrease [5,6], alternative strategies for prevention and/or treatment of bacterial colonization and infection, such as a vaccines [7] and antimicrobial peptides [8], are urgently needed. To date no clinically successful vaccine against S. aureus has been developed, despite the promising results of vaccines targeting diverse virulence factors of this pathogen in animal models [9,10]. Currently, the awareness that multiple virulence factors of S. aureus should be targeted for any vaccine or other strategy to be successful is increasing [9]. Moreover, some relation between the expression of antibodies against S. aureus virulence factors and protection from infection has been made [11].
The capacity of S. aureus to cause infections is attributed to its vast array of virulence factors which include adhesive surface proteins, secreted immune modulators, enzymes and toxins [7]. Moreover, many infections such as those of (wounded) skin, mucosae and artificial surfaces [12] are believed to involve biofilm formation by S. aureus. Biofilms are defined as complex communities of bacteria encased in an extracellular polymeric matrix and biofilm formation is believed to contribute to bacterial virulence, reduced susceptibility to antibiotics [13–15] and reduced clearance by the immune system. Despite the plethora of studies examining the involvement of biofilm formation [16] and/or single virulence factors [17,18] in e.g. skin infections, so far only a few studies has focussed on the involvement of multiple virulence factors in association with biofilm formation by S. aureus during infection [19,20].
Biofilm formation by S. aureus on polystyrene (PS) has been extensively characterized before [21,22]. However, biofilm formation on human biotic surfaces is much less characterized and the associated pathogen-host interactions are unclear. Earlier we reported that Leiden epidermal models (LEMs) mimic the human skin in many ways, including epidermal morphology and barrier properties [23]. In addition, full thickness human skin equivalents have been used to study skin colonization by (methicillin resistant) S. aureus [24,25].
The aim of the current study was to establish the presence of 52 proteins, including virulence factors such as alpha-toxin, during biofilm formation by five different (methicillin-resistant) S. aureus strains on LEMs and PS. Using the novel competitive Luminex-based assay (CLA; [26] we detected six proteins (ClfB, glucosaminidase, IsdA, IsaA, SACOL0688 and nuclease) in biofilms of all biofilm-forming strains on the two surfaces. At the same time, surface- and strain-dependent differences were found for the presence of a wide range of other proteins, such as immune modulators and toxins like alpha-toxin.
Materials and Methods
Ethics statement
Human serum was obtained from healthy volunteers who gave written consent for use of serum solely for research purposes within the department of Medical Microbiology and Infectious Diseases at the Erasmus MC Rotterdam. Serum was coded, pooled and has been used for this and earlier studies [27,28]. The original list with documented volunteer names was only accessible to qualified physicians within the department, amongst the current authors only including PMdR. This sampling procedure was approved by the Medical Ethics Committee of the Erasmus Medical Center Rotterdam (MEC-2007-106, addendum 2) [28]. All primary human skin cells from healthy donors used by the Department of Dermatology are isolated from surplus tissue collected according to article 467 of the Dutch Law on Medical Treatment Agreement and the Code for proper Use of Human Tissue of the Dutch Federation of Biomedical Scientific Societies [29]. According to article 467, coded anonymous surplus tissue can be used if no objection is made by the patient. All patients were informed of the possibility that surplus tissue could be used for scientific research and all patients were offered the opportunity to give written refusal to this. Only tissue from patients who did not opt out was used. None of the authors were involved in the tissue sampling and only birth date, gender and skin type of the subjects were documented. These data were only accessible to EMH and PHN. Because this procedure, as published previously [8,24–25], is in accordance with national law and additional approval of an ethics committee regarding scientific use of surplus tissue is not required, we did not seek specific approval by our ethics committee. The Declaration of Helsinki principles were followed when working with human tissue.
Staphylococcus aureus strains
The following S. aureus strains were used in this study: methicillin-resistant strains LUH14616 (sequence type 247), a kind gift of dr. S. Croes [30]; LUH15051 (ST 239) obtained from dr. M.E.O.C. Heck, (Laboratory of Infectious Diseases and Screening, RIVM, Bilthoven, The Netherlands); USA300 strain Sac042w (ST 8) described earlier [31]; a strain derived from an impetigo patient LUH15091 (ST121) within the Erasmus Medical Center and NCTC 8325–4 (ST 8). All strains were typed using multi locus sequence typing (MLST) [27,32]. Before usage the strains were grown on sheep blood agar plates (Biomerieux).
Biofilm formation on polystyrene plates
A routine biofilm model was used as described before [21,22]. In short, overnight plate cultures of S. aureus were re-suspended in Iscove’s Modified Dulbecco’s Medium (IMDM, Life technologies, Carlsbad, CA, USA) without phenol red until an optical density (OD, 660nm) of 2 was reached. IMDM medium was chosen because of its significant impact on detectable levels of bacterial proteins, e.g. IsdA, ClfB and Efb, expressed by S. aureus biofilms on PS [26]. One μl of this bacterial suspension was added to 199 μl of TSB supplemented with 0.5% (wt/v) glucose and 3% (wt/v) NaCl or IMDM without any supplement in sterile 96-wells PS plates (Greiner Bio-one). Plates were then incubated at 37°C with gentle shaking at 200 rpm for various intervals. Biofilm mass was measured by staining with 1% crystal violet. OD was measured at 490 nm.
Leiden epidermal models
The epidermis and dermis of pieces of fresh plastic surgery surplus skin were enzymatically and mechanically separated, and each layer was subsequently digested to obtain single-cell suspensions [33]. The keratinocytes were cultured in keratinocyte medium, i.e. 3 parts DMEM (Gibco/Invitrogen) and 1 part Ham's F12 medium supplemented with 5% (v/v) fetal bovine serum (FBS; HyClone/Greiner), 0.5 μm hydrocortisone, 1 μm isoproterenol, 0.1 μm insulin (all from Sigma–Aldrich, Zwijndrecht, The Netherlands), 100 U/ml penicillin and 100 μg/ml streptomycin (both from Invitrogen). Leiden epidermal models (LEMs; Fig 1A) were made with these primary human keratinocytes as described before [34]. Briefly, one day before generation of the models, medium of the keratinocyte cultures was switched to Dermalife (Lifeline Cell Technology) supplemented with penicillin (10,000 U/ml) and streptomycin (10 mg/ml). The next day 2×105 keratinocytes were seeded onto a filter insert (0.4 μM Costar inserts; Corning) in 12-well plates in this Dermalife medium. Three days thereafter the apical medium was removed, leaving the keratinocytes air-exposed. The medium under the filter insert was switched to CnT-02-3D medium (CellnTech) mixed with keratinocyte medium supplemented with 2.4×10−2 μM bovine serum albumin and lipids/antibiotics as described above. One day before bacterial inoculation of the LEMs, the medium was switched to this medium without antibiotics. All experiments were performed on 10-day air-exposed cultures.
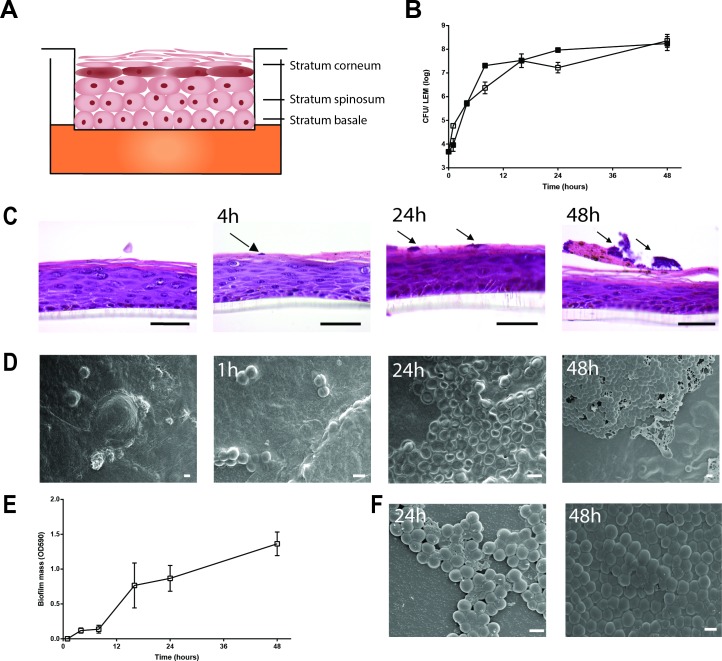
Fig 1. Biofilm formation by S. aureus LUH14616 on LEMs and PS surfaces.
(A) Schematic representation of LEM. (B) Bacterial counts were performed on LEM exposed to LUH14616 for various intervals. Adherent bacteria are represented by open symbols and non-adherent/loosely adherent bacteria by closed symbols. Results are displayed as the mean and SD of four experiments. (C) Haematoxilin and eosine staining of LEMs at various intervals after inoculation with LUH14616. Arrows indicate microcolonies, scale bars = 50 μm. (D) Cryo scanning electron microscopy of LEMs colonized with LUH14616 for various intervals. Photographs are representative for three different keratinocyte donors. (E) Biofilm formation by LUH14616 on PS in IMDM medium. Results are the mean and SEM of three experiments. (F) Cryo scanning electron microscopy of S. aureus LUH14616 biofilms formed on PS at 24 and 48 hrs after adherence to wells. Scale bars = 1 μm.
Colonization of Leiden epidermal model
LEMs were exposed for 1 h at 37°C in 7.3% CO2 to 300 μl of a log-phase bacterial suspension containing 3.3x105 CFU/ml. Next, the non-adherent bacteria were removed by aspiration and at different intervals thereafter, the viable detachable bacteria were collected in 1 ml of PBS, and serially diluted, and 50 μl of these samples were plated onto diagnostic sensitivity test (DST) agar plates (Oxoid) to determine the number of CFU. To assess the number of adherent bacteria, a model was cut in two equally sized pieces. One piece was used for histology and the other was homogenized in PBS using a glass Potter-Elvehjem tissue homogenizer, and the homogenates were subsequently serially diluted and plated as described above. The lower limits of detection for detachable and adherent bacteria were 20 and 40 CFU/LEM, respectively.
Histology
One biopsy of each model was fixed in 4% (v/v) formaldehyde, dehydrated, and embedded in paraffin. Next, paraffin blocks were cut into 5-μm sections, deparaffinized, rehydrated, and then stained with hematoxylin and eosin (H&E) staining.
Cryo scanning electron microscopy
For the morphological study of (methicillin resistant) S. aureus biofilms on LEM or PS by cryo-scanning electron microscopy (SEM), specimens were quickly frozen in liquid nitrogen slush and transferred directly to the cryo-transfer attachment (Gatan Alto2500). Samples were sublimated at -90 in high vacuum for 5 min and subsequently sputter-coated with a layer of 20 nm gold/paladium and examined in a JEOL JSM6700F scanning electron microscope.
Multiplex bead assay for assessment of the presence of proteins during S. aureus biofilm formation
A multiplex competitive Luminex assay [26] (CLA) with minor modifications was used to indirectly detect the presence of 52 IgG-accessible proteins in bacterial cultures (all bacterial proteins are described in S1 File). In brief, log-phase cultures of S. aureus were diluted 1:200 and incubated in PS wells for 1, 8, 24 and 48 hrs. After washing with ice-cold PBS supplemented with 0.5% (wt/v) sodium azide (Sigma-Aldrich), adherent bacteria residing in biofilms on PS or LEMs were incubated at 8°C and continuous shaking (500 rpm) with 200 μl of a 1:200 dilution of polyclonal human IgG (PHG), isolated using the HiTrap™ Protein G HP column according to the manufacturer’s guidelines (GE Healthcare Bio-sciences, Piscataway, New Jersey, USA), from pooled serum of 40 healthy volunteers (19 non-nasal carriers, 6 intermittent and 15 persistent nasal carriers of S. aureus as determined earlier [35]. After 35 min incubation the PHG samples were recovered from biofilms. The remaining non-bound IgG antibody levels in these samples, specifically directed against 52 proteins of S. aureus, were measured using a multiplex bead-based flow cytometry technique (xMAP®, Luminex corporation) wherein recombinant proteins were covalently coupled to the beads as described previously [27,28,36]. As negative controls PHG samples incubated with empty PS wells or sterile LEMs were included in all experiments.
Next, the percentage decrease in the levels of specific IgG antibodies for each protein was calculated in relation to the negative control. The percentage decrease can be considered a semi-quantitative measure of the protein-specific antibody absorption from PHG by the biofilm, thus indirectly reflecting the presence of the particular S. aureus protein by the biofilm [26]. The average percentage decrease plus two times the standard deviation, obtained at 8, 24 and 48 hours biofilm growth, for the three non-S. aureus control proteins and all S. aureus proteins of which genes were not present in LUH14616 were chosen as cut-off value (35% at 8 and 24 hrs biofilm growth and 40% at 48 hrs, respectively).
In case of bacteria adherent to LEMs, the same protocol was followed with the single modification that PHG samples were directly incubated on top of the LEM. To determine the presence of S. aureus proteins in culture supernatants, growth medium that covered biofilms grown on PS was analyzed using the same protocol, with the modification that medium was removed at designated time points and incubated with PHG samples in sterile wells.
Reverse transcriptase PCR
Early biofilms (8 and 16 hrs) were grown in 96-well plates (Cellstar culture plates, Greiner Bio-One) in 200 μl of IMDM (Gibco). Biofilms were resuspended, pooled and centrifuged at 4000 rpm for 10 min at 4°C. Pellets were resuspended in 200 μl of RNA protect™ Bacterial reagents (Qiagen), stabilized for 5 min and then centrifuged for 10 min at 4°C. The pellet was dissolved in 1 ml of RNA-pro solution (Fast RNA Pro Blue kit, MP Biomedicals) and stored at -20°C until use. RNA was isolated using the Fast RNA Pro Blue kit according to the manufacturer’s protocol. Each 10 μg of isolated RNA was treated twice with 2 U TURBO DNase (Ambion, Life Technologies). The reaction was stopped by adding 0.2 volumes of DNase inactivation reagent (Ambion) and incubation for 2 min at ambient temperature. RNA containing supernatants were collected by centrifugation (1.5 min at 9000 g at ambient temperature) and each 2 μg DNase-treated RNA was treated with 2 U DNase I (Fermentas, Fisher Scientific). One μg of prepared RNA was transcribed into cDNA using 200 U RevertAid H Minus Reverse transcriptase (Fermentas), 4 μl of 5x reaction buffer (Fermentas), 20 U of RiboLock RNase inhibitor (Fermentas) and 2 μl of 10 mM dNTP mix (Fermentas) in a final volume of 20 μl of DEPC-treated water. This was incubated for 60 min at 42°C and then terminated by heating at 70°C for 5 min. For each RNA sample a negative control without reverse transcriptase was processed similarly. The presence of cDNA in all samples was examined using PCR as described previously [27].
Proteomics
A total of 48 biofilms of strain LUH14616 were grown for 8 hours in PS wells as described above, resuspended in 200 μl of PBS per well, pooled and spun down at 4,000 rpm for 5 min. The resulting pellet was resuspended in 50 μl of PBS, mixed with 50 μl of Laemni buffer and heated for 5 min at 95°C. Fifty μl of this suspension containing denatured proteins were run on a 15% SDS gel (Biorad) and gel lanes were cut into ~1 mm slices. Lanes were subjected to in-gel reduction with dithiothreitol, alkylation with chloroacetamide and digestion with trypsin (Promega, Leiden, The Netherlands). Nanoflow LC-MS/MS was performed on an 1100 series capillary LC system (Agilent Technologies) coupled to an LTQ Orbitrap XL mass spectrometer (Thermo), operating in positive mode and equipped with a nanospray source. Mass spectra were acquired in continuum mode; fragmentation of the peptides was performed in data-dependent mode by CID. Peak lists were automatically created from raw data files using the Proteome Discoverer (version 1.3; Thermo). The Mascot search algorithm (version 2.2, MatrixScience) was used for searching against the Uniprot database (release 2013_06.fasta, taxonomy: S. aureus, strains USA300, Newman, NCTC 8325–4 and COL). The peptide tolerance was set to 10 ppm and the fragment ion tolerance was set to 0.8 Da. A maximum number of 2 missed cleavages by trypsin were allowed and carbamido-methylated cysteine and oxidized methionine were set as fixed and variable modifications, respectively. The Mascot score cut-off value for a positive protein hit was set to 65. Individual peptide MS/MS spectra with Mascot scores below 25 were checked manually and either interpreted as valid identifications or discarded.
Construction of the hla promotor upstream of GFPuvr
S. aureus strains LUH14616 and Sac042w containing a vector with an hla promotor upstream of GFPuvr were prepared as described earlier [37] with some modifications. First, the promotor of hla was amplified using primers hlapr1 (cggaattcgatatttctatgtaatggca) and hlapr2 (gctctagacttctatttttttgaacgat) and as a template DNA from S. aureus strain Newman. Next, the amplification product was ligated into the EcoRI XbaII site of pALC1484 (a kind gift from dr A.L. Cheung, Dartmouth College, New Hampshire, US) and cloned into E. coli DH10beta. From positive colonies on LB agar supplemented with 50 μg of ampicillin/ml, recombinant plasmids were isolated, checked by PCR and sequencing, and then electroporated into S. aureus RN4220. Finally, from positive colonies on BHI agar supplemented with 10 μg of chloramphenicol/ml, plasmids were isolated and electroporated into S. aureus LUH14616 and Sac042w. As positive and negative control we electroporated respectively pWVW 163, a plasmid containing a phage promotor yielding a strong, constant expression of GFP, and pALC1484, an empty vector [38], into the same S. aureus strains as described above.
Data analysis
All data were analysed using Microsoft Excel version 2010 and graphics were made using Graphpad Prism version 5 (Graphpad Inc. La Jolla, CA, USA).
Results
Biofilm formation by MRSA strain LUH14616 on LEMs and PS
Firstly, the ability of the clinical isolate MRSA LUH14616 to form biofilms on both the human skin model (Leiden Epidermal Model: LEM, schematically represented in Fig 1A), and polystyrene (PS) was examined. This MRSA strain was able to adhere to and stably colonize both surfaces, as reflected by an increase in bacterial counts on LEM (Fig 1B) and an increase in crystal violet staining on PS (Fig 1E) within the first 24 hrs after inoculation. Interestingly, haematoxylin-eosin staining of the colonized LEMs showed that the bacteria adhered to the stratum corneum and formed small colonies after 16 hrs, but did not invade the epidermis (Fig 1C). To further examine biofilm formation by MRSA strain LUH14616 on these surfaces, bacterial colonization on LEM (Fig 1D) and PS (Fig 1F) was visualized with scanning electron microscopy. Results revealed a tightly adherent layer of bacteria on both LEMs and PS after 24–48 hrs, indicating the development of a mature biofilm on both surfaces. Biofilm-associated bacteria on LEM appeared to be completely encased in an extracellular matrix (Fig 1D), while bacteria on PS appeared to be incompletely encased (Fig 1F).
Detection of toxins, immune modulators and other proteins of MRSA strain LUH14616 during biofilm formation on PS
We used a competitive Luminex-based assay (CLA) to establish the presence of 52 bacterial proteins during biofilm formation by MRSA strain LUH14616 on polystyrene (PS).
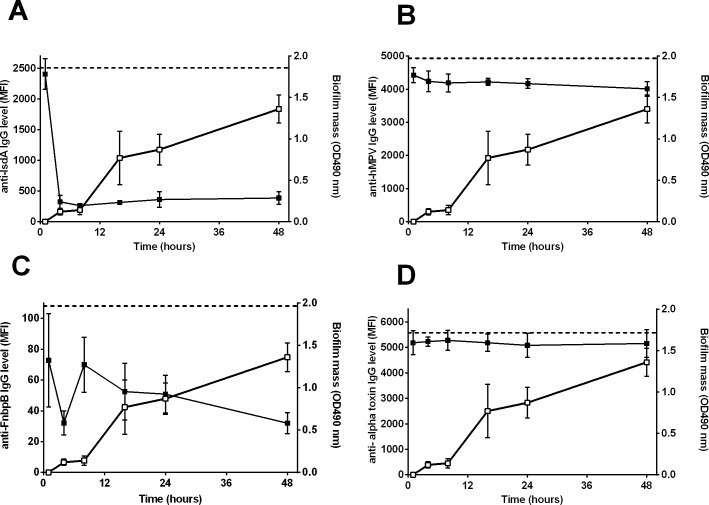
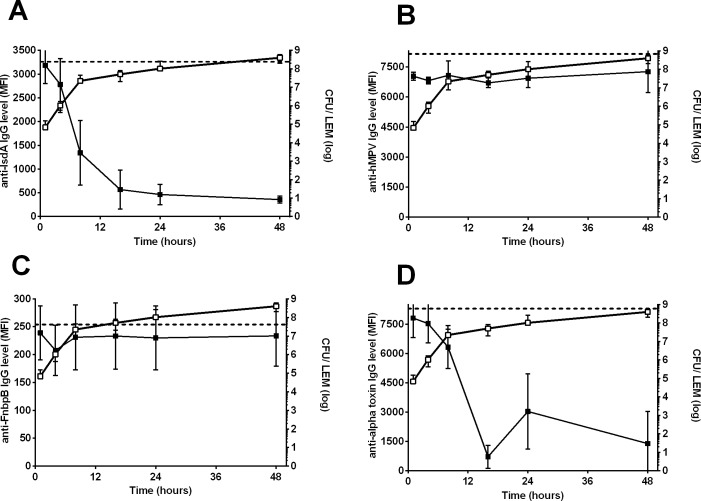
In line with previous results [26], biofilm mass-dependent absorption of specific IgG for several S aureus proteins, such as IsdA (Fig 2A), FnbpB (Fig 2C) and glucosaminidase by biofilms was detected, while no such reduction was seen for the levels of IgG antibodies directed against control proteins, e.g. the protein derived from human metapneumovirus (hMPV) (Fig 2B). Based on the percentage decrease in the levels of IgG directed against the three non-S. aureus control proteins and against the 28 S. aureus proteins of which genes were not found in LUH14616 using PCR, cut-off values of at least 35% decrease in specific IgG at 24 hrs biofilm growth and 40% at 48 hrs were calculated. CLA measurements for five proteins [ESX-1-associated factors EsxA and EsxB, iron surface determinants H (IsdH), Staphylococcal enterotoxin J (SEJ) and foldase-protein PrsA] were excluded from further analysis due to low MFI’s with standard deviations larger than 25% between repeated CLA measurements.
Fig 2. Detection of S. aureus proteins during biofilm formation of LUH14616 on PS.
Closed symbols indicate the mean fluorescence intensity (MFI, left Y-axis), reflecting the level of remaining non-bound IgG directed against specific proteins after incubation of PHG with the biofilms, while open symbols indicate biofilm mass (OD490 nm, right Y-axis). Both are plotted against the time of biofilm growth (hrs). Results are shown for (A) IsdA, (B) control protein of human metapneumovirus (hMPV), (C) FnbpB and (D) alpha toxin. Dashed horizontal lines indicate the average MFI of sterile controls. Symbols and error bars indicate mean and SD of four experiments.
Using the above mentioned cut-off values, we detected 8 proteins in 24 hrs and 48 hrs-old S. aureus biofilms: the surface proteins fibronectin-binding protein B (FnbpB), CflB, glucosaminidase, iron-responsive surface determinant A (IsdA), immunodominant antigen A (IsaA), SACOL0688, nuclease, and the immune modulator Efb (Table 1). In addition, a significant decrease in the levels of IgG specifically directed against chemotaxis inhibitory protein of S. aureus (CHIPS) with 48 hrs-old biofilms, but not 24 hrs-old biofilms, was observed. No significant decrease in the levels of specific IgG for 15 other proteins, despite the presence of corresponding genes in LUH14616 such as for alpha toxin, was observed (Fig 2D). Additional experiments showed that the secreted proteins alpha-toxin, HlgB, FLIPr and SSL1 could neither be detected in the growth medium covering biofilms, excluding the possibility of false-negative signals for these secreted proteins (S1 Fig). CLA data were further validated by confirming the presence of 7 out of the 8 detected proteins in early (8 hrs) biofilms using mass-spectrometry, while mRNA was detected for 5 of these proteins in early biofilms.
Table 1. Detection of mRNA and proteins during biofilm formation of LUH14616 on LEMs and PS.
| Biofilms on polystyrene | Biofilms on polystyrene | Biofilms on LEM | |||||||
|---|---|---|---|---|---|---|---|---|---|
| mRNA present3 | Protein detectable4 | Significant reduction in specific IgG5 | Significant reduction in specific IgG5 | ||||||
| Protein1 | Gene2 | Functional class | 8 hrs | 8 hrs | 8 hrs | 24 hrs | 48 hrs | 24 hrs | 48 hrs |
| CHIPS | chp | immmune modulator | Yes | Yes | - | - | + | - | + |
| ClfB | clfB | surface protein | Yes | Yes | + | + | + | + | + |
| Glucosaminidase | Atl | housekeeping | No | Yes | + | + | + | + | + |
| IsaA | isaA | housekeeping | Yes | Yes | + | + | + | + | + |
| IsdA | isdA | surface protein | Yes | Yes | + | + | + | + | + |
| Nuc | nuc | housekeeping/ toxin | No | Yes | + | + | + | + | + |
| SACOL0688 | MntC | housekeeping | Yes | Yes | + | + | + | + | + |
| Efb | efb | immmune modulator | No | Yes | + | + | + | - | - |
| FnBPB | fnbB | surface protein | Yes | No | + | + | + | - | - |
| Alpha toxin | hla | toxin | Yes | No | - | - | - | + | + |
| FlipR | flr | immmune modulator | Yes | No | - | - | - | + | + |
| HlgB | hlgB | toxin | Yes | No | - | - | - | + | + |
| Lipase | lip | housekeeping/ toxin | Yes | No | - | - | - | + | + |
| LukD | lukD | toxin | Yes | No | - | - | - | + | + |
| LukE | lukE | toxin | Yes | No | - | - | - | + | + |
| LytM | lytM | housekeeping | Yes | No | - | - | - | + | + |
| SSL1 | ssl1 | immmune modulator | Yes | No | - | - | - | - | + |
| FnBPA | fnbA | surface protein | No | Yes | - | - | - | - | - |
| SCIN | scn | immmune modulator | Yes | No | - | - | - | - | - |
| SdrD | sdrD | surface protein | Yes | Yes | - | - | - | - | - |
| SEA | sea | toxin | Yes | No | - | - | - | - | - |
| SSL3 | ssl3 | immmune modulator | Yes | No | - | - | - | - | - |
| SSL5 | ssl5 | immmune modulator | Yes | No | - | - | - | - | - |
| SSL10 | ssl10 | immmune modulator | Yes | No | - | - | - | - | - |
1Only proteins are shown for which corresponding genes were detected in LUH14616 and for which standard deviation between 4 CLA experiments did not exceed 25%. From top to bottom protein groups are shown that were detected on both LEMs and PS, only on PS, only on LEMs or on neither surface, respectively.
2Additional ORF IDs for all genes, based on sequences of S. aureus strain 8325–4 (SAOUHSC) or Newman (NWMN), are available online (http://www.uniprot.org/).
3Presence of mRNA was established using RT-PCR in early 8 hrs biofilms on PS.
4Presence of proteins was established using mass spectrometry in early 8 hrs biofilms on PS
5Significant reduction in the levels of IgG specific for each protein, indicative of the presence of the protein during biofilm formation, was defined as a reduction in IgG (compared to sterile controls) of at least 35% at 8 and 24 hrs biofilm growth and 40% at 48 hrs.
Detection of toxins, immune modulators and other proteins of MRSA strain LUH14616 during biofilm formation on LEMs
Next we screened for the presence of the same 52 proteins in biofilms of LUH14616 grown on LEM. Similar to biofilms grown on PS we observed time dependent absorption of antibodies against diverse antigens such as IsdA (Fig 3A) and glucosaminidase, whereas no such reduction was observed for antibodies directed against the non-S. aureus control proteins (Fig 3B) and the proteins of which the gene was not found in LUH14616. This prompted us to use the same cut-off values.
Fig 3. Detection of S. aureus proteins during biofilm formation of LUH14616 on LEMs.
Closed symbols indicate the mean fluorescence intensity (MFI, left Y-axis), reflecting the level of remaining non-bound IgG directed against specific proteins after incubation of PHG with the bacterial biofilms, while open symbols indicate biofilm mass (OD490 nm, right Y-axis). Both are plotted against the time of biofilm growth (hrs). Results are shown for (A) IsdA, (B) control protein of human metapneumovirus (hMPV), (C) FnbpB and(D) alpha toxin. Dashed horizontal lines indicate the average MFI of sterile controls. Symbols and error bars indicate mean and SD of four experiments, respectively.
Thirteen proteins were detected in 24 and 48 hrs-old biofilms on LEMs (Table 1): the surface proteins clumping factor B (CflB), glucosaminidase, IsdA, IsaA, glycyl-glysine endopeptidase (LytM), and SACOL0688; the toxins alpha-toxin (Fig 3D), gamma-hemolysin B (HlgB), leukocidins (Luk) D and E, lipase and nuclease; and the immune modulator formyl peptide receptor-like inhibitory protein (FLIPr). In addition, CHIPS and staphylococcal superantigen-like protein 1 (SSL 1) were detected in 48 hrs biofilms, but not 24 hrs biofilms. In contrast to biofilms on PS, no significant reduction was observed for antibodies against FnbpB at any time point (Fig 3C).
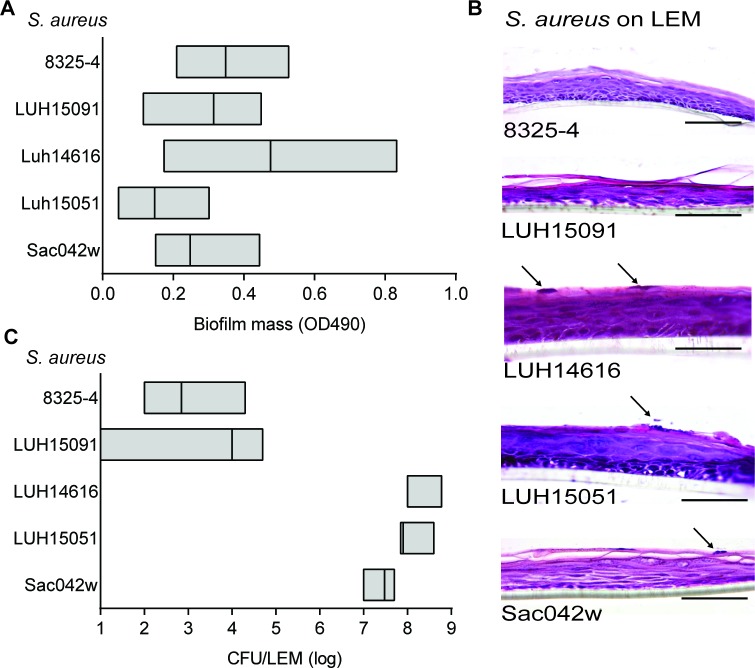
Detection of proteins during biofilm formation on LEMs and PS by different S. aureus strains
To determine whether the results obtained for MRSA LUH14616 are representative for other S. aureus strains, experiments with 24 hrs-old biofilms of an additional set of four, genetically diverse S. aureus strains were performed: i.e. LUH15051, LUH15091, the USA300 strain Sac042w, and NCTC 8325–4. Results revealed considerable variance in biofilm mass formed on the PS plates and LEMs among the different strains (Fig 4A–4C). Interestingly, strains 8325–4 and LUH15091 formed a significant biofilm on PS, but not on LEMs. The latter two strains were therefore excluded from further analyses. The same cut-off values were used as for LUH14616.
Fig 4. Biofilm formation by 5 different S. aureus strains on LEMs and PS surfaces.
(A) Biofilm formation after 24 hrs on PS was measured by crystal violet staining. (B) Hematoxylin and eosine staining of LEMs 24 hrs after exposure to S. aureus 8325–4, LUH15091, LUH15051, LUH14616 or Sac042w, arrows indicate S. aureus. Photographs are representative for three different experiments. Scale bars = 50 μm. (C) The number of viable bacteria present on epidermal models after 24 hrs inoculation was determined microbiologically (CFU/LEM). Results are boxplots showing the median and range. Results are means and SEM of three to five experiments.
In agreement with the results for LUH14616, the proteins ClfB, IsdA, IsaA, SACOL0688 and glucosaminidase were detected in 24 hrs-old biofilms of LUH15051 and Sac042w on both PS and LEMs (S1 Table). In addition, the toxins HIgB, LukD and E and the immune modulator SSL1 were detected in biofilms of both strains only on LEMs, while FnBPB was detected only on PS. In contrast to results obtained with LUH14616, we additionally detected the proteins CHIPS, efb, lipase and lytM (in biofilms of both LUH15051 and Sac042w) and alpha-toxin and FLipR (Sac042w only) on both surfaces. Finally, we detected SEA in biofilms of LUH15051 and Sac042w on respectively LEMS and PS, while SdrD was detected for both strains on LEMS.
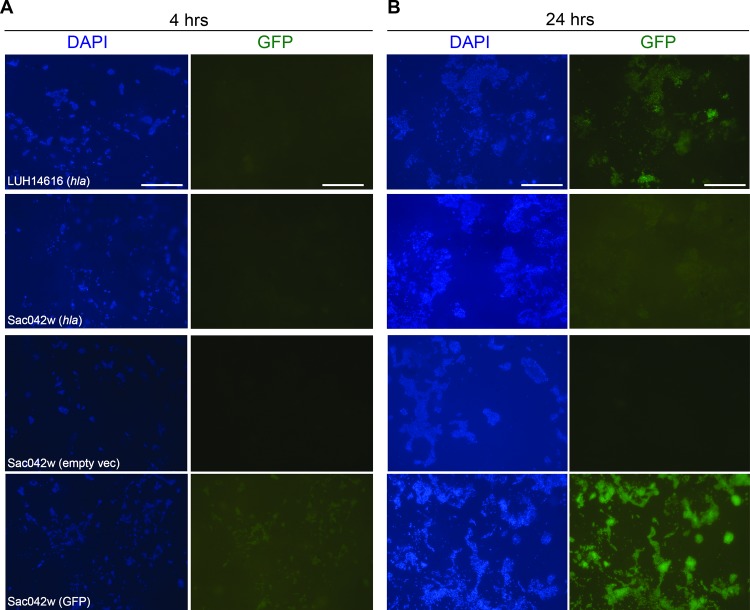
Alpha-toxin expression by MRSA strains LUH14616 and Sac042w during biofilm formation on LEMs and PS
The differential detection of alpha-toxin, an important virulence factor during skin infections caused by S. aureus, in biofilms of different strains on LEMs and PS was further investigated using GFP-reporter technology. Visualization of alpha-toxin produced by S. aureus was performed by using strains LUH14616 and Sac042w transformed with a vector containing the promoter for hla, coupled to GFP. Using fluorescence microscopy, small microcolonies of these bacteria were observed that did not express hla after 4 hrs of colonization of epidermal models (Fig 5A), whereas at 24 hrs of colonization LUH14616 highly expressed hla, as indicated by the green fluorescent signal (Fig 5B). In contrast to results seen at the protein level, hla expression by LUH14616 was also visualized after 24 hrs of colonization of polystyrene (S2 Fig), suggesting that the gene is transcribed but not translated and/or that protein is rapidly degraded. Similar results were obtained for Sac042w, although this was less pronounced than for LUH14616 (Fig 5B, S2 Fig).
Fig 5. Expression of hla by S. aureus LUH14616 and Sac042w during biofilm formation on LEMs.
LUH14616 and Sac042w containing hla-GFP (hla), empty vector (empty vec) or a construct yielding constant GFP expression (GFP), (A) at 4 hrs and (B) at 24 hrs after bacterial colonization of LEMs. LEMs were incubated for 4 or 24 hrs with the different bacterial strains, subsequently fixed in 1% paraformaldehyde, and stained with DAPI. hla expressing bacteria are presented in green, DAPI staining is presented in blue. Scale bars = 50 μm.
Discussion
In this study we established the presence of 52 proteins in biofilms of five genetically different S. aureus strains on two different types of surfaces, i.e. Leiden epidermal modes (LEMs) and polystyrene (PS). We detected six functionally diverse proteins in biofilms of three different strains on both surfaces. Several of these proteins, including ClfB, glucosaminidase and SA0688, have been previously associated with biofilm formation [39–42], although so far not on a human biotic surface. In this context, surface- and strain-dependent differences in the presence of a wide range of proteins, including alpha-toxin, were found. The detection of multiple toxins (HlgB, LukD/E and alpha toxin) in biofilms of multiple strains on LEMs, but not PS, indicates surface specific protein expression. This implicates that currently used biofilm models, such as those on PS, might not adequately reflect biofilm formation on a more complex surface, such as the human skin. However, we should realize that the biofilms on LEMs and PS were formed under different conditions, i.e. submerged in culture medium for biofilms on PS and on an air-exposed, dry surface in case of biofilm formation on LEMs.
Biofilm formation by strain LUH14616 on LEMs and PS was confirmed using EM. Interestingly, bacteria in a biofilm on LEM but not on PS were completely encased by an extracellular matrix, indicating a phenotypic difference in bacterial biofilm formation on the two models. However, in the current study we did not characterize the material encasing bacteria in more detail, e.g. using immunoelectron microscopy [43].
The detection of S. aureus toxins, most notably alpha-toxin, in biofilms on LEMs is in agreement with their well-established roles in the pathogenesis of skin infections [18,44]. The cytolytic pore-forming alpha-toxin [45] lyses human cells including skin tissue, interferes with the innate and adaptive immune responses in a murine skin infection model [46], and is essential for biofilm development on mucosal surfaces [47]. Interestingly, in human skin, the filaggrin protein may inhibit alpha-toxin’s cytotoxicity by its ability to regulate the secretion of sphingomyelinase [48]. In line with this, >90% of the atopic dermatitis (AD) patients, who often have reduced filaggrin expression, are colonized by S. aureus [49], whereas about 25% of the normal population is persistently colonized by this bacterium [50]. Moreover, S. aureus strains isolated from AD patients displayed a higher alpha-toxin production than strains from healthy controls, while the amount of alpha-toxin produced was correlated with disease severity [51].
The other toxins detected in biofilms in this study, including HlgB and the leukocidins D/ E, have also been associated with S. aureus skin colonization and infection. This is supported by data from both murine models [52,53] and clinical-epidemiological studies [54,55]. Other data also supports the presence of other, non-toxin proteins detected in this study. For instance, the detected lipase might support the persistence of S. aureus in the fatty secretions of mammalian skin [56,57]. A recent study demonstrated that lipases are essential for S. aureus biofilm formation [56].
The PHG used in this study to establish bacterial protein presence consisted of a previously described pool of serum from both nasal and non-nasal carriers of S. aureus [35]. Specific IgG against all tested proteins was detected in PHG and these IgG levels were generally higher than in serum from individual patients suffering from a S. aureus bacteremia [27] (unpublished data). Combined with the high sensitivity of the Luminex assay [58,59] we think that it is unlikely that the current CLA would not detect antibody absorption by IgG-accessible proteins. However, future studies using other antibody sources (e.g. specific monoclonal antibodies) might further increase the sensitivity of this assay.
A limitation of the PHG used in this study is the aspecific decrease in IgG that was observed against leukocidins S and F, while genes for these proteins were not present in strain LUH14616 and proteomics data could not confirm the presence of HlgB or Luk D/E in 8-hrs biofilms on PS. The known immunological cross-reactivity between Luk D/E, S/F and HlgB [60,61] may explain these conflicting findings. In addition, an incomplete protein library used during mass-spec analysis might explain why CLA results for a particular protein could not be confirmed. Additional mass-spectrometry should be performed on mature biofilms on LEMs to confirm or exclude the presence of these proteins.
Expression on LEMs of hla, the gene encoding alpha toxin, was confirmed for two strains using GFP reporter technology. The low levels of hla expression by the USA300-derived strain Sac042w may be explained by strain-specific traits [62], possibly caused by mutations in upstream regulators such as sarA [63]. Interestingly, for strain LUH14616 hla expression was also observed on PS, while CLA nor mass-spectrometry detected alpha toxin at the protein level on this surface. This suggests that hla is transcribed but not translated and/or that the protein is rapidly degraded by the bacteria on PS, which has been observed previously for other S. aureus strains during planktonic growth [63–66].
Regulation of hla and other genes for S. aureus virulence factors is influenced by many factors, including the accessory gene regulatory locus (Agr), RNAIII [67], downstream transcription factors Rot [68,69], SarA and -S and Sae [70]. In this connection, we noted that several proteins detected during biofilm formation on LEMs, including alpha-toxin, LytM, SSLs and Spa are (indirectly) regulated by RNAIII [67,71]. Moreover, RNAIII can also directly interfere with mRNA of LytM leading to its down-regulation [72]. Therefore, it may well be that the quorum sensing system of AgrA/RNAIII of S. aureus is activated differently upon interaction of S. aureus with either LEMs or PS, leading to up- or down-regulation of specific genes depending on the surface. However, further studies including quantitative mass-spectrometry and transcriptomic analysis are necessary to clarify the role of the diverse regulatory systems [73–75] involved in the expression of hla and other genes during biofilm formation on LEMs.
In the context of new anti-infective therapies, such as vaccines, our data indicate that diverse proteins of S. aureus in biofilms are accessible to human IgG. Although biofilm-associated bacteria are thought to be more resistant to antimicrobials and effectors of the human immune system [13–15], our data suggests that, in addition to animal models [41], also vaccine-boosted human antibodies can target biofilms. Further insights into the functionality of antibodies, specifically in regard to (the inhibition of) biofilm growth, are required.
Alternatively, it may be interesting to choose an anti-virulence based therapy, for example by targeting interfering RNAs, such as RNAIII that affect the expression of many virulence factors [76]. For example, the RnpA- inhibitor RNPA1000, was shown to have in vitro antimicrobial effect against S. aureus (and other gram positive pathogens). Moreover, this enzyme dose-dependently protected against the pathogenesis of S. aureus in a mouse infection model [77]. Based on our data such an anti-virulence therapy may be effective against biofilms on skin of e.g. AD patients colonized by S. aureus, but not against biofilms on abiotic surfaces, such as that of a colonized catheter.
We conclude that functionally diverse virulence factors of (methicillin-resistant) S. aureus are present during biofilm formation on PS and LEMs. We specifically confirmed the presence of alpha-toxin during biofilm formation of MRSA strains LUH14616 and Sac042w on LEMs. In addition, the presence of several toxins, including alpha-toxin, immune modulators and other proteins appear to differ depending on the studied strain and surface. These observations merit more mechanistic studies to elucidate the function of specific proteins and the regulation of their expression within S. aureus biofilms. However, the present data further suggests that specific proteins, such as the ubiquitously present IsdA or SA0688, could be potential targets for novel agents to prevent biofilm formation and/or to reduce biofilm formation not only in animal models but also on human biotic surfaces.
Supporting Information
Results are shown for (A) alpha-toxin, (B) HlgB, (C) FlipR, and (D) SSL1. Remaining non-bound IgG specific against the different proteins was separately measured after incubation of PHG with biofilms on PS and after incubation with the IMDM culture medium covering the biofilms. Closed squares indicate IgG measurements from the biofilm samples and open triangles indicate measurements from medium samples. Biofilm mass on PS is indicated by open squares, which are plotted on the right Y-axis. Dashed horizontal lines indicate average MFI of sterile controls. Results are presented as the mean of 2–4 experiments.
(TIF)
LUH14616 and Sac042w containing hla-GFP (hla), an empty vector or a construct yielding constant GFP expression (GFP), at 4 hrs and 24 hrs after bacterial colonization of PS. hla expressing bacteria are presented in green.
(TIF)
(DOCX)
(DOCX)
Acknowledgments
We thank Maartje Ruijken for technical assistance. The electron microscopy data was acquired at the Section Electron Microscopy of the department Molecular Cell Biology of the Leiden University Medical Center in the Netherlands. This work was supported by the Dutch Burns Foundation (project number 10.106). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors declare no conflict of interest.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by the Dutch Burns Foundation (project number 10.106; https://brandwondenstichting.nl/). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Emmerson AM, Enstone JE, Griffin M, Kelsey MC, Smyth ET (1996) The Second National Prevalence Survey of infection in hospitals—overview of the results. J Hosp Infect 32: 175–190. [DOI] [PubMed] [Google Scholar]
- 2.Enright MC, Robinson DA, Randle G, Feil EJ, Grundmann H, Spratt BG (2002) The evolutionary history of methicillin-resistant Staphylococcus aureus (MRSA). Proc Natl Acad Sci U S A 99: 7687–7692. 10.1073/pnas.122108599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jones RN (2003) Global epidemiology of antimicrobial resistance among community-acquired and nosocomial pathogens: a five-year summary from the SENTRY Antimicrobial Surveillance Program (1997–2001). Semin Respir Crit Care Med 24: 121–134. 10.1055/s-2003-37923 [DOI] [PubMed] [Google Scholar]
- 4.Laxminarayan R, Duse A, Wattal C, Zaidi AK, Wertheim HF, Sumpradit N, Vlieghe E, Hara GL, Gould IM, Goossens H, Greko C, So AD, Bigdeli M, Tomson G, Woodhouse W, Ombaka E, Peralta AQ, Qamar FN, Mir F, Kariuki S, Bhutta ZA, Coates A, Bergstrom R, Wright GD, Brown ED, Cars O (2013) Antibiotic resistance-the need for global solutions. Lancet Infect Dis 13: 1057–1098. S1473-3099(13)70318-9 [pii]; 10.1016/S1473-3099(13)70318-9 [DOI] [PubMed] [Google Scholar]
- 5.Piddock LJ (2012) The crisis of no new antibiotics—what is the way forward? Lancet Infect Dis 12: 249–253. S1473-3099(11)70316-4 [pii]; 10.1016/S1473-3099(11)70316-4 [DOI] [PubMed] [Google Scholar]
- 6.Boucher HW, Talbot GH, Bradley JS, Edwards JE, Gilbert D, Rice LB, Scheld M, Spellberg B, Bartlett J (2009) Bad bugs, no drugs: no ESKAPE! An update from the Infectious Diseases Society of America. Clin Infect Dis 48: 1–12. 10.1086/595011 [DOI] [PubMed] [Google Scholar]
- 7.Daum RS, Spellberg B (2012) Progress toward a Staphylococcus aureus vaccine. Clin Infect Dis 54: 560–567. cir828 [pii]; 10.1093/cid/cir828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haisma EM, de Breij A, Chan H, van Dissel JT, Drijfhout JW, Hiemstra PS, El GA, Nibbering PH (2014) LL-37-derived peptides eradicate multidrug-resistant Staphylococcus aureus from thermally wounded human skin equivalents. Antimicrob Agents Chemother 58: 4411–4419. AAC.02554-14 [pii]; 10.1128/AAC.02554-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Otto M (2010) Staphylococcus aureus toxin gene hitchhikes on a transferable antibiotic resistance element. Virulence 1: 49–51. 10453 [pii]; 10.4161/viru.1.1.10453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pier GB (2013) Will there ever be a universal Staphylococcus aureus vaccine? Hum Vaccin Immunother 9: 1865–1876. 25182 [pii]; 10.4161/hv.25182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fritz SA, Tiemann KM, Hogan PG, Epplin EK, Rodriguez M, Al-Zubeidi DN, Bubeck WJ, Hunstad DA (2013) A serologic correlate of protective immunity against community-onset Staphylococcus aureus infection. Clin Infect Dis 56: 1554–1561. cit123 [pii]; 10.1093/cid/cit123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davis SC, Ricotti C, Cazzaniga A, Welsh E, Eaglstein WH, Mertz PM (2008) Microscopic and physiologic evidence for biofilm-associated wound colonization in vivo. Wound Repair Regen 16: 23–29. WRR303 [pii]; 10.1111/j.1524-475X.2007.00303.x [DOI] [PubMed] [Google Scholar]
- 13.Babra C, Tiwari J, Costantino P, Sunagar R, Isloor S, Hegde N, Mukkur T (2014) Human methicillin-sensitive Staphylococcus aureus biofilms: potential associations with antibiotic resistance persistence and surface polysaccharide antigens. J Basic Microbiol 54: 721–728. 10.1002/jobm.201200557 [DOI] [PubMed] [Google Scholar]
- 14.Brady RA, Leid JG, Calhoun JH, Costerton JW, Shirtliff ME (2008) Osteomyelitis and the role of biofilms in chronic infection. FEMS Immunol Med Microbiol 52: 13–22. FIM357 [pii]; 10.1111/j.1574-695X.2007.00357.x [DOI] [PubMed] [Google Scholar]
- 15.Donlan RM, Costerton JW (2002) Biofilms: survival mechanisms of clinically relevant microorganisms. Clin Microbiol Rev 15: 167–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Percival SL, Hill KE, Williams DW, Hooper SJ, Thomas DW, Costerton JW (2012) A review of the scientific evidence for biofilms in wounds. Wound Repair Regen 20: 647–657. 10.1111/j.1524-475X.2012.00836.x [DOI] [PubMed] [Google Scholar]
- 17.Itoh S, Yamaoka N, Kamoshida G, Takii T, Tsuji T, Hayashi H, Onozaki K (2013) Staphylococcal superantigen-like protein 8 (SSL8) binds to tenascin C and inhibits tenascin C-fibronectin interaction and cell motility of keratinocytes. Biochem Biophys Res Commun 433: 127–132. S0006-291X(13)00310-0 [pii]; 10.1016/j.bbrc.2013.02.050 [DOI] [PubMed] [Google Scholar]
- 18.Kennedy AD, Bubeck WJ, Gardner DJ, Long D, Whitney AR, Braughton KR, Schneewind O, DeLeo FR (2010) Targeting of alpha-hemolysin by active or passive immunization decreases severity of USA300 skin infection in a mouse model. J Infect Dis 202: 1050–1058. 10.1086/656043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brady RA, Leid JG, Camper AK, Costerton JW, Shirtliff ME (2006) Identification of Staphylococcus aureus proteins recognized by the antibody-mediated immune response to a biofilm infection. Infect Immun 74: 3415–3426. 74/6/3415 [pii]; 10.1128/IAI.00392-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gil C, Solano C, Burgui S, Latasa C, Garcia B, Toledo-Arana A, Lasa I, Valle J (2014) Biofilm matrix exoproteins induce a protective immune response against Staphylococcus aureus biofilm infection. Infect Immun 82: 1017–1029. IAI.01419-13 [pii]; 10.1128/IAI.01419-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Luong TT, Lei MG, Lee CY (2009) Staphylococcus aureus Rbf activates biofilm formation in vitro and promotes virulence in a murine foreign body infection model. Infect Immun 77: 335–340. IAI.00872-08 [pii]; 10.1128/IAI.00872-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Van Wamel WJ, Hendrickx AP, Bonten MJ, Top J, Posthuma G, Willems RJ (2007) Growth condition-dependent Esp expression by Enterococcus faecium affects initial adherence and biofilm formation. Infect Immun 75: 924–931. IAI.00941-06 [pii]; 10.1128/IAI.00941-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thakoersing VS, Danso MO, Mulder A, Gooris G, El Ghalbzouri A., Bouwstra JA (2012) Nature versus nurture: does human skin maintain its stratum corneum lipid properties in vitro? Exp Dermatol 21: 865–870. 10.1111/exd.12031 [DOI] [PubMed] [Google Scholar]
- 24.Holland DB, Bojar RA, Farrar MD, Holland KT (2009) Differential innate immune responses of a living skin equivalent model colonized by Staphylococcus epidermidis or Staphylococcus aureus. FEMS Microbiol Lett 290: 149–155. FML1402 [pii]; 10.1111/j.1574-6968.2008.01402.x [DOI] [PubMed] [Google Scholar]
- 25.Haisma EM, Rietveld MH, de Breij A, van Dissel JT, El Ghalbzouri A, Nibbering PH (2013) Inflammatory and antimicrobial responses to methicillin-resistant Staphylococcus aureus in an in vitro wound infection model. PLoS One 8: e82800 10.1371/journal.pone.0082800;PONE-D-13-29187 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hansenova MS, Bikker FJ, Veerman EC, van Belkum A, Van Wamel WJ (2013) Rapid detection and semi-quantification of IgG-accessible Staphylococcus aureus surface-associated antigens using a multiplex competitive Luminex assay. J Immunol Methods 397: 18–27. S0022-1759(13)00228-7 [pii]; 10.1016/j.jim.2013.07.016 [DOI] [PubMed] [Google Scholar]
- 27.den Reijer PM, Lemmens-den Toom N, Kant S, Snijders SV, Boelens H, Tavakol M, Verkaik NJ, van BA, Verbrugh HA, Van Wamel WJ (2013) Characterization of the humoral immune response during Staphylococcus aureus bacteremia and global gene expression by Staphylococcus aureus in human blood. PLoS One 8: e53391 10.1371/journal.pone.0053391;PONE-D-12-25651 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Verkaik N, Brouwer E, Hooijkaas H, van Belkum A, van Wamel W (2008) Comparison of carboxylated and Penta-His microspheres for semi-quantitative measurement of antibody responses to His-tagged proteins. J Immunol Methods 335: 121–125. S0022-1759(08)00085-9 [pii]; 10.1016/j.jim.2008.02.022 [DOI] [PubMed] [Google Scholar]
- 29.Dutch Federation of Biomedical Scientific Societies (Federa). Human tissue and medical research: code of conduct for responsible use. 2011. Available online at https://www.federa.org/sites/default/files/digital_version_first_part_code_of_conduct_in_uk_2011_12092012.pdf
- 30.Croes S, Deurenberg RH, Boumans ML, Beisser PS, Neef C, Stobberingh EE (2009) Staphylococcus aureus biofilm formation at the physiologic glucose concentration depends on the S. aureus lineage. BMC Microbiol 9: 229 1471-2180-9-229 [pii]; 10.1186/1471-2180-9-229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lemmens N, van Wamel W, Snijders S, Lesse AJ, Faden H, van Belkum A (2011) Genomic comparisons of USA300 Staphylococcus aureus colonizating the nose and rectum of children with skin abscesses. Microb Pathog 50: 192–199. S0882-4010(10)00196-8 [pii]; 10.1016/j.micpath.2010.12.006 [DOI] [PubMed] [Google Scholar]
- 32.Enright MC, Day NP, Davies CE, Peacock SJ, Spratt BG (2000) Multilocus sequence typing for characterization of methicillin-resistant and methicillin-susceptible clones of Staphylococcus aureus. J Clin Microbiol 38: 1008–1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ponec M, Weerheim A, Kempenaar J, Mulder A, Gooris GS, Bouwstra J, Mommaas AM (1997) The formation of competent barrier lipids in reconstructed human epidermis requires the presence of vitamin C. J Invest Dermatol 109: 348–355. [DOI] [PubMed] [Google Scholar]
- 34.El Ghalbzouri A, Siamari R, Willemze R, Ponec M (2008) Leiden reconstructed human epidermal model as a tool for the evaluation of the skin corrosion and irritation potential according to the ECVAM guidelines. Toxicol In Vitro 22: 1311–1320. S0887-2333(08)00098-2 [pii]; 10.1016/j.tiv.2008.03.012 [DOI] [PubMed] [Google Scholar]
- 35.Verkaik NJ, de Vogel CP, Boelens HA, Grumann D, Hoogenboezem T, Vink C, et al. Anti-staphylococcal humoral immune response in persistent nasal carriers and noncarriers of Staphylococcus aureus. J Infect Dis. 2009;199(5):625–32. 10.1086/596743 [DOI] [PubMed] [Google Scholar]
- 36.Martins TB, Augustine NH, Hill HR (2006) Development of a multiplexed fluorescent immunoassay for the quantitation of antibody responses to group A streptococci. J Immunol Methods 316: 97–106. S0022-1759(06)00230-4 [pii]; 10.1016/j.jim.2006.08.007 [DOI] [PubMed] [Google Scholar]
- 37.Rooijakkers SH, Ruyken M, van Roon J, van Kessel KP, van Strijp JA, van Wamel WJ (2006) Early expression of SCIN and CHIPS drives instant immune evasion by Staphylococcus aureus. Cell Microbiol 8: 1282–1293. CMI709 [pii]; 10.1111/j.1462-5822.2006.00709.x [DOI] [PubMed] [Google Scholar]
- 38.Rooijakkers SH, van Wamel WJ, Ruyken M, van Kessel KP, van Strijp JA (2005) Anti-opsonic properties of staphylokinase. Microbes Infect 7: 476–484. S1286-4579(05)00036-5 [pii]; 10.1016/j.micinf.2004.12.014 [DOI] [PubMed] [Google Scholar]
- 39.Abraham NM, Jefferson KK. Staphylococcus aureus clumping factor B mediates biofilm formation in the absence of calcium. Microbiology. 2012;158(Pt 6):1504–12. Epub 2012/03/24. 10.1099/mic.0.057018-0 ; PubMed Central PMCID: PMCPmc3541775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brady RA, Leid JG, Camper AK, Costerton JW, Shirtliff ME. Identification of Staphylococcus aureus proteins recognized by the antibody-mediated immune response to a biofilm infection. Infect Immun. 2006;74(6):3415–26. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brady RA, O'May GA, Leid JG, Prior ML, Costerton JW, Shirtliff ME. Resolution of Staphylococcus aureus biofilm infection using vaccination and antibiotic treatment. Infect Immun. 2011;79(4):1797–803. 10.1128/IAI.00451-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Speziale P, Pietrocola G, Foster TJ, Geoghegan JA. Protein-based biofilm matrices in Staphylococci. Front Cell Infect Microbiol. 2014;4:171 Epub 2014/12/30. 10.3389/fcimb.2014.00171 ; PubMed Central PMCID: PMCPmc4261907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.O'Riordan K, Lee JC. Staphylococcus aureus capsular polysaccharides. Clin Microbiol Rev. 2004;17(1):218–34. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kobayashi SD, Malachowa N, Whitney AR, Braughton KR, Gardner DJ, Long D, Bubeck WJ, Schneewind O, Otto M, DeLeo FR (2011) Comparative analysis of USA300 virulence determinants in a rabbit model of skin and soft tissue infection. J Infect Dis 204: 937–941. jir441 [pii]; 10.1093/infdis/jir441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ezepchuk YV, Leung DY, Middleton MH, Bina P, Reiser R, Norris DA (1996) Staphylococcal toxins and protein A differentially induce cytotoxicity and release of tumor necrosis factor-alpha from human keratinocytes. J Invest Dermatol 107: 603–609. 0022202X96864141 [pii]. [DOI] [PubMed] [Google Scholar]
- 46.Tkaczyk C, Hamilton MM, Datta V, Yang XP, Hilliard JJ, Stephens GL, Sadowska A, Hua L, O'Day T, Suzich J, Stover CK, Sellman BR (2013) Staphylococcus aureus alpha toxin suppresses effective innate and adaptive immune responses in a murine dermonecrosis model. PLoS One 8: e75103 10.1371/journal.pone.0075103;PONE-D-13-19704 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Anderson MJ, Lin YC, Gillman AN, Parks PJ, Schlievert PM, Peterson ML (2012) Alpha-toxin promotes Staphylococcus aureus mucosal biofilm formation. Front Cell Infect Microbiol 2: 64 10.3389/fcimb.2012.00064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brauweiler AM, Bin L, Kim BE, Oyoshi MK, Geha RS, Goleva E, Leung DY (2013) Filaggrin-dependent secretion of sphingomyelinase protects against staphylococcal alpha-toxin-induced keratinocyte death. J Allergy Clin Immunol 131: 421–427. S0091-6749(12)01698-3 [pii]; 10.1016/j.jaci.2012.10.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Roll A, Cozzio A, Fischer B, Schmid-Grendelmeier P (2004) Microbial colonization and atopic dermatitis. Curr Opin Allergy Clin Immunol 4: 373–378. 00130832-200410000-00008 [pii]. [DOI] [PubMed] [Google Scholar]
- 50.Muthukrishnan G, Lamers RP, Ellis A, Paramanandam V, Persaud AB, Tafur S, Parkinson CL, Cole AM (2013) Longitudinal genetic analyses of Staphylococcus aureus nasal carriage dynamics in a diverse population. BMC Infect Dis 13: 221 1471-2334-13-221 [pii]; 10.1186/1471-2334-13-221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hong SW, Choi EB, Min TK, Kim JH, Kim MH, Jeon SG, Lee BJ, Gho YS, Jee YK, Pyun BY, Kim YK (2014) An Important Role of alpha-Hemolysin in Extracellular Vesicles on the Development of Atopic Dermatitis Induced by Staphylococcus aureus. PLoS One 9: e100499 10.1371/journal.pone.0100499;PONE-D-14-03221 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Katayama Y, Baba T, Sekine M, Fukuda M, Hiramatsu K (2013) Beta-hemolysin promotes skin colonization by Staphylococcus aureus. J Bacteriol 195: 1194–1203. JB.01786-12 [pii]; 10.1128/JB.01786-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Prevost G, Cribier B, Couppie P, Petiau P, Supersac G, Finck-Barbancon V, Monteil H, Piemont Y (1995) Panton-Valentine leucocidin and gamma-hemolysin from Staphylococcus aureus ATCC 49775 are encoded by distinct genetic loci and have different biological activities. Infect Immun 63: 4121–4129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mesrati I, Saidani M, Ennigrou S, Zouari B, Ben RS (2010) Clinical isolates of Pantone-Valentine leucocidin- and gamma-haemolysin-producing Staphylococcus aureus: prevalence and association with clinical infections. J Hosp Infect 75: 265–268. [DOI] [PubMed] [Google Scholar]
- 55.Shallcross LJ, Fragaszy E, Johnson AM, Hayward AC (2013) The role of the Panton-Valentine leucocidin toxin in staphylococcal disease: a systematic review and meta-analysis. Lancet Infect Dis 13: 43–54. S1473-3099(12)70238-4 [pii]; 10.1016/S1473-3099(12)70238-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hu C, Xiong N, Zhang Y, Rayner S, Chen S (2012) Functional characterization of lipase in the pathogenesis of Staphylococcus aureus. Biochem Biophys Res Commun 419: 617–620. S0006-291X(12)00290-2 [pii]; 10.1016/j.bbrc.2012.02.057 [DOI] [PubMed] [Google Scholar]
- 57.Rosenstein R, Gotz F (2000) Staphylococcal lipases: biochemical and molecular characterization. Biochimie 82: 1005–1014. S0300-9084(00)01180-9 [pii]. [DOI] [PubMed] [Google Scholar]
- 58.Porcelijn L, Huiskes E, Comijs-van Osselen I, Chhatta A, Rathore V, Meyers M, et al. A new bead-based human platelet antigen antibodies detection assay versus the monoclonal antibody immobilization of platelet antigens assay. Transfusion. 2014;54(6):1486–92. 10.1111/trf.12509 [DOI] [PubMed] [Google Scholar]
- 59.Wu W, Zhang S, Qu J, Zhang Q, Li C, Li J, et al. Simultaneous detection of IgG antibodies associated with viral hemorrhagic fever by a multiplexed Luminex-based immunoassay. Virus Res. 2014;187:84–90. 10.1016/j.virusres.2013.12.037 [DOI] [PubMed] [Google Scholar]
- 60.Gouaux E, Hobaugh M, Song L (1997) alpha-Hemolysin, gamma-hemolysin, and leukocidin from Staphylococcus aureus: distant in sequence but similar in structure. Protein Sci 6: 2631–2635. 10.1002/pro.5560061216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kamio Y, Rahman A, Nariya H, Ozawa T, Izaki K (1993) The two Staphylococcal bi-component toxins, leukocidin and gamma-hemolysin, share one component in common. FEBS Lett 321: 15–18. 0014-5793(93)80611-W [pii]. [DOI] [PubMed] [Google Scholar]
- 62.Tavares A, Nielsen JB, Boye K, Rohde S, Paulo AC, Westh H, et al. Insights into alpha-hemolysin (Hla) evolution and expression among Staphylococcus aureus clones with hospital and community origin. PLoS One. 2014;9(7):e98634 10.1371/journal.pone.0098634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zielinska AK, Beenken KE, Joo HS, Mrak LN, Griffin LM, Luong TT, et al. Defining the strain-dependent impact of the Staphylococcal accessory regulator (sarA) on the alpha-toxin phenotype of Staphylococcus aureus. J Bacteriol. 2011;193(12):2948–58. 10.1128/JB.01517-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kolar SL, Ibarra JA, Rivera FE, Mootz JM, Davenport JE, Stevens SM, et al. Extracellular proteases are key mediators of Staphylococcus aureus virulence via the global modulation of virulence-determinant stability. Microbiologyopen. 2013;2(1):18–34. 10.1002/mbo3.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Morfeldt E, Taylor D, von Gabain A, Arvidson S. Activation of alpha-toxin translation in Staphylococcus aureus by the trans-encoded antisense RNA, RNAIII. Embo J. 1995;14(18):4569–77. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zielinska AK, Beenken KE, Mrak LN, Spencer HJ, Post GR, Skinner RA, et al. sarA-mediated repression of protease production plays a key role in the pathogenesis of Staphylococcus aureus USA300 isolates. Mol Microbiol. 2012;86(5):1183–96. 10.1111/mmi.12048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Guillet J, Hallier M, Felden B (2013) Emerging functions for the Staphylococcus aureus RNome. PLoS Pathog 9: e1003767 10.1371/journal.ppat.1003767;PPATHOGENS-D-13-01470 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Benson MA, Lilo S, Wasserman GA, Thoendel M, Smith A, Horswill AR, Fraser J, Novick RP, Shopsin B, Torres VJ (2011) Staphylococcus aureus regulates the expression and production of the staphylococcal superantigen-like secreted proteins in a Rot-dependent manner. Mol Microbiol 81: 659–675. 10.1111/j.1365-2958.2011.07720.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chu X, Xia R, He N, Fang Y (2013) Role of Rot in bacterial autolysis regulation of Staphylococcus aureus NCTC8325. Res Microbiol 164: 695–700. S0923-2508(13)00102-2 [pii]; 10.1016/j.resmic.2013.06.001 [DOI] [PubMed] [Google Scholar]
- 70.Li D, Cheung A (2008) Repression of hla by rot is dependent on sae in Staphylococcus aureus. Infect Immun 76: 1068–1075. IAI.01069-07 [pii]; 10.1128/IAI.01069-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fechter P, Caldelari I, Lioliou E, Romby P (2014) Novel aspects of RNA regulation in Staphylococcus aureus. FEBS Lett 588: 2523–2529. S0014-5793(14)00424-4 [pii]; 10.1016/j.febslet.2014.05.037 [DOI] [PubMed] [Google Scholar]
- 72.Chunhua M, Yu L, Yaping G, Jie D, Qiang L, Xiaorong T, Guang Y (2012) The expression of LytM is down-regulated by RNAIII in Staphylococcus aureus. J Basic Microbiol 52: 636–641. 10.1002/jobm.201100426 [DOI] [PubMed] [Google Scholar]
- 73.Goerke C, Fluckiger U, Steinhuber A, Zimmerli W, Wolz C. Impact of the regulatory loci agr, sarA and sae of Staphylococcus aureus on the induction of alpha-toxin during device-related infection resolved by direct quantitative transcript analysis. Mol Microbiol. 2001;40(6):1439–47. Epub 2001/07/10. . [DOI] [PubMed] [Google Scholar]
- 74.Vandenesch F, Kornblum J, Novick RP. A temporal signal, independent of agr, is required for hla but not spa transcription in Staphylococcus aureus. J Bacteriol. 1991;173(20):6313–20. Epub 1991/10/01. ; PubMed Central PMCID: PMCPmc208961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Xiong YQ, Willard J, Yeaman MR, Cheung AL, Bayer AS. Regulation of Staphylococcus aureus alpha-toxin gene (hla) expression by agr, sarA, and sae in vitro and in experimental infective endocarditis. J Infect Dis. 2006;194(9):1267–75. Epub 2006/10/17. 10.1086/508210 . [DOI] [PubMed] [Google Scholar]
- 76.Morrison JM, Dunman PM (2011) The modulation of Staphylococcus aureus mRNA turnover. Future Microbiol 6: 1141–1150. 10.2217/fmb.11.102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Olson PD, Kuechenmeister LJ, Anderson KL, Daily S, Beenken KE, Roux CM, Reniere ML, Lewis TL, Weiss WJ, Pulse M, Nguyen P, Simecka JW, Morrison JM, Sayood K, Asojo OA, Smeltzer MS, Skaar EP, Dunman PM (2011) Small molecule inhibitors of Staphylococcus aureus RnpA alter cellular mRNA turnover, exhibit antimicrobial activity, and attenuate pathogenesis. PLoS Pathog 7: e1001287 10.1371/journal.ppat.1001287 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Results are shown for (A) alpha-toxin, (B) HlgB, (C) FlipR, and (D) SSL1. Remaining non-bound IgG specific against the different proteins was separately measured after incubation of PHG with biofilms on PS and after incubation with the IMDM culture medium covering the biofilms. Closed squares indicate IgG measurements from the biofilm samples and open triangles indicate measurements from medium samples. Biofilm mass on PS is indicated by open squares, which are plotted on the right Y-axis. Dashed horizontal lines indicate average MFI of sterile controls. Results are presented as the mean of 2–4 experiments.
(TIF)
LUH14616 and Sac042w containing hla-GFP (hla), an empty vector or a construct yielding constant GFP expression (GFP), at 4 hrs and 24 hrs after bacterial colonization of PS. hla expressing bacteria are presented in green.
(TIF)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.