Abstract
Objective
To determine whether injection augmentation reduces the likelihood of ultimately needing definitive framework surgery in unilateral vocal fold paralysis (UVFP) patients.
Study Design
Retrospective cohort study
Methods
All patients diagnosed with UVFP (2008–2012) at the academic center were identified. Time from symptom onset to presentation to either a community otolaryngologist and/or academic center as well as any directed treatment(s) were recorded. Stepwise, multivariate logistic regression analysis was used to determine whether injection augmentation independently affected odds of needing definitive, framework surgery among patients seen within nine months of symptom onset and who had not undergone any prior rehabilitative procedures.
Results
Cohort consisted of 633 patients (55% female, 80% Caucasian, median age 60 years) with UVFP. The majority of etiologies were either surgery (48%) or idiopathic (37%). Duration to presentation at community otolaryngologist was shorter than to the academic center (median 2 vs. 6 months). Overall, less than half of UVFP patients had any operation (46%). Multivariate logistic regression found that earlier injection augmentation did not affect odds of ultimately undergoing framework surgery (OR 1.13, CI 0.92 – 1.40; p=0.23).
Conclusion
Nearly half of UVFP patients do not require any rehabilitative procedure. When indicated, early injection augmentation is effective at temporarily alleviating associated symptoms, but does not reduce likelihood of needing a definitive framework operation in patients with UVFP. Understanding practice patterns and fostering early detection and treatment may improve quality of life in this patient population.
Keywords: Unilateral vocal fold paralysis, injection augmentation, injection laryngoplasty, type I laryngoplasty, framework surgery, time to presentation, selection bias
INTRODUCTION
Over the last 20 years, the at-risk population for unilateral vocal fold paralysis (UVFP) has increased in conjunction with 3- and 8-fold increases in thyroidectomy1,2 and anterior cervical disk fusion procedures3. These, in addition to other operations, carry significant risks of vocal fold paralysis4,5. UVFP variably causes dysfunction in voice, swallowing, and breathing and has major quality of life consequences6,7. The basic tenet of treatment is to reestablish symmetrical medial closure of both vocal folds to reduce symptomatic glottic insufficiency. Treatment decisions are based on symptom severity, etiology, and paralysis duration prior to presentation.
Vocal fold injection augmentation is used when symptomatic paralysis is considered temporary, prognosis for recovery is unknown, or if other medical conditions preclude definitive management. It is highly effective at ameliorating associated UVFP symptoms8. Most practitioners opt for injection augmentation prior to considering definitive framework operations9. Large epidemiological studies indicate that over 80% of post-thyroidectomy UVFP cases are transient10,11. Recognizing the possibility of spontaneous recovery, most surgeons recommend patients wait 6 – 12 months prior to offering framework operations12. An injection augmentation can effectively manage symptoms during this recovery period.
While advocated as a temporary treatment, early vocal fold injection augmentation has been proposed to reduce the need for more definitive framework surgery13–15. These studies posit that early injection could alleviate symptoms and have a lasting effect (beyond the time expected simply by the presence of injectate), obviating the need for further invasive operations. However, overrepresentation of patients with transient paralyses (early presenters) in these studies could bias results. Investigation into the association requires adjustment for this selection bias. The primary aim of the present retrospective cohort study was to investigate whether injection augmentation reduces the likelihood of ultimately needing framework surgery. Secondary analysis audited practice patterns in UVFP management that may affect time to presentation and treatment.
METHODS
The retrospective cohort study was performed in accordance with the Declaration of Helsinki, Good Clinical Practice, and approved by the Institutional Review Board (IRB#140076).
Overall Cohort
New unilateral vocal fold paralysis (UVFP) patients were identified using International Classification of Disease version 9 (ICD-9) codes (478.30, 478.31, 478.32) derived from Vanderbilt Department of Otolaryngology administrative billing records from 2008 through 2012. Each patient’s diagnosis was confirmed by medical record review. Excluded were patients with incongruous diagnoses (e.g., vocal fold fixation, bilateral vocal fold immobility) and those less than 18 years of age. Records were reviewed in summer 2014, yielding a range of follow-up between 1.5 and 6 years. Each patient was tracked longitudinally from symptom inception to presentation and through any UVFP-directed treatment to final clinical outcome (e.g., stabilization of symptoms).
Data Collected
Data extracted included patient characteristics [age, gender, race], UVFP etiology, UVFP treatments [observation, voice therapy, injection augmentation, framework surgery], and Each patient’s time from symptom onset to presentation to community otolaryngology and, ultimately, to the academic center. Time to treatment(s) and between treatments was recorded. UVFP characteristics upon presentation to the academic center were recorded including sidedness [right/left], degree of paralysis [partial/complete], and whether vocal folds achieved complete closure with maximal effort during laryngoscopic examination (i.e. glottic gap) [yes/no]. All data were entered and stored in the secure, web-based REDCap (Research Electronic Data Capture) (1 UL1 RR024975 NCRR/NIH). Two independent extractions were performed to confirm data accuracy.
Surgical Treatments
All vocal fold injection augmentation procedures during this time period were performed using Cymetra (LifeCell, Corp., Bridgewater, NJ) and done in the operating suite during direct microlaryngoscopy. The injection was placed into the ipsilateral paraglottic soft tissue to medialize the vocal fold. Definitive type I laryngoplasty ± arytenoid adduction, hereafter referred to as framework surgery, was performed when UVFP was 1) known to be permanent, 2) symptomatic enough to cause substantial diminishment of a patient’s quality of life, and 3) persisting at least 6 months since any injection augmentation to allow any residual injectate to be resorbed. Framework surgery is considered a surrogate outcome for failure to regain adequate reinnervation or favorable synkinesis.
Statistical Analysis
Statistical analyses were performed using Excel (Microsoft Corp; Redmond, WA) and STATA 12MP (STATA Corp; College Station, TX). Summary analyses [median, interquartile range (IQR), and percentages] described patient characteristics, etiology, treatment, and UVFP characteristics. Interval from symptom onset to presentation and treatment by a community otolaryngologist and/or laryngologist at the academic center were calculated. Comparisons used Pearson and Fisher exact chi2 tests, where appropriate. For continuous variables, non-parametric Kruskal-Wallis Rank-Sum Tests were used.
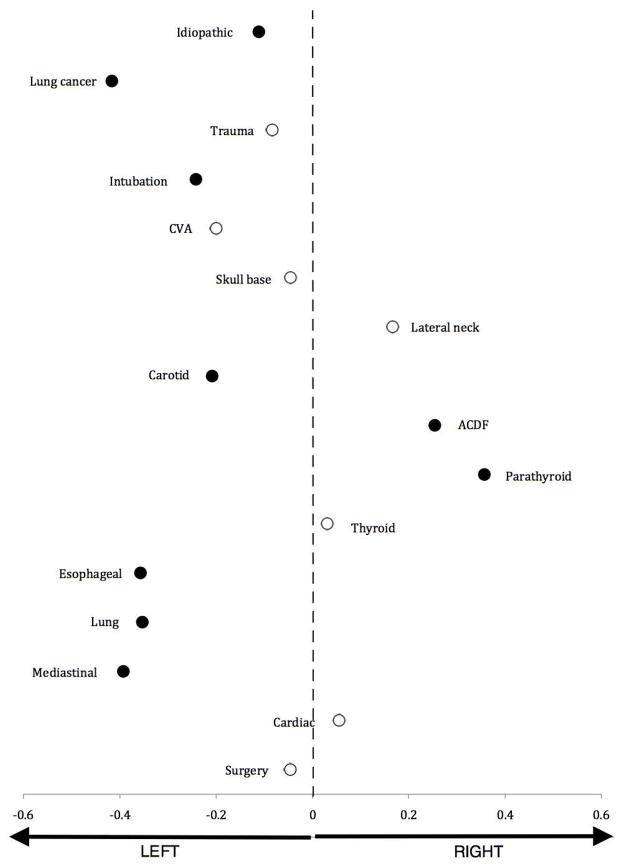
Skew of UVFP side was determined using methodology previously described16. In brief, laterality skew was calculated using the equation: Skew = (# cases on right/total # cases) – 0.5. Skew is zero when there is no laterality predilection. However, as ratio of left-sided cases increases, the value becomes more negative, with a maximum/minimum value of ±0.516. Skewness was measured and plotted for each UVFP etiology that had greater than 5 cases in the cohort and statistical significance assessed using Pearson’s or Fisher’s exact chi2 tests, as appropriate.
To analyze the effect of early injection augmentation on the ultimate need for framework surgery, we included patients 1) presenting to the academic center directly (or indirectly, but without previous surgery) 2) presenting within 9 months of symptom onset, 3) without a known recurrent laryngeal nerve transection or sacrifice, 4) without current or history of laryngeal cancer, 5) surviving greater than 18 months following injection, and 6) not lost to follow-up. Univariate analyses determined whether characteristics were associated with receiving framework surgery. The primary analysis assessed whether earlier injection augmentation affected odds of ultimately undergoing framework surgery. In this analysis, only those patients meeting criteria and who had undergone injection augmentation at the academic center were included.
Stepwise, multivariate logistic regression analysis assessed which variables independently changed odds of undergoing framework surgery. Variables considered for the model were age (continuous), gender (male/female), etiology (surgical, non-surgical), completeness of vocal fold closure at presentation (yes/no), side of paralysis (right/left), degree of paralysis at presentation (partial/complete), and duration of symptoms (months). A significance level of p<0.20 was the criterion for inclusion of these variables in multivariate models, although a p<0.05 was required for statistical significance.
RESULTS
Of 764 identified, 633 patients (55% female [347/632], 80% Caucasian [506/633], median age 60 years [IQR 50 – 70; range 18 – 98]) had confirmed unilateral vocal fold paralysis (UVFP) between 2008 and 2012. Characteristics are described in Table 1. The annual number of new UVFP patients seen at our tertiary laryngology center increased 1.82-fold (93 to 169) from 2008 to 2012. Based on laryngoscopy, 48% had incomplete vocal fold closure (44% complete, 8% not recorded), and 19% had partial paralyses at presentation.
Table 1.
Patient Characteristics, Symptoms, and Laryngoscopic Findings
| Patient Characteristics | Summary (n=633) |
|---|---|
| Age, median (IQR; range) | 60 (50 – 70; 18 – 98) |
| Female | 55% |
| Race | |
| White | 80% |
| Black | 7.1% |
| Other | 1.9% |
| Not recorded | 11% |
| Laterality of Paralysis | |
| Right | 40% |
| Left | 60% |
| Mobility | |
| Reduced mobility | 19% |
| Complete immobility | 81% |
| Closure* at presentation | |
| Incomplete | 48% |
| Complete | 44% |
| Not recorded | 8.0% |
Vocal folds meet with phonatory effort
Etiology
Etiologies were varied and included surgery (48%, 304/633), idiopathic (37%, 234/633), intubation (4.9%, 31/633), trauma (3.8%, 24/633), malignancy-related (3.6%, 23/633), cerebrovascular accident (1.6%, 10/633), and others (Table 2). Thyroid operations represented the most common surgical etiology for UVFP (32%, 98/304) followed by anterior cervical disk fusion (ACDF) (20%, 61/304). Overall, 60% (378/633) of patients had left-sided paralyses. Significant side propensities exist based on etiology (Figure 1).
Table 2.
Etiology of Unilateral Vocal Fold Paralysis
| Surgery | 304 (48%) |
| Thyroid surgery | 98 (15%) |
| Cervical spine surgery | 61 (9.6%) |
| Lung surgery | 34 (5.4%) |
| Mediastinal surgery | 28 (4.4%) |
| Carotid surgery | 24 (3.9%) |
| Esophageal surgery | 14 (2.2%) |
| Skull base surgery | 11 (1.7%) |
| Lateral neck surgery | 9 (1.4%) |
| Cardiac surgery | 9 (1.4%) |
| Parathyroid surgery | 7 (1.1%) |
| Intrinsic neurosurgery | 5 (0.80%) |
| Oral surgery | 2 (0.32%) |
| Open neck lymph node biopsy | 1 (0.16%) |
| Vagal nerve stimulator placement | 1 (0.16%) |
| Idiopathic | 234 (37%) |
| Intubation | 31 (4.9%) |
| Only for surgical procedure | 19 (3.0%) |
| <1 week | 3 (0.47%) |
| 1 – 2 weeks | 2 (0.32%) |
| >2 weeks | 2 (0.32%) |
| Not specified | 5 (0.79%) |
| Trauma | 24 (3.8%) |
| Malignancy-Related | 23 (3.6%) |
| Lung cancer | 12 (1.9%) |
| Paraganglioma | 3 (0.47%) |
| Oropharyngeal cancer | 2 (0.32%) |
| Esophageal cancer | 2 (0.32%) |
| Thyroid cancer | 1 (0.16%) |
| Laryngeal cancer | 1 (0.16%) |
| Lymphoma | 1 (0.16%) |
| Metastatic cancer | 1 (0.16%) |
| Other | 16 (2.5%) |
| Cerebrovascular accident | 10 (1.6%) |
| Asthma attack | 1 (0.16%) |
| Allergy to contrast | 1 (0.16%) |
| Esophagogastroduodenoscopy | 1 (0.16%) |
| Nasogastric tube | 1 (0.16%) |
| Seizure | 1 (0.16%) |
| Vagal nerve stimulator | 1 (0.16%) |
Figure 1.
Side propensity (skew) of unilateral vocal fold paralysis based on etiology is shown. The dashed line represents no skew with those farther from the line demonstrating greater side propensity. Black circles indicate statistically significant skew for that etiology.
Time to Presentation
Community Otolaryngology
In all, community otolaryngologists saw 54% (341/633) of patients that were eventually seen at the academic center. Median time from UVFP symptoms onset to being seen by a community otolaryngologist was two months (IQR 1 – 5; Range <1 week – 144 months; Table 3). Management of these patients consisted of observation and supportive care (58%; 199/341), surgery (30%; 103/341), voice therapy (7.3%; 25/341), and both voice therapy and surgery (4.1%; 14/341). Surgical interventions included injection augmentation (78/123), framework surgery (24/123), and injection augmentation followed by framework surgery (21/123). In the community setting, there were a median 4 (IQR 1 – 10.5, range 1 – 120) and twelve months (IQR 6 – 26, range 1 – 216) from symptom onset to injection augmentation and framework surgery, respectively.
Table 3.
Months from UVFP symptom onset to presentation to community otolaryngology and/or academic center
| Community | Academic Primary* | Academic Secondary** | Overall | |
|---|---|---|---|---|
| Symptom Onset to Presentation | 2m [1 – 5; 1 – 144] | 4m (2 – 9; 1 – 672] | 9m [5 – 24; 1 – 576] | 6m (3 – 15; 1 – 672) |
| Symptom Onset to Surgery | ||||
| Injection | 4m [1 – 10.5, 1 – 120] | 4.5m (3 – 8; 2 – 109) | 7m (5 – 14; 2 – 433) | 6m [4 – 10; 2 – 433) |
| Framework | 12m [6 – 26; 1 – 216] | 11m (7 – 20; 3 – 433) | 17m (12 – 33; 2 – 415) | 16m [11 – 33; 2 – 433) |
| Overall | 5m (1 – 11; 1 – 216) | 6m (3 – 11; 2 – 433) | 13m (7 – 25; 2 – 433) | 10m (5 – 19; 2 – 433) |
Median months (Interquartile Range; Range)
Primary = seen at academic center without prior outside otolaryngology consultation
Secondary = seen at academic center after outside otolaryngology consultation
Academic Center
A total of 292 UVFP patients presented directly to the academic center within a median four months after symptom onset (IQR 2 – 9, range <1 – 672) compared with nine months (IQR 5 – 24, range <1 – 576) if seen previously by a community otolaryngologist (chi2=68.0 p=0.0001) (Table 3). Among these patients, treatments employed were observation/supportive care (53%; 156/292), surgery (36%; 105/292), voice therapy (6.9%; 20/292), and both voice therapy and surgery (3.8%; 11/292). In order, operations were injection augmentation (72%; 82/114), framework surgery (17%; 19/114), and injection augmentation followed by framework surgery (11%; 13/114). Of those injected, 14% went on to undergo framework surgery (13/95). The remainder avoided further intervention because of symptomatic improvement (66%, 63/95), loss to follow-up (12%, 11/95), death (6.3%, 6/95) or due to another reason (2.1%, 2/95).
Ultimate Treatment for UVFP
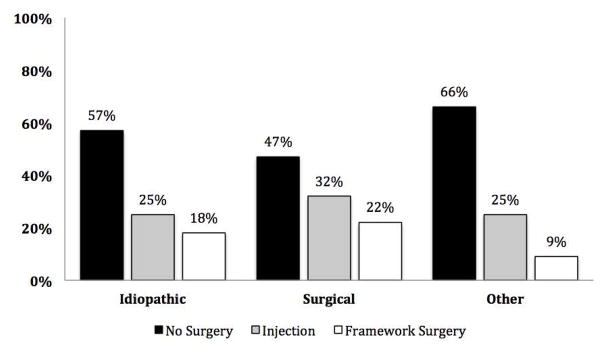
“Ultimate treatment” was defined as the terminal procedure performed to rehabilitate each of the 633 patients in the cohort regardless of whether it was performed in the community or academic setting. Options include 1) no procedure/operation, 2) injection augmentation, or 3) framework surgery. In all, 46% required no procedure/operation. 28% and 26% had an injection augmentation and framework surgery as the ultimate treatment, respectively. Treatment distribution differed based on whether the etiology was surgery, idiopathic, or other (Pearson chi2=27.7, p<0.001; Figure 2). There was no difference in rate of injection between etiologic categories (Pearson chi2=3.70; p=0.16). In contrast, framework surgery was performed more often among patients with surgically-induced than those with idiopathic (Pearson chi2=10.8, p=0.001) or other UVFP etiologies (Pearson chi2=9.92, p=0.002).
Figure 2.
Ultimate treatment based on etiology of unilateral vocal fold paralysis
Factors Associated with Framework Surgery
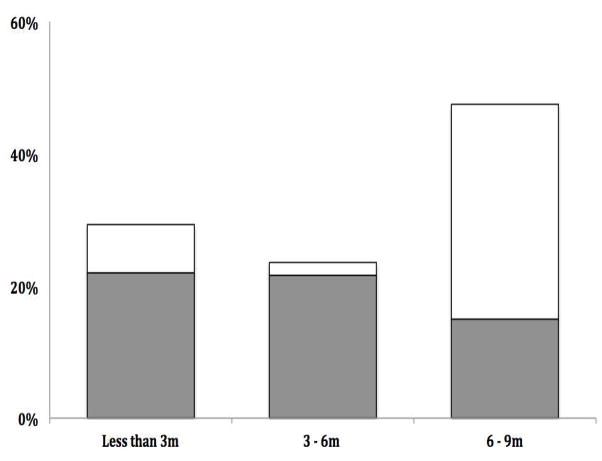
From the cohort of 633 UVFP patients, 325 met inclusion criteria. Less than half (41%, 132/325) underwent a rehabilitative procedure and of these, 87% (115/132) had injection augmentation. All injection naïve patients ultimately underwent framework surgery (17/17). In comparison, 19% (23/115) who had undergone prior injection later received framework surgery (Pearson chi2=44.9, p<0.001). Patients who were injected presented earlier than those who were not [median 4 months (IQR 2 – 5) vs. 7 months (IQR 6 – 8); chi2=12.2, p<0.001]. Framework surgery was more commonly performed in patients presenting between 6 and 9 months than in either the 0 – 3 or 3 – 6 month period after symptom onset (chi2=8.06; p=0.018) (Figure 3). During this later time interval, 68% of framework surgeries were performed without antecedent injection augmentation.
Figure 3.
Percent of patients who had framework surgery with (grey) or without (white) prior injection augmentation based on months from symptom onset to presentation at academic center
Table 4 compares characteristics among injected patients based on whether they ultimately underwent definitive framework surgery. There was no difference in time to injection, age, gender, or vocal fold closure at presentation or paralysis side between groups. Etiology distribution differed non-significantly between groups (chi2=3.18, p=0.075). Patients with a surgical etiology had a higher rate of framework surgery than either idiopathic or other etiologies. Multivariate logistic regression adjusting for etiology, found that time to injection augmentation did not affect odds of ultimately undergoing framework surgery (OR 1.13, CI 0.92 – 1.40; p=0.23) (Table 5). Compared to non-surgical etiologies, those caused by surgery were associated with increased odds of needing framework surgery (OR 4.25, CI 0.90 – 20.1; p=0.07).
Table 4.
Comparison of injected patients based on whether they ultimately underwent framework surgery
| Framework Surgery? | |||
|---|---|---|---|
| Characteristics | NO (N=92) | YES (n=23) | P |
| Age, median (IQR) | 61 (51.5 – 70) | 64 (52 – 71) | 0.72 |
| Gender | |||
| Male | 55% | 56% | 0.93 |
| Female | 45% | 44% | |
| Etiology | |||
| Non-Surgical | 74% | 21% | 0.08 |
| Surgical | 26% | 2% | |
| Complete VF closure* | 32% | 41% | 0.42 |
| Paralysis Side | |||
| Right | 37% | 35% | 0.85 |
| Left | 63% | 65% | |
| Duration of symptoms**, median (IQR) | 4m (2 – 5) | 4m (2 – 6) | 0.32 |
IQR = Interquartile range
VF = vocal fold; vocal fold closure was complete with maximal effort at initial presentation to laryngology
Complete vocal fold closure with maximal effort on flexible laryngoscopy
Duration of UVFP symptoms prior to treatment
Table 5.
Multivariate Analysis of Predictors of Framework Surgery among patients who underwent injection augmentation
| Characteristics | Odds Ratio | 95% CI | P |
|---|---|---|---|
| Etiology | |||
| Non-surgical | Reference | ||
| Surgical | 4.25 | 0.90 – 20.1 | 0.068 |
| Months before treatment | 1.13 | 0.92 – 1.40 | 0.233 |
DISCUSSION
The standard approach to treating symptomatic unilateral vocal fold paralysis (UVFP) is to reestablish vocal fold closure through surgical modification of the affected vocal fold position (e.g., injection augmentation, framework surgery). There is clinical suspicion that patients who undergo earlier injection augmentation for UVFP appear less likely to require definitive framework surgery – a surrogate for vocal fold recovery13–15. This has raised the question whether injection augmentation promotes recovery. The biologic mechanism underlying this observation is unclear, and there is concern that the association may be related to selection bias.
Bias in this setting would provide a distorted estimate of the effect of injection augmentation, and would arise from the way patients were selected for early injection, or differential surveillance, diagnosis, and referral into the study17. In this setting, patients diagnosed earlier are more likely to have spontaneous recovery12. Moreover, UVFP patients presenting earlier to an otolaryngologist are more likely to have injection augmentation earlier. The potential misattribution of recovery to injection is illustrated in a population-based study in which nearly half of the 142 monitored and untreated cases of unilateral vocal fold paralyses had spontaneous recovery between 1 – 6 week and 6 months follow-up visits18. Thus, there is a risk of falsely attributing recovery to the injection when, in fact, it may have occurred spontaneously.
Our study aimed to further investigate this clinical observation and analyze whether early injection augmentation for UVFP reduces odds of ultimately requiring definitive framework surgery. To address the risk of this bias, the stepwise multivariate analysis included time to otolaryngology presentation for treatment as a continuous variable and the UVFP etiology (surgery, non-surgical). In contrast with previous studies, our results demonstrated that timing of injection augmentation within the first nine months did not change odds of requiring framework surgery. In other words, earlier injection did not affect the chance of ultimately needing a more permanent intervention. This corroborates recent findings from the Pei et al. open-label randomized trial in which early hyaluronate injection did not improve nerve regeneration, but it made a significant impact on patient quality of life19.
Several previous studies have considered this relationship. Yung et al. found that 26% (5/19) of patients injected versus 66% (23/35) of patients not injected ultimately required definitive type I laryngoplasty13. Another study by Friedman et al. that compared early (<6 months from onset) versus late (>6 months from onset) injection augmentation for UVFP found 62.5% (20/32) patients who were injected early were able to avoid definitive open surgery due to persistent improvement compared with 0% (0/3) who were injected later14. Alghonaim et al. using a similar study design concluded that earlier augmentation diminished the likelihood of needing framework surgery15. The observed associations in these prior case series could alternatively be explained by selection bias; those presenting earlier were diagnosed with UVFP earlier and therefore had a higher likelihood of spontaneous recovery regardless of intervention type (or lack thereof).
Time to Treatment
Regardless of whether injection augmentation affects vocal fold recovery, there is a clear advantage to early treatment of the UVFP attributed symptoms in order improve patient quality of life19,20. Without a temporizing injection patients often wait 6 – 12 months with debilitating voice, swallowing, and breathing difficulties until they are considered candidates for definitive framework surgery. Therefore, shorter time to otolaryngology presentation is preferable. The present study audited the time to presentation to community and to the academic center to better understand current practice.
UVFP patients presented to community otolaryngologists within 2 months of symptom onset. Interval to presentation to the academic center depended on whether they had a previous consultation. Those presenting directly to the academic center were seen 2.5 months earlier than those evaluated elsewhere first (4.5 versus 7 months). These intervals are similar to those reported by Spataro et al.16. Time to treatment also varied by practice pattern. Community otolaryngologists saw patients earlier, but deferred treatment a median of two months, presumably to allow for spontaneous recovery. In contrast, patients presented to the academic center later and underwent initial intervention earlier, usually within the first month of presentation. Understanding these practice patterns is a first step toward optimizing care in the UVFP population. Earlier injection and/or referral may prevent short-term UVFP associated disability.
Etiology
In this cohort, nearly half (46%) of patients did not undergo any rehabilitative operation. Patients who had a surgical cause of UVFP were more likely to undergo framework surgery. In contrast those with idiopathic and other etiologies were more often managed with supportive care and avoided definitive surgery. Etiologies encountered in this study coincide with those described in large case series in the literature16,21–24. Similarly, the laterality propensity based on etiology corresponds closely that described in a recent study16. No other patient or disease characteristic was associated with worse or better prognosis.
Limitations
Results must be considered in context of the inherent limitations of its retrospective cohort study design. Moreover, any study showing change in vocal fold functional recovery can be confounded by a baseline and spontaneous recovery rate, which is exemplified by the transience of UVFP after many surgical procedures11,18,25–27. Also, avoidance of framework surgery is a surrogate outcome for sufficient recovery to mitigate patient symptoms. It is considered an important outcome because the decision to undergo definitive surgery is patient-driven, based on symptoms and effect on quality of life.
CONCLUSIONS
Nearly half of UVFP patients do not require any surgical intervention. When indicated, injection augmentation is highly effective at temporarily alleviating attributable symptoms and improving quality of life. However, it does not reduce the likelihood of needing definitive surgical intervention in patients with UVFP. Understanding practice patterns and fostering early detection and treatment may improve quality of life in this population. Further studies assessing the relationship the effect of injection augmentation on need for ultimate framework surgery must carefully consider and control for selection bias.
Acknowledgments
Dr. Francis is supported by NIH NIDCD K23DC013559. The project described was also supported by CTSA award No. UL1TR000445 from the National Center for Advancing Translational Sciences.
Footnotes
Conflicts of Interest: None by any authors
Its contents are solely the responsibility of the authors and do not necessarily represent official views of the National Center for Advancing Translational Sciences or the National Institutes of Health.
Financial Disclosures: Dr. Francis is supported through NIH/NIDCD K23DC013559
References
- 1.Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA. 2006;295:2164–2167. doi: 10.1001/jama.295.18.2164. [DOI] [PubMed] [Google Scholar]
- 2.Davies L, Welch HG. Current thyroid cancer trends in the United States. JAMA Otolaryngol Head Neck Surg. 2014;140:317–322. doi: 10.1001/jamaoto.2014.1. [DOI] [PubMed] [Google Scholar]
- 3.Marawar S, Girardi FP, Sama AA, et al. National trends in anterior cervical fusion procedures. Spine. 2010;35:1454–1459. doi: 10.1097/BRS.0b013e3181bef3cb. [DOI] [PubMed] [Google Scholar]
- 4.Kriskovich MD, Apfelbaum RI, Haller JR. Vocal fold paralysis after anterior cervical spine surgery: incidence, mechanism, and prevention of injury. Laryngoscope. 2000;110:1467–1473. doi: 10.1097/00005537-200009000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Jung A, Schramm J, Lehnerdt K, Herberhold C. Recurrent laryngeal nerve palsy during anterior cervical spine surgery: a prospective study. Journal of neurosurgery Spine. 2005;2:123–127. doi: 10.3171/spi.2005.2.2.0123. [DOI] [PubMed] [Google Scholar]
- 6.Cohen SM, Dupont WD, Courey MS. Quality-of-life impact of non-neoplastic voice disorders: a meta-analysis. Ann Otol Rhinol Laryngol. 2006;115:128–134. doi: 10.1177/000348940611500209. [DOI] [PubMed] [Google Scholar]
- 7.Fang TJ, Li HY, Gliklich RE, Chen YH, Wang PC, Chuang HF. Quality of life measures and predictors for adults with unilateral vocal cord paralysis. Laryngoscope. 2008;118:1837–1841. doi: 10.1097/MLG.0b013e31817e7431. [DOI] [PubMed] [Google Scholar]
- 8.Misono S, Merati AL. Evidence-based practice: evaluation and management of unilateral vocal fold paralysis. Otolaryngologic clinics of North America. 2012;45:1083–1108. doi: 10.1016/j.otc.2012.06.011. [DOI] [PubMed] [Google Scholar]
- 9.Carroll TL, Rosen CA. Trial vocal fold injection. Journal of voice : official journal of the Voice Foundation. 2010;24:494–498. doi: 10.1016/j.jvoice.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 10.Jeannon JP, Orabi AA, Bruch GA, Abdalsalam HA, Simo R. Diagnosis of recurrent laryngeal nerve palsy after thyroidectomy: a systematic review. Int J Clin Pract. 2009;63:624–629. doi: 10.1111/j.1742-1241.2008.01875.x. [DOI] [PubMed] [Google Scholar]
- 11.Francis DO, Pearce EC, Ni S, Garrett CG, Penson DF. Epidemiology of vocal fold paralyses after total thyroidectomy for well-differentiated thyroid cancer in a Medicare population. Otolaryngol Head Neck Surg. 2014;150:548–557. doi: 10.1177/0194599814521381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sulica L. The natural history of idiopathic unilateral vocal fold paralysis: evidence and problems. Laryngoscope. 2008;118:1303–1307. doi: 10.1097/MLG.0b013e31816f27ee. [DOI] [PubMed] [Google Scholar]
- 13.Yung KC, Likhterov I, Courey MS. Effect of temporary vocal fold injection medialization on the rate of permanent medialization laryngoplasty in unilateral vocal fold paralysis patients. Laryngoscope. 2011;121:2191–2194. doi: 10.1002/lary.21965. [DOI] [PubMed] [Google Scholar]
- 14.Friedman AD, Burns JA, Heaton JT, Zeitels SM. Early versus late injection medialization for unilateral vocal cord paralysis. Laryngoscope. 2010;120:2042–2046. doi: 10.1002/lary.21097. [DOI] [PubMed] [Google Scholar]
- 15.Alghonaim Y, Roskies M, Kost K, Young J. Evaluating the timing of injection laryngoplasty for vocal fold paralysis in an attempt to avoid future type 1 thyroplasty. Journal of otolaryngology - head & neck surgery = Le Journal d’oto-rhino-laryngologie et de chirurgie cervico-faciale. 2013;42:24. doi: 10.1186/1916-0216-42-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Spataro EA, Grindler DJ, Paniello RC. Etiology and Time to Presentation of Unilateral Vocal Fold Paralysis. Otolaryngol Head Neck Surg. 2014;151:286–293. doi: 10.1177/0194599814531733. [DOI] [PubMed] [Google Scholar]
- 17.Hennekens CHBJE. Epidemiology in Medicine. Little, Brown, and Co; 1987. [Google Scholar]
- 18.Bergenfelz A, Jansson S, Kristoffersson A, et al. Complications to thyroid surgery: results as reported in a database from a multicenter audit comprising 3,660 patients. Langenbecks Arch Surg. 2008;393:667–673. doi: 10.1007/s00423-008-0366-7. [DOI] [PubMed] [Google Scholar]
- 19.Pei YC, Fang TJ, Hsin LJ, Li HY, Wong AM. Early hyaluronate injection improves quality of life but not neural recovery in unilateral vocal fold paralysis: An open-label randomized controlled study. Restorative neurology and neuroscience. 2015;33:121–130. doi: 10.3233/RNN-140439. [DOI] [PubMed] [Google Scholar]
- 20.Chandrasekhar SS, Randolph GW, Seidman MD, et al. Clinical practice guideline: improving voice outcomes after thyroid surgery. Otolaryngol Head Neck Surg. 2013;148:S1–37. doi: 10.1177/0194599813487301. [DOI] [PubMed] [Google Scholar]
- 21.Rosenthal LH, Benninger MS, Deeb RH. Vocal fold immobility: a longitudinal analysis of etiology over 20 years. Laryngoscope. 2007;117:1864–1870. doi: 10.1097/MLG.0b013e3180de4d49. [DOI] [PubMed] [Google Scholar]
- 22.Merati AL, Shemirani N, Smith TL, Toohill RJ. Changing trends in the nature of vocal fold motion impairment. American journal of otolaryngology. 2006;27:106–108. doi: 10.1016/j.amjoto.2005.07.020. [DOI] [PubMed] [Google Scholar]
- 23.Ko HC, Lee LA, Li HY, Fang TJ. Etiologic features in patients with unilateral vocal fold paralysis in Taiwan. Chang Gung medical journal. 2009;32:290–296. [PubMed] [Google Scholar]
- 24.Chen HC, Jen YM, Wang CH, Lee JC, Lin YS. Etiology of vocal cord paralysis. ORL; journal for oto-rhino-laryngology and its related specialties. 2007;69:167–171. doi: 10.1159/000099226. [DOI] [PubMed] [Google Scholar]
- 25.Godballe C, Madsen AR, Sorensen CH, et al. Risk factors for recurrent nerve palsy after thyroid surgery: a national study of patients treated at Danish departments of ENT Head and Neck Surgery. Eur Arch Otorhinolaryngol. 2013 doi: 10.1007/s00405-013-2767-7. [DOI] [PubMed] [Google Scholar]
- 26.Rosato L, Avenia N, Bernante P, et al. Complications of thyroid surgery: analysis of a multicentric study on 14,934 patients operated on in Italy over 5 years. World J Surg. 2004;28:271–276. doi: 10.1007/s00268-003-6903-1. [DOI] [PubMed] [Google Scholar]
- 27.Thomusch O, Machens A, Sekulla C, et al. Multivariate analysis of risk factors for postoperative complications in benign goiter surgery: prospective multicenter study in Germany. World J Surg. 2000;24:1335–1341. doi: 10.1007/s002680010221. [DOI] [PubMed] [Google Scholar]