Abstract
Background
Cast Chromium Cobalt alloy has been the material of choice for fabricating Removable Partial Dentures (RPDs) but has certain drawbacks. Newer materials like the flexible Nylon based Super Polyamide have been introduced to overcome these drawbacks. The present study has compared the above two materials for nine clinical parameters.
Method
The study was carried out on 30 patients presenting with a Kennedy Applegate class II partially edentulous situation who were divided into two equal groups and clinically assessed.
Result
Statistically significant results were obtained in favor of flexible RPDs, in the parameters of ‘aesthetics’ and ‘overall patient satisfaction’. Both groups showed more or less similar values for ‘frequency of fracture of the prosthesis during usage’ with the incidence being slightly higher for patients wearing the cast RPDs. The clinical parameters of ‘oral soft tissue tolerance’, ‘gingival health’, ‘periodontal health’ and ‘adaptability in areas with undercut’ were statistically at par for all the 30 patients thus suggesting the comparable biocompatibility of the two materials. The highlight of this study was the relative ease in fabrication of the flexible RPDs as compared to the cast RPDs.
Conclusion
Based on the favorable clinical results of this study, it can be summarized that the flexible RPDs is a viable alternative to cast RPDs in Kennedy Applegate class II partially edentulous situation in the short term.
Keywords: Kennedy Applegate class II partially edentulous situation, Cast chromium cobalt alloy removable partial denture, Flexible removable partial denture, Clinical comparison
Introduction
Removable Partial Dentures (RPDs) are provided to restore facial form and masticatory function after tooth loss. Chromium–Cobalt (Cr–Co) alloy has been traditionally used as the material of choice in the fabrication of definitive cast RPDs, since 1929.1 However, in the Kennedy Applegate class II partially edentulous condition, the use of metal alloys together with the design considerations pose unique challenges to the esthetic and biological acceptance of the restoration.2
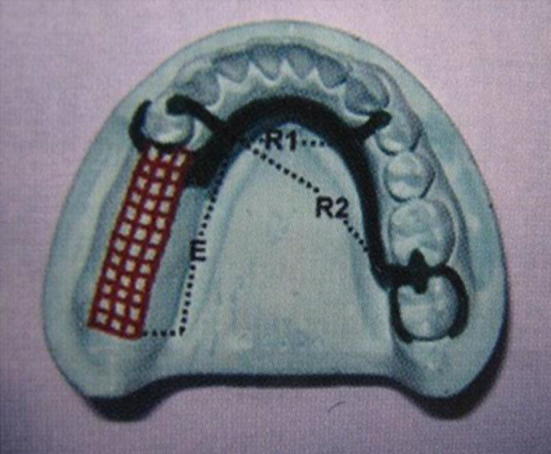
In this clinical situation, the conventional circumferential clasp design along with the distal occlusal rest, instead of transferring the forces along the long axis of the terminal abutment, causes torquing which intensifies as the ridge resorbs3, 4 (Fig. 1). This adversely affects denture function and causes patient discomfort by traumatizing the supporting tissues. In a bid to counter the deleterious effect of such forces, special clasp designs and stress breakers have been employed.5, 6, 7, 8 However, these designs are technique sensitive, involve invasive procedures and are expensive because of the complexity of design and skill required. Moreover, the cast clasps are unsightly and pose problems in bilateral inoperable undercuts, along with difficulty in reline and repair procedures.
Fig. 1.
Unilateral distal extension RPD acts as class I lever. Conventional circumferential clasp with disto-occlusal rest induces torque stresses on the abutment.
Recent improvisations to the nylon based thermoplastic resins are promising as an alternate material which could overcome the challenges posed by the cast metal RPDs. They have been introduced as super polyamide wherein the resin polymers are reinforced with glass fillers or aramid fibers to produce a material which is much more stable in nature and provides resistance to polymer unzipping. This material is claimed to have higher creep resistance, flexibility, fatigue endurance, dimensional stability, wear characteristics and solvent resistance. It also matches tooth and tissue color, is light weight and heat resistant.
There is a paucity of literature on the efficacy of this material as a substitute for cast chromium cobalt alloy and needs testing in various clinical situations to allow universal acceptance. This in vivo study was therefore undertaken to compare the clinical efficacy and use of RPDs made of the nylon based super polyamide with those made of the age old Cast Cr–Co alloy (employing the circumferential clasp design with distal occlusal rests), in Kennedy Applegate class II partially edentulous situations.
Material and methods
30 patients presenting with Kennedy Applegate class II partially edentulous situation were randomly selected for the study out of those who reported to the daily OPD of Command Military Dental Centre (Western Command). These patients were individuals between age group of 25–45 years, from a middle income group/socioeconomic strata, medically fit, having an average oral health status and without any significant deleterious habits. Approval of ethical committee was taken. Patient's written consent for undergoing this study was recorded in the individual's clinical assessment form.
After thorough oral prophylaxis and preliminary dental treatment in the form of restorations, extractions and occlusal equilibration wherever required, these 30 patients were randomly assigned to two groups of 15 patients each i.e. Group A and Group B. Group A patients received RPDs made of cast Cr–Co alloy incorporating the cast circumferential clasps with distal occlusal rests and denture bases made of heat cured poly methyl methacrylate (PMMA) (ProBase Hot, Ivoclar Vivadent, USA) resin. Group B patients received flexible RPDs made of the nylon based super polyamide resin. After insertion of the prosthesis, their Clinical performances were reviewed periodically during one and half years for the nine parameters as listed in Table 1. The periodicity of recall was twenty four hours, one week, one month, three months and six months after insertion of prostheses.
Table 1.
Clinical parameters observed.
| Clinical parameter assessed | Feature of parameter observed | Scores | |
|---|---|---|---|
| 1 | Esthetics Subjective Assessment | Question: Are you happy with the way your prosthesis looks? | Not satisfactory – Score of 0 Satisfactory – Score of 1 Highly satisfactory – Score of 2 |
| 2 | Esthetics; objective assessment | Was made by the use of clinical photographs. Both extra oral and intra oral photographs were taken. | Not satisfactory – Score of 0 Satisfactory – Score of 1 Highly satisfactory – Score of 2 |
| 3 | Oral soft tissue tolerance; subjective assessment: | Question: Do you have any sore spots in your mouth? | Answer: Yes/No No discomfort at all – Score of 0 Slight Discomfort, but not affecting the wear of the RPD – Score of 1 Discomfort, causing intermittent wear – Score of 2 Discomfort sufficient for patient to totally discontinue wear of the RPD – Score of 3 |
| 4 | Oral soft tissue tolerance; objective assessment: | Observing redness, inflammation, soreness or ulceration | No redness, inflammation, soreness or ulceration seen – Score of 0 Frank redness, inflammation, soreness or ulceration seen – Score of 1 |
| 5 | Gingival health | Was assessed using Gingival index of Loe H and Sillness J (1963): | Absence of inflammation/Normal gingiva – Score of 0 Mild inflammation, slight change in color, slight edema, no bleeding on probing – Score of 1 Moderate inflammation, moderate glazing, redness, edema and hypertrophy, bleeding on probing – Score of 2 Severe inflammation, marked redness and hypertrophy. Ulcerations and tendency to spontaneous bleeding – Score of 3 |
| 6 | Periodontal health | Was assessed using periodontal index of AL Russell (1967): | Clinically normal supportive tissues – Score of 0–0.2 Simple gingivitis – Score of 0.3–0.9 Beginning destructive periodontal disease – Score of 0.7–1.9, reversible stage of disease Established destructive periodontal disease – Score of 1.6–5.0, irreversible stage of disease Terminal disease – Score of 3.8–8.0, Irreversible stage of disease |
| 7 | Adaptability in areas with undercut, Objective assessment | Whether undercuts required a block out or not | Undercuts did not require to be blocked out – Score of 0 Undercuts had to be blocked out – Score of 1 |
| 8 | Frequency of fracture/repair of the RPD; objective assessment | Whether fracture of any component of partial denture occurred? | Fracture of partial denture component occurred – Score of 0 Fracture of partial denture component did not occur – Score of 1 |
| 9 | Overall patient satisfaction; subjective assessment | Question: Are you satisfied with your prosthesis? | Answer: Not satisfied – Score of 0 Satisfaction level is adequate – Score of 1 Satisfaction level is good – Score of 2 Satisfaction level is very good – Score of 3 |
Fabrication and insertion of conventional cast Cr–Co alloy RPD for Group A patients
All the cast RPDs were fabricated from the same material (Bego, Germany). Diagnostic casts of each individual patient's mouth were obtained after routine impression procedures and thereafter surveyed using the Ney's dental surveyor. Whenever required, the abutment teeth were prepared to receive Full metal/Ceramo-metal coronal coverage (Wiron 99, Bego, Germany & Ceramco, Dentsply, USA). After mouth preparation, preliminary impressions in a reasonably fitting perforated stainless steel stock tray using Polyvinyl Siloxane impression material (3M ESPE, USA) were made. Secondary impressions were made using a customized impression tray made of chemically cured PMMA resin and the altered cast technique was adopted to ensure that the fabricated metal framework and the acrylic Denture Base will be related in the same relationship as that which exists between the abutment teeth and the supporting mucosa when the base is subjected to occlusal loads.
The master casts were modified for location of retentive and reciprocating clasp arms. This modified cast was then duplicated using reversible hydrocolloid to produce the refractory cast. Wax pattern framework was formulated on this refractory cast which was followed by spruing, investing, burnout, casting and finishing of the removable partial denture framework. Record bases of chemically cured PMMA resin were fabricated with the framework seated on the secondary cast obtained from the altered cast technique. Standard procedures were employed for jaw relation records, teeth arrangements, clinical try-in and acrylisation, to obtain individual cast Cr–Co alloy RPDs (Fig. 2).
Fig. 2.

Post op view of inserted cast RPD in Mandibular arch.
Fabrication and insertion of flexible RPDs for Group B patients
The materials and equipment employed for fabrication of the flexible RPDs were from Valplast (USA). Initial impressions with reversible hydrocolloid (JeltrateA, Dentsply, USA) in a properly selected stock tray were made which suffices for the fabrications of the flexible RPDs. Impressions were poured with die stone (Valstone, Valplast, USA). Master casts thus obtained were visually surveyed to determine the path of insertion.
After the master cast was designed and prepared it was duplicated using reversible hydrocolloid. The relief and blocking wax from the master cast was removed by boiling and this was then articulated for teeth set up and try-in. Next the set up was transferred on to the duplicate model. The buccal and labial saddles were waxed by flowing very hot flush of wax to achieve a uniform thickness of 1.5 mm and then trimmed to the design line. Preformed palate (thickness of 1.5 mm)/lingual bar (2 mm border thickness narrowing to 1 mm) wax patterns were softened, adapted and trimmed including the region around the necks of the teeth. The wax up was flamed gently to obtain a smooth surface. The teeth were cleaned and occlusion was checked once again.
The waxed casts along with the teeth set up were invested in the recommended valplast flask and sprued. After boil out and bench cooling, the acrylic teeth were prepared for mechanical retention. After preparation, each tooth was cemented back into its place in the top half of the flask with valcement (cement provided with the valplast system which neither discolors with the heat of injection nor does it bond permanently with the surface of the teeth as cyanoacrylate or other cementing agents do). The flasks were then injection molded with the recommended valplast resin cartridge (Valplast, USA) and polymerized followed by bench cooling for thirty minutes. The prostheses were thereafter carefully retrieved from the flask, finished, polished, washed thoroughly in an ultrasonic cleaner, disinfected and inserted (Fig. 3).
Fig. 3.

Post op view of maxillary arch with valplast RPD in situ.
Results
Clinically assessed values for the above cited nine clinical parameters are tabulated in Table 2A, Table 2B for Group A and B respectively. The mean and standard deviation of these values are plotted in Table 3. Results and statistical analysis for these 30 patients was further tabulated using Nonparametric; Man Whitney test and Cross Tabulations.
Table 2A.
Cast chromium cobalt alloy RPD.
| Clinical cases | Prosthesis inserted | Esthetics; subjective assessment | Esthetics; objective assessment | Oral soft tissue tolerance; subjective assessment | Oral soft tissue tolerance; objective assessment | Gingival health | Periodontal health | Adaptability in areas with undercut | Frequency of fracture | Overall patient satisfaction |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Cast RPD | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| 2 | Cast RPD | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 |
| 3 | Cast RPD | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 |
| 4 | Cast RPD | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 2 |
| 5 | Cast RPD | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| 6 | Cast RPD | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 2 |
| 7 | Cast RPD | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 2 |
| 8 | Cast RPD | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 |
| 9 | Cast RPD | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 2 |
| 10 | Cast RPD | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 |
| 11 | Cast RPD | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 2 |
| 12 | Cast RPD | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 2 |
| 13 | Cast RPD | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| 14 | Cast RPD | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 |
| 15 | Cast RPD | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 2 |
Table 2B.
Nylon based super polyamide (Valplast, Flexible RPD).
| Clinical cases | Prosthesis inserted | Esthetics; subjective assessment | Esthetics; objective assessment | Oral soft tissue tolerance; subjective assessment | Oral soft tissue tolerance; objective assessment | Gingival health | Periodontal health | Adaptability in areas with undercut | Frequency of fracture | Overall patient satisfaction |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Flexible RPD | 2 | 2 | 1 | 0 | 0 | 0 | 1 | 1 | 2 |
| 2 | Flexible RPD | 2 | 2 | 1 | 0 | 0 | 0 | 1 | 1 | 2 |
| 3 | Flexible RPD | 2 | 2 | 0 | 0 | 0 | 0 | 1 | 1 | 2 |
| 4 | Flexible RPD | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 |
| 5 | Flexible RPD | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 2 |
| 6 | Flexible RPD | 1 | 2 | 0 | 0 | 0 | 0 | 1 | 1 | 1 |
| 7 | Flexible rpd | 2 | 2 | 0 | 0 | 0 | 0 | 1 | 1 | 2 |
| 8 | Flexible RPD | 2 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 2 |
| 9 | Flexible RPD | 2 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 2 |
| 10 | Flexible RPD | 2 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 2 |
| 11 | Flexible RPD | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 3 |
| 12 | Flexible RPD | 2 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 3 |
| 13 | Flexible RPD | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| 14 | Flexible RPD | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| 15 | Flexible RPD | 2 | 2 | 0 | 0 | 0 | 0 | 1 | 0 | 3 |
Table 3.
Mean & standard deviation – statistical analysis.
| Group | Esthetics; subjective assessment | Esthetics; objective assessment | Oral soft tissue tolerance; subjective assessment | Oral soft tissue tolerance; objective assessment | Gingival health | Periodontal health | Adaptability In areas with undercut | Frequency of fracture | Overall patient satisfaction | |
|---|---|---|---|---|---|---|---|---|---|---|
| Flexible RPD | Mean | 1.67 | 1.4 | 0.27 | 0 | 0 | 0 | 0.73 | 0.67 | 2.07 |
| N | 15 | 15 | 15 | 15 | 15 | 15 | 15 | 15 | 15 | |
| Std. Deviation | 0.488 | 0.507 | 0.458 | 0 | 0 | 0 | 0.458 | 0.488 | 0.594 | |
| Minimum | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | |
| Maximum | 2 | 2 | 1 | 0 | 0 | 0 | 1 | 1 | 3 | |
| Median | 2 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 2 | |
| Cast RPD | Mean | 0.67 | 0 | 0.13 | 0 | 0 | 0 | 0.87 | 0.8 | 1.47 |
| N | 15 | 15 | 15 | 15 | 15 | 15 | 15 | 15 | 15 | |
| Std. Deviation | 0.488 | 0 | 0.352 | 0 | 0 | 0 | 0.352 | 0.414 | 0.516 | |
| Minimum | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | |
| Maximum | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 2 | |
| Median | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | |
| Total | Mean | 1.17 | 0.7 | 0.2 | 0 | 0 | 0 | 0.8 | 0.73 | 1.77 |
| N | 30 | 30 | 30 | 30 | 30 | 30 | 30 | 30 | 30 | |
| Std. Deviation | 0.699 | 0.794 | 0.407 | 0 | 0 | 0 | 0.407 | 0.45 | 0.626 | |
| Minimum | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | |
| Maximum | 2 | 2 | 1 | 0 | 0 | 0 | 1 | 1 | 3 | |
| Median | 1 | 0.5 | 0 | 0 | 0 | 0 | 1 | 1 | 2 |
The statistical description indicates that means of first and second parameters (Esthetics subjective assessment and Esthetics Objective assessment) with values of 1.67 and 1.40 for the Group B patients were close to the highly satisfactory value (value of 2) as compared to the respective values of 0.67 and 0.00 for the same parameters for Group A patients. The values for the third and fourth parameters (Oral soft tissue tolerance; subjective and objective assessment) were nearly the same for both the groups with Group A having values of 0.13 and 0.00 respectively and Group B having values of 0.20 and 0.00 respectively. The consistent values of 0.00 for fifth and sixth parameters (gingival and periodontal health) for both the Groups indicate clinically normal supportive tissues in all the thirty patients. The adaptability in areas with undercuts i.e. parameter seven had comparable values for both the groups (Group A had a value of 0.73, Group B had a value of 0.80) which are close to the value of 1 thus indicating that the undercuts had to be blocked out during the laboratory processing for both the types of prosthesis. Parameter eight (frequency of fracture) for both the groups, recorded nearly similar values with the incidence being slightly higher for Group A (Group A having a mean of 0.80 while Group B having a mean of 0.67). Parameter nine i.e. overall patient satisfaction shows that it is clearly higher for Group B patients with the value being 1.77 as compared to the value of 1.47 for Group A patients. The narrow ranges of standard deviation indicated that the values for each parameter for the two groups were more or less consistent and the range did not show much variance.
Discussion
The Results clearly show esthetic superiority of the Flexible RPDs over the Cast RPDs. This is because the Nylon based super polyamide resin has the translucency required to pick up the underlying tissue shade very effectively (Fig. 4). Unlike the cast RPDs, clasps are not used on the surfaces of teeth in the flexible RPDs and even when employed around the gingival tissue, the clasps were thin, translucent and appeared natural. Moreover, there were no changes in the appearance of the prostheses over the period of this study. This was in contrast to the unsightly metal clasps of the cast RPDs as well as the opaque pink look of the heat cured PMMA used to replace missing tissues.
Fig. 4.

Translucent valplast prosthesis.
During the observation period for this research study, the Valplast RPDs displayed a biocompatibility similar to that of the cast RPDs. Just like the cast RPDs, the flexible partials also do not engage the abutment teeth alone for support and retention hence the relative stresses on the abutment teeth are relieved. Retention here depends primarily on the tissue and only a small portion of abutment tooth. Also the ends of the Valplast partial move independently so that stress at one end of the prosthesis does not produce a counter-movement at the opposite end. A portion of the masticatory stress is also absorbed by the base material itself.
Clinical parameter of frequency of fracture of the prosthesis during usage had more or less similar values for both the groups with the incidence being slightly higher for Group A patients. This can be attributed to the brittle and stiffer nature of the Chromium Cobalt alloy owing to its low density and high elastic modulus as compared to the flexure modulus of 470 Mpa at body temperature of the super polyamide making it a virtually unbreakable material. The clinical parameter of overall patient satisfaction also showed favorable results for patients of Group B as compared to those of Group A. This difference was clearly influenced by the difference in appearance of the two prostheses and also with the softer, comfortable feel of the flexible RPDs as compared to the hard and rigid feel of the cast RPDs. Owing to its good dimensional stability, elastic memory and volumetric stability in moist environments the flexible RPDs maintain a relaxed position while fitting comfortably in the patient's mouth.
During this study it was observed that the fabrication of cast RPDs involves elaborate, time consuming mouth preparation procedures which includes precise preparation of guide planes, rest seats, re-contouring of abutment to relocate the survey lines and modification of undercuts. Impression making procedures for the cast RPDs were also more elaborate as compared to that for the flexible RPDs. Laboratory steps followed for fabrication of the cast Cr–Co alloy RPDs too were more elaborate, technique sensitive and time consuming.
Conclusion
Based on the assessment of these prostheses, of the nine stated clinical parameters, over an 18 months period and within the constraints of this study, it can be concluded that:
-
i
Removable partial dentures made of Nylon based Super polyamide can be considered as a viable option in the restoration of unilateral distal extension partial edentulism.
-
ii.
Removable partial dentures made of the newly introduced super polyamide resin can also be selected for patients who have high esthetic concerns but are reluctant to go in for invasive procedures required for the definitive cast Cr–Co alloy RPD or Fixed prosthesis.
-
iii.
Super polyamide resin can be also be the material of choice for making appliances for patients with compromised neuro-motor function or for individuals involved in high physical activity as in the case of armed forces personal indulging in contact sports.
However, further long term in vivo and in vitro studies are required to confirm the promising clinical behavior of this resin not only in Removable Prosthodontics but also in the other specialties of Dentistry as in Orthodontics, Oral and Maxillofacial Surgery, Periodontics, Pedodontics when used for fabricating different types of dental appliances like orthodontic retainers, temporomandibular splints, gum veneers, space maintainers etc.
Conflicts of interest
All authors have none to declare.
References
- 1.Tyson K., Robert Y., Scott B. Oxford University Press Inc; New York: 2008. Understanding Partial Denture Design. 11–12. [Google Scholar]
- 2.Lanier R.B., Kenneth D.R., Robert J., Strunk R. Making chromium cobalt removable partial dentures, a modified technique. J Prosthet Dent. 1971;25:197–205. doi: 10.1016/0022-3913(71)90108-9. [DOI] [PubMed] [Google Scholar]
- 3.Kratochvil F.J. Influence of occlusal rest position and clasp design on movement of abutment teeth. J Prosthet Dent. 1963;13:114–123. [Google Scholar]
- 4.Krol A.J. Clasp design for extension-base removable partial dentures. J Prosthet Dent. 1973;29:408–415. doi: 10.1016/s0022-3913(73)80018-6. [DOI] [PubMed] [Google Scholar]
- 5.Ben Ur Z., Aviv I., Cardash H.S. A modified direct retainer design for distal extension removable partial dentures. J Prosthet Dent. 1998;60:342–344. doi: 10.1016/0022-3913(88)90280-6. [DOI] [PubMed] [Google Scholar]
- 6.Eliason C.M. RPA clasp design for distal extension removable dentures. J Prosthet Dent. 1983;49:25–27. doi: 10.1016/0022-3913(83)90232-9. [DOI] [PubMed] [Google Scholar]
- 7.Goodman J.J., Goodman H.W. Balance of force in precision free-end restorations. J Prosthet Dent. 1963;13:302–308. [Google Scholar]
- 8.Brudvik J.S. 1st ed. Quintessence Books; Illinios: 1999. Advanced Removable Partial Dentures. 27–28. [Google Scholar]


