Abstract
The dermoid cyst is an uncommon clinicopathological lesion of developmental origin. The term dermoid cyst is used to describe 3 cysts that are closely related histologically: dermoid cyst, epidermoid cyst, and teratoma. Epidermoid and dermoid cysts are benign nature, which may occur anywhere in the body, but most predominantly in the ovary and scrotal regions. Only about 7% are found in the head and neck. The occurrence of such cysts in the oral cavity is extremely rare, with approximately 1.6% located in this area. The floor of the mouth is one of the most commonly affected area, however, these cysts can also be found in the tongue, lips, buccal mucosa and jaw bones.
There is always a difficulty of making a correct diagnosis of these lesions with clinical examinations and conventional radiography. To achieve a diagnosis and to develop correct surgical strategy specialized imaging examinations such as ultrasonography (US), computed tomography (CT), Magnetic Resonance Imaging (MRI) and histopathological examination should be carried out.
Treatment comprises total surgical excision the approach remains dictated logically by the cyst's location. Ample understanding and vigilance about this slow growing painless mass is essential not only because of the symptoms it produces but also due to its malignant potential. When dermoid cysts occur on the floor of the mouth, they may enlarge to such an extent that they can interfere with deglutition and produce respiratory obstruction. Early diagnosis and treatment are essential for these cystic entities.
Keywords: Dermoid cyst, Epidermal inclusion cyst, Teratoid cyst
Introduction
The dermoid cyst is an uncommon clinicopathological lesion of developmental origin which describes three histologically closely related lesions: dermoid cyst, epidermoid cyst and teratoma. Epidermoid and dermoid cysts are benign nature, which may occur anywhere in the body, but most predominantly in the ovary and scrotal regions.1 Only about 7% are found in the head and neck region. The floor of the mouth is the second most common site in the head and neck region after the lateral eyebrow as these are the sites of embryonic fusion. The occurrence in oral cavity is approximately 1.6%. The floor of the mouth is one of the most commonly affected areas, however, these cysts can also be found in the tongue, lips, buccal mucosa and jaw bones.2, 3
Dermoid cysts are derived from epithelial rests that are included during midline union of the first and second branchial arches. The vast majority of dermoid cysts of the floor of mouth (DCFOM) are located in the midline (sublingual 52%, submental 26%), 16% involve more than 1 of the 3 possible spaces in the floor of the mouth region (submental, sublingual, submandibular), and only 6% are situated exclusively in the submandibular space where they appear to be lateral neck cysts.4
There is always a difficulty of making a correct diagnosis of these lesions with clinical examinations and conventional radiography. To achieve a diagnosis and to develop correct surgical strategy, specialised imaging examinations such as ultrasonography (US), computed tomography (CT), Magnetic Resonance Imaging (MRI) and histopathological examination should be carried out.5
We report and review the cases of dermoid cyst of head and neck region treated in our centre.
Case – 1, sublingual dermoid cyst
A 28-year-old male patient reported with a complaint of persistent swelling of the floor of the mouth and chin since two years. A painless swelling gradually increased in size and he had difficulty in speech since last 6 months. He was moderately built with no history of any systemic illness. He had undergone extraction of lower anterior teeth for the same complaint.
On maxillofacial examination there was an oval shaped swelling of about 6 × 3.5 cm in size in the submental area giving double chin appearance [Fig. 1]. The edges were indistinct, surface was smooth, soft in consistency, non tender and the overlying skin was normal. It was compressible, non-pulsatile, non reducible and was not fixed to the underlying structures. There was no lymphadenopathy. Oral examination revealed the floor of the mouth and tongue were elevated. The mass was bimanually palpable and on digital pressure over submental area the swelling protrudes into the oral cavity. The tongue movements were restricted. The oral mucosa and Wharthin's ducts were healthy.
Fig. 1.
Pre and post operative photographs.
All routine laboratory investigations were normal. Computed tomography revealed a well encapsulated unilocular cystic lesion of 6 cm × 4 cm in size in the midline in the sublingual region above the mylohyoid muscle [Fig. 2]. Aspiration biopsy revealed white granular cheesy material. The histopathological examination confirmed the presence of keratin and sebum like aspirate suggestive of a dermoid cyst. Pre anaesthetic protocol was completed.
Fig. 2.
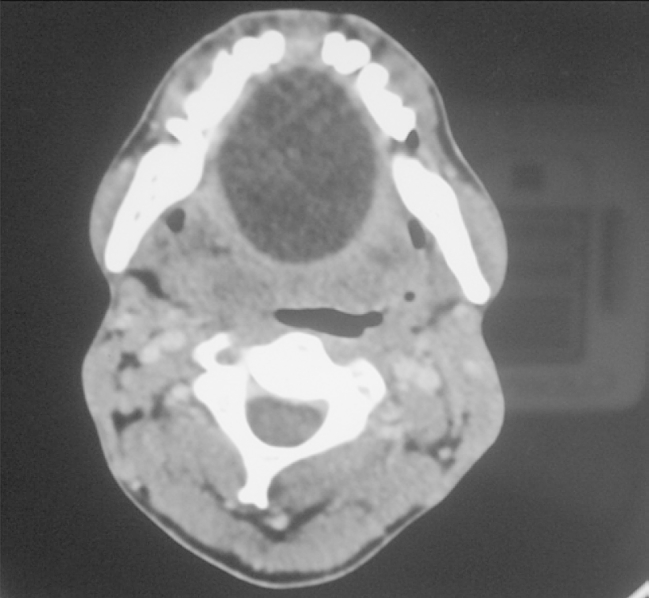
Axial scan showing the lesion.
Surgical excision was planned under general anaesthesia (GA). The incision was placed in lingual vestibule parallel to the Wharton's duct and the lesion was exposed. It was decompressed by aspirating some of the cystic content to avoid rupture. Blunt dissection was carried out and the lesion enucleated. Surgical wound closed in layers. The postoperative healing was uneventful [Fig. 1].
Histopathological examination depicted stratified squamous epithelial lining with keratin filaments and sebaceous glands confirming the diagnosis of dermoid cyst.
Case – 2, recurrent epidermal inclusion cyst
A 72-year-old male patient reported with a chief complaint of pain, swelling and pus discharge since one month from the left lower jaw. Past medical history was nil relevant with no significant family history. He had undergone multiple teeth extractions in past 6 months. Maxillofacial examination revealed an indurated swelling of approximately 3 × 4 cm in size extending from the mid symphyseal region to the commissure of the left side [Fig. 3]. Overlying skin was inflamed and adherent and two draining sinuses were present with purulent discharge. On palpation the swelling was tender. Submental lymph nodes were enlarged and tender.
Fig. 3.
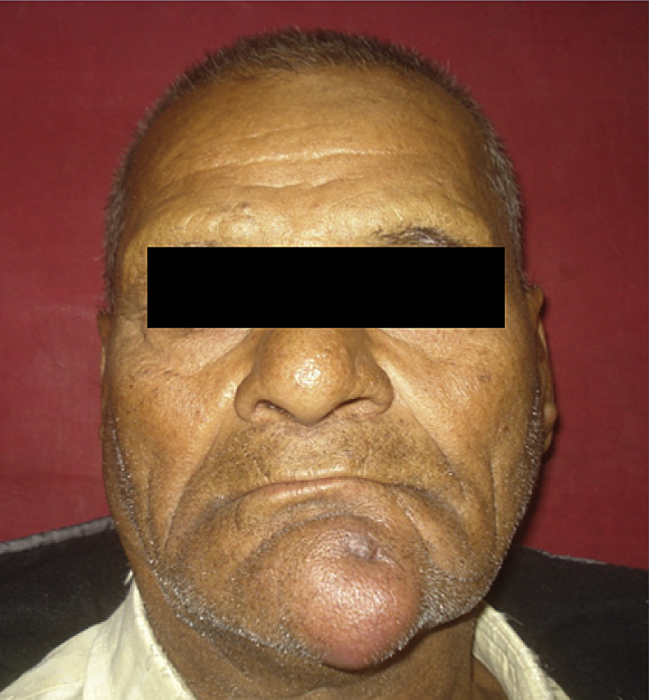
Preoperative photograph.
Mouth opening was 35 mm. The patient was completely edentulous with obliteration of lower labial vestibule. Clinical impression was that of a submental space infection with discharging sinuses. The differential diagnosis included osteomyelitis, secondarily infected dermoid and an infected submental lymph node. Radiographs revealed no bony abnormality.
The discharge was sent for culture, antibiotic sensitivity test (ABST) and histopathological analysis. There was polymicrobial growth sensitive to penicillin, cephalosporin, aminoglycosides and imipenem. Hispathological examination revealed keratin, sebum and heavy infiltration of polymorphonuclear leucocytes suggestive of an infected dermoid cyst.
The lesion was excised under GA and primary closure was achieved. Histopathological examination of the specimen showed the lining as a stratified squamous epithelium with keratin filaments [Fig. 4]. Diagnosis of epidermal inclusion cyst was confirmed.
Fig. 4.
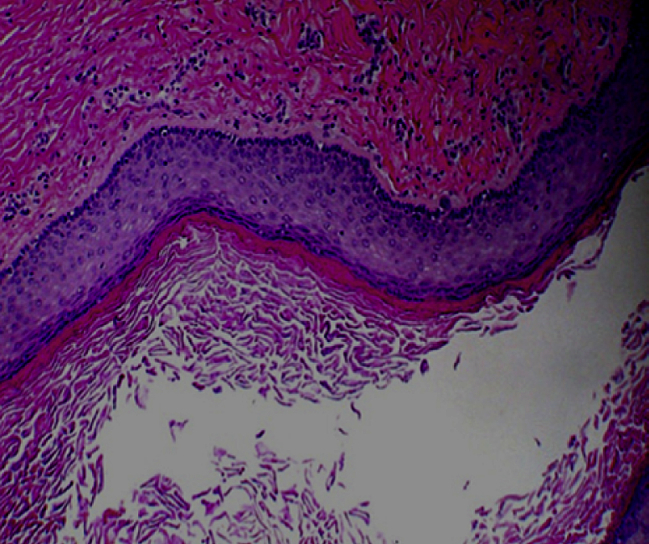
Micro photograph (403) showing stratified squamous epithelial lining with keratin filaments.
Patient reported back after six months with recurrence. Wide local excision was done under general anaesthesia. A full thickness rotational flap was used to reconstruct the defect [Fig. 5]. The healing was uneventful. Patient is under review since last 1 year without any recurrence.
Fig. 5.

Rotational flap for reconstruction.
Case – 3, teratoid cyst
A twenty-one-year-old male patient was referred to Department of Oral and Maxillofacial Surgery with a chief complaint of recurrent swelling on the right malar region since last 2 years. He was previously treated by incision and drainage two times and the swelling recurred 4–5 months after each surgery.
On clinical examination a diffuse, doughy soft and non tender swelling was present on the right zygomatic area. A linear scar on the centre of swelling was evident [Fig. 6]. On intraoral examination of the zygomaticomaxillary buttress region there was a smooth bony projection extending posterior and inferiorly partially obliterating the vestibule, was palpable.
Fig. 6.

Swelling at the right malar region with scarring.
The 3 dimensional CT revealed a bony projection from the body of right zygoma hanging on to the vestibule [Fig. 7]. Coronal view revealed a well demarcated radiolucent cystic mass in the body of zygoma extending as a bony projection and partially obliterating the maxillary antrum. There was no antral breach. Fine needle aspiration biopsy revealed keratin and sebum like white granular material suggestive of dermoid cyst.
Fig. 7.
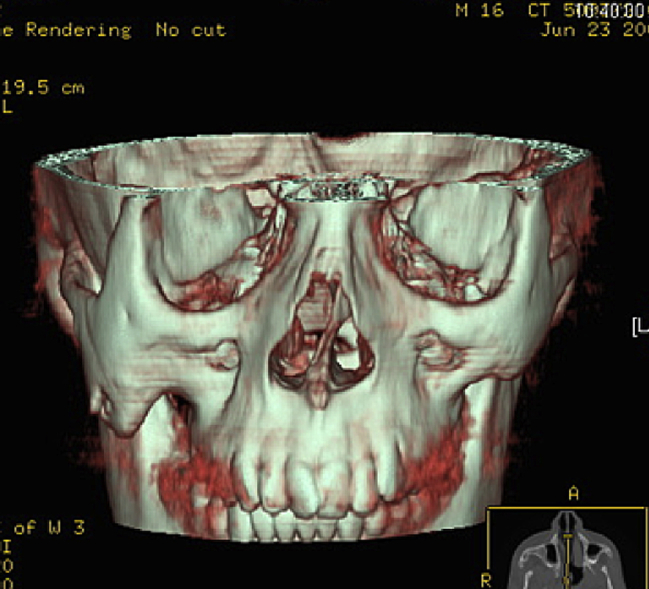
3D CT scan depicting bony projection from right zygoma.
The lesion was exposed by Weber-Furguson approach under general anaesthesia. The bony extension of the lesion was delineated with osteotome. The lesion was enucleated in toto. It contained hair strands and cheesy granular material [Fig. 8].
Fig. 8.
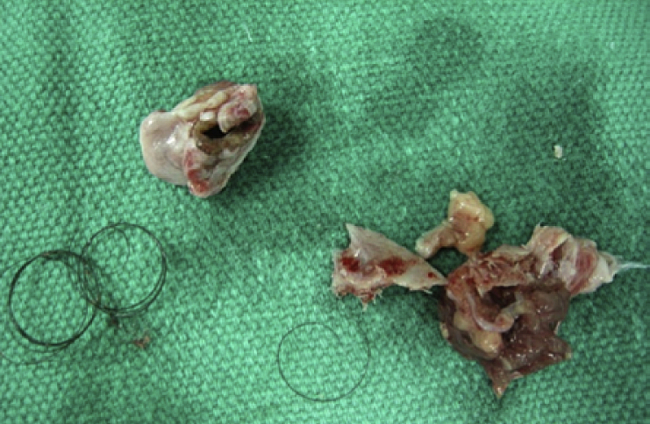
Specimen with hair strands.
Histopathologic examination showed the lesion as a benign teratoma with tridermal derivatives predominantly consisting of well-differentiated embryonic components, including bone, cartilage, fibrous tissue, focal calcification, nerve tissues and hair follicles [Fig. 9]. Postoperative healing was uneventful without any recurrence during 2 years follow up.
Fig. 9.
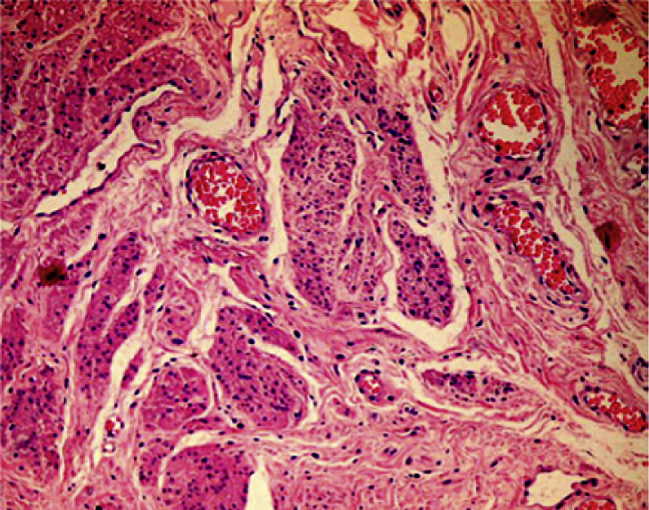
Micro photograph (403) showing tridermal derivatives.
Discussion
The generic term “dermoid cyst” or “dermoid” was used to describe 3 histological varieties, (a) Epidermoid cyst: lined with simple squamous epithelium with a fibrous wall and no adnexal structures (b) True dermoid cyst: an epithelial-lined cavity with keratinization and with skin appendages (sebaceous and sweat glands and hair follicles in the cyst wall). This is also known as a compound cyst and (c) Teratoid cyst: lined with a range of epithelia, from simple squamous to ciliated epithelium, containing derivatives of ectoderm, mesoderm and endoderm. This is also known as a complex cyst. All three types may contain a cheesy keratinous material.6
Dermoid cysts of the floor of the mouth are an uncommon entity, hence rarely considered in the differential diagnosis (Table 1). They usually manifest during the second or third decade of life as yellowish masses in the midline of floor of mouth or submental area. Dysontogenetic, traumatic and thyroglossal anomaly theories have been postulated for pathogenesis.7 Most congenital dermoid and epidermoid cysts perhaps begin due to an embryologic accident during the early stages of development but hardly noticed until their size causes annoyance.8 The origin of epidermoid cysts is believed to be from entrapment of epithelial remnants during midline closure of the bilateral first and second branchial arches.7, 9 It has also been opined that ectodermal differentiation of multipotential cells, most probably pinched off at the point of anterior neuropore closure may give rise to these cysts.7 They may also crop up from the tuberculum impar of His.10
Table 1.
Differential diagnosis of dermoid cyst of the floor of the mouth.
| Mucus extravasation phenomena |
| Mucocele |
| Plunging (cervical) ranula |
| Embryologic anomalies |
| Thyroglossal duct cyst |
| Branchial cleft cyst |
| Dermoid cyst |
| Cystic hygroma |
| Infection |
| Acute bacterial infection/cellulitis of oral floor |
| Sialadentitis of sublingual or submandibular gland |
| Viral lymphadenitis (EBV, CMV) |
| Granulomatous disease |
| Infectious |
| Mycobacterial disease |
| Cat-scratch disease |
| Actinomycosis |
| Toxoplasmosis |
| Tularaemia |
| Histoplasmosis |
| Blastomycosis |
| Noninfectious |
| Sarcoidosis |
| Wegener's granulomatosis |
| Langerhans' cell histiocytosis |
| Crohn's disease |
| Non-granulomatous inflammatory disease |
| Kawasaki's disease |
| Tumour |
| Benign tumours of salivary glands |
| Lipoma |
| Fibroma |
| Haemangioma |
| Lymphangioma |
| Angioma |
| Neurofibroma |
| Malignant tumours of salivary glands* |
| Lymphoma |
| Rhabdomyosarcoma |
| Neuroblastoma |
| Metastatic neoplasm |
| Other |
| Normal fat in the submental or submandibular area |
| HIV-related lymphadenopathy |
| Pneumocystis lymphadenitis |
| Persistent generalized lymphadenopathy |
| Nocardiosis |
| Non-Hodgkin’s lymphoma |
| Metastatic Kaposi's sarcoma |
Although floor of the mouth in the midline is most favoured site, occasional occurrence involving the buccal mucosa, tongue, lips, uvula, temporomandibular joint dermal graft, intradiploic, intracranial and intraosseous location within the mandible and maxilla also have been cited in literature.11 Depending upon the anatomical location DCFOM are classified as supramylohyoid (intraoral or sublingual), inframylohyoid (cervical), peri- and trans-mylohyoid (both intraoral and cervical).12
Symptoms of dysphagia, dyspnoea and dysphonia may occur due to upward displacement of tongue by this sublingual swellings.10 Growth in an inferior direction may give rise to appearance of characteristic “double chin”.7, 10 These well encapsulated lesions typically feel “dough like” on palpation. The first case had these clinical features.
Fine needle aspiration cytology, ultrasound, CT and MRI provide essential information on the cyst location that allows optimal preoperative planning. Ultrasonographic findings comprise solid and cystic structures within a heterogeneous mass.3 On CT scans, the dermoid cyst appear as moderately thin walled, unilocular masses filled with a homogeneous, hypoattenuating fluid substance with numerous hypoattenuating fat nodules giving the pathognomonic “sack-of-marbles” appearance.8 MRI of dermoid cysts give variable signal intensity on T1-weighted images and are usually hyperintense on T2-weighted images and are of considerable importance in depicting the relationship of cystic mass and muscles of floor of the mouth.
Treatment comprises surgical excision. The lesions can be exposed by intraoral or extraoral approach depending upon its location in relation to mylohyoid muscle. Lateral DCFOMs of the submandibular or sublingual space and are most conveniently excised via submandibular approach.12 Large lesions may require both intraoral and extraoral incisions to provide direct visualization. We aspirated the cystic contents to avoid rapture. Recurrences are unusual after total surgical excision.7, 8
Histopathologically, an epidermoid cyst consists of squamous epithelium with a fibrous wall, whereas a dermoid cyst has, in addition, a varying number of skin appendages such as hair follicles and sebaceous glands. Reports of malignant transformation of sublingual dermoid and epidermoid cyst have been reported.7 5% rate of malignant transformation of the teratoid variety of oral dermoid cysts has also been reported in literature.8 In our cases though the lesions were long standing, there was no evidence of malignant transformation.
Epidermal inclusion cyst has been referred by various terms including sebaceous cyst, epidermal cyst, seborrhoeic cyst and epidermoid cyst. They may form by implantation of epidermal rests during embryonal period, occlusion of pilosebaceous units or surgical implantation of epithelium in to the jaw mesenchyme resulting in proliferation of epidermal cells within dermis. The source of this epidermis is often from the infundibulum of hair follicle.13 Human papilloma virus type 57 or 60 may be additional factors in development of palmo-plantar epidermoid cyst.14 Epidermal inclusion cyst lacks ectodermal appendages. Clinically they present as a firm and slow growing asymptomatic lump underneath the skin. One of the cases presented here had a fixed, indurated and painful swelling associated with extraoral draining sinuses. Due to infection the margins of the lesion were not well delineated. Surgical excision is a treatment of choice; however recurrences are frequent if keratin producing lining of the cyst is not removed. The recurrence in one of our cases might be due to incomplete removal of the lining.
Occurrence of teratomas in head and neck area is one in every 20,000 to 40,000 live births and 90% of head and neck teratomas present during the neonatal and infantile period.15 In this clinical report, we presented a case of teratoma of the zygomatic bone in an adult patient which is a rare entity.
Teratomas have heterogeneous histologic characteristics. Mature teratomas may contain all manners of adult tissues with varying degrees of organoid development, whereas immature lesions may produce embryonic or extra embryonic foetal tissue. Neural tissue is commonly found in a disproportionate number of benign teratomas (68%), predominating the solid portion of these tumours.16 Although most teratomas are benign, the rate of malignant degeneration increases in cases not diagnosed or treated until adolescence.17
Plain radiographs may show calcifications or the presence of teeth in the mass. In the present case plain radiograph was not much of help as it was within the body of zygomatic bone. Computed tomography is a very useful tool. It also can help in differentiating oral maxillofacial teratomas from encephaloceles, which often display erosion of the bone or skull base.17
Surgical excision is the treatment of choice. Our patient had recurrence two times following incision and drainage. Recurrence of teratoma is attributed to incomplete excision.18 Local drainage procedures can implant cyst epithelium along the drainage tract, thereby increasing the likelihood of recurrence. The patient is under review since last 3 years without any recurrence.
Conclusion
Dermoid cysts are malformations lined by epidermis like epithelium, which contains dermal adnexal structures in the cyst wall. They are derived from epithelial rests that are included during midline union of the first and second branchial arches. Dermoid cysts found on the floor of the mouth are rare. Ample understanding and vigilance about this slow growing painless mass is essential not only because of the symptoms it produces but also due to its malignant potential. When dermoid cysts occur on the floor of the mouth, they may enlarge to such an extent that they can interfere with deglutition and produce respiratory obstruction. Early diagnosis and treatment are essential for these cystic entities.
Conflicts of interest
All authors have none to declare.
References
- 1.De Ponte F.S., Brunelli A., Marchetti E., Bottini D.J. Sublingual epidermoid cyst. J Craniofac Surg. 2002;13:308–310. doi: 10.1097/00001665-200203000-00024. [DOI] [PubMed] [Google Scholar]
- 2.Fuchshuber S., Grevers G., Issing W.J. Dermoid cyst of the floor of the mouth – a case report. Eur Arch Otorhinolaryngol. 2002;259:60–62. doi: 10.1007/s004050100413. [DOI] [PubMed] [Google Scholar]
- 3.Bataineh A.B., Mansour M.J. Extraoral epidermoid cysts. Br J Oral Maxillofac Surg. 1997;35:49–51. doi: 10.1016/s0266-4356(97)90010-3. [DOI] [PubMed] [Google Scholar]
- 4.King R.C., Smith B.R., Burk J.L. Dermoid cyst in the floor of the mouth. Review of the literature and case reports. Oral Surg Oral Med Oral Pathol. 1994;78:567. doi: 10.1016/0030-4220(94)90166-x. [DOI] [PubMed] [Google Scholar]
- 5.Chikui T., Shimizu M., Goto T.K. Interpretation of the origin of a submandibular mass by CT and MRI imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:721–729. doi: 10.1016/j.tripleo.2004.02.054. [DOI] [PubMed] [Google Scholar]
- 6.Meyer I. Dermoid cysts of the floor of the mouth. Oral Surg Oral Med Oral Pathol. 1955;8:1149. doi: 10.1016/0030-4220(55)90380-7. [DOI] [PubMed] [Google Scholar]
- 7.Koca H., Seckin T., Sipahi A., Kaznac A. Epidermoid cyst in the floor of the mouth: report of a case. Quintessence Int. 2007;38:473–477. [PubMed] [Google Scholar]
- 8.Pancholi A., Raniga S., Vohra P.A., Vaidya V. Midline submental epidermoid cyst: a rare case. Int J Otorhinolaryngol. 2006;4(2):74–77. [Google Scholar]
- 9.Hemaraju N., Nanda S.K., Mediker S.B. Sublingual dermoid cyst. Indian J Otolaryngol Head Neck Surg. 2004;3:218–220. doi: 10.1007/BF02974355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kandogan T., Koc M., Vardar E., Selek E., Sezgin O. Sublingual epidermoid cyst: a case report. J Med Case Reports. 2007;1:87. doi: 10.1186/1752-1947-1-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shear M., Speight P. Cysts of Oral and Maxillofacial Region. 4th ed. Blackwell Munksgaard; Singapore: 2007. From developmental cysts of head and neck; pp. 181–183. [Google Scholar]
- 12.Teszler Christian B., El-Naaj Imad Abu, Emodi Omri, Lunt Michal, Peled Micha. Dermoid cysts of the lateral floor of the mouth: a comprehensive anatomo-surgical classification of cysts of the oral floor. J Oral Maxillofac Surg. 2007;65:327–332. doi: 10.1016/j.joms.2005.06.022. [DOI] [PubMed] [Google Scholar]
- 13.Cotran R.S., Kumar V., Robbins S.L. 5th ed. WB Saunders; Philadelphia: 1994. Pathologic Basis of Disease; pp. 1182–1183. [Google Scholar]
- 14.Lee S., Lee W., Chung S. Detection of human papilloma virus 60 in epidermal cyst of non palmoplantar location. Am J Dermatopathol. Jun 2003;25(3):243–247. doi: 10.1097/00000372-200306000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Azizkhan R.G., Haase G.M., Applebaum H. Diagnosis, management, and outcome of cervicofacial teratomas in neonates: a Children’s Cancer Group Study. J Pediatr Surg. 1995;30:312–316. doi: 10.1016/0022-3468(95)90580-4. [DOI] [PubMed] [Google Scholar]
- 16.Jordan R.B., Gauderer M.W. Cervical teratomas: an analysis. Literature review and proposed classification. J Pediatr Surg. 1988;23:583–591. doi: 10.1016/s0022-3468(88)80373-7. [DOI] [PubMed] [Google Scholar]
- 17.Batsakis J.G., el-Naggar A.K., Luna M.A. Teratomas of the head and neck with emphasis on malignancy. Ann Otol Rhinol Laryngol. 1995;104:496–500. doi: 10.1177/000348949510400616. [DOI] [PubMed] [Google Scholar]
- 18.Modolo F., de Melo Alves S., Jr., de Almeida Milani B. Congenital teratoid cyst of the floor of the mouth. Otolaryngol Head Neck Surg. 2007;136:134. doi: 10.1016/j.otohns.2006.03.021. [DOI] [PubMed] [Google Scholar]



