Introduction
Chronic abdominal pain can have a myriad of causes. A mesenteric cyst is an infrequent cause for this condition. It commonly originates from the small bowel mesentery although a proportion of them have been found to originate from the mesocolon (24%) and the retroperitoneum (14.5%).1
As such, mesocolic cysts are very uncommon and usually arise from the right side. A mesenteric cyst originating in the sigmoid mesocolon is a rare finding. To the best of our knowledge, only 4 cases have been reported so far.2, 3, 4, 5 Surgery is the cornerstone of management for a mesenteric cyst but surgery for a sigmoid mesenteric cyst can be complicated due to its close relation with the iliac vessels and ureter apart from the bowel wall. With the advent of minimally invasive surgery, laparoscopic management of mesenteric cyst is known from 1993 though no large series have been reported so far.6 Further, a laparoscopic management of a sigmoid mesenteric cyst is only recently being reported.4, 5
We, in this report, describe two cases of this rare entity that were successfully managed by a laparoscopic excision and share our experience.
Case report
Case 1
A 48 year old female patient presented with 2-month's history of pain and lump in her left lower abdomen. She had no other symptoms referable to bowel or bladder. Her abdominal examination revealed a firm, non-tender, mobile lump in the left lower quadrant of abdomen. Clinically, a diagnosis of ovarian cyst was entertained with a mesenteric, omental or a hydatid cyst being the other possibilities. A contrast enhanced CT scan was done which showed a 15 × 10 cm unilocular cystic lesion with thin wall, in the retroperitoneum displacing and compressing the sigmoid colon with the ureter and iliac vessels draping its posterior wall (Fig. 1). Both the ovary and uterus were normal. A diagnostic laparoscopy was planned which showed a thin walled cystic lesion in the sigmoid mesentery in close relationship with the left ureter and iliac vessels (Fig. 2). A laparoscopic total excision of the cyst was done safeguarding the ureter, iliac vessels and sigmoid colon. The cyst was then transferred into an endobag, a controlled aspiration was done ensuring no spillage and then delivered through one of the ports.
Fig. 1.

Axial section on a contrast enhanced CT scan showing a 15 × 10 cm thin-walled cystic lesion (C) compressing the sigmoid colon (white arrow head) and in close relation to iliac vessels (black arrow head).
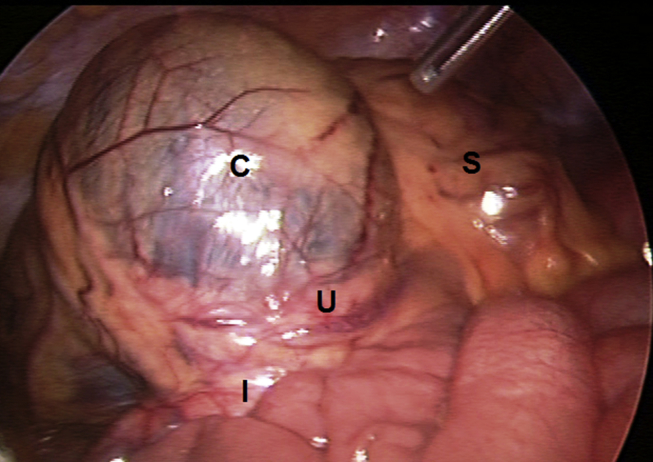
Fig. 2.
Intraoperative photograph showing the Cyst (C) in the sigmoid mesocolon, in close relation to the iliac vessels (I) and left ureter (U). S Sigmoid colon.
Case 2
A 55 year old female patient, who had been previously treated for spinal tuberculosis, was admitted with vague lower abdominal pain for the last 3 months. There were no other symptoms and there were no findings on abdominal examination. An ultrasound of abdomen was ordered which picked up an 8 × 6 cm cystic lesion at the bifurcation of aorta which on CT scan was seen as a thin walled unilocular cyst, adjacent to the sigmoid colon in the retroperitoneum with normal ovaries. With a provisional diagnosis of mesenteric cyst, the patient was taken up for a diagnostic laparoscopy. This revealed a cystic lesion in sigmoid mesentery and was excised in total. Towards the end of procedure, the cyst ruptured accidentally leaking straw colored fluid. Control was taken of the cyst wall opening, the cyst sucked out completely of its content and delivered.
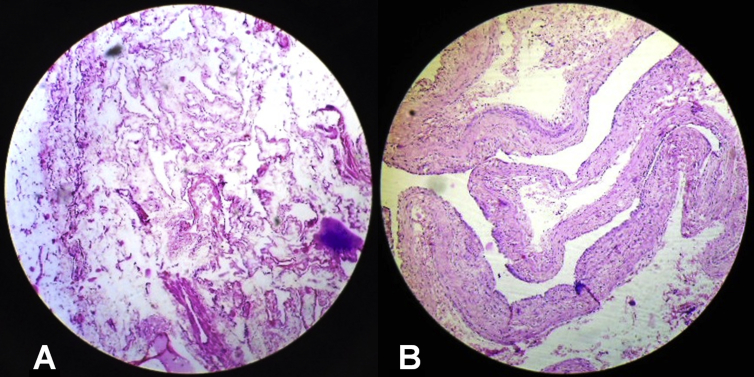
Both the patients had an uneventful recovery and were discharged on the 2nd post-operative day. The histopathology of the cysts in both the cases was reported as lymphatic cyst (Fig. 3).
Fig. 3.
A & B Photomicrographs of the two cases showing flattened endothelial lining with fibrocollagenous tissue.
Discussion
Mesenteric cysts were first described by Bless et al,7 way back in 1507, though its surgery was only first reported in 1880 by Tillaux et al.8 Its incidence is said to vary from 1 per 100,000 to 250,000 admissions.9 The location of mesenteric cyst is variable and can be found anywhere – from the duodenum to the rectum. A mesenteric cyst in the sigmoid mesocolon is a rare occurrence.
These cysts are usually a result of developmental anomalies and their origin lends to their classification. Beahrs et al10 first classified mesenteric cysts in to embryonic/developmental, traumatic, neoplastic and infective/degenerative cysts. A more accepted and recent classification is the one given by Ross et al,11 a histological classification, correlated with the radiological findings: Lymphangiomas, enteric duplication, enteric cysts, mesothelial cysts and non-pancreatic pseudocysts.
Those presenting in childhood have a male preponderance whereas the majority present later usually in the fifth decade with a female preponderance.12 This was seen in our cases too. These cysts can be of variable size, from a few centimeters to large masses almost occupying the whole abdomen. Most of these cysts are asymptomatic, only being picked up on imaging though sometimes they present with vague abdominal pain or as a lump. The pain may be due to the stretching of the mesentery or due to one of the complications, namely, torsion, rupture, infection, hemorrhage or intestinal obstruction. A malignant transformation is rare but has been described in up to 3% of the cases.1 Clinically, when palpable the cyst demonstrates a characteristic mobility perpendicular to the line of attachment of the small bowel mesentery (Tillaux sign) though the direction is more horizontal for a sigmoid mesenteric cyst as was in our case.
An ultrasound can pick up these cyst but a cross sectional imaging - CT scan or an MRI is needed to define its relationship/differentiating with the surrounding structures.13 This is more relevant with the cysts in sigmoid mesocolon with the ureter and iliac vessels at risk during surgery.
Surgery is the cornerstone of its management with failure of other modalities like marsupialization, percutaneous aspiration or lap deeroofing, which inevitably lead to recurrences.1 The enterogenous cyst share a common supply with the adjacent bowel and as such would need a concomitant resection of this segment of bowel. In all other cases, the cysts can be excised/enucleated due to its independent blood supply. Mackenzie et al in 1993, reported the first laparoscopic excision of a mesenteric cyst.6 Since then many cases have been reported but no large series exists to make definite recommendation. The largest series has been by Shamiyeh et al; 3 cases of which 2 were excised and 1 underwent deroofing only to recur 10 months later.14 Laparoscopic excision of mesenteric cyst offers the advantage of reduced physiological trauma, decreased pain, early discharge to home and better cosmesis with same results as in open resection. This offsets the longer operative time taken in laparoscopic surgery. A laparoscopic resection for mesenteric cysts in sigmoid mesocolon has only recently been attempted.4, 5
We could accomplish a laparoscopic excision of the cyst with the use of three ports – a 10-mm camera port lateral to right rectus muscle border just above the umbilicus and two 5-mm working ports, supra-umbilical and right lower quadrant. The patient needs to be placed in steep trendelenburg position with left side elevated. The cyst has to be handled carefully due to its thin wall which could easily get punctured during its dissection leading to spillage which can be a problem if it is infected or the very rare occurrence of malignancy in it. A practical approach would be to transfer the completely excised cyst into an endobag and then aspirate it in a controlled fashion and then deliver the cyst in the endobag through one of the ports. Also, it is vital to be oriented to the anatomy at all the times, especially in large cysts as vital structures like the ureter and iliac vessels are draped on the posterior aspect of these cysts. Both our cases could be completed in less than an hour which, in our opinion, would not be more than what it would have taken to resect it via a laparotomy.
After an extensive literature search, we could identify only 4 previously reported cases of sigmoid mesenteric cysts (Table 1). The age ranged from 26 to 42 years and all were symptomatic. Our patients were older. Of the four cases, two underwent a laparotomy whereas two were laparoscopically resected with no reported morbidities.
Table 1.
Reported cases of mesenteric cysts in sigmoid mesocolon in literature.
| Sl no | Author | Year | Age/sex | Presentation | Management | Histopathology |
|---|---|---|---|---|---|---|
| 1 | Smith, et al. | 1995 | 29/F | Lump | Excision | Urogenital remnant of Mullerian type |
| 2 | Iida, et al. | 2003 | 31/F | Pain abd | Excision | Pseudocyst |
| 3 | Wang JH, et al. | 2012 | 26/M | Pain abd | Lap excision | Duplication cyst |
| 4 | Bhandarwar AH, et al. | 2013 | 42/F | Pain abd | Lap excision | Lymphatic cyst |
| 5 | Our cases | 2014 | 48/F | Pain abd | Lap excision | Lymphatic cyst |
| 62/F | Pain abd/lump | Lap excision | Lymphatic cyst |
Abd: abdomen, Lap: laparoscopic.
Conclusion
Mesenteric cysts arising from sigmoid mesocolon are rare. The diagnosis is usually straightforward with the widespread availability of imaging modalities. These cysts lend themselves to laparoscopic management which can be accomplished without much morbidity.
Conflicts of interest
All authors have none to declare.
References
- 1.Kurtz R.J., Heimann T.M., Beck A.R. Mesenteric and retroperitoneal cysts. Ann Surg. 1986;203:109–112. doi: 10.1097/00000658-198601000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smith G.L., Thorpe P.A., Karimjee S., Dawson P.M. An abdominal cyst. Postgrad Med J. 1995;71:637–638. doi: 10.1136/pgmj.71.840.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iida T., Suenaga M., Takeuchi Y., Kobayashi T., Tobinaga J., Sakai M. Mesenteric pseudocyst of the Sigmoid Mesocolon. J Gastroenterol. 2003;38:1081–1085. doi: 10.1007/s00535-003-1200-1. [DOI] [PubMed] [Google Scholar]
- 4.Wang J.H., Lin J.T., Hsu C.W. Laparoscopic excision of mesenteric duplication enteric cyst embedded in sigmoid mesocolon mimicking retroperitoneal neurogenic tumor in adults. Surg Laparosc Endosc Percutan Tech. 2012;22:e294–e296. doi: 10.1097/SLE.0b013e3182611d07. [DOI] [PubMed] [Google Scholar]
- 5.Bhandarwar A.H., Tayade M.B., Borisa A.D., Kasat G.V. Laparoscopic excision of mesenteric cyst of sigmoid mesocolon. J Minim Access Surg. 2013 Jan-Mar;9(1):37–39. doi: 10.4103/0972-9941.107138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mackenzie D.J., Shapiro S.J., Gordon L.A. Laparoscopic excision of a mesenteric cyst. J Laparoendosc Surg. 1993;3:295–299. doi: 10.1089/lps.1993.3.295. [DOI] [PubMed] [Google Scholar]
- 7.Bless D.P., Coffin C., Bower R.S. Mesenteric cyst in children. Surgery. 1994;115:571–577. [PubMed] [Google Scholar]
- 8.Tillaux P., Millard P. Kyste de mésentere chez un homme. Bull Acad Méd. 1880;17:831. [Google Scholar]
- 9.Liew S.C., Glenn D.C., Storey D.W. Mesenteric cyst. Aust N Z J Surg. 1994 Nov;64(11):741–744. doi: 10.1111/j.1445-2197.1994.tb04530.x. [DOI] [PubMed] [Google Scholar]
- 10.Beahrs O.H., Judd E., Dockerty M.B. Chylous cysts of the abdomen. Surg Clin North Am. 1950;30:1081–1096. doi: 10.1016/s0039-6109(16)33090-0. [DOI] [PubMed] [Google Scholar]
- 11.Ross P.P., Olmsted W., Moser R.P. Mesenteric and omental cyst classification with imaging correlation. Radiology. 1987;164:327–332. doi: 10.1148/radiology.164.2.3299483. [DOI] [PubMed] [Google Scholar]
- 12.Dursun A.S., Gokhan A., Volkan S., Osman S., Cigdem T., Osman N.D. Laparoscopic enucleation of mesenteric cyst: a case report. Mt Sinai J Med. 2006;73:1019–1020. [PubMed] [Google Scholar]
- 13.Fujita N., Noda Y., Kobayashi G. Chylous cyst of the mesentery; US and CT diagnosis. Abdom Imaging. 1995;20:259. doi: 10.1007/BF00200410. [DOI] [PubMed] [Google Scholar]
- 14.Shamiyeh A., Rieger R. Role of laparoscopic surgery in the treatment of mesenteric cysts. Surg Endosc. 1999;13:937–939. doi: 10.1007/s004649901140. [DOI] [PubMed] [Google Scholar]