Introduction
Disseminated histoplasmosis can occur in immunosuppressed as well as immunocompetent individuals. It causes hemophagocytic lymphophagocytosis in the bone marrow. Histoplasma capsulatum is a dimorphic fungus that remains in a mycelial form at ambient temperatures and grows as yeast at body temperature and transmitted by inhalation of the spores.1 It enters the reticuloendothelial system and resides in macrophages. Most individuals with intact cellular immunity are asymptomatic. Approximately, 10% cases of histoplasmosis develop into progressive disseminated histoplasmosis.2 We report this case as in this case patient presented with pyrexia of unknown origin and there was evidence of hemophagocytosis in the bone marrow. The patient had recurrent erythema nodosum and subsequently liver and spleen biopsy clinched the diagnosis.
Case report
A 52 years male patient, a known case of chronic obstructive pulmonary disease for three years, Type II DM for 6 months, Recurrent erythema nodosum for 6 months, Acid peptic disorder and Polyarthralgia presented with skin rashes below knee for 6 months, fever for 2 weeks and black stool for 3 days. On examination there was pallor, Pedal edema, Hepatomegaly 5 cm below Rt subcostal margin, Splenomegaly – 8 cm below left subcostal margin. Hemoglobin was low (Range 6–7.3 gm/dl), total leucocyte count was 4200/cumm. CT scan of thorax and abdomen showed hepatosplenomegaly, retroperitoneal lymphadenopathy with mild ascites, solitary lesion in spleen. Colonoscopy showed normal study. He was planned for liver biopsy. Two units of packed red cells and six units of platelets were infused. Bone marrow aspirate and biopsy showed evidence of hemophagocytic lymphohistiocytosis. Serum ferritin was 306 ng/dl. He was treated with intravenous amphotericin-B at a dose of 0.9 mg/kg body weight He was receiving antibiotics and other symptomatic measures. Skin biopsy was done which was reported as erythema nodosum. The patient succumbed to his illness. Post mortem needle biopsy after proper consent was taken from liver, spleen, lungs and kidneys as the next of kin did not give consent for an autopsy. Core biopsy of the liver and spleen shows the tissue was densely infiltrated with chronic inflammatory cells including eosinophils. These included many histiocytes with a small number of lymphocytes and plasma cells, the histiocytes show cytoplasmic vacuoles and cells containing histoplasma capsulatum.
Discussion
Histoplasmosis is an endemic infection in most of the USA, Asia and Africa caused by infectious soil inhabited by bats and birds, as their excretions contaminate the soil. Disseminated histoplasmosis may present either as self-limited disease or progressive disseminated histoplasmosis. Progressive disseminated histoplasmosis of course can occur in immunocompetent patients at extremes of age and immunocompromised patients. Clinical presentations vary depending on the size of the inoculum, host's immune status and presence of underlying lung disease. Overt symptoms occur in only 5% of individuals after low-level exposure, but in 75% cases after heavy exposure in healthy hosts. Approximately 10% cases of histoplasmosis develop progressive disseminated histoplasmosis.3, 4 Most people have no symptoms, or only have a mild flu-like illness. If symptoms do occur, they may include fever, chills, sweating, cough, and chest pain, joint pains, mouth sores, red skin nodular lesions called erythema nodosum, most often on the lower legs. The infection may be active for a short period of time, and then the symptoms go away.5, 6 Sometimes, the lung infection may become long-term (chronic). Histoplasmosis may spread throughout the body, causing irritation and swelling (inflammation) in response to the infection. The acute syndrome can range from mild (lasting 1–5 d) to severe (lasting 10–21 d); the latter is associated with weight loss, fatigue, and night sweats. Fatigue may persist for weeks after the acute symptoms resolve. Patients may develop a variety of clinical manifestations including acute or subacute pulmonary disease, progressive disseminated disease, pericarditis, arthritis or, less commonly, fibrosing mediastinitis.7, 8, 9, 10 Hepatomegaly, splenomegaly, and bone marrow suppression may occur. Our patient presented with fever, fatigue, chronic obstructive pulmonary disease, recurrent erythema nodosum, acid peptic disorder polyarthralgia with skin rashes below knee and black stools. These symptoms along with anemia and hepatosplenomegaly well corroborated with the symptoms and signs in cases of disseminated histoplasmosis as reported in literature.11, 12 Histoplasmosis can be diagnosed by growth of histoplasma in culture, fungal stains (Bone marrow aspirate, peripheral blood smear, lymph node biopsy, bronchoalveolar lavage fluid, transbrochial biopsy specimen and biopsy from cutaneous lesions, serologic tests for antibodies, and antigen detection). Among all these, bone marrow examination has the highest diagnostic yield. Antigen detection in urine and serum by radioimmunoassay is useful in immunocompromised patient when antibody production may be impaired. It is highly sensitive in disseminated infection. Other laboratory abnormalities include anemia, leukopenia, pancytopenia, elevated liver enzymes, increased ferritin and serum lactate dehydrogenase. Our case was diagnosed as disseminated histoplasmosis on the basis of clinical presentation and histopathology of liver and spleen. Although culture was negative, histomorphological features were characteristic for diagnosis (Fig. 1, Fig. 2). The progressive disseminated histoplasmosis is reported to occur in one or two per 1000 patients of any age due to many predisposing factors. Fever, cough, weight loss, lymphadenopathy and hepatosplenomegaly are usual mode of presentation. But our case presented with fever, erythema nodosum and hemophagocytosis in bone marrow. Awareness of this infection is important because 100% mortality is seen in untreated group which comes down to 70% when adequately treated with Amphotericin-B5. Disseminated disease is to be differentiated from common diseases like tuberculosis, lymphoma or metastatic malignancy.
Fig. 1.
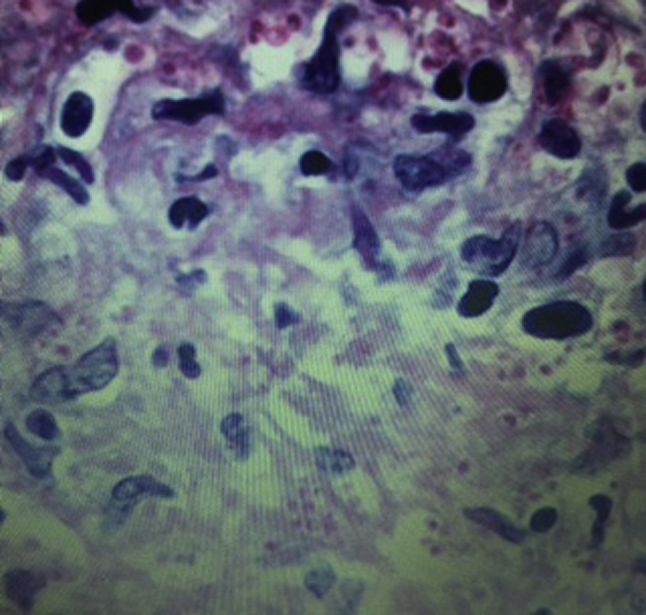
Shows microphotograph showing liver biopsy with PAS stain showing red colored yeast firm of histoplasmosis.
Fig. 2.
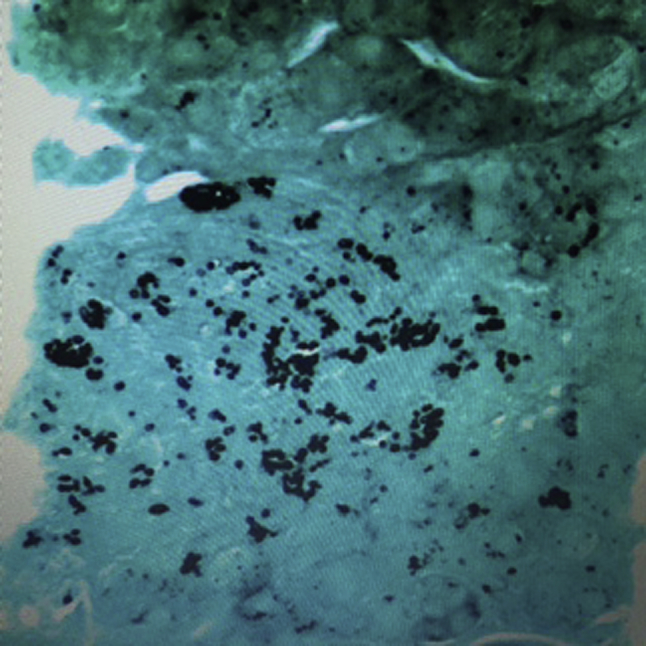
Shows microphotograph GMS stain showing black colored histoplasmosis in liver biopsy.
Conflicts of interest
All authors have none to declare
References
- 1.Deepe G.S., Jr. Histoplasma capsulatum. In: Mandell G.L., Bennett J.E., Dolin R., editors. Principles and Practice of Infectious Diseases. 7th ed. Elsevier Churchill Livingstone; Philadelphia, PA: 2009. chap 264. [Google Scholar]
- 2.Kauffman C.A. Histoplasmosis. In: Goldman L., Schafer A.I., editors. Cecil Medicine. 24th ed. Saunders Elsevier; Philadelphia, PA: 2011. chap 340. [Google Scholar]
- 3.Cano M.V., Hajjeh R.A. The epidemiology of histoplasmosis: a review. Semin Respir Infect. 2001;16(2):109–118. doi: 10.1053/srin.2001.24241. [DOI] [PubMed] [Google Scholar]
- 4.Islam N., Chowdhury N.A. Histoplasmosis from Bangladesh: a case report. Bangladesh Med Res Counc Bull. 1982;8(1):21–24. [PubMed] [Google Scholar]
- 5.Benenson A.S., editor. Control of Communicable Diseases Manual. 16th ed. American Public Health Association; Washington DC: 1995. pp. 237–240. [Google Scholar]
- 6.Subramanian S., Abraham O.C., Rupali P. Disseminated histoplasmosis. J Assoc Physicians India. 2005;53:185–189. [PubMed] [Google Scholar]
- 7.Rappo U., Beitler U.R., Faulhaber J.R. Expanding the horizons of histoplasmosis: disseminated histoplasmosis in a renal transplant patient after a trip to Bangladesh. Transpl Infect Dis. 2009:1–6. doi: 10.1111/j.1399-3062.2009.00466.x. [DOI] [PubMed] [Google Scholar]
- 8.Mahbub M.S., Ahsan M.N., Miah M.T. Disseminated histoplasmosis. J Med. 2010;11:70–73. [Google Scholar]
- 9.Rahman M.M., Hossain S.M., Faiz M.A., Rahman J., Sultan M.T., Dewanjee A.K. Disseminated histoplanmosis in AIDS. J BCPS. 2005;23:43–45. [Google Scholar]
- 10.Joshi S.A., Kagal As, Bharadwaj Rs. disseminated histoplasmosis. Indian J Med Microbiol. 2006;24:297–298. doi: 10.4103/0255-0857.29393. [DOI] [PubMed] [Google Scholar]
- 11.Wheat L.J., Conger N.G. Histoplasmosis. In: Hospenthal D.R., Rinaldi M.G., editors. Diagnosis and Treatment of Human Mycoses. Humana Press; New Jersey: 2008. pp. 318–329. [Google Scholar]
- 12.Doughan A. Disseminated histoplasmosis: case report and brief review. Travel Med Infect Dis. 2006;4:332–335. doi: 10.1016/j.tmaid.2006.01.013. [DOI] [PubMed] [Google Scholar]


