Abstract
Although vascular complications (VCs) following orthotopic liver transplantation (OLT) seldom occur, they are the most feared complications with a high incidence of both graft loss and mortality, as they compromise the blood flow of the transplant (either inflow or outflow). Diagnosis and therapeutic management of VCs constitute a major challenge in terms of increasing the success rate of liver transplantation. While surgical treatment used to be considered the first choice for management, advances in endovascular intervention have increased to make this a viable therapeutic option. Considering VC as a rare but a major and dreadful issue in OLT history, and in view of the continuing and rapid progress in recent years, an update on these uncommon conditions seemed necessary. In this sense, this review comprehensively discusses the important features (epidemiological, clinical, paraclinical, prognostic and therapeutic) of VCs following OLT.
Keywords: Vascular complications, Orthotopic liver transplantation, Liver transplantation, Endovascular intervention
Core tip: Although vascular complications (VCs) following orthotopic liver transplantation (OLT) seldom occur, they are the most feared complications with a high incidence of both graft loss and mortality, as they compromise the blood flow of the transplant (either inflow or outflow). Diagnosis and therapeutic management of VCs constitute a major challenge in terms of increasing the success rate of liver transplantation. This review comprehensively discusses the important features (epidemiological, clinical, paraclinical, prognostic and therapeutic) of VCs following OLT.
INTRODUCTION
Although vascular complications (VCs) following orthotopic liver transplantation (OLT) are seldom, they are one of the most dreaded complications with a high incidence of both graft loss and mortality, as they compromise the blood flow of the transplant (either inflow or outflow). Khalaf[1], in 2010, reported that patient who presented VCs had significantly inferior graft and patient survival rates. The overall incidence of VCs in adults varies widely among transplant centers worldwide, but remains around 7% in various series of deceased donor liver transplantation (DDLT), and around 13% involving living donor liver transplantation (LDLT)[1-5]. Bleeding, stenosis and thrombosis can arise at any of the vascular anastomoses, as well as aneurysms at the arterial anastomosis and exceptionally on the portal vein[6,7], with an overall reported incidence of 7.2%-15% in adults (mainly arterial 5%-10%, following by portal 1%-3% and caval < 2%) (Table 1)[5,8-10]. In this sense, diagnosis and therapeutic management of VCs constitute a major challenge in terms of increasing the success rate of liver transplantation. This explains why, currently, many transplant teams perform close surveillance of all vascular anastomoses using Doppler ultrasonography, which allows prompt detection and treatment before ineluctable graft failure. All vascular problems must be treated aggressively, particularly in- or out-flows and sudden vascular occlusions (i.e., thrombosis or kinking), such as hepatic artery thrombosis (HAT) and portal vein thrombosis (PVT), which are the most common, and more rarely hepatic veins or cavo-caval thrombosis. Indeed, they can suddenly interrupt hepatic blood supply with both high graft loss and retransplantation rates[1,5,10]. Usually, therapeutic options include surgical revascularization, percutaneous thrombolysis, percutaneous angioplasty, retransplantation and a conservative approach. Although surgical treatment used to be considered the first choice for management, advances in endovascular intervention have increased to make this a viable therapeutic option following OLT. In recent decades, huge advances in the field of interventional radiology have radically changed the diagnostic and therapeutic approaches to VCs in liver transplant patients. For example, technical improvements made in the catheterization of hepatic vessels and computed imaging allow a specific and localized intervention on these pathological vessels, in a less invasive way[1,5,11-18]. As a matter of fact, percutaneous endovascular therapies (i.e., catheter-based thrombolytic intervention, balloon angioplasty and stenting) provided by an experienced interventional radiologist are commonly employed and have supplanted surgery as the therapy of choice in almost all cases[18-20].
Table 1.
Vascular complications following orthotopic liver transplantation
| Type | Delay (incidence) | Clinical presentation | Diagnosis | Treatment |
| Arterial complications | ||||
| HAT incidence: 3.5% | Early HAT (2.9%) | Abnormal transaminase | DUS | Emergent revascularization |
| Fever | ce-MDCT | by endovascular intervention | ||
| Biliary complications | Angiography | or surgical revascularization | ||
| Graft failure | or rLT | |||
| Coagulopathy | ||||
| Late HAT (2.2%) | Asymptomatic | |||
| Fever | ||||
| Abnormal transaminase | ||||
| Bile leak | ||||
| Hepatic abscess | ||||
| Cholangitis | ||||
| HAS incidence: 2%-13% | Early HAS | Graft failure | DUS | Endovascular intervention |
| Biliary complications | ce-MDCT | or surgical revascularization | ||
| Angiography | ||||
| Late HAS | Asymptomatic | DUS | Endovascular intervention | |
| Fever | ce-MDCT | or surgical revascularization | ||
| Abnormal liver function | Angiography | |||
| HAP incidence: 2.5% | Asymptomatic | DUS | Endovascular intervention | |
| Abdominal pain | ce-MDCT | or surgical resection and revascularization | ||
| Fever | Angiography | |||
| HAR incidence: 0.64% | Gastrointestinal bleeding | None in emergency | Emergent surgical hemostasis | |
| Massive bleeding through abdominal drains | and surgical repair | |||
| Hemorrhagic shock | ||||
| Portal vein complications | ||||
| PVT incidence: < 3% | Early | Abnormal transaminase | DUS | rLT |
| Graf dysfunction | ce-MDCT | or surgical repair | ||
| Multi-organe failure | (portal phase) | or endovascular interventions | ||
| Variceal bleeding | Portography | |||
| Late | Ascite | DUS | Curative anticoagulant therapy | |
| Portal vein hypertension | ce-MDCT | |||
| Splenomegaly | (portal phase) | |||
| Variceal bleeding | Portography | |||
| PVS incidence: 2%-3% | Early | Asymptomatic | DUS | Endovascular interventions |
| Portal vein hypertension | ce-MDCT | |||
| Abnormal transaminase | (portal phase) | |||
| Portography | ||||
| Late | Asymptomatic | DUS | Anticoagulant therapy | |
| Ascite | ce-MDCT | and/or | ||
| Abnormal liver test function | (portal phase) | Endovascular interventions | ||
| Portography | ||||
| Caval anastomosis complications | ||||
| Caval resection and end-to-end | Early | Acute Budd-Chiari syndrome | DUS | Endovascular intervention |
| cavo-caval anastomosis | Graf failure | ce-MDCT | or surgical repair | |
| Intestinal congestion | Cavography | or rLT | ||
| Renal dysfunction | ||||
| Lower limb edema | ||||
| Late | Moderate Budd-Chiari syndrome | DUS | Endovascular intervention | |
| Ascite | ce-MDCT | |||
| Cavography | ||||
| Piggy-back | Early | Acute Budd Chiari | DUS | Surgical repair |
| Graf failure | ce-MDCT | or rLT | ||
| Intestinal congestion | Cavography | |||
| Renal dysfunction | ||||
| Lower extremity edema | ||||
| Late | Moderate Budd-Chiari | DUS | Endovascular intervention | |
| Ascite | ce-MDCT | |||
| Lower extremity edema | Cavography | |||
| Renal dysfunction | ||||
| Abdormal liver test function |
Clinical characteristics of arterial and caval complications. rLT: Re-liver transplantation; DUS: Doppler ultrasound; HAT: Hepatic artery thrombosis; HAS: Hepatic artery stenosis; HAP: Hepatic artery pseudoaneurysm; HAR: Hepatic artery rupture; PVT: Portal vein thombosis; PVS: Portal vein stenosis; MDCT: Multi-detector computed tomography.
Considering VCs as rare but as major and dreadful issues of OLT history, and in view of the continuing and rapid progresses in recent years, an update on these uncommon conditions seems necessary. In this sense, this review comprehensively presents the important features (either epidemiological, clinical, paraclinical, prognostic and therapeutic) of VCs following OLT. In this review, only VCs following adult OLT (DDLT or LDLT) are presented, excluding pediatric liver transplantation. Taking into account that biliary complications following OLT also constitute a major therapeutic challenge, and that they are intrinsically linked with hepatic arterial pathology, they are beyond the subject of this article and therefore will not be discussed herein.
ARTERIAL COMPLICATIONS
Arterial complications are still a major source of morbidity and mortality after OLT. Normally, the liver allograft maintains a dual inflow blood supply: Portal and arterial. Hepatic artery (HA) plays a major physiological role, because it provids the blood supply for both the liver parenchyma and the biliary tree. Arterial reconstruction is a frequent therapeutic option after the ligation of different collaterals until, finally, the celiac trunk remains the only arterial vascular supply to the transplanted liver[21]. In patients with traumatic liver rupture with currative ligation of the hepatic artery, it has been reported that bile duct necrosis is not always associated[22]. On the contrary, the interruption or the reduction of arterial flow during liver transplant is frequently associated with biliary tree complications due to ischemic processes (i.e., bile duct necrosis, liver abscesses and graft dysfunction)[23]. This discrepancy can be explained by the absence of collaterals in an OLT recipient[2,24]. In the native liver, HAT or even acute ligation, is usually well-tolerated due to the abundant arterial collateral sources which avoid ischemia of the liver parenchyma. In contrast, disruption of these collaterals inevitably occurs when performing total hepatectomy for OLT. Thus, the allograft may survive by portal and arterial inflows via portal and hepatic artery anastomoses. In cases of HA complications (HAC) perturbing the arterial inflow, the allograft may survive by portal inflow, but only if arterial collaterals exist[2,24,25]. These facts explain why recognition and prompt management of HAC is of great importance for graft and patient survival. The etiology underlying most HAC involves the anastomosis, including: (1) HAT: 1.9%-16.6% (the most frequent and pejorative); (2) anastomotic stricture [i.e., hepatic artery stenosis (HAS)]: 0.8%-9.3%; (3) pseudoaneurysm formation [i.e., hepatic artery pseudoaneurysm (HAP)]: 0%-3%; and (4) hepatic artery rupture (HAR): 0.64%[8,9,18,26]. These complications can be classified into two categories (Table 1): Early (< 1 mo) or late (delayed, i.e., > 1 mo). Very particular attention should be focused on early complications, because they are associated with graft loss and a high mortality rate. In different studies, the definition of early and late complications continues to be discussed. Most of the authors have defined late complications as those occurring after 4 wk, and others after 6 mo[13,25,27,28]. In this review, we consider the recent consensus which defines early complication when it appears within the first month[10,13,18,27,28].
HAT
HAT represent more than 50% of all arterial complications. It is the most frequent and severe vascular complication following OLT. Table 2 usually more frequent after pediatric liver transplantation[5,10,16,17,28-31]. It is the first cause of primary non-function of the liver transplant, which can lead to allotransplant loss and patient death in the early postoperative period. HAT is associated with a high incidence of liver transplant failure (more than 50%) and carries a mortality of more than 50% in the absence of revascularization or retransplantation. In recent years, early revascularization by means of endovascular catheter-based intervention has been a viable option for graft salvage before considering retransplantation. Indeed, the retransplantation rate is very high in untreated HAT (25%-83%) compared to graft revascularization treated patients (28%-35%)[3,10,13,16,17,30,32-40].
Table 2.
Hepatic artery thrombosis highlights
| Summary of the clinical characteristics about HAT |
| HA supplies exclusively the bile duct, so HAT is associated with a high frequency of biliary complications |
| HAT represents more than 50% of all arterial complications following OL |
| The incidence of HAT following OLT is 3.5% with early and late HAT incidences of 2.9% and 2.2%, respectively |
| HAT carries an incidence of graft failure and mortality of more than 50% without prompt treatment |
| The median time to detection of early and late HAT was 6.9 d (range: 1-17.5 POD) and 6 mo (range: 1.8-79 mo), respectively |
| No differences in HAT incidences were observed between DDLT and LDLT |
| Clinical presentation spectrum: Mild elevation of serum transaminase and bilirubin levels (75%), biliary complications (15%), fever and sepsis (6%), graft dysfunction or failure (4%) |
| Risk factors of early HAT are mainly represented by technical problems, LDLT, cigarette smoking and hypercoagulability state, while late HAT is usually related to ischemic or immunologic injury: CMV positive donor, female donor and male recipient and hepatitis C seropositive recipient |
| Early diagnosis is achieved by assessing the serum transaminase level and performing Doppler ultrasound monitoring in the postoperative period and confirmed by contrast-enhanced abdominal CT scan and/or visceral angiography |
| Currently, the literature on the curative management of early HAT suggests the following procedures: First endovascular radiological intervention (IAT, PTA and stent placement), secondly open surgical revascularization, and finally retransplantation, which is associated with the best survival rate compared with revision or thrombolysis, but is a limited therapeutic option due to organ shortage |
HA: Hepatic artery; HAT: Hepatic artery thrombosis; OLT: Orthotopic liver transplantation; DDLT: Deceased donor liver transplantation; LDLT: Living donor liver transplantation; CMV: Cytomegalovirus; IAT: Intra-arterial thrombolysis; PTA: Percutaneous transluminal angioplasty; CT: Computed tomography.
Definition: HAT is defined as a thrombotic occlusion of the hepatic artery. It has been classified, as described above, into two types depending on the time of presentation following OLT: Early HAT [within the first 30 d of liver transplantation (LT)] and late HAT (after 30 d of LT)[13,17,28]. The hepatic artery supplies the biliary tree of the transplant, explaining the high frequency of biliary complications in HAT (i.e., biliary ischemia, necrosis, stricture, sepsis) and eventually hepatic insufficiency and graft loss[31].
Incidence: The true incidence of early HAT following OTL is unknown, but it varies widely from 0% to 12% in adults[5,9,24,25,27,30,38,41]. Bekker et al[28] (2009) reported in a systematic review comprising 21822 OLT cases an incidence of 843 cases (adults and children) of early HAT with an overall incidence of 4.4%. In adults, the incidence of HAT was 2.9%. They also showed that the incidence of early HAT had decreased over time since the first report in 1982 by Starzl (6.9% in 1996 vs 3.2% in 2006) with improvements in perioperative care. They reported that there were no differences in incidence among transplantation centers worldwide[2,28]. Median times to the occurrence detection of early and late HAT were respectively 6.9 postoperative days (range: 1-17.5) and 6 mo (range: 1.8-79 mo)[17].
In literature, it does not confirm that HAT incidence in LDLT is significantly lower or higher compared to HAT incidence in DDLT. Many studies show contradictory results[1,9,17,28,41] but, a meta-analysis on HAT found no significant difference with an incidence of 3.1% and 4.6% in LDLT and DDLT, respectively[28]. Furthermore, it was reported that arterial anastomosis with operation microscope or loupe mangnification did not show any difference in incidence HAT[9,17,28,41].
Late HAT shows a lower incidence, ranging from 1% to 25%[38,42]. Torras et al[34] (1999) reported an incidence of 7.5% (35/413) following OLT. Sixteen cases occurred during the first month (early HAT): Diagnosis made from 1 to 13 d after OLT (median: 2.5). Nineteen cases were late HAT (> 30 d, from 2 to 79 mo after OLT (median: 5 mo)[34].
Clinical presentation: The clinical presentation of HAT range from a mild elevation in serum amino transferase (most frequently in patients with HAT) and bilirubin levels to fulminant hepatic necrosis. HAT is associated with elevated transaminases in 75%, biliary complications in 15%, fever and sepsis in 6% and graft dysfunction or failure in 4% of cases[5]. The clinical expression depends on the timing of the onset of HAT as well as on the existence of collaterals[5,25,27]. Usually, initial non-function or severe allograft dysfunction predominately occurs in patients with early HAT. This explains the importance of symptomatic expression, whereas biliary tract complications (i.e., bile duct strictures or bile leaks sometimes leading to biliary hepatic abscesses) are more frequently, but not exclusively, associated with late HAT. Indeed, clinical expression depends on the existence of collaterals, which can develop as early as within two weeks[17,24,27]. Therefore, two main forms of HAT are recognized: (1) acute presentation (early HAT) characterized by a severe clinical course; and (2) delayed presentation (late HAT) generally associated with a milder clinical course[25].
In every cases, early HAT clinically manifests with fever, increase leukocytosis and a important elevation in liver enzyme levels. The natural history of early HAT could be summarized as biliary tract necrosis followed by uncontrolled septic shock in the immunosuppressed population, and even by the patient’s death[17,27,28,31,38]. The pathophysiological process of early HAT results in injury to the bile duct epithelium and to hepatocytes. This leads to massive necrosis in the allograft, partly due to the disruption of arterial inflows (i.e., main flow by HA and accessory physiological collaterals), explaining the high incidence of biliary sepsis in early HAT[25,27,28].
It is usually assumed that late HAT is due to ischemic or immunological damages with a more insidious onset. Up to 50% of patients with late HAT can be asymptomatic with elevated liver function tests only[10,19,27,36]. Symptomatic patients often present with biliary complications including recurrent cholangitis, bile duct stricture/stenosis, biliary leakage, biliary tract necrosis and abscess formation revealed by relapsing fever and bacteremia. The presentation may be insidious. Liver graft ischemia and liver failure are other classical insidious clinical outcomes revealing late HAT[17,27,28,36,38,42,43].
Risk factors: Several reports studied the risk factors associated with HAT[5,10,17,19,25,27,28,34,44,45]. They can be divided into several categories. It is usually considered that technical problems are mainly associated with early HAT. Conversely, risk factors for late HAT are less well-defined. However, a donor positive CMV status and a recipient negative cytomegalovirus (CMV) status have repeatedly been shown to be a possible risk factor for late HAT[27,45]. Moreover, specific factors of late HAT reported include the association of female donor and male recipient, hepatitis C virus positive recipients, episodes of rejection, tobacco consumption and retransplantation[10,17,27,45,46]. Besides, while some authors believe that HAS and hepatic artery kinking are the initiating factors, others suggest a perioperative hypercoagulable state as a possible underlying cause[5,10,17,28,29].
Truly, the cause of early HAT is still under debate and remains unknown in most cases. Up to 20% of HAT cases are probably due to surgical causes (technical problems) in the arterial anastomosis, such as difficult anastomosis, technical imperfections with the anastomosis, kinking, stenotic anastomosis, small vessel size, reduction in a disparate diameters of the arteries, dissection of the hepatic arterial wall, celiac stenosis or compression by the median arcuate ligament, the presence of multiple arteries, aberrant or complex donor/recipient arterial anatomy or arterial abnormalities requiring complex arterial reconstructions, complex backtable arterial reconstruction of the allograft, poor quality donor and recipient vessels and high-resistance microvascular arterial outflow caused by rejection or severe ischemia-reperfusion injury. Those problems are more common among centers performing fewer than 30 OLT a year; the incidence of HAT diminishes with the surgical team’s experience. Therefore, surgical causes probably do not represent the main risk factor for HAT[17,28,29,31,38].
It has been reported that HAT can occurs within a few hours after LDLT, which indicates a population at higher risk of HAT. Indeed it has been shown that these patients displayed a higher rate of VCs explained by the complexity vascular reconstructions linked to smaller and shorter caliber of donor and recipient vessels[1,10,47].
Regarding the non-surgical risk factors involved in the occurrence of HAT, donor age > 60 years, extended cold ischemia time, lack of ABO compatibility, cigarette smoking, hypercoagulability state, donor positive for CMV in a CMV-negative recipient, rejection, regrafts and transplant for primary sclerosing cholangitis have been shown to be statistically linked with the occurrence of HAT[17,28,38,46]. However, the literature review dealing with this issue displayed conflicting results. Indeed, some authors reported that some parameters like cold ischemic time, donor age and the presence of rejection were not found to be factors related to the development of HAT[34]. This emphasizes the difficulty in accurately determining the risk factors associated with early HAT. In a recent study, Panaro et al[48] (2014) have shown a statistical association between TACE and the radiological and histological arterial wall injury, as in the past 25 years TACE has been widely used in the treatment of HCC. This procedure may potentially cause vascular lesions in the arterial wall (catheterization and drug infusion), suggesting that previous transarterial chemoembolization (TACE) could constitute a risk factor of HAT when future OLT is performed[5,48].
Some practices could prevent the occurrence of HAT, and the data reported by Duffy et al[5] (2009) demonstrates that arterial reconstructions which restore the normal anatomy and gentle handling of vessels are of great importance in the accomplishment of hepatic arterial anastomosis. Some studies reported that recipients with multiple anastomoses for arterial reconstruction should receive aspirin and Doppler ultrasound (DUS) assessment to screen the patency of the reconstructed hepatic artery. Moreover, the use of aortic conduits for arterial reconstruction is a risk factor that warrants the initiation of prophylaxis in the post-transplant period[5,10,17,19,25,31,44]. For patients with inheritable thrombophilic diseases; given the devastating effects of HAT on graft outcomes, it should be necessary to identify these to prevent thrombotic complications. It is likely that patients who present both hematological and operative factors are most at risk, and routine anticoagulation in the post-OLT setting should be instituted. In sum, many studies recommand peritransplantation anticoagulation with heparin or an antiplatelet agent in patients with extraanatomic conduits, complex backtable reconstruction, or pre-OLT TACE. However, the best prophylactic approach is controversial, and this should be clarified by randomized, controlled trials[5,10,17,19,31,44,25]. An interesting report by Marín-Gómez et al[40] (2012) demonstrates that intraoperative blood flow allows for a prediction of the occurrence of HAT when it is less than 100 mL/min with 84.5% sensitivity and a predictive positive value of 97.8%.
Diagnosis: Early diagnosis is mandatory to allow immediate treatment and to prevent graft loss. The detection of these patients includes biological (serum transaminase levels) and morphological (DUS) exams, while visceral angiography allows to confirm the diagnosis. DUS is a proven non-invasive technique and the gold standard investigation to assess hepatic artery patency. It detects the absence of hepatic artery flow, even in its intrahepatic branches. The DUS diagnosis comprize the lack of HA signal (Se = 92%) or an increased resistive index (RI)[25,17,38]. Even though the screening protocol varies between liver transplant centers, a DUS surveillance protocol of the hepatic artery can detect reduced hepatic arterial flow and to allow for prompt revascularization management, which may result in transplant salvage[17]. In sum, in case of an abnormal elevation in liver enzymes and suggestive findings on DUS, abdominal computed tomography (CT) angiogram or angiography confirmed diagnosis and it can precisely shows an underlying anatomical defects (stenosis or kinking) with a high sensitivity and specificity specificity (Figure 1)[17]. Pareja et al[38] (2010) established a screening protocol for early HAT, consisting of a first Doppler ultrasound within 48 h of OLT and in another Doppler ultrasound 7 d later. If the first examination is conclusive, they perform contrast ultrasound (microbubbles) or computed tomography. When HAT is confirmed, arteriography should be performed[38]. Intimal hyperplasia causing progressive HAS may precede late HAT and may be screen by regular (yearly) post-OLT DUS assessment. In some cases, HAS is likely to stimulate the development of arterial collaterals that protect the liver from ischemia at the time of HAT[25,48].
Figure 1.
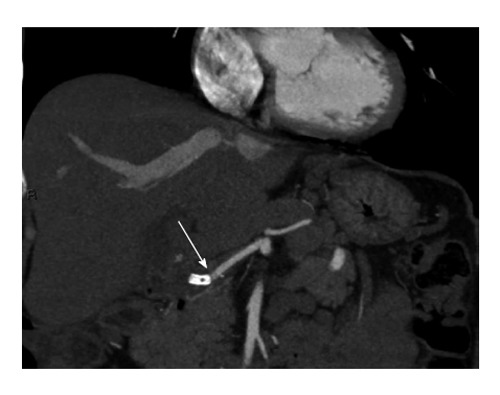
Contrast-enhanced-multidetector-row computed tomography-scan showing hepatic artery thrombosis after an endovascular intervention with stent placement. Thrombus (arrow).
Therapeutic management: Classically, we consider several treatment modalities for HAT: (1) revascularization (surgical or endovascular); (2) retransplantation; and (3) observation. Currently, the most effective treatment approach remains controversial and the choice of any of these treatments depends on the time of diagnosis. Early diagnosis, prompt revascularization and retransplantation have been considered the only solution to rescue patients with HAT. Historically, retransplantation is the treatment of choice for most groups, offering the best survival results[5,16]. However, this possibility is strongly conditioned by the shortage of donors and by the patient’s condition[16,17,27,38,39]. Percutaneous endovascular treatments including intra-arterial thrombolysis (IAT), percutaneous transluminal angioplasty (PTA) and stent placement have shown hopeful outcomes in the literature. Finally, some patients survive without revascularization or retransplantation by developing collateral circulation distal to the thrombosis, but this occurs in rare cases[17,20,24,38,39]. Despite these encouraging results of endovascular interventions, the efficacy and risk of complications (mainly represented by hemorrhage risk) make this therapeutic option still controversial. Moreover, in some cases these are ineffective and surgical intervention (including anastomotic revision and retransplantation) must be applied. The complications of PTA include thrombosis, vascular dissection and rupture. Thus, urgent revascularization by means of endovascular interventions as a primary option offers could give a chance to avoid rLT, but only in asymptomatic patients[8,10,17,20]. Despite the proof of efficacy and safety of thrombolytic treatment with different products and regimens (urokinase, streptokinase, alteplase), the best protocol is not still known and there are currently no specific guidelines for thrombolytic therapy application. Furthermore, several studies recommend low dose of heparin in association with thrombolytic despite incresing the risk of adverse bleeding. Indeed, hemorrhage is the most frequent adverse effect and concern about 20% of patients: Ranging from blood in the drainage to intra-abdominal hemorrhage, which could be fatal in some cases. This is mainly true in early postoperative period, but selective thrombolysis via the hepatic artery presents several advantages, such as a smaller thrombolytic dose, a highly localized concentration and little influence on systemic coagulation[17,20]. Endoluminal IAT with restoration of flow should be associated with underlying anatomic defects treatment if present, including reduction of kinking, treatment of an anastomotic stenosis and often requires balloon angioplasty and/or stent placement[16,20]. Association of IAT with PTA and/or stenting showed better efficacy and survival rates when compared to IAT alone. In summary, PTA and stent placement are currently tried first to resolve the problem in many centers[10,20]. Open surgical revascularization of thrombosed liver transplant is considered a viable option to save the transplant and to avoid retransplantation. Open surgical revascularization can be performed in various ways depending on the length and on the integrity of the recipient and on the graft arterial stumps. The procedure in its simplest form can be a Fogarty thrombectomy and a primary resuture of the end-to-end hepatic artery anastomosis[16]. Duffy et al[10] evaluated 4234 LT from 1984 to 2007: 203 (5%) developed HAT including 133 early and 70 late HAT; the occurrence of HAT was 3.9% in adults. Overall 90 patients were treated with surgical exploration, thrombectomy, or anastomotic revision. Nine patients were treated with catheter-based thrombolysis and 13 patients received anticoagulation. Of the patients with early HAT who underwent thrombectomy and anastomotic revision, only 9 (10.5%) had graft salvage, and the remaining patients needed re-transplantation. Overall, re-transplantation was necessary in 153 (75%) patients with HAT. Therefore, retransplantation after HAT has a better survival rate compared with revision or thrombolysis[5,10].
In contrast, some patients with late HAT survive without revascularization or retransplantation by developing a collateral circulation distal to the thrombosis. The mean time between the diagnosis of HAT and the neovascularized liver is 4.1 mo (range: 3-5.5 mo). Four factors are associated with the development of a neovascularized liver: Late HAT, early HAS, site of thrombosis, and Roux-en-Y anastomosis[24,39]. These results confirm that a slow arterial obstruction process allows for the formation of arterial substitute pathways, but this striking neoangiogenesis capacity, only significant in cases of chronic ischemia, is insufficiently rapid in the case of early HAT. Given the improved outcome of the conservative treatment of liver transplant recipients, in whom late HAT develops without revascularization or retransplantation, revascularization in this condition is controversial. Based on two limitations (the relative lack of utility of revascularization of late HAT and the contraindication to early postoperative thrombolysis), Saad et al[16] (2007) proposed that the clinical window of the applicability of transcatheter thrombolysis should be most likely from 1 to 3 wk to 1 to 3 mo post-transplantation, respecting contraindications to avoid fatal bleeding complications. However, successful and safe pharmaceutical thrombolysis was described by Figueras et al[11] (1995) 3 d after OLT. In the literature, the time interval between the transplant and thrombolysis procedures ranges from 2 to 120 d (mean, 53 d)[11,16,27,49-51].
Prognosis: At the time of revascularization, survival rates is 40% in symptomatic vs 82% in asymptomatic patients[17]. The incidence of HAT has a significant impact on transplant and recipient survivals. Indeed, Silva et al[27] (2006) reported an overall mortality rate of 23% in those developing HAT post-OLT. In the meta-analysis reported by Bekker et al[28] (2009) HAT was a major cause of graft loss (53.1%) and mortality (33.3%) in the early postoperative period.
Conclusion: HAT is rare but it represent the most common vascular complication following LT. A definitive diagnosis is achieve by angiography, which may detect predisposing anatomical anomalies. Moreover, it allows prompt therapeutic management in the same time. IAT can be performed alone and an eventual anatomical anomaly may then be corrected by endovascular procedures such as balloon angioplasty and/or stent placement, or a surgical intervention. Currently, it seems reasonable to propose endovascular treatment first, mainly due to organ shortage and the high mortality related to retransplantation, considering the highly individualized outcome and depending of the competence of the transplant center. However, in the early post-transplant period, it is widely accepted that symptomatic patients with severe allotransplant dysfunction and symptoms related to arterial thrombosis need retransplantation.
Hepatic artery stricture/HAS
Definition: HAS following OLT is defined as a narrowing of the transverse diameter of the HA, more or less extended, resulting in graft ischemia mainly revealed by elevated liver function tests[2,16,52-56]. Significant HAS is usually defined as a narrowing of the transverse diameter > 50% on angiogram associated with clinical suspicion and a RI < 0.5 (defined by peak systolic flow-end diastolic flow/peak systolic flow) and a peak systolic velocity > 400 cm/s detected by DUS[16,57,58]. HAS and HAT are the most common hepatic arterial complications, with high rates of morbidity and mortality[56,58] (Table 3).
Table 3.
Hepatic artery stenosis highlights
| Summary of the clinical characteristics about HAS |
| Significant HAS is defined as a narrowing of the transverse diameter > 50% on the angiogram associated with clinical suspicion, with a resistive index < 0.5 and a peak systolic velocity > 400 cm/s detected by DUS |
| HAS occurs in 2% to 13% of transplants, at the level of the anastomosis (59% of cases), graft HA (41%) or recipient HA (2.6%) |
| HAS has been speculated to progress to HAT in 65% of cases at 6 mo for untreated HAS |
| The median time to diagnosis is 100 (range: 1-1220) d following OLT |
| Most of patients with HAS are asymptomatic and most commonly present only with abnormal liver function tests and in rare cases with graft failure |
| Routine screening by DUS during the postoperative period is mandatory because of the insidious clinical presentation |
| The risk factors are not really known, but among these, technical and surgical factors (vascular injury such as clamp injury, intimal dissection, faulty placement of anastomotic sutures, excessive length with kinking and angulation, differences in the vessel caliber that require and oblique anastomosis, vasa vasorum disruption) or acute cellular rejection |
| DUS is a non-invasive method for the assessment of HA patency, but a contrast-enhanced CT scan and angiography are required to confirm the diagnosis |
| Radiological endovascular intervention by PTA with or without stent placement is often used to treat post-transplant HAS and are both efficacious, with 7% to 12% of complications including dissection and arterial rupture, restenosis or thrombosis (25%) and 12% failed attempts |
| Surgical revision and retransplant showed a high rate of success, but the overall mortality rate was as high as 20%. In some case, HAS may be an early sign of chronic rejection |
DUS: Doppler ultrasound; HA: Hepatic artery; HAT: Hepatic artery thrombosis; HAS: Hepatic artery stenosis; OLT: Orthotopic liver transplantation; PTA: Percutaneous transluminal angioplasty; CT: Computed tomography.
Incidence: HAS occurs in 2% to 13% of transplants and has been suggested to progress to HAT implicating, at least in part, that HAS and HAT are two contiguous components of the broader allotransplant ischemic spectrum[2,16,30,52,53,55,56,58-60]. Wozney et al[2] (1986) reported three cases in which untreated anastomotic strictures of the hepatic artery progressed to HAT. Saad et al[52] (2005) emphasized the correlative progression of untreated significant HAS to HAT with an incidence rate of 65% at six months for untreated HAS[2,16,52]. Abbasoglu et al[57] (1997) reported an incidence of 4.8% in a cohort of 857 consecutive OLT from 1988 to 1995. The median time to diagnosis was 100 d (range: 1-1220 d) following OLT, which was also reported by Denys et al[60] (2002) with a mean time to diagnosis at 94 d post-OLT[57,60]. Similar to HAT, HAS may be divided in two groups: HAS occurring within 30 d after OLT (early HAS), and HAS occurring more than 30 d after OLT (late HAS). Chen et al[61] (2009) reported an overall HAS incidence of 2.8%, with an early HAS incidence of 40% vs a late HAS incidence of 60% (mean time elapsed between transplantation to diagnosis: 91 d; range: 1-430 d). Abbasoglu et al[57] (1997) reported that stenosis occurred in 59% of cases at the level of the anastomosis with a median time of diagnosis at 75 d post-OLT, in 41% of cases at the level of the graft HA with a median time of diagnosis at 160 d post-OLT, and in 2.6% at the level of the recipient HA[57]. Saad et al[52] (2005) did not confirm these results. Indeed, the literature has established that the anastomotic stenosis is the most common place for the development of HAS within three months after LT[10,62].
Clinical presentation: The clinical presentation of HAT range from normal liver function to transplant failure secondary to ischemia or necrosis. Moreover, HAS can lead to an insidious form of graft disorder, both in the early and later postoperative stages. Many patients with HAS are asymptomatic and most commonly present only with abnormal liver function tests (LFT)[16,52,57,58,60,63,64]. Indeed, Abbasoglu et al[57] (1997) reported that an elevation in LFT was the main clinical presentation. Most asymptomatic patients are detected during routine DUS screening. In fact, the non-specific and insidious clinical presentation of HAS mandates to perform routine screening DUS at regular time intervals. In contrast, it is obvious that DUS screening should be highly required for OLT asymptomatic patients presenting elevated LFT.
Compared with HAT, the risks of developing biliary complications, including biliary strictures and bile leaks, are less frequent with HAS. Ideally, HAS should be diagnosed before the occurrence of biliary complications, because of the significant impact on both graft and patient survival[10,19,57]. Indeed, incidence of biliary complications is reported to be as high as 67% in liver transplant recipients with HAS[52,63,64].
Risk factors: The risk factors of HAS are not really known and seem to have a multifactorial origin[60]. Many authors suggest perioperative factors (technical) of vascular injury (clamp injury, intimal dissection, faulty placement of anastomotic sutures), donor and recipient factors (excessive length with kinking and angulation, differences in vessel caliber that require oblique anastomosis), and others, such as extrinsic compression and microvascular injury, i.e., vasa vasorum disruption or acute cellular rejection[52]. Abbasoglu et al[57] (1997) demonstrated that a low mean initial HA flow (less than 400 mL/min) after OLT is a risk factor for developing anastomotic HAS, but they did not identify a risk factor. Moreover, they showed that the presumed immunological bases, such as autoimmune hepatitis, primary biliary cirrhosis and primary sclerosing cholangitis for their OLT, were not risk factors for HAS[57].
Diagnosis: DUS is a well-established non-invasive method for the assessment of HA patency, and its efficiency in the early diagnosis of HAS has been reported in several studies[52,57]. Abbasoglu et al[57] (1997) showed a DUS sensitivity of 85% in detecting HA stenosis. DUS showed a sensitivity of 100%, a specificity of 99.5%, a positive predictive value of 95% and a negative predictive value of 100%, and an overall accuracy of 99.5% in early HAS diagnosis[10,57,62,65]. Many teams also use MDCTA and standard angiography to confirm the diagnosis, which is the gold standard for HAS diagnosis[10,62,65].
Therapeutic management: The therapeutic management of HAS includes either surgical revision, retransplant or percutaneous endovascular interventions, such as PTA with or without stent placement[52,57,60,63,64,66] (Figures 2 and 3). Abbasoglu et al[57] (1997) reported 35 cases of surgical revision, including aortohepatic iliac artery graft (from banked donor vessels), autologous saphenous vein patch angioplasty and resection of the stenotic segment either with primary reanastomosis or with interposition of a banked iliac artery or saphenous vein graft. In this group, HA flow was reestablished successfully in all patients. At a mean follow-up of 25 mo, 67% of patients were asymptomatic with normal liver function. Six patients were treated with PTA. Five of them were found to be asymptomatic at a mean follow-up of 25 mo[57]. Indeed, balloon angioplasty can be an effective treatment option in these cases[10,19]. Similar to Abbasoglu et al[57] (1997), Saad et al[52] (2005) also reported 81% successful treatment of cases in a series of 42 cases of significant HAS treated by PTA, with an incidence of immediate complication of 7% including dissection and arterial rupture[52,57]. Delayed complications (i.e., HAT) within 30 d of PTA occurred in 5% of cases, yielding a total complication rate of 12% and 12% total failed attempts without consequences. In this treatment modality, very different rates of restenosis have been reported from no restenosis to rates as high as 75%[60,63,64,67,68]. Denys et al[60] (2002) reported a low rate of HAT among 13 HAS patients treated by HA stent placement, which may be attributed to anticoagulation and/or antiplatelet regimens that were routinely given to their patients[52,60]. In their study, they also reported a post-HA stent placement HAT in one patient, and four patients with intra-stent restenosis in whom restenosis was dilated successfully. Other teams showed that primary stenting of the HA is feasible and offers a low complication rate with an acceptable one-year patency rate[60,69]. Ueno et al[69] (2006) reported an incidence of restenosis of 25% after stent placement, which is significant, but Sommacale et al[56] (2013) demonstrated that repeated endovascular treatment of recurring HA stenosis carries a high rate of success[56,69]. However the best time for the earliest endovascular intervention after liver transplant is currently still discussed. Boyvat et al[66] (2008) reported endovascular intervention performed within seven days after transplant in nine patients, with a mean intervention time of 34.6 d (range: 6 h-210 d). They experienced extravasation or HAR in five patients and used graft-covered stents to solve this issue in all patients. They suggested that this technique should allow for safer endovascular intervention with no restriction time after surgery and with an acceptable benefit/risk ratio[66]. Finally, a recent published meta-analysis of case series has reported that interventional radiological procedures are often used to treat post-transplant HAS, and that PTA with balloon dilation alone or associated to stent placement are both efficacious and show similar complication rates and decrease the retransplantation rate[55].
Figure 2.
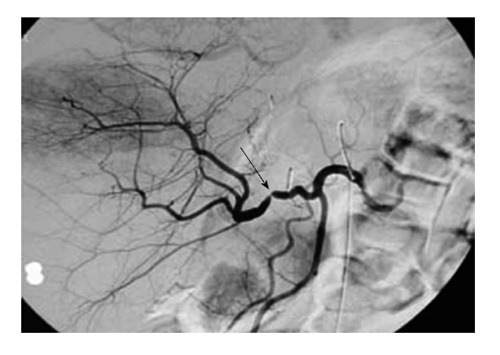
Arteriography showing an anastomotic hepatic artery stenosis after orthotopic liver transplantation. Stenosis (arrow).
Figure 3.
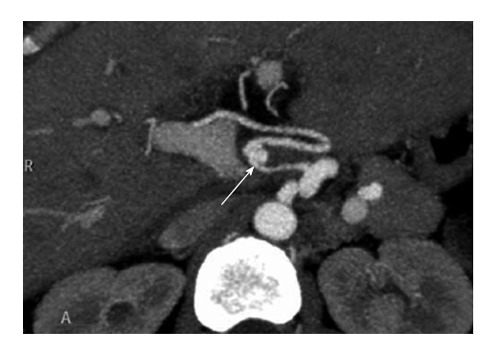
Contrast-enhanced-multidetector-row computed tomography-scan showing a hepatic artery pseudoaneurysm following orthotopic liver transplantation. Pseudoaneurysm (arrow).
Prognosis: In the study by Abbasoglu et al[57] (1997) the overall mortality was 20%, mainly in the surgical revision group. Nineteen percent of patients with HAS had retransplantation with a median time of four months (range: 11 d-21 mo). It is interesting to note that among these, five had chronic rejection not diagnosed prior to HA revision, suggesting that HA stenosis should be an early sign of chronic rejection[57]. Therefore, Abbasoglu et al[57] (1997) recommended that every HAS patients should be screened for chronic rejection. The patient and graft survival rates at four years in the revised HA group were 65% and 56%, respectively; these rates were not significantly different from those of the control group[57].
Conclusion: To conclude, HAS requiring revision is an uncommon condition after OLT. Early diagnosis by means of systematic DUS in the postoperative period and prompt revascularization procedures, with percutaneous endovascular methods with or without stent placement first, are usually successful with long-term graft and patient survival[56]. Individualized therapeutic regimens should be applied to treat HAS according to the technical platform available within transplant centers. When endovascular intervention fails to rescue arterial blood inflow, surgical revascularization should be attempted, especially if HAS is associated with biliary complications before considering retransplantation, which carries a higher mortality rate[70]. Finally, a meticulous arterial anastomosis suture with careful attention of a sufficient arterial flow into the liver transplant seems prevent this complication.
HAP
Definition: HAP is defined as a dilated hepatic artery, which occurs after iatrogenic injury in most cases, causing blood to leak and pool outside the artery wall into surrounding tissue, with a persistent communication between the HA and the resultant adjacent cavity (Table 4). This is a very unusual event, with a reported incidence of 0.27%-3%[26,30,71-80].
Table 4.
Hepatic artery pseudoaneurysm highlights
| Summary of the clinical characteristics about HAP |
| The reported incidence of HAP is ranging from 0.27% to 3% following OLT |
| In most cases, HAP is localized extra-hepatic and occurred in the early postoperative period around 1 mo post-OLT (69% within 20 d and 81% within 35 POD) |
| Clinical presentation varies from the asymptomatic state and incidental diagnosis to abdominal pain with fever and gastrointestinal bleeding (25% of cases, massive bleeding through the abdominal drain or acutely with hemorrhagic shock) |
| Risk factors include peritoneal infection, biliary leak, bilbo-digestive anastomosis and digestive leak |
| Diagnosis of HAP is confirmed by DUS (with lower performance), contrast-enhanced CT scan, magnetic resonance angiography or angiography |
| Treatment of HAP includes reoperation (urgent laparotomy for HA ligation: Mortality rate 60%; HAP excision and immediate revascularization with a cryopreserved arterial allograft: Mortality rate 28%) or interventional radiology (HA embolization with a coil or HAP exclusion with a covered stent) |
| HAP has a worse prognosis with an overall mortality of more than 50% (ranging from 53% to 100%) |
| Early recognition of HAP in the population at high risk is mandatory and allows for a successful therapeutic outcome in 100% of cases |
DUS: Doppler ultrasound; HA: Hepatic artery; HAP: Hepatic artery pseudoaneurysm; OLT: Orthotopic liver transplantation; CT: Computed tomography.
Incidence: In the retrospective cohort studied by Volpin et al[81] (2014) on 787 LT performed between January 1990 and 31 December 2005, a HAP incidence of 2.5% was reported, uniformly distributed over the 16-year period. The authors showed that this complication did not significantly affect any specific indication for liver transplantation. In the 16 patients that were concerned, the anatomical localization of HAP was extra-hepatic and occurred after the first liver transplant. In fact, most HAP occurred in the early postoperative period around one month post-OLT: 69% presented within 20 d and 81% within 35 d following LT. The median time of presentation of HAP was 13 d. This corresponds to the median time reported by many authors, varying from 13.4 to 29 d post-LT[26,30,78,80,81].
Clinical presentation: The clinical presentation of HAP varies from the asymptomatic state and incidental diagnosis upon imaging to abdominal pain associated with fever, gastrointestinal bleeding (25% of cases), massive bleeding through the abdominal drain in the very early post-LT period (31% of cases) and acutely with hemorrhagic shock (81% of cases, the most frequent in the series of Volpin et al[81], 2014). These imply additional investigations, such as emergent abdominal imaging.
Risk factors: Several predisposing factors have been suggested, including peritoneal infections, technical difficulties during the completion of arterial anastomosis and biliary leak[26,30,71-83]. The rate of patients with extra-hepatic HAP and with bacterial or fungal organisms isolated from the peritoneal fluid or from the arterial wall is very high. In the series of Volpin et al[81] (2014), these patients accounted for 81% of the total (microorganisms cultured from the HAP wall: 50% of cases; cultured from the abdominal fluid: 31% of cases), and other authors report a rate varying from 66% to 100%[26,30,71,73-81,84,85]. Four patients of the Volpin series had a biliary leak discovered before or at the same time as HAP. Indeed, bile leak and bilio-digestive anastomosis were found to be risk factors for HAP, suggesting that enterotomy, bile and digestive leaks could be a source of peritoneal contamination, be considered very seriously and treated promptly because of the risk of HAP formation. In contrast, LDLT, reduced size, split, auxiliary LT and retransplantation were not risk factors for HAP.
Diagnosis: In the study by Volpin et al[81] (2014), the diagnosis of HAP was made by DUS, contrast-enhanced CT scan or angiography (Volpin et al[81], 2014) (Figure 4).
Figure 4.

Arteriography showing a hepatic artery stenosis due to a kinking following orthotopic liver transplantation. Kinking stenosis (arrow).
Therapeutic management: Treatment of HAP can be achieved by reoperation or interventional radiology[26,75,78,81,86]. In the series of Volpin et al[81] (2014), five patients underwent urgent laparotomy for HA ligation; three of them died in the immediate postoperative course with a mortality rate of 60%. The two survivors had biliary complications[81]. Among patients treated by HA ligation, other authors confirmed this unfavorable outcome: 28% mortality in the series of Madariaga et al[73] (1992), 75% in the series of Marshall et al[78] (2001) and 85% in the series of Bonham et al[74] (1999). Moreover, this treatment exposes survivors to impaired liver function, graft loss and finally retransplantation[81,85]. Despite these poor outcomes, Boleslawski et al[26] (2013) reported that HA ligation without revascularization is regarded as a reasonable option, with no early mortality in 10 patients with HAP rupture treated by ligature without revascularization. Six of them were still alive without retransplantation after a median follow-up of 70 mo[26]; seven patients underwent HAP excision and immediate revascularization. The arterial continuity was directly restored in five cases and cryopreserved arterial allograft conduits were interposed in two cases. In three cases, concomitant biliary complication was treated simultaneously by bilio-enteric anastomoses. Two patients died postoperatively (mortality rate of 28%). In this subgroup of treated patients, 66% of cases had an uneventful outcome, which seems to offer the best outcome in an emergency setting. Finally, two patients were treated by interventional radiology. One patient underwent embolization with a coil for deliberate HA occlusion; at 10.5 years of follow-up, this patient has good liver function without biliary complications. Another patient had HAP exclusion with a covered stent inserted into the HA; this patient has good liver function at 10 years of follow-up[81].
Prognosis: Volpin et al[81] (2014) reported an overall mortality of 50%. Among patients who presented with HAP rupture, the mortality rate was 53%. The three patients treated before HAP rupture occurred are still alive after 10 years of follow-up[81]. In the literature, HAP is associated with a high mortality rate, ranging from 69% to 100%[26,30,71-81].
Conclusion: To conclude, the early recognition of HAP in a high risk population (patient presenting with a documented peritoneal infection, bacteremia, bile and/or digestive leak, or bilio-digestive anastomosis) is crucial to expressly carry out diagnostic assessment and therapeutic management by percutaneous endovascular techniques first. Surgical intervention for HAP excision should be followed by immediate revascularization, even in an infected field, if endovascular management has failed. Recognition before rupture should allow a successful outcome in 100% of cases. Keeping in mind that HAP is usually asymptomatic before rupture, that it occurs most often within the first five weeks post-LT and the poor performance of DUS[87], Volpin et al[81] (2014) suggested that a contrast-enhanced CT scan or magnetic resonance angiography should be performed.
HAR
Definition, incidence and risk factors: HAT is defined as a severe hemorrhage from the trunk or from a main branch of the HA. It is a very serious complication that results in the disruption of the arterial blood supply of the transplant. This is a very exceptional but a dramatic complication after OLT which carries very high incidence of liver transplant loss and high mortality rate. In most cases, this condition complicates a pseudoaneurysm of the HA, leading to major bleeding that requires emergency operation. Many reports reported the role of infectious pathogens as the cause in the development of pseudoaneurysms. Diagnosis of pseudoaneurysms is accessible with various radiological techniques, but in half of cases, HAP is not recognized before rupture, requiring immediate surgery[26] (Table 5).
Table 5.
Hepatic artery rupture highlights
| Summary of the clinical characteristics about HAR |
| HAT is defined as a severe hemorrhage from the trunk or from a main branch of the HA, resulting in disruption of graft arterial blood supply |
| This is a very rare (incidence of 0.64%) but a dramatic complication following OLT with a high mortality rate |
| In most cases, HAR complicates a pseudoaneurysm of the HA |
| The median time of HAR is 29 d (range: 2-92 d) following OLT |
| The clinical presentation is always a sudden hemorrhage: Hemoperitoneum, gastrointestinal bleeding, hematoma and hemobilia |
| Treatment comprises urgent laparotomy with definitive ligation of the HA, anastomotic revision and aortohepatic grafting or interventional radiology with percutaneous embolization |
HA: Hepatic artery; HAT: Hepatic artery thrombosis; OLT: Orthotopic liver transplantation; HAR: Hepatic artery rupture.
In cases of acute bleeding, many therapeutic possibilities are available: endovascular intervention with embolization with or without stenting, surgical intervention for anastomotic revision, aorto-hepatic grafting, HA ligation or emergency/elective retransplantation. In case of HAR, mortality remains very high and currently there is no consensus on the indications for these procedures[26,73,78,80,88]. Boleslawski et al[26] (2013) published the largest series of ruptured post-transplant HAP; they highlighted the efficacy of primary HA ligation on both early and late survival. They reported an HAR incidence of 0.64% (17 patients out of 2649 OLTs from 1997 to 2007). The mean age was 47.9 years (range: 27-65 years; 13 men and 4 women). The median time between transplant and HAR occurrence was 29 d (range: 2-92 d), but the distribution of events was bimodal with only four late HA ruptures occurring after two months[26].
Clinical presentation and diagnosis: In the study by Boleslawski et al[26] (2013), clinical presentation was always sudden hemorrhage: Hemoperitoneum in ten patients, gastrointestinal bleeding in five patients, hematoma in one patient and hemobilia in one patient. The presence of a fungal infection in the arterial wall was confirmed in six patients. Biliary leak was observed in seven patients[26].
Therapeutic management: In the study by Boleslawski et al[26] (2013), immediate treatment included urgent laparotomy (15 patients) with definitive ligation of the HA (10 patients), anastomotic revision (3 patients) and aortohepatic grafting (2 patients). One patient had a percutaneous embolization and one patient died before treatment. Treatment of the associated biliary leak was performed either synchronously or after the first surgery in seven patients. In this series, the early mortality rate was 35% (0-80 d from HAR and 16-172 d from transplantation) because of hemorrhagic relapse or sepsis[26].
Prognosis: Boleslawski et al[26] (2013) also studied the effect of HA ligation on survival. They compared patients with (n = 10) and without (n = 6) HA ligation treatment. Of the 6 patients that received percutaneous embolization or revascularization, only 1 survived beyond 90 d (mortality rate: 83%). The 10 patients with HA ligation survived after postoperative day 90. Additionally, the one- and three-year graft survival rates for patients without HA ligation were 14% and 14%, respectively, vs 80% and 70%, respectively, in patients with HA ligation. The one- and three-year overall survival probabilities were 14% and 14%, respectively, in patients without HA ligation vs 100% and 80%, respectively, in patients with HA ligation[26].
Conclusion: Finally, in this retrospective study, Boleslawski et al[26] (2013) recommended that HA revascularization should be avoided, especially when mycotic pseudoaneurysm is suspected (i.e., if there was a gastrointestinal wound during liver procurement, documented systemic candidiasis prior to HAR, or if HAR occurred several weeks after transplant with associated lesions, such as biliary leak or gastroduodenal perforation). In contrast, HA ligation seems to be a reasonable life-saving option because it prevents hemorrhagic recurrence and should achieve a successful long-term outcome, with or even without retransplantation. Expected biliary complications, such as ischemic cholangitis, following HA ligation could be managed afterward by percutaneous and/or endoscopic interventions[26].
VENOUS COMPLICATIONS
Compared to arterial complications, venous complications are less frequent with an estimated overall incidence of less than 3%[4,5,8,9,62,89-91]. They can be potentially devastating and lead to graft failure, and therefore represent an important source of morbidity and mortality after OLT, especially if they occur in the early post-operative period[9,90,91]. Numerous literature reports have demonstrated that the incidence of venous complications in pediatric transplants is higher than in adult transplants[9,62,92,93]. Venous complications following OLT include: Portal (1%-3%) and caval (< 2%) problems[5,8,9,91]. The etiology underlying most of these involves the anastomosis, including: (1) PVT: < 3% (the most pejorative), portal vein stenosis (PVS): 2%-3%; and (2) caval and hepatic veins with specific complications depending to the type of anastomosis either end to end caval anastomosis: Thrombosis, stenosis (< 2%); or piggyback: Thrombosis, stenosis, kinking < 2%[4,5,8,9,91,94,95]. In the same fashion as HACs, they can be classified into two categories (Table 1): Early (< 1 mo) or late (delayed, i.e., > 1 mo). In the recent years, the literature has been in favor of endovascular intervention management of venous complications, with very good outcomes[8,9,10,62,91].
Portal vein complications
The incidence of portal vein complications (PVCs) following liver transplantation is relatively uncommon, occurring in 1% to 3% of patients[4,5,8,9,89-91,96]. These complications are associated with high morbidity and graft loss[8,9]. An another important fact to mention is that PVCs are more common with split liver and LDLT and also in pediatric transplantation[91,97]. Regarding PVCs, DUS, contrast enhanced ultrasound (CEUS) and contrast-enhanced CT are the usual tools for diagnosis; more recently, magnetic resonance venography using the gadofosveset trisodium agent has been proposed[8,9,98]. Therapeutic PVCs management ranges from thrombectomy and anastomosis revision to retransplantation depending to the delay of occurrence after OLT. Nowadays, except early PVT, endovascular procedures are now considered to be the first line treatment for post-transplant PVCs, and many studies have shown highly successful results[62,93,99,100].
PVT: The incidence of PVT in OLT ranges from 0.3%-2.6%[1,90] (Table 6). From the UCLA experience, Duffy et al[5] (2009) reported a PVT incidence of 2% in more than 4200 patients. However, the incidence of PVT is close to 4% in adult LDLT due to technical difficulties in PV reconstructions, mainly related to a shorter vessel pedicle and limited vessel graft[101]. In LDLT, PVT occurs more frequently in the early period, defined as within 3 mo by Kyoden et al[101] (2008) (73% of cases from Kyoden’s series; median, 58 d; range, 1-68 d).
Table 6.
Portal vein thombosis highlights
| Summary of the clinical characteristics about PVT |
| The incidence of PVT is uncommon and ranges from < 3% following OLT |
| PVT incidence is higher in pediatric transplantation, LDLT and split liver transplantation |
| Early PVT is more frequent than late PVT with a median time to diagnosis of 5 d following OLT (range: 1 to 15 d) |
| The clinical presentation of early PVT ranges from portal hypertension manifestations (abdominal pain, ascites, gastrointestinal bleeding, splenomegaly) to severe allograft dysfunction and multiorgan failure |
| The most common causes leading to PVT are technical errors and anatomic complications such as venous redundancy, kinking and/or stenosis of the anastomosis |
| Risk factors are the presence of portal thrombosis prior OLT, small diameter of the portal vein, previous splenectomy, large portosystemic collaterals and the use of cryopreserved venous conduits for PV reconstruction |
| DUS, CEUS, contrast-enhanced CT, MRI and portography are imaging tools used for a positive diagnosis |
| PVT treatment includes systemic anticoagulation therapy, catheter-based thrombolytic therapy by percutaneous radiological intervention (transhepatic or transjugular access depending of the coagulation state) with or without stent placement to portosystemic shunting (TIPS) to retransplantation in highly unresolvable cases |
| PVT is associated with poor survival without treatment, but with prompt management, outcomes in terms of morbidity and mortality are satisfying |
DUS: Doppler ultrasound; PVT: Portal vein thombosis; OLT: Orthotopic liver transplantation; LDLT: Living donor liver transplantation; CEUS: Contrast enhanced ultrasound; MRI: Magnetic resonance imaging; CT: Computed tomography; TIPS: Transjugular intrahepatic portosystemic shunt.
The clinical presentation depends on the time the thrombosis occurs. When it occurs early, severe acute liver insufficiency or graft failure predominates. If it occurs late, clinical symptoms depend of the portocaval collateral circulation existence. Portal hypertension manifestations including upper gastrointestinal bleeding due to esophagogastric varices and ascites are the most frequent clinical presentations. In contrast, liver failure is rare[30,90,96]. Langnas et al[30] (1991) reported a mean diagnosis time of 5 d following OLT (range: 1 to 15 d), which was confirmed by Kyoden et al[101] (2008), who reported that PVT occurred more frequently in the early period, i.e., 8/11 cases (72%).
The most common causes of PVT are technical errors related to venous redundancy and kinking and/or stenosis of the anastomosis[90]. Other reported risk factors include prior surgery on the portal or splanchnic venous system or a pre-transplant portal thrombosis requiring thrombectomy during the operation, a small diameter of the portal vein (< 5 mm), previous splenectomy, hypoplastic portal vein, large portosystemic collaterals and the use of venous conduits for portal vein reconstruction[90,96]. Specific risk factors found in adult LDLT are: Small PV size, liver graft position and the type of venous conduits used to connect the PV of the donor to the recipient such as a cryo-preserved vein, the use of which is discouraged by Kyoden et al[101] (2008)[30,90,96,102-105].
DUS should be the first imaging tool used and is easily employed to evaluate vascular patency. It allows, in most cases, for an immediate non-invasive diagnosis and provides a rapid evaluation of vascular flow patency. DUS protocols vary widely worldwide among liver transplant centers, but most teams recommend performing DUS daily (some authors recommend twice daily) in the immediate post-operative period until POD 5 or in the presence of abnormalities of liver function tests or a clinical suspicion of the diagnosis[106-109]. Recently, other authors have proposed the use of CEUS to avoid frequent false-positive results after DUS[108,110]. CEUS may help in assessing the severity of portal insufficiency, based on evidence of parenchymal perfusion status. It allows to show small thrombus in a peripheral portal branch[108,110]. In a retrospective evaluation of 23 patients, CEUS was used as an additional diagnostic method to DUS, CT and magnetic resonance imaging[110]. The authors reported new clinically relevant findings in 52% of cases, such as PVT confirmed during surgery or other radiological results.
Therapeutic options for PVT range from systemic anticoagulation to catheter-based thrombolytic therapy, to surgical revision until retransplantation. The three percutaneous options presented in the literature include transhepatic portal vein angioplasty (with or without stent placement), percutaneous thrombolytic therapy via transjugular intrahepatic portosystemic shunt (TIPS) creation and the transplenic approach[111-114]. In practice, three different therapeutic situations that require specific care may be distinguished: (1) complete PVT within the first 48 h post-OLT; (2) PVT (complete or partial) at 48 h and not more than at 30 d (early PVT); and (3) after more than at 30 d (late PVT).
Early complete PVT within the first 72 h post-LT: In a patient who shows signs of multiorgan failure, surgical revision of the anastomosis is mandatory. In the presence of kinking or twisting that caused the thrombosis, anastomotic revision and systemic anticoagulation are sufficient to resolve this condition. If this procedure is unsuccessful in obtaining satisfactory portal transplant revascularization, emergent retransplantation should be indicated.
Early PVT (PVT > 72 h and < 30 d): Independently of PVT presentation (partial or complete), non-surgical treatment should be reasonably attempted. The most frequent procedure is percutaneous thrombolysis associated with stent placement[111,113,115-117]. Cherukuri et al[113] (1998) reported the necessity that thrombolytic doses should be relatively low and maintained for only a few hours for efficacy and safety Concerning the modality for stent placement, two different possibilities are described in the literature: The classical percutaneous transhepatic approach and the transjugular approach. It is obvious that the latter should be preferred in patients with a coagulopathy or ascites, to minimize the risk of bleeding from transhepatic puncture[118-120]. This method has already been used in transplanted patients in the presence of decompensated cirrhosis, veno-occlusive disease or portal hypertension. The success rate with different endovascular methods ranges from 68%-100% and the mortality and morbidity rates are between 0% and 11%, respectively[121].
Late PVT (PVT > 30 d): Two clinical presentations should be distinguished. Late PVT involving or not the superior mesenteric vein and normal liver function tests develop de novo hepato-portal collaterals and cavernoma formation. In these cases, observation may be justified, because of the appropriate venous inflow from the splenic circulation[19]; Late PVT with symptomatic manifestations such as acute gastroesophageal bleeding or ascites that should be treated with percutaneous or transjugular transhepatic procedures. Regarding the transjugular experience, Lodhia et al[122] (2010) reported 3 cases of acute PVT occurring years following LT treated with an approach combining a TIPS and mechanical thrombectomy. To reduce the risk of periprocedural pulmonary emboli, the authors performed direct PV thrombolysis prior to placing the TIPS stent in order to allow time for clot dissolution[122]. Another possibility reported by Guckelberger et al[123] (1999) was described for cases of late PVT with complete recanalization using a systemic low dose recombinant tissue plasminogen activator (rt-PA). The authors reported their experience with late PVT 45 mo after LT and justified the use of systemic low dose rt-PA lysis continuously for 10 d, along with 25000 IU heparin per day to adjust the partial thromboplastin time to favorable administration[123]. In fact, although, streptokinase (SK) and urokinase (UK) have been shown to be largely effective for thrombolytic therapies, both are characterized by limited thrombolytic potencies and major clinical disadvantages compared to rt-PA[124]. While streptokinase has a high antigenicity, both SK and UK, unlike rt-PA, lack fibrin-specific action which results in systemic consumption of plasminogen and decreased thrombolytic efficacy. Furthermore, it may increase bleeding complications[124].
PVT is associated with poor survival without treatment, but in cases of prompt diagnosis and adequate management, the literature shows good results in terms of morbidity and mortality.
To conclude, PVT is a rare but serious complication when it occurs in the early post-operative period. Diagnosis is mandatory as soon as possible by DUS screening protocols or with suspicious clinico-biological findings including abnormal abdominal pain and/or elevated liver enzymes and unexpected decrease PT. Surgical thrombectomy is traditionally required in the early post-operative period, but percutaneous radiological intervention has progressively become the best therapeutic option with good outcomes and safety.
PVS
The true incidence of PVS after LT is not really known, and the only data reported in the literature concerning the incidence of venous complications is < 3%[91] (Table 7).
Table 7.
Portal vein stenosis highlights
| Summary of the clinical characteristics about PVS |
| The true incidence of PVS is not really known, but is thought to be < 3% |
| The major complication of PVS is the evolution to PVT if not treated |
| The majority of patients with PVS are asymptomatic and the diagnosis of stenosis is an incidental finding detected on routine DUS screening |
| Risk factors of PVS are almost exclusively represented by technical errors, particularly if a tapered anastomosis is required in the case of a vessel size mismatch between donor and recipient |
| Pre-OLT radiotherapy is another major predisposing factor of PVS |
| DUS with the finding of a stenosis ratio > 50% or a portal velocity ratio > 3:1 defines PVS. Contrast-enhanced CT and portography are used to confirm the diagnosis |
| If PVS is asymptomatic, no therapeutic intervention with close surveillance is possible, but anticoagulation therapy is recommended |
| In patients with clinical manifestations, percutaneous radiological intervention is the method of choice by transhepatic or transjugular access to perform angioplasty with our without stent placement; this prevents recurrence with a high rate of success and low rate of complications |
PVT: Portal vein thombosis; PVS: Portal vein stenosis; DUS: Doppler ultrasound; OLT: Orthotopic liver transplantation; CT: Computed tomography.
When PVS occurs, it can be present with graft failure or the complication of portal hypertension[125]. In practice, the majority of patients with PVS are asymptomatic and the diagnosis of stenosis is an incidental finding detected on routine screening ultrasound. Conversely, when the patients are symptomatic, they may present with signs of portal hypertension, which include upper gastrointestinal tract bleeding from gastroesophageal varices, ascites and splenomegaly. Abnormal liver function tests are not constant, and are therefore not a reliable sign for PVS diagnosis[91].
Regarding the risk factors of PVS, similar to PVT, it is well-established that the major concern is surgical technical errors[91]. Classically, the portal anastomosis is end-to-end and is usually simple in OLT, though a tapered anastomosis may be required when a significant size mismatch exists between the recipient and the donor, which constitutes a risk factor of stenosis. It explains in part why the pediatric population represents a population highly at risk to PVS[91]. In most cases, early PVS is the consequence of a surgical mistake due to technical difficulties in the anastomosis and could evolve into an early thrombosis if not treated promptly. In contrast, it is assumed that late PVS is secondary to fibrosis or intimal hyperplasia[126]. Schneider et al[125] (2011) reported some cases of PVS after neoadjuvant radiotherapy for cholangiocarcinoma, and highlighted radiotherapy as a predisposing factor in venous complications; 21% of the patients who received a LT following the Mayo protocol for cholangiocarcinoma developed PVCs[125,127].
Concerning a positive diagnosis, although DUS is the first screening morphological tool to use, its definition is still controversial because of the lack of definite and objective criteria. Moreover, DUS is sensitive for PVS but it is not specific. The PVS criteria for diagnosis include portal caliber size, velocities at the anastomotic site, as well as the preanastomotic and postanastomotic gradients. Recently Huang et al[107] (2010) reported a formula that can estimate the portal stenosis ratio in LDLT: They calculated the portal stenosis ratio (SR) = PRE-AS/PRE > 50% [anastomotic stenosis (AS); pre-stenotic stenosis (PRE)]; significant PVS was defined as a PVS with an SR > 50%. The portal velocity ratio (VR) was also calculated between AS and PRE, such that > 3:1 is defined as a significant VR value correlating with the SR evaluation. If these are confirmed, the patient should undergo contrast-enhanced CT to confirm the diagnosis[107]. Some authors consider the pressure gradient between the pre- and post-stenosis site. Wei et al[126] (2009) considered a gradient of > 5 mmHg to initiate treatment, while Shibata et al[128] (2005) used a significant gradient of > 3 mmHg. Other authors did not measure gradients if the stenosis was noted to be greater than 75% of the main portal vein diameter.
Surgical treatment, including anastomotic revision or retransplantation, is usually preferred for early portal inflow abnormalities following OLT[129]. In cases of asymptomatic patients with normal hepatic function test results, PVS may be solely observed with no therapeutic intervention[102]. In these particular cases, and in view of the possible evolution to PVT, it is reasonable to screen regularly by DUS to check for the patency of the PV. Moreover, in this condition, the use of anticoagulant therapy is still discussed and there is no international consensus or recommendation on this issue. In patients with clinical manifestations and radiological confirmation of significant stenosis, therapeutic intervention is mandatory to avoid graft loss, retransplantation and mortality. Interventional radiology has become widely recognized as the first choice for treatment for PVS after LT[103-105,111,125,126,128-132]. Regarding PVS management, it is possible to use the transhepatic access or transjugular access[133], but most authors choose a transhepatic approach, usually from the right side. Shibata et al[128] (2005) reported that a single balloon dilatation was sufficient to maintain patency in 77.7% of patients, with a mean follow-up of 24.8 mo. In some series, stent placement associated with PTA was used to prevent recurrence. However, problems related to stent placement have been reported by Zajko et al[130] (1994), i.e., a thrombus that developed around the stent that could not be lysed, requiring retransplantation. However, Ko et al[129] (2007) reported on their experience in PVS management by percutaneous transhepatic primary stent placement after LDLT. In this series, technical and clinical success was obtained in 77.8% by using this method with a complication rate of 33% (including hemoperitoneum caused by blood oozing from the transhepatic tract and intrahepatic pseudoaneurysms)[129]. Finally, regarding the recurrence rate, this ranges between 0%-100%. Shibata et al[128] (2005) reported the most important series in the literature where the recurrence rate was 28.6%. Some authors recommend the use of anticoagulant therapy for the prevention of recurrent PVT[134]. Recently, Sanada et al[134] (2010) concluded that the use of three anticoagulant therapies, i.e., low-molecular-weight heparin, warfarin and aspirin, significantly reduced the recurrence of thrombosis with a median follow-up of three months[134]. Additionally, some authors have coupled endovascular treatment with surgical PV access[106].
To conclude, PVS represents an uncommon venous complication following OLT. This condition is more specific to pediatric LT and LDLT. As described earlier, a DUS screening protocol is an important diagnostic tool to help the clinician because the majority of asymptomatic cases can progress until PVT if not promptly treated, with negative effects on the prognosis of the graft and ultimately patient survival. Currently, it is obvious that percutaneous transhepatic radiological intervention with stent placement is the method of choice to address this complication with a high rate of success and a low rate of recurrence and/or complications.
Caval vein complications
Currently, transplant outflow obstruction by kinking, stenosis or thrombosis of the inferior vena cava (IVC) or hepatic vein, especially in LDLT, are relatively uncommon complications following liver transplantation with an reported incidence of less than 3%[94,95] (Table 8 and Figure 5).
Table 8.
Caval anastomosis complication highlights
| Summary of the clinical characteristics about CAC |
| The incidence of CAC is not known and is thought to be less than 3% |
| CAC is represented by stenosis, thrombosis and kinking depending on the type of caval anastomosis (cava resection or PB) |
| Clinical presentation of CAC ranges from lower limb edema, hepatomegaly, ascites, pleural effusions, Budd-Chiari syndrome, liver and renal failure, and hypotension, leading to allograft loss and even death |
| The main risk factor is a technical error in the creation of the anastomosis, which leads to kinking stenosis and thrombosis |
| Modified-PB with the three-hepatic vein seems to offer better outcomes because it has been demonstrated to be an efficient and safe method |
| Diagnosis tools include DUS, contrast-enhanced CT and cavography |
| Percutaneous radiological intervention is the method of choice via a transjugular approach or transhepatic approach if the anastomosis cannot be catheterized |
| It includes angioplasty by balloon dilatation and recurrences should be prevented by stent placement |
CAC: Caval anastomosis complication; DUS: Doppler ultrasound; CT: Computed tomography; PB: Piggyback.
Figure 5.

Contrast-enhanced-multidetector-row computed tomography-scan showing median and left thromboses hepatic veins following orthotopic liver transplantation (arrow).
Clinical presentation ranges from lower limb edema, hepatomegaly, ascites, pleural effusions, Budd-Chiari syndrome, liver and renal failure to hypotension leading to allograft loss and multiorgan failure[4,89,135].
The main risk factor leading to caval anastomosis complications (CACs) is represented by technical errors in the connection of caval anastomoses, which lead to kinking or thrombosis in the early post-operative course. In the late post-operative period, chronic stenosis in the anastomotic area is the result of fibrosis, hyperplasia and/or extrinsic compression from the enlarged liver graft[2,136,137].
Diagnosis should be achieved by DUS, contrast-enhanced CT, and finally by cavography which allows for providing treatment.
Many techniques for caval anastomosis connection can avoid these complications, such as piggyback (PB) and subsequently modified-PB, first described by Starzl et al[138] (1968). The method described by Starzl et al[138] (1968) consists of a complete resection of the recipient IVC and interposition of the donor intrahepatic part of the vena cava with two end-to-end anastomoses[138-144]. The preservation of the recipient IVC with the PB technique has been associated with an increased risk of suprahepatic IVC thrombosis or stenosis, leading to acute or chronic Budd-Chiari syndrome in 0% to 1.6%, venous congestion of the liver allograft in 1%, and with an increased incidence of post-transplant ascites[89,135]. To avoid such complications, techniques for optimizing outflow with the piggyback technique have been described; the main of these in undoubtfully the width of the caval anastomosis, while other authors have reported methods using either the two-vein or the three-vein technique for anastomosis with a low rate of CACs[89,94,135,145-149]. Finally, several studies have demonstrated the superiority of modified-PB with the three-hepatic vein technique, which should be routinely used in OLT because it is safe and efficient and involves few surgical complications[89,94,143]. Hepatic venous stenosis is specific to LDLT with an incidence of 2% to 4%, because of the different techniques of donor graft outflow venoplasty, leading to Budd-Chiari syndrome or outflow block syndrome after LDLT[150].
Therapeutic management of CACs depends on the time of the presentation and the delay following OLT. In the case of severe allograft dysfunction or multiorgan failure, retransplantation is always indicated. Beyond this particular situation, percutaneous radiological intervention is the method of choice, where mortality after interventional transplant salvage procedure is 11.1% as compared with 41.6% mortality for those patients managed by retransplantation[121,137]. Treatment can be performed by transjugular approach, but percutaneous transhepatic access may be necessary when the anastomosis cannot be catheterized from the jugular access. Angioplasty by balloon dilatation can restore anastomotic patency in almost 100% of cases, but recidive of stenosis is frequent and repeat angioplasties may be applied[137]. PTA associated with stent placement may be the better solution with a high rate of success ranging from 73% to 100% in the literature; this technique is safe and apparently durable[121,130,136,137,151-157].
To conclude, the incidence of CACs is very low, and particular attention should be paid to the caval anastomosis connection. Currently, modified-PB using the three-hepatic vein technique seems to show better outcomes. As with other VCs, prompt diagnosis and management are required if the patient is clinically symptomatic. The percutaneous endovascular method should be attempted to rescue the outflow patency, reserving surgical revision in unresolvable cases and ultimately retransplantation in patients presenting multiorgan failure.
CONCLUSION
VCs continue to be a major problem following transplantation with a relatively frequent incidence (7%). They carry a high rate of morbidity and mortality, especially if they occur in the immediate post-operative period (first month) and if diagnosed late. The only solution to reduce their gravity is to prevent it by controlling risk factors and, if this is not possible, to diagnose them as early as can be, even in asymptomatic or paucisymptomatic patients. Many transplant teams worldwide advocate the routine use of complementary explorations such as DUS and, if in doubt, a contrast-enhanced CT scan or classical arteriography, which is the reference. Currently, if recognized promptly, and if there is no graft or multiorgan failure, endovascular treatment should be attempted first if a technical plateau is available, because this has demonstrated efficacious and safe outcomes. Conversely, if there are severe liver repercussions, the most efficient therapeutic procedure is an emergency retransplant which shows better outcomes in terms of efficacy and survival, but the organ shortage dramatically limits this therapeutic option.
ACKNOWLEDGMENTS
We thank Emmanuel Schaeffer and Pr. Jocelyne Wuibout for the proofreading and the correction of this manuscript.
Footnotes
P- Reviewer: Kambadakone A S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
Conflict-of-interest statement: Authors declare no conflict of interests for this article.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: June 6, 2015
First decision: July 25, 2015
Article in press: December 21, 2015
References
- 1.Khalaf H. Vascular complications after deceased and living donor liver transplantation: a single-center experience. Transplant Proc. 2010;42:865–870. doi: 10.1016/j.transproceed.2010.02.037. [DOI] [PubMed] [Google Scholar]
- 2.Wozney P, Zajko AB, Bron KM, Point S, Starzl TE. Vascular complications after liver transplantation: a 5-year experience. AJR Am J Roentgenol. 1986;147:657–663. doi: 10.2214/ajr.147.4.657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Karatzas T, Lykaki-Karatzas E, Webb M, Nery J, Tsaroucha A, Demirbas A, Khan F, Ciancio G, Montalvo B, Reddy R, et al. Vascular complications, treatment, and outcome following orthotopic liver transplantation. Transplant Proc. 1997;29:2853–2855. doi: 10.1016/s0041-1345(97)00706-9. [DOI] [PubMed] [Google Scholar]
- 4.Pawlak J, Grodzicki M, Leowska E, Małkowski P, Michałowicz B, Nyckowski P, Rowiński O, Pacho R, Zieniewicz K, Andrzejewska M, et al. Vascular complications after liver transplantation. Transplant Proc. 2003;35:2313–2315. doi: 10.1016/s0041-1345(03)00836-4. [DOI] [PubMed] [Google Scholar]
- 5.Duffy JP, Hong JC, Farmer DG, Ghobrial RM, Yersiz H, Hiatt JR, Busuttil RW. Vascular complications of orthotopic liver transplantation: experience in more than 4,200 patients. J Am Coll Surg. 2009;208:896–903; discussion 903-905. doi: 10.1016/j.jamcollsurg.2008.12.032. [DOI] [PubMed] [Google Scholar]
- 6.Bonnet S, Sauvanet A, Bruno O, Sommacale D, Francoz C, Dondero F, Durand F, Belghiti J. Long-term survival after portal vein arterialization for portal vein thrombosis in orthotopic liver transplantation. Gastroenterol Clin Biol. 2010;34:23–28. doi: 10.1016/j.gcb.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 7.Schwope RB, Margolis DJ, Raman SS, Kadell BM. Portal vein aneurysms: a case series with literature review. J Radiol Case Rep. 2010;4:28–38. doi: 10.3941/jrcr.v4i6.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pérez-Saborido B, Pacheco-Sánchez D, Barrera-Rebollo A, Asensio-Díaz E, Pinto-Fuentes P, Sarmentero-Prieto JC, Rodríguez-Vielba P, Martínez-Díaz R, Gonzalo-Martín M, Rodríguez M, et al. Incidence, management, and results of vascular complications after liver transplantation. Transplant Proc. 2011;43:749–750. doi: 10.1016/j.transproceed.2011.01.104. [DOI] [PubMed] [Google Scholar]
- 9.Steinbrück K, Enne M, Fernandes R, Martinho JM, Balbi E, Agoglia L, Roma J, Pacheco-Moreira LF. Vascular complications after living donor liver transplantation: a Brazilian, single-center experience. Transplant Proc. 2011;43:196–198. doi: 10.1016/j.transproceed.2010.12.007. [DOI] [PubMed] [Google Scholar]
- 10.Hejazi Kenari SK, Zimmerman A, Eslami M, F Saidi R. Current state of art management for vascular complications after liver transplantation. Middle East J Dig Dis. 2014;6:121–130. [PMC free article] [PubMed] [Google Scholar]
- 11.Figueras J, Busquets J, Dominguez J, Sancho C, Casanovas-Taltavull T, Rafecas A, Fabregat J, Torras J, Jaurrieta E. Intra-arterial thrombolysis in the treatment of acute hepatic artery thrombosis after liver transplantation. Transplantation. 1995;59:1356–1357. [PubMed] [Google Scholar]
- 12.Boyvat F, Aytekin C, Firat A, Harman A, Karakayali H, Haberal M. Diagnostic and therapeutic management of hepatic artery thrombosis and stenosis after orthotopic and heterotopic liver transplantation. Transplant Proc. 2003;35:2791–2795. doi: 10.1016/j.transproceed.2003.09.086. [DOI] [PubMed] [Google Scholar]
- 13.Stange BJ, Glanemann M, Nuessler NC, Settmacher U, Steinmüller T, Neuhaus P. Hepatic artery thrombosis after adult liver transplantation. Liver Transpl. 2003;9:612–620. doi: 10.1053/jlts.2003.50098. [DOI] [PubMed] [Google Scholar]
- 14.Zhou J, Fan J, Wang JH, Wu ZQ, Qiu SJ, Shen YH, Shi YH, Huang XW, Wang Z, Tang ZY, et al. Continuous transcatheter arterial thrombolysis for early hepatic artery thrombosis after liver transplantation. Transplant Proc. 2005;37:4426–4429. doi: 10.1016/j.transproceed.2005.10.113. [DOI] [PubMed] [Google Scholar]
- 15.Li ZW, Wang MQ, Zhou NX, Liu Z, Huang ZQ. Interventional treatment of acute hepatic artery occlusion after liver transplantation. Hepatobiliary Pancreat Dis Int. 2007;6:474–478. [PubMed] [Google Scholar]
- 16.Saad WE, Davies MG, Saad NE, Westesson KE, Patel NC, Sahler LG, Lee DE, Kitanosono T, Sasson T, Waldman DL. Catheter thrombolysis of thrombosed hepatic arteries in liver transplant recipients: predictors of success and role of thrombolysis. Vasc Endovascular Surg. 2007;41:19–26. doi: 10.1177/1538574406296210. [DOI] [PubMed] [Google Scholar]
- 17.Singhal A, Stokes K, Sebastian A, Wright HI, Kohli V. Endovascular treatment of hepatic artery thrombosis following liver transplantation. Transpl Int. 2010;23:245–256. doi: 10.1111/j.1432-2277.2009.01037.x. [DOI] [PubMed] [Google Scholar]
- 18.Chen J, Weinstein J, Black S, Spain J, Brady PS, Dowell JD. Surgical and endovascular treatment of hepatic arterial complications following liver transplant. Clin Transplant. 2014;28:1305–1312. doi: 10.1111/ctr.12431. [DOI] [PubMed] [Google Scholar]
- 19.Porrett PM, Hsu J, Shaked A. Late surgical complications following liver transplantation. Liver Transpl. 2009;15 Suppl 2:S12–S18. doi: 10.1002/lt.21893. [DOI] [PubMed] [Google Scholar]
- 20.Abdelaziz O, Hosny K, Amin A, Emadeldin S, Uemoto S, Mostafa M. Endovascular management of early hepatic artery thrombosis after living donor liver transplantation. Transpl Int. 2012;25:847–856. doi: 10.1111/j.1432-2277.2012.01509.x. [DOI] [PubMed] [Google Scholar]
- 21.Gordon G, Carmody IC. In: Transplantation of the liver. 2nd ed. Philadelphia: 2005. pp. 953–961. [Google Scholar]
- 22.Moore FA, Moore EE, Seagraves A. Nonresectional management of major hepatic trauma. An evolving concept. Am J Surg. 1985;150:725–729. doi: 10.1016/0002-9610(85)90417-9. [DOI] [PubMed] [Google Scholar]
- 23.Crossin JD, Muradali D, Wilson SR. US of liver transplants: normal and abnormal. Radiographics. 2003;23:1093–1114. doi: 10.1148/rg.235035031. [DOI] [PubMed] [Google Scholar]
- 24.Panaro F, Gallix B, Bouyabrine H, Ramos J, Addeo P, Testa G, Carabalona JP, Pageaux G, Domergue J, Navarro F. Liver transplantation and spontaneous neovascularization after arterial thrombosis: “the neovascularized liver”. Transpl Int. 2011;24:949–957. doi: 10.1111/j.1432-2277.2011.01293.x. [DOI] [PubMed] [Google Scholar]
- 25.Pastacaldi S, Teixeira R, Montalto P, Rolles K, Burroughs AK. Hepatic artery thrombosis after orthotopic liver transplantation: a review of nonsurgical causes. Liver Transpl. 2001;7:75–81. doi: 10.1053/jlts.2001.22040. [DOI] [PubMed] [Google Scholar]
- 26.Boleslawski E, Bouras AF, Truant S, Liddo G, Herrero A, Badic B, Audet M, Altieri M, Laurent A, Declerck N, et al. Hepatic artery ligation for arterial rupture following liver transplantation: a reasonable option. Am J Transplant. 2013;13:1055–1062. doi: 10.1111/ajt.12135. [DOI] [PubMed] [Google Scholar]
- 27.Silva MA, Jambulingam PS, Gunson BK, Mayer D, Buckels JA, Mirza DF, Bramhall SR. Hepatic artery thrombosis following orthotopic liver transplantation: a 10-year experience from a single centre in the United Kingdom. Liver Transpl. 2006;12:146–151. doi: 10.1002/lt.20566. [DOI] [PubMed] [Google Scholar]
- 28.Bekker J, Ploem S, de Jong KP. Early hepatic artery thrombosis after liver transplantation: a systematic review of the incidence, outcome and risk factors. Am J Transplant. 2009;9:746–757. doi: 10.1111/j.1600-6143.2008.02541.x. [DOI] [PubMed] [Google Scholar]
- 29.Tzakis AG, Gordon RD, Shaw BW, Iwatsuki S, Starzl TE. Clinical presentation of hepatic artery thrombosis after liver transplantation in the cyclosporine era. Transplantation. 1985;40:667–671. doi: 10.1097/00007890-198512000-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Langnas AN, Marujo W, Stratta RJ, Wood RP, Shaw BW. Vascular complications after orthotopic liver transplantation. Am J Surg. 1991;161:76–82; discussion 82-83. doi: 10.1016/0002-9610(91)90364-j. [DOI] [PubMed] [Google Scholar]
- 31.Drazan K, Shaked A, Olthoff KM, Imagawa D, Jurim O, Kiai K, Shackelton C, Busuttil R. Etiology and management of symptomatic adult hepatic artery thrombosis after orthotopic liver transplantation (OLT) Am Surg. 1996;62:237–240. [PubMed] [Google Scholar]
- 32.Pinna AD, Smith CV, Furukawa H, Starzl TE, Fung JJ. Urgent revascularization of liver allografts after early hepatic artery thrombosis. Transplantation. 1996;62:1584–1587. doi: 10.1097/00007890-199612150-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sheiner PA, Varma CV, Guarrera JV, Cooper J, Garatti M, Emre S, Guy SR, Schwartz ME, Miller CM. Selective revascularization of hepatic artery thromboses after liver transplantation improves patient and graft survival. Transplantation. 1997;64:1295–1299. doi: 10.1097/00007890-199711150-00011. [DOI] [PubMed] [Google Scholar]
- 34.Torras J, Lladó L, Figueras J, Ramos E, Lama C, Fabregat J, Rafecas A, Escalante E, Dominguez J, Sancho C, et al. Diagnostic and therapeutic management of hepatic artery thrombosis after liver transplantation. Transplant Proc. 1999;31:2405. doi: 10.1016/s0041-1345(99)00403-0. [DOI] [PubMed] [Google Scholar]
- 35.Pawlak J, Wróblewski T, Małkowski P, Nyckowski P, Zieniewicz K, Grzelak I, Alsharabi A, Michałowicz B, Krawczyk M, Karwowski A. Vascular complications related to liver transplantation. Transplant Proc. 2000;32:1426–1428. doi: 10.1016/s0041-1345(00)01281-1. [DOI] [PubMed] [Google Scholar]
- 36.Bhattacharjya S, Gunson BK, Mirza DF, Mayer DA, Buckels JA, McMaster P, Neuberger JM. Delayed hepatic artery thrombosis in adult orthotopic liver transplantation-a 12-year experience. Transplantation. 2001;71:1592–1596. doi: 10.1097/00007890-200106150-00018. [DOI] [PubMed] [Google Scholar]
- 37.Jain A, Costa G, Marsh W, Fontes P, Devera M, Mazariegos G, Reyes J, Patel K, Mohanka R, Gadomski M, et al. Thrombotic and nonthrombotic hepatic artery complications in adults and children following primary liver transplantation with long-term follow-up in 1000 consecutive patients. Transpl Int. 2006;19:27–37. doi: 10.1111/j.1432-2277.2005.00224.x. [DOI] [PubMed] [Google Scholar]
- 38.Pareja E, Cortes M, Navarro R, Sanjuan F, López R, Mir J. Vascular complications after orthotopic liver transplantation: hepatic artery thrombosis. Transplant Proc. 2010;42:2970–2972. doi: 10.1016/j.transproceed.2010.07.063. [DOI] [PubMed] [Google Scholar]
- 39.Fouzas I, Sklavos A, Bismpa K, Paxiadakis I, Antoniadis N, Giakoustidis D, Katsiki E, Tatsou N, Mouloudi E, Karapanagiotou A, et al. Hepatic artery thrombosis after orthotopic liver transplantation: 3 patients with collateral formation and conservative treatment. Transplant Proc. 2012;44:2741–2744. doi: 10.1016/j.transproceed.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 40.Marín-Gómez LM, Bernal-Bellido C, Alamo-Martínez JM, Porras-López FM, Suárez-Artacho G, Serrano-Diaz-Canedo J, Padillo-Ruiz J, Gómez-Bravo MA. Intraoperative hepatic artery blood flow predicts early hepatic artery thrombosis after liver transplantation. Transplant Proc. 2012;44:2078–2081. doi: 10.1016/j.transproceed.2012.07.077. [DOI] [PubMed] [Google Scholar]
- 41.Unal B, Gonultas F, Aydin C, Otan E, Kayaalp C, Yilmaz S. Hepatic artery thrombosis-related risk factors after living donor liver transplantation: single-center experience from Turkey. Transplant Proc. 2013;45:974–977. doi: 10.1016/j.transproceed.2013.02.070. [DOI] [PubMed] [Google Scholar]
- 42.Gunsar F, Rolando N, Pastacaldi S, Patch D, Raimondo ML, Davidson B, Rolles K, Burroughs AK. Late hepatic artery thrombosis after orthotopic liver transplantation. Liver Transpl. 2003;9:605–611. doi: 10.1053/jlts.2003.50057. [DOI] [PubMed] [Google Scholar]
- 43.Margarit C, Hidalgo E, Lázaro JL, Murio E, Charco R, Balsells J. Biliary complications secondary to late hepatic artery thrombosis in adult liver transplant patients. Transpl Int. 1998;11 Suppl 1:S251–S254. doi: 10.1007/s001470050472. [DOI] [PubMed] [Google Scholar]
- 44.Sakamoto Y, Harihara Y, Nakatsuka T, Kawarasaki H, Takayama T, Kubota K, Kimura W, Kita Y, Tanaka H, Ito M, et al. Rescue of liver grafts from hepatic artery occlusion in living-related liver transplantation. Br J Surg. 1999;86:886–889. doi: 10.1046/j.1365-2168.1999.01166.x. [DOI] [PubMed] [Google Scholar]
- 45.Oh CK, Pelletier SJ, Sawyer RG, Dacus AR, McCullough CS, Pruett TL, Sanfey HA. Uni- and multi-variate analysis of risk factors for early and late hepatic artery thrombosis after liver transplantation. Transplantation. 2001;71:767–772. doi: 10.1097/00007890-200103270-00014. [DOI] [PubMed] [Google Scholar]
- 46.Pungpapong S, Manzarbeitia C, Ortiz J, Reich DJ, Araya V, Rothstein KD, Muñoz SJ. Cigarette smoking is associated with an increased incidence of vascular complications after liver transplantation. Liver Transpl. 2002;8:582–587. doi: 10.1053/jlts.2002.34150. [DOI] [PubMed] [Google Scholar]
- 47.Jiang XZ, Yan LN, Li B, Zhao JC, Wang WT, Li FG, Wen TF, Ma YK, Zeng Y, Xu MQ, et al. Arterial complications after living-related liver transplantation: single-center experience from West China. Transplant Proc. 2008;40:1525–1528. doi: 10.1016/j.transproceed.2007.11.078. [DOI] [PubMed] [Google Scholar]
- 48.Panaro F, Ramos J, Gallix B, Mercier G, Herrero A, Niampa H, Pageaux GP, Navarro F. Hepatic artery complications following liver transplantation. Does preoperative chemoembolization impact the postoperative course? Clin Transplant. 2014;28:598–605. doi: 10.1111/ctr.12358. [DOI] [PubMed] [Google Scholar]
- 49.Vorwerk D, Günther RW, Klever P, Riesener KP, Schumpelick V. Angioplasty and stent placement for treatment of hepatic artery thrombosis following liver transplantation. J Vasc Interv Radiol. 1994;5:309–311; discussion 312-314. doi: 10.1016/s1051-0443(94)71489-5. [DOI] [PubMed] [Google Scholar]
- 50.Bjerkvik S, Vatne K, Mathisen O, Søreide O. Percutaneous revascularization of postoperative hepatic artery thrombosis in a liver transplant. Transplantation. 1995;59:1746–1748. doi: 10.1097/00007890-199506270-00021. [DOI] [PubMed] [Google Scholar]
- 51.Cotroneo AR, Di Stasi C, Cina A, De Gaetano AM, Evangelisti R, Paloni F, Marano G. Stent placement in four patients with hepatic artery stenosis or thrombosis after liver transplantation. J Vasc Interv Radiol. 2002;13:619–623. doi: 10.1016/s1051-0443(07)61657-1. [DOI] [PubMed] [Google Scholar]
- 52.Saad WE, Davies MG, Sahler L, Lee DE, Patel NC, Kitanosono T, Sasson T, Waldman DL. Hepatic artery stenosis in liver transplant recipients: primary treatment with percutaneous transluminal angioplasty. J Vasc Interv Radiol. 2005;16:795–805. doi: 10.1097/01.RVI.0000156441.12230.13. [DOI] [PubMed] [Google Scholar]
- 53.da Silva RF, Raphe R, Felício HC, Rocha MF, Duca WJ, Arroyo PC, Palini GL, Vasquez AM, Miquelin DG, Reis LF, et al. Prevalence, treatment, and outcomes of the hepatic artery stenosis after liver transplantation. Transplant Proc. 2008;40:805–807. doi: 10.1016/j.transproceed.2008.02.041. [DOI] [PubMed] [Google Scholar]
- 54.Hamby BA, Ramirez DE, Loss GE, Bazan HA, Smith TA, Bluth E, Sternbergh WC. Endovascular treatment of hepatic artery stenosis after liver transplantation. J Vasc Surg. 2013;57:1067–1072. doi: 10.1016/j.jvs.2012.10.086. [DOI] [PubMed] [Google Scholar]
- 55.Rostambeigi N, Hunter D, Duval S, Chinnakotla S, Golzarian J. Stent placement versus angioplasty for hepatic artery stenosis after liver transplant: a meta-analysis of case series. Eur Radiol. 2013;23:1323–1334. doi: 10.1007/s00330-012-2730-9. [DOI] [PubMed] [Google Scholar]
- 56.Sommacale D, Aoyagi T, Dondero F, Sibert A, Bruno O, Fteriche S, Francoz C, Durand F, Belghiti J. Repeat endovascular treatment of recurring hepatic artery stenoses in orthotopic liver transplantation. Transpl Int. 2013;26:608–615. doi: 10.1111/tri.12089. [DOI] [PubMed] [Google Scholar]
- 57.Abbasoglu O, Levy MF, Vodapally MS, Goldstein RM, Husberg BS, Gonwa TA, Klintmalm GB. Hepatic artery stenosis after liver transplantation--incidence, presentation, treatment, and long term outcome. Transplantation. 1997;63:250–255. doi: 10.1097/00007890-199701270-00013. [DOI] [PubMed] [Google Scholar]
- 58.Sabri SS, Saad WE, Schmitt TM, Turba UC, Kumer SC, Park AW, Matsumoto AH, Angle JF. Endovascular therapy for hepatic artery stenosis and thrombosis following liver transplantation. Vasc Endovascular Surg. 2011;45:447–452. doi: 10.1177/1538574411407088. [DOI] [PubMed] [Google Scholar]
- 59.Blumhardt G, Ringe B, Lauchart W, Burdelski M, Bechstein WO, Pichlmayr R. Vascular problems in liver transplantation. Transplant Proc. 1987;19:2412. [PubMed] [Google Scholar]
- 60.Denys AL, Qanadli SD, Durand F, Vilgrain V, Farges O, Belghiti J, Lacombe P, Menu Y. Feasibility and effectiveness of using coronary stents in the treatment of hepatic artery stenoses after orthotopic liver transplantation: preliminary report. AJR Am J Roentgenol. 2002;178:1175–1179. doi: 10.2214/ajr.178.5.1781175. [DOI] [PubMed] [Google Scholar]
- 61.Chen GH, Wang GY, Yang Y, Li H, Lu MQ, Cai CJ, Wang GS, Xu C, Yi SH, Zhang JF, et al. Single-center experience of therapeutic management of hepatic artery stenosis after orthotopic liver transplantation. Report of 20 cases. Eur Surg Res. 2009;42:21–27. doi: 10.1159/000166601. [DOI] [PubMed] [Google Scholar]
- 62.Uller W, Knoppke B, Schreyer AG, Heiss P, Schlitt HJ, Melter M, Stroszczynski C, Zorger N, Wohlgemuth WA. Interventional radiological treatment of perihepatic vascular stenosis or occlusion in pediatric patients after liver transplantation. Cardiovasc Intervent Radiol. 2013;36:1562–1571. doi: 10.1007/s00270-013-0595-1. [DOI] [PubMed] [Google Scholar]
- 63.Orons PD, Sheng R, Zajko AB. Hepatic artery stenosis in liver transplant recipients: prevalence and cholangiographic appearance of associated biliary complications. AJR Am J Roentgenol. 1995;165:1145–1149. doi: 10.2214/ajr.165.5.7572493. [DOI] [PubMed] [Google Scholar]
- 64.Orons PD, Zajko AB, Bron KM, Trecha GT, Selby RR, Fung JJ. Hepatic artery angioplasty after liver transplantation: experience in 21 allografts. J Vasc Interv Radiol. 1995;6:523–529. doi: 10.1016/s1051-0443(95)71128-9. [DOI] [PubMed] [Google Scholar]
- 65.Frongillo F, Grossi U, Lirosi MC, Nure E, Sganga G, Avolio AW, Inchingolo R, Di Stasi C, Rinaldi P, Agnes S. Incidence, management, and results of hepatic artery stenosis after liver transplantation in the era of donor to recipient match. Transplant Proc. 2013;45:2722–2725. doi: 10.1016/j.transproceed.2013.08.007. [DOI] [PubMed] [Google Scholar]
- 66.Boyvat F, Aytekin C, Harman A, Sevmiş S, Karakayali H, Haberal M. Endovascular stent placement in patients with hepatic artery stenoses or thromboses after liver transplant. Transplant Proc. 2008;40:22–26. doi: 10.1016/j.transproceed.2007.12.027. [DOI] [PubMed] [Google Scholar]
- 67.Abad J, Hidalgo EG, Cantarero JM, Parga G, Fernandez R, Gomez M, Colina F, Moreno E. Hepatic artery anastomotic stenosis after transplantation: treatment with percutaneous transluminal angioplasty. Radiology. 1989;171:661–662. doi: 10.1148/radiology.171.3.2524086. [DOI] [PubMed] [Google Scholar]
- 68.Mondragon RS, Karani JB, Heaton ND, Thomas S, Wong PY, O’Grady JG, Tan KC, Williams R. The use of percutaneous transluminal angioplasty in hepatic artery stenosis after transplantation. Transplantation. 1994;57:228–231. doi: 10.1097/00007890-199401001-00013. [DOI] [PubMed] [Google Scholar]
- 69.Ueno T, Jones G, Martin A, Ikegami T, Sanchez EQ, Chinnakotla S, Randall HB, Levy MF, Goldstein RM, Klintmalm GB. Clinical outcomes from hepatic artery stenting in liver transplantation. Liver Transpl. 2006;12:422–427. doi: 10.1002/lt.20628. [DOI] [PubMed] [Google Scholar]
- 70.Sommacale D, Rochas Dos Santos V, Dondero F, Francoz C, Durand F, Sibert A, Paugam-Burtz C, Sauvanet A, Belghiti J. Simultaneous surgical repair for combined biliary and arterial stenoses after liver transplantation. Transplant Proc. 2011;43:1765–1769. doi: 10.1016/j.transproceed.2011.01.171. [DOI] [PubMed] [Google Scholar]
- 71.Houssin D, Ortega D, Richardson A, Ozier Y, Stephan H, Soffer M, Chapuis Y. Mycotic aneurysm of the hepatic artery complicating human liver transplantation. Transplantation. 1988;46:469–472. doi: 10.1097/00007890-198809000-00033. [DOI] [PubMed] [Google Scholar]
- 72.Lerut J, Gordon RD, Iwatsuki S, Starzl TE. Surgical complications in human orthotopic liver transplantation. Acta Chir Belg. 1987;87:193–204. [PMC free article] [PubMed] [Google Scholar]
- 73.Madariaga J, Tzakis A, Zajko AB, Tzoracoleftherakis E, Tepetes K, Gordon R, Todo S, Starzl TE. Hepatic artery pseudoaneurysm ligation after orthotopic liver transplantation--a report of 7 cases. Transplantation. 1992;54:824–828. doi: 10.1097/00007890-199211000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bonham CA, Kapur S, Geller D, Fung JJ, Pinna A. Excision and immediate revascularization for hepatic artery pseudoaneurysm following liver transplantation. Transplant Proc. 1999;31:443. doi: 10.1016/s0041-1345(98)01698-4. [DOI] [PubMed] [Google Scholar]
- 75.Lowell JA, Coopersmith CM, Shenoy S, Howard TK. Unusual presentations of nonmycotic hepatic artery pseudoaneurysms after liver transplantation. Liver Transpl Surg. 1999;5:200–203. doi: 10.1002/lt.500050306. [DOI] [PubMed] [Google Scholar]
- 76.Stange B, Settmacher U, Glanemann M, Nuessler NC, Bechstein WO, Neuhaus P. Aneurysms of the hepatic artery after liver transplantation. Transplant Proc. 2000;32:533–534. doi: 10.1016/s0041-1345(00)00877-0. [DOI] [PubMed] [Google Scholar]
- 77.Leonardi LS, Soares C, Boin IF, Oliveira VC. Hemobilia after mycotic hepatic artery pseudoaneurysm after liver transplantation. Transplant Proc. 2001;33:2580–2582. doi: 10.1016/s0041-1345(01)02103-0. [DOI] [PubMed] [Google Scholar]
- 78.Marshall MM, Muiesan P, Srinivasan P, Kane PA, Rela M, Heaton ND, Karani JB, Sidhu PS. Hepatic artery pseudoaneurysms following liver transplantation: incidence, presenting features and management. Clin Radiol. 2001;56:579–587. doi: 10.1053/crad.2001.0650. [DOI] [PubMed] [Google Scholar]
- 79.Turrión VS, Alvira LG, Jimenez M, Lucena JL, Ardaiz J. Incidence and results of arterial complications in liver transplantation: experience in a series of 400 transplants. Transplant Proc. 2002;34:292–293. doi: 10.1016/s0041-1345(01)02767-1. [DOI] [PubMed] [Google Scholar]
- 80.Leelaudomlipi S, Bramhall SR, Gunson BK, Candinas D, Buckels JA, McMaster P, Mirza DF, Mayer AD. Hepatic-artery aneurysm in adult liver transplantation. Transpl Int. 2003;16:257–261. doi: 10.1007/s00147-003-0551-0. [DOI] [PubMed] [Google Scholar]
- 81.Volpin E, Pessaux P, Sauvanet A, Sibert A, Kianmanesh R, Durand F, Belghiti J, Sommacale D. Preservation of the arterial vascularisation after hepatic artery pseudoaneurysm following orthotopic liver transplantation: long-term results. Ann Transplant. 2014;19:346–352. doi: 10.12659/AOT.890473. [DOI] [PubMed] [Google Scholar]
- 82.Jarzembowski TM, Sankary HN, Bogetti D, Manzelli A, Ong E, Oberholzer J, Benedetti E, Testa G. Living donor liver graft salvage after rupture of hepatic artery pseudoaneurysm. Int Surg. 2008;93:300–303. [PubMed] [Google Scholar]
- 83.Panaro F, Miggino M, Bouyabrine H, Carabalona JP, Berthet JP, Canaud L, Nougaret S, Ramos J, Navarro F. Reversed saphenous bypass for hepatic artery pseudoaneurysm after liver transplantation. Ann Vasc Surg. 2013;27:1088–1097. doi: 10.1016/j.avsg.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 84.Sellers MT, Haustein SV, McGuire BM, Jones C, Bynon JS, Diethelm AG, Eckhoff DE. Use of preserved vascular homografts in liver transplantation: hepatic artery aneurysms and other complications. Am J Transplant. 2002;2:471–475. doi: 10.1034/j.1600-6143.2002.20513.x. [DOI] [PubMed] [Google Scholar]
- 85.Fistouris J, Herlenius G, Bäckman L, Olausson M, Rizell M, Mjörnstedt L, Friman S. Pseudoaneurysm of the hepatic artery following liver transplantation. Transplant Proc. 2006;38:2679–2682. doi: 10.1016/j.transproceed.2006.07.028. [DOI] [PubMed] [Google Scholar]
- 86.Patel JV, Weston MJ, Kessel DO, Prasad R, Toogood GJ, Robertson I. Hepatic artery pseudoaneurysm after liver transplantation: treatment with percutaneous thrombin injection. Transplantation. 2003;75:1755–1757. doi: 10.1097/01.TP.0000063936.94587.10. [DOI] [PubMed] [Google Scholar]
- 87.Kim HJ, Kim KW, Kim AY, Kim TK, Byun JH, Won HJ, Shin YM, Kim PN, Ha HK, Lee SG, et al. Hepatic artery pseudoaneurysms in adult living-donor liver transplantation: efficacy of CT and Doppler sonography. AJR Am J Roentgenol. 2005;184:1549–1555. doi: 10.2214/ajr.184.5.01841549. [DOI] [PubMed] [Google Scholar]
- 88.Golse N, Spina A, Abdelaal A, Mennesson N, Feugier P, Dumortier J, Boillot O, Adham M. Extra-anatomical hepatic artery reconstruction following post-embolization iatrogenic dissection and arterial anastomotic rupture in two liver transplant recipients. Gastroenterol Clin Biol. 2010;34:111–114. doi: 10.1016/j.gcb.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 89.Parrilla P, Sánchez-Bueno F, Figueras J, Jaurrieta E, Mir J, Margarit C, Lázaro J, Herrera L, Gómez-Fleitas M, Varo E, et al. Analysis of the complications of the piggy-back technique in 1,112 liver transplants. Transplantation. 1999;67:1214–1217. doi: 10.1097/00007890-199905150-00003. [DOI] [PubMed] [Google Scholar]
- 90.Sánchez-Bueno F, Hernández Q, Ramírez P, Robles R, Acosta F, Rodríguez JM, Parrilla P. Vascular complications in a series of 300 orthotopic liver transplants. Transplant Proc. 1999;31:2409–2410. doi: 10.1016/s0041-1345(99)00406-6. [DOI] [PubMed] [Google Scholar]
- 91.Woo DH, Laberge JM, Gordon RL, Wilson MW, Kerlan RK. Management of portal venous complications after liver transplantation. Tech Vasc Interv Radiol. 2007;10:233–239. doi: 10.1053/j.tvir.2007.09.017. [DOI] [PubMed] [Google Scholar]
- 92.Yilmaz A, Arikan C, Tumgor G, Kilic M, Aydogdu S. Vascular complications in living-related and deceased donation pediatric liver transplantation: single center’s experience from Turkey. Pediatr Transplant. 2007;11:160–164. doi: 10.1111/j.1399-3046.2006.00601.x. [DOI] [PubMed] [Google Scholar]
- 93.Orlandini M, Feier FH, Jaeger B, Kieling C, Vieira SG, Zanotelli ML. Frequency of and factors associated with vascular complications after pediatric liver transplantation. J Pediatr (Rio J) 2014;90:169–175. doi: 10.1016/j.jped.2013.08.010. [DOI] [PubMed] [Google Scholar]
- 94.Audet M, Piardi T, Panaro F, Cag M, Habibeh H, Gheza F, Portolani N, Cinqualbre J, Jaeck D, Wolf P. Four hundred and twenty-three consecutive adults piggy-back liver transplantations with the three suprahepatic veins: was the portal systemic shunt required? J Gastroenterol Hepatol. 2010;25:591–596. doi: 10.1111/j.1440-1746.2009.06084.x. [DOI] [PubMed] [Google Scholar]
- 95.Schmitz V, Schoening W, Jelkmann I, Globke B, Pascher A, Bahra M, Neuhaus P, Puhl G. Different cava reconstruction techniques in liver transplantation: piggyback versus cava resection. Hepatobiliary Pancreat Dis Int. 2014;13:242–249. doi: 10.1016/s1499-3872(14)60250-2. [DOI] [PubMed] [Google Scholar]
- 96.Lerut J, Tzakis AG, Bron K, Gordon RD, Iwatsuki S, Esquivel CO, Makowka L, Todo S, Starzl TE. Complications of venous reconstruction in human orthotopic liver transplantation. Ann Surg. 1987;205:404–414. doi: 10.1097/00000658-198704000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Buell JF, Funaki B, Cronin DC, Yoshida A, Perlman MK, Lorenz J, Kelly S, Brady L, Leef JA, Millis JM. Long-term venous complications after full-size and segmental pediatric liver transplantation. Ann Surg. 2002;236:658–666. doi: 10.1097/00000658-200211000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Strovski E, Liu D, Scudamore C, Ho S, Yoshida E, Klass D. Magnetic resonance venography and liver transplant complications. World J Gastroenterol. 2013;19:6110–6113. doi: 10.3748/wjg.v19.i36.6110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Goss JA, Shackleton CR, McDiarmid SV, Maggard M, Swenson K, Seu P, Vargas J, Martin M, Ament M, Brill J, et al. Long-term results of pediatric liver transplantation: an analysis of 569 transplants. Ann Surg. 1998;228:411–420. doi: 10.1097/00000658-199809000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Charco R, Fuster J, Fondevila C, Ferrer J, Mans E, García-Valdecasas JC. Portal vein thrombosis in liver transplantation. Transplant Proc. 2005;37:3904–3905. doi: 10.1016/j.transproceed.2005.09.120. [DOI] [PubMed] [Google Scholar]
- 101.Kyoden Y, Tamura S, Sugawara Y, Matsui Y, Togashi J, Kaneko J, Kokudo N, Makuuchi M. Portal vein complications after adult-to-adult living donor liver transplantation. Transpl Int. 2008;21:1136–1144. doi: 10.1111/j.1432-2277.2008.00752.x. [DOI] [PubMed] [Google Scholar]
- 102.Kaneko J, Sugawara Y, Ohkubo T, Matsui Y, Kokudo N, Makuuchi M. Successful conservative therapy for portal vein thrombosis after living donor liver transplantation. Abdom Imaging. 2003;28:58–59. doi: 10.1007/s00261-001-0151-3. [DOI] [PubMed] [Google Scholar]
- 103.Cheng YF, Ou HY, Tsang LL, Yu CY, Huang TL, Chen TY, Concejero A, Wang CC, Wang SH, Lin TS, et al. Vascular stents in the management of portal venous complications in living donor liver transplantation. Am J Transplant. 2010;10:1276–1283. doi: 10.1111/j.1600-6143.2010.03076.x. [DOI] [PubMed] [Google Scholar]
- 104.Azzam AZ, Tanaka K. Management of vascular complications after living donor liver transplantation. Hepatogastroenterology. 2012;59:182–186. doi: 10.5754/hge10453. [DOI] [PubMed] [Google Scholar]
- 105.Abdelaziz O, Hosny K, Elmalt O, Emad-Eldin S, Hosny A. Intra-operative Ultrasound-guided Thrombectomy and Thrombolysis for Post-operative Portal Vein Thrombosis in Living Liver Donors. Int J Organ Transplant Med. 2015;6:33–40. [PMC free article] [PubMed] [Google Scholar]
- 106.Cheng YF, Huang TL, Chen CL, Lee TY, Chen TY, Chen YS, Liu PP, Chiang YC, Eng HL, Wang CC, et al. Intraoperative Doppler ultrasound in liver transplantation. Clin Transplant. 1998;12:292–299. [PubMed] [Google Scholar]
- 107.Huang TL, Cheng YF, Chen TY, Tsang LL, Ou HY, Yu CY, Wang CC, Wang SH, Lin CL, Cheung HK, et al. Doppler ultrasound evaluation of postoperative portal vein stenosis in adult living donor liver transplantation. Transplant Proc. 2010;42:879–881. doi: 10.1016/j.transproceed.2010.02.036. [DOI] [PubMed] [Google Scholar]
- 108.Lee SJ, Kim KW, Kim SY, Park YS, Lee J, Kim HJ, Lee JS, Song GW, Hwang S, Lee SG. Contrast-enhanced sonography for screening of vascular complication in recipients following living donor liver transplantation. J Clin Ultrasound. 2013;41:305–312. doi: 10.1002/jcu.22044. [DOI] [PubMed] [Google Scholar]
- 109.Lee H, Lim CW, Yoo SH, Koo CH, Kwon WI, Suh KS, Ryu HG. The effect of Doppler ultrasound on early vascular interventions and clinical outcomes after liver transplantation. World J Surg. 2014;38:3202–3209. doi: 10.1007/s00268-014-2721-x. [DOI] [PubMed] [Google Scholar]
- 110.Rennert J, Dornia C, Georgieva M, Roehrl S, Fellner C, Schleder S, Stroszczynski C, Jung EM. Identification of early complications following liver transplantation using contrast enhanced ultrasound (CEUS). First results. J Gastrointestin Liver Dis. 2012;21:407–412. [PubMed] [Google Scholar]
- 111.Olcott EW, Ring EJ, Roberts JP, Ascher NL, Lake JR, Gordon RL. Percutaneous transhepatic portal vein angioplasty and stent placement after liver transplantation: early experience. J Vasc Interv Radiol. 1990;1:17–22. doi: 10.1016/s1051-0443(90)72496-7. [DOI] [PubMed] [Google Scholar]
- 112.Durham JD, LaBerge JM, Altman S, Kam I, Everson GT, Gordon RL, Kumpe DA. Portal vein thrombolysis and closure of competitive shunts following liver transplantation. J Vasc Interv Radiol. 1994;5:611–615; discussion 616-618. doi: 10.1016/s1051-0443(94)71562-1. [DOI] [PubMed] [Google Scholar]
- 113.Cherukuri R, Haskal ZJ, Naji A, Shaked A. Percutaneous thrombolysis and stent placement for the treatment of portal vein thrombosis after liver transplantation: long-term follow-up. Transplantation. 1998;65:1124–1126. doi: 10.1097/00007890-199804270-00018. [DOI] [PubMed] [Google Scholar]
- 114.Kensinger CD, Sexton KW, Baron CM, Lipnik AJ, Meranze SG, Gorden DL. Management of portal vein thrombosis after liver transplantation with a combined open and endovascular approach. Liver Transpl. 2015;21:132–134. doi: 10.1002/lt.24011. [DOI] [PubMed] [Google Scholar]
- 115.Haskal ZJ, Naji A. Treatment of portal vein thrombosis after liver transplantation with percutaneous thrombolysis and stent placement. J Vasc Interv Radiol. 1993;4:789–792. doi: 10.1016/s1051-0443(93)71974-0. [DOI] [PubMed] [Google Scholar]
- 116.Bhattacharjya T, Olliff SP, Bhattacharjya S, Mirza DF, McMaster P. Percutaneous portal vein thrombolysis and endovascular stent for management of posttransplant portal venous conduit thrombosis. Transplantation. 2000;69:2195–2198. doi: 10.1097/00007890-200005270-00042. [DOI] [PubMed] [Google Scholar]
- 117.Baccarani U, Gasparini D, Risaliti A, Vianello V, Adani GL, Sainz M, Sponza M, Bresadola F. Percutaneous mechanical fragmentation and stent placement for the treatment of early posttransplantation portal vein thrombosis. Transplantation. 2001;72:1572–1582. doi: 10.1097/00007890-200111150-00016. [DOI] [PubMed] [Google Scholar]
- 118.Lerut JP, Goffette P, Molle G, Roggen FM, Puttemans T, Brenard R, Morelli MC, Wallemacq P, Van Beers B, Laterre PF. Transjugular intrahepatic portosystemic shunt after adult liver transplantation: experience in eight patients. Transplantation. 1999;68:379–384. doi: 10.1097/00007890-199908150-00009. [DOI] [PubMed] [Google Scholar]
- 119.Ciccarelli O, Goffette P, Laterre PF, Danse E, Wittebolle X, Lerut J. Transjugular intrahepatic portosystemic shunt approach and local thrombolysis for treatment of early posttransplant portal vein thrombosis. Transplantation. 2001;72:159–161. doi: 10.1097/00007890-200107150-00030. [DOI] [PubMed] [Google Scholar]
- 120.López-Benítez R, Barragán-Campos HM, Richter GM, Sauer P, Mehrabi A, Fonouni H, Golriz M, Schmidt J, Hallscheidt PJ. Interventional radiologic procedures in the treatment of complications after liver transplantation. Clin Transplant. 2009;23 Suppl 21:92–101. doi: 10.1111/j.1399-0012.2009.01115.x. [DOI] [PubMed] [Google Scholar]
- 121.Cavallari A, Vivarelli M, Bellusci R, Jovine E, Mazziotti A, Rossi C. Treatment of vascular complications following liver transplantation: multidisciplinary approach. Hepatogastroenterology. 2001;48:179–183. [PubMed] [Google Scholar]
- 122.Lodhia N, Salem R, Levitsky J. Transjugular intrahepatic portosystemic shunt with thrombectomy for the treatment of portal vein thrombosis after liver transplantation. Dig Dis Sci. 2010;55:529–534. doi: 10.1007/s10620-009-0735-2. [DOI] [PubMed] [Google Scholar]
- 123.Guckelberger O, Bechstein WO, Langrehr JM, Kratschmer B, Loeffel J, Settmacher U, Neuhaus R, Lopez Haenninen E, Venz S, Vogl TJ, et al. Successful recanalization of late portal vein thrombosis after liver transplantation using systemic low-dose recombinant tissue plasminogen activator. Transpl Int. 1999;12:273–277. doi: 10.1007/s001470050222. [DOI] [PubMed] [Google Scholar]
- 124.Gulba DC, Bode C, Runge MS, Huber K. Thrombolytic agents--an overview. Ann Hematol. 1996;73 Suppl 1:S9–27. [PubMed] [Google Scholar]
- 125.Schneider N, Scanga A, Stokes L, Perri R. Portal vein stenosis: a rare yet clinically important cause of delayed-onset ascites after adult deceased donor liver transplantation: two case reports. Transplant Proc. 2011;43:3829–3834. doi: 10.1016/j.transproceed.2011.09.068. [DOI] [PubMed] [Google Scholar]
- 126.Wei BJ, Zhai RY, Wang JF, Dai DK, Yu P. Percutaneous portal venoplasty and stenting for anastomotic stenosis after liver transplantation. World J Gastroenterol. 2009;15:1880–1885. doi: 10.3748/wjg.15.1880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Mantel HT, Rosen CB, Heimbach JK, Nyberg SL, Ishitani MB, Andrews JC, McKusick MA, Haddock MG, Alberts SR, Gores GJ. Vascular complications after orthotopic liver transplantation after neoadjuvant therapy for hilar cholangiocarcinoma. Liver Transpl. 2007;13:1372–1381. doi: 10.1002/lt.21107. [DOI] [PubMed] [Google Scholar]
- 128.Shibata T, Itoh K, Kubo T, Maetani Y, Shibata T, Togashi K, Tanaka K. Percutaneous transhepatic balloon dilation of portal venous stenosis in patients with living donor liver transplantation. Radiology. 2005;235:1078–1083. doi: 10.1148/radiol.2353040489. [DOI] [PubMed] [Google Scholar]
- 129.Ko GY, Sung KB, Yoon HK, Lee S. Early posttransplantation portal vein stenosis following living donor liver transplantation: percutaneous transhepatic primary stent placement. Liver Transpl. 2007;13:530–536. doi: 10.1002/lt.21068. [DOI] [PubMed] [Google Scholar]
- 130.Zajko AB, Sheng R, Bron K, Reyes J, Nour B, Tzakis A. Percutaneous transluminal angioplasty of venous anastomotic stenoses complicating liver transplantation: intermediate-term results. J Vasc Interv Radiol. 1994;5:121–126. doi: 10.1016/s1051-0443(94)71467-6. [DOI] [PubMed] [Google Scholar]
- 131.Park KB, Choo SW, Do YS, Shin SW, Cho SG, Choo IW. Percutaneous angioplasty of portal vein stenosis that complicates liver transplantation: the mid-term therapeutic results. Korean J Radiol. 2005;6:161–166. doi: 10.3348/kjr.2005.6.3.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Shiba H, Sadaoka S, Wakiyama S, Ishida Y, Misawa T, Yanaga K. Successful treatment by balloon angioplasty under portography for late-onset stenosis of portal vein after cadaveric liver transplantation. Int Surg. 2013;98:466–468. doi: 10.9738/INTSURG-D-12-00031.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Glanemann M, Settmacher U, Langrehr JM, Kling N, Hidajat N, Stange B, Staffa G, Bechstein WO, Neuhaus P. Portal vein angioplasty using a transjugular, intrahepatic approach for treatment of extrahepatic portal vein stenosis after liver transplantation. Transpl Int. 2001;14:48–51. doi: 10.1007/s001470050742. [DOI] [PubMed] [Google Scholar]
- 134.Sanada Y, Kawano Y, Mizuta K, Egami S, Hayashida M, Wakiya T, Fujiwara T, Sakuma Y, Hydo M, Nakata M, et al. Strategy to prevent recurrent portal vein stenosis following interventional radiology in pediatric liver transplantation. Liver Transpl. 2010;16:332–339. doi: 10.1002/lt.21995. [DOI] [PubMed] [Google Scholar]
- 135.Navarro F, Le Moine MC, Fabre JM, Belghiti J, Cherqui D, Adam R, Pruvot FR, Letoublon C, Domergue J. Specific vascular complications of orthotopic liver transplantation with preservation of the retrohepatic vena cava: review of 1361 cases. Transplantation. 1999;68:646–650. doi: 10.1097/00007890-199909150-00009. [DOI] [PubMed] [Google Scholar]
- 136.Weeks SM, Gerber DA, Jaques PF, Sandhu J, Johnson MW, Fair JH, Mauro MA. Primary Gianturco stent placement for inferior vena cava abnormalities following liver transplantation. J Vasc Interv Radiol. 2000;11:177–187. doi: 10.1016/s1051-0443(07)61462-6. [DOI] [PubMed] [Google Scholar]
- 137.Darcy MD. Management of venous outflow complications after liver transplantation. Tech Vasc Interv Radiol. 2007;10:240–245. doi: 10.1053/j.tvir.2007.09.018. [DOI] [PubMed] [Google Scholar]
- 138.Starzl TE, Groth CG, Brettschneider L, Penn I, Fulginiti VA, Moon JB, Blanchard H, Martin AJ, Porter KA. Orthotopic homotransplantation of the human liver. Ann Surg. 1968;168:392–415. doi: 10.1097/00000658-196809000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Calne RY, Williams R. Liver transplantation in man. I. Observations on technique and organization in five cases. Br Med J. 1968;4:535–540. doi: 10.1136/bmj.4.5630.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Tzakis A, Todo S, Starzl TE. Orthotopic liver transplantation with preservation of the inferior vena cava. Ann Surg. 1989;210:649–652. doi: 10.1097/00000658-198911000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Belghiti J, Panis Y, Sauvanet A, Gayet B, Fékété F. A new technique of side to side caval anastomosis during orthotopic hepatic transplantation without inferior vena caval occlusion. Surg Gynecol Obstet. 1992;175:270–272. [PubMed] [Google Scholar]
- 142.Bismuth H, Castaing D, Sherlock DJ. Liver transplantation by “face-à-face” venacavaplasty. Surgery. 1992;111:151–155. [PubMed] [Google Scholar]
- 143.Cherqui D, Lauzet JY, Rotman N, Duvoux C, Dhumeaux D, Julien M, Fagniez PL. Orthotopic liver transplantation with preservation of the caval and portal flows. Technique and results in 62 cases. Transplantation. 1994;58:793–796. [PubMed] [Google Scholar]
- 144.Kishi Y, Sugawara Y, Matsui Y, Akamatsu N, Makuuchi M. Late onset portal vein thrombosis and its risk factors. Hepatogastroenterology. 2008;55:1008–1009. [PubMed] [Google Scholar]
- 145.Lázaro JL, Charco R, Revhaug A, Murio E, Balsells J, Hidalgo E, Mora A, Cortés C, Margarit C. Hemodynamics in human liver transplantation with inferior vena cava preservation. Transplant Proc. 1997;29:2851–2852. doi: 10.1016/s0041-1345(97)00705-7. [DOI] [PubMed] [Google Scholar]
- 146.Robles R, Parrilla P, Acosta F, Bueno FS, Ramirez P, Lopez J, Lujan JA, Rodriguez JM, Fernandez JA, Picó F. Complications related to hepatic venous outflow in piggy-back liver transplantation: two- versus three-suprahepatic-vein anastomosis. Transplant Proc. 1999;31:2390–2391. doi: 10.1016/s0041-1345(99)00395-4. [DOI] [PubMed] [Google Scholar]
- 147.Wojcicki M, Post M, Pakosz-Golanowska M, Zeair S, Lubikowski J, Jarosz K, Czuprynska M, Milkiewicz P. Vascular complications following adult piggyback liver transplantation with end-to-side cavo-cavostomy: a single-center experience. Transplant Proc. 2009;41:3131–3134. doi: 10.1016/j.transproceed.2009.07.092. [DOI] [PubMed] [Google Scholar]
- 148.Tayar C, Kluger MD, Laurent A, Cherqui D. Optimizing outflow in piggyback liver transplantation without caval occlusion: the three-vein technique. Liver Transpl. 2011;17:88–92. doi: 10.1002/lt.22201. [DOI] [PubMed] [Google Scholar]
- 149.Nishida S, Nakamura N, Vaidya A, Levi DM, Kato T, Nery JR, Madariaga JR, Molina E, Ruiz P, Gyamfi A, et al. Piggyback technique in adult orthotopic liver transplantation: an analysis of 1067 liver transplants at a single center. HPB (Oxford) 2006;8:182–188. doi: 10.1080/13651820500542135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Mizuno S, Yokoi H, Yamagiwa K, Tabata M, Isaji S, Yamakado K, Takeda K, Uemoto S. Outflow block secondary to stenosis of the inferior vena cava following living-donor liver transplantation? Clin Transplant. 2005;19:215–219. doi: 10.1111/j.1399-0012.2004.00321.x. [DOI] [PubMed] [Google Scholar]
- 151.Yamagiwa K, Yokoi H, Isaji S, Tabata M, Mizuno S, Hori T, Yamakado K, Uemoto S, Takeda K. Intrahepatic hepatic vein stenosis after living-related liver transplantation treated by insertion of an expandable metallic stent. Am J Transplant. 2004;4:1006–1009. doi: 10.1111/j.1600-6143.2004.00440.x. [DOI] [PubMed] [Google Scholar]
- 152.Wang SL, Sze DY, Busque S, Razavi MK, Kee ST, Frisoli JK, Dake MD. Treatment of hepatic venous outflow obstruction after piggyback liver transplantation. Radiology. 2005;236:352–359. doi: 10.1148/radiol.2361040327. [DOI] [PubMed] [Google Scholar]
- 153.Liu XL, Li FQ, Li X, Li B, Yan LN, Wei YG. Treatment of hepatic venous outflow stenosis after living donor liver transplantation by insertion of an expandable metallic stent. Hepatobiliary Pancreat Dis Int. 2009;8:424–427. [PubMed] [Google Scholar]
- 154.Ikeda O, Tamura Y, Nakasone Y, Yamashita Y, Okajima H, Asonuma K, Inomata Y. Percutaneous transluminal venoplasty after venous pressure measurement in patients with hepatic venous outflow obstruction after living donor liver transplantation. Jpn J Radiol. 2010;28:520–526. doi: 10.1007/s11604-010-0463-8. [DOI] [PubMed] [Google Scholar]
- 155.Lee JM, Ko GY, Sung KB, Gwon DI, Yoon HK, Lee SG. Long-term efficacy of stent placement for treating inferior vena cava stenosis following liver transplantation. Liver Transpl. 2010;16:513–519. doi: 10.1002/lt.22021. [DOI] [PubMed] [Google Scholar]
- 156.Ferro C, Andorno E, Guastavino A, Rossi UG, Seitun S, Bovio G, Valente U. Endovascular treatment with primary stenting of inferior cava vein torsion following orthotopic liver transplantation with modified piggyback technique. Radiol Med. 2014;119:183–188. doi: 10.1007/s11547-013-0325-4. [DOI] [PubMed] [Google Scholar]
- 157.Lorenz JM, van Beek D, Funaki B, Van Ha TG, Zangan S, Navuluri R, Leef JA. Long-term outcomes of percutaneous venoplasty and Gianturco stent placement to treat obstruction of the inferior vena cava complicating liver transplantation. Cardiovasc Intervent Radiol. 2014;37:114–124. doi: 10.1007/s00270-013-0643-x. [DOI] [PubMed] [Google Scholar]


