Abstract
The concept of pediatric emergency medicine (PEM) is virtually nonexistent in India. Suboptimally, organized prehospital services substantially hinder the evaluation, management, and subsequent transport of the acutely ill and/or injured child to an appropriate facility. Furthermore, the management of the ill child at the hospital level is often provided by overburdened providers who, by virtue of their training, lack experience in the skills required to effectively manage pediatric emergencies. Finally, the care of the traumatized child often requires the involvement of providers trained in different specialities, which further impedes timely access to appropriate care. The recent recognition of Doctor of Medicine (MD) in Emergency Medicine (EM) as an approved discipline of study as per the Indian Medical Council Act provides an unprecedented opportunity to introduce PEM as a formal academic program in India. PEM has to be developed as a 3-year superspeciality course (in PEM) after completion of MD/Diplomate of National Board (DNB) Pediatrics or MD/DNB in EM. The National Board of Examinations (NBE) that accredits and administers postgraduate and postdoctoral programs in India also needs to develop an academic program – DNB in PEM. The goals of such a program would be to impart theoretical knowledge, training in the appropriate skills and procedures, development of communication and counseling techniques, and research. In this paper, the Joint Working Group of the Academic College of Emergency Experts in India (JWG-ACEE-India) gives its recommendations for starting 3-year DM/DNB in PEM, including the curriculum, infrastructure, staffing, and training in India. This is an attempt to provide an uniform framework and a set of guiding principles to start PEM as a structured superspeciality to enhance emergency care for Indian children.
Keywords: India, pediatric emergency medicine, white paper
INTRODUCTION
The United Nations adopted the eight Millenium Development Goals (MDGs) in the year 2000 with the aim of global development. MDG 4 specifically targets the reduction of childhood mortality by two-thirds by 2015. The Sustainable Development Goals (SDGs) will replace the MDGs later in 2015; Goal 4 of the Draft SDGs is to ensure healthy lives and promote the well-being for all people of all ages. The fact sheet by the World Health Organization (WHO) in 2013 reported 6.6 million deaths under 5 years of age globally. Most of these deaths are from preventable causes, the leading ones being pneumonia, prematurity, diarrhea, and malaria.[1] These statistics, unfortunately, have not been showing much improvement, especially in low-income, developing countries. Primary prevention is certainly a strategy that works but a large number of these patients require hospitalization.
An improvement in emergency hospital care significantly reduces inpatient mortality rates. Clarke et al. have demonstrated that an improvement in short-term mortality can be achieved by small changes including; a designated area for emergency care, staff allocation to improve triage, the presence of simple medical equipment such as pulse oximetry and thermometry, and training.[2] WHO and the United Nations Children's Fund (UNICEF) have also incorporated a strengthened emergency care in the concept of Integrated Management of Childhood Illnesses.[3] However, Emergency medicine (EM) in India has recently gained acceptance as a specialty. Currently there are 24 medical colleges that offer 48 MD seats in emergency medicine and are recognized by the Government of India as per the Indian Medical Council (IMC) Act. Additionally, there are 66 Diplomate of National Board (DNB) seats of the National Board of Examination (NBE) in 20 accredited hospitals for emergency medicine. The introduction of these programs has created a momentum for development of academic standards, faculty development, and accreditation standards for quality EM services in the country.
In contrast, pediatric emergency medicine (PEM) is still in its infancy in India. This is not dissimilar to many countries that have an unstructured approach to the evaluation of the ill and injured child. Indeed, deficits in areas such as triaging, or managing disasters and trauma along with prolonged waiting times in emergency departments (ED) secondary to the lack of comprehensive emergency team services adversely affect the outcomes of children requiring emergency management.[4] As majority of the mortality occurs in the first 24–48 h of hospital admission in the ED itself; it is imperative that efforts to strengthen the pediatric emergency care infrastructure be pursued.[5] This white paper aims to provide a status update on the the current state of PEM in India and also suggests a model for establishing PEM largely based on what is currently being practiced in the USA.
PEDIATRIC EMERGENCY CARE: INDIAN SCENARIO
The pediatric ED in India is not an ED in the true sense. An initial study from a leading pediatrics center in Northern India showed that fever was the most common presenting complaint and upper respiratory tract infection and acute gastroenteritis were the two most common illnesses that required an ED evaluation.[6] Residents in the pediatric ED screen all the patients and manage minor illnesses as well; however, they are overburdened in a majority of instances. There are substantial gaps in; (a) the prehospital arena including lack of adequately trained ambulance personnel and appropriately equipped ambulances, (b) inadequate in-hospital triage systems, (c) lack of formal training in the evaluation and management of pediatric trauma leading to a lack of skilled medical personnel including nursing and other support services, and (d) availability of evidence-based patient management protocols.
Prehospital services in India
The medical system in India constitutes a multitude of private and public sector organizations that are managed at different levels; however, the coordination within the system is lacking. The emergency transport system of patients is mostly by private vehicles ranging from bullock carts to autorickshaws to cars and patients are often transported by family members or relatives.[7] Roads are often congested, which adds to the delay in accessing hospital services. Thus, the basic tenets of managing the ABCs, i.e., airway, breathing, and circulation of patients in an acute emergency is delayed. Verma et al. reported an average delay of 168 min (~3 h) in reaching the trauma facility.[8] Most of these children were accompanied by their fathers, or both the parents, and not by any trained prehospital transport team. Few states at present have their centralized emergency ambulance system, e.g. Delhi, the capital of India, has Centralized Accident and Trauma Services (CATS) but the number of ambulances are inadequate to meet the current demand and many of the ambulances do not have the age-appropriate equipment. Furthermore, prehospital services vary substantially among different states and do not have a universal phone number. The basic principle of transport, i.e., transport of the “right patient to the right hospital” is often not followed and as a result, patients arrive at a place where appropriate facilities are unavailable. This is especially true for trauma victims, both adult and pediatric.
Ramanujam et al. reported that half of the trauma victims reporting to the ED actually received no prehospital care.[9] Pallavisarjii et al. in their study from Southern India documented the lack of adequate skills among laypersons, including police, taxi drivers, and primary and middle school teachers, to handle an emergency although most of them revealed a willingness to learn these skills.[10] Roy et al.78] suggested training informal service providers who exist such as traffic police and taxi drivers in prehospital emergency medical service (EMS). Joshi et al. emphasized the need of Integrated Emergency Communication Response Service in India and proposed a model for development in the country.[11]
Hospital emergency care system
Most of the pediatric emergencies, including tertiary care teaching hospitals, are managed by pediatric residents who are trained in pediatric medical care that often excludes trauma training. Many of these pediatric providers are overburdened and simultaneously manage non-emergent conditions such as upper respiratory infections and acute gastroenteritis without dehydration.[6] Dedicated triage teams are unavailable in pediatric EDs. As a result, the management of sick patients is delayed, thus adversely affecting the outcome. According to a systematic review by Rowe et al., Triage Nurse Ordering was an effective intervention in mitigating overcrowding in ED and it reduced the length of stay in the ED substantially.[12] Triaging is especially important in the context of mass casualties and disasters. Quick survey using Pediatric Assessment Triangle (PAT) from Pediatric Advanced Life Support guidelines can be used to identify life-threatening illnesses. Combination of certain simple clinical signs can identify hypoxemia in an emergency and help in prioritizing patients.[13] The availability of simple bedside tests such as pulse oxymetry can be a useful and cost-effective adjunct to improve emergency care.[14] Certain clinical scores such as “signs of inflammation in children that kill (SICK),” and “temperature, oxygen saturation, pulse rate, respiratory rate, saturation and seizures (TOPRS)” have been validated in Indian children and used for the purpose of triaging.[15,16]
Pediatric disaster management
Large volumes of incoming patients involved in natural disasters such as earthquakes and tsunamis or unnatural disasters such as terrorist attacks can immediately overwhelm even the most advanced and resourced setting. Children are likely to suffer even more for multiple reasons: children may arrive unaccompanied, inexperience of the staff in the pediatric emergency setting, inadequate infrastructure including equipment, the need for subspecialists such as dedicated trauma surgeons, orthopedicians, burn specialists, and pediatric residents who are the first-line providers and who often have no experience in these specialties and hence, no exposure to handle these situations. The International Pediatric Association (IPA) started “training of trainers” on a worldwide level with the aim to manage children during disasters. The Indian Academy of Pediatrics formed a National Task Force on “Child at Risk” and the first report by the “Disaster Management Committee” was published in the year 2005. It emphasized the coordinated efforts of the government, along with nongovernment agencies (NGOs), the Red Cross, armed forces, international agencies, UNICEF, etc.[17,18] This was the first ever effort from India in the field of disaster management; however, further efforts in this direction are urgently needed.
USA MODEL OF PEM TRAINING PROGRAM
Since the recognition of PEM as a separate field in pediatrics and EM in the 1980s, fellowship programs have evolved and continue to evolve both in terms of the structure and quality in which PEM training is conducted. Many EM programs were established prior to that decade yet none devoted more than 8 weeks of training for pediatric surgical and medical emergencies, which was considered as the weakest link.[19] As the programs were gradually established, core competencies evolved within a decade to address the needed skills to complete the requirements for this nascent specialty.[20,21,22] Residency graduates from pediatrics or EM training programs in the USA are eligible to apply for PEM fellowship, with clearly defined difference in duration of training and requirements for scholarly activities to successfully achieve fellowship completion. In 1990, the American Board of Emergency Medicine (ABEM) and the American Board of Pediatrics (ABP) sought the approval of the American Board of Medical Specialties (ABMS) to recognize PEM as a superspeciality requiring independent certification. The request was granted in 1991 and the first exam was conducted in 1992.[23,24] In 1998, PEM became a fully accredited training course by the Accreditation Council of Graduate Medical Education (ACGME) that shaped the final outlook of a three-year training program that included a mandatory 1-year research component for pediatricians. However, applicants from EM residency programs have a 2-year training program compared to the 3 years for pediatric residency-trained applicants. Fellowship programs (if accepting fellows from both boards) are required to establish two separate formal curricula to address the differences in training experience.[25] ACGME also defined the program role, faculty responsibility, and facility requirements in creating an environment that would help the trainees to achieve their educational goal. These steps helped to develop the scope of training and create its goals and objectives that are being implemented in many training programs in the USA at present.
Rotations
Clinical rotations have gone through many iterations and multiple revisions to help create the ideal experience for trainees to acquire the needed knowledge, experience, and ability to manage children in acute care settings.[22] The clinical experience includes four main domains (teaching, consulting, administrative, and research training) that fellows in PEM are exposed to, through the three years of training. Research training and clinical pediatric ED are in the form of twelve one-month blocks spread throughout training to meet the required educational experience. Other rotations are scheduled and planned to address the much-needed exposure (when available) to medical and surgical subspecialties [anesthesia, adult emergencies, orthopedic surgery, pediatric intensive care, EMS, pediatric radiology, toxicology, trauma, ultrasound, administration and risk management]. Although different programs vary in their structure and design they all share a common core of essential rotations in trauma, orthopedic surgery, pediatric ED, anesthesia, intensive care, EMS, and adult emergencies. Furthermore, programs require fellows to be certified in Advanced Trauma Life Support (ATLS), Neonatal Advanced Life Support (NALS), Pediatric Basic (PBLS), and Advanced Life Support (PALS).
Pediatric emergency services in the USA
The need for prehospital care was first recognized with a joint landmark report in 1966 when the National Academy of Science (NAS) and the National Research Council (NRC) highlighted trauma as the leading cause for disability and death for persons 1–37 years of age in the USA.[26] Prior to that report, ambulance services were inconsistent, privately-owned, and lacked appropriate equipment and training specifically designed to meet pediatric demands. During the 1970s, the EMS system grew to its general form with increasing national awareness of the benefits of reducing morbidity and mortality of the adult population. The Emergency Medical Service Systems Act of 1973 changed the shape of medical practice by recognizing this need for developing comprehensive, area-wide emergency medical systems that are well-funded and well-connected.[27] This law also mandated the development of local plans and provided funding for the initial establishment of operational systems, the conduct of research in emergency medical techniques and devices, expansion of acceptable existing systems, creation of adequate communications systems, and the providing of appropriate education for emergency medical personnel. By the 1980s, the system realized the gap of care for children when Seidel et al. published that needs of children in prehospital settings were not met[28] that potentially contributed to higher mortality rates when compared to adults. Within the same period, curricula were established to train EMS personnel in pediatric care and pediatric surgeons took the lead in establishing specialized prehospital trauma care for children. These steps have helped shape the initial steps in creating regional EMS systems for the decades that followed and the Institute of Medicine (IOM) published its report on prehospital and hospital care for children that provided some insight of the current shortfalls in the system.[24] Finally, the current system recognizes a multilevel of care tailored to the individual needs of the children transported (first responders, emergency medical technician (EMT)–basic, EMT–intermediate, EMT–paramedic). Each of these levels exercise different abilities and equipments that are essential to manage the target population referred by the central command of the regional EMS system. Despite all these steps, the current system still needs improvement of coordination between hospitals and prehospital care, improvement of disaster preparedness, and the establishment of an evidence base for assessing as to how the specialty is evolving to meet the current needs.
PEDIATRIC EMERGENCY TRAINING PROGRAM IN INDIA
Current lacunae in pediatric emergency care underscore the need for incorporation of PEM training program in our medical education and training system. The Medical Council of India (MCI) has already recognized a 3-year MD course in EM in 24 medical colleges across the country. Children are physiologically, developmentally and emotionally, substantially different from adults and it is increasingly being recognized that providers need to be trained to meet those special needs. We are about to have MCI-recognized postgraduate degree and diploma courses in pediatric emergency medicine. It is imperative that a well structured postdoctoral superspeciality training program in pediatric EM is developed to enhance the emergency care for India's children.
Current training in India
Comprehensive management of the patient and taking care of surgical, orthopedic, ophthalmologic, otolaryngologic, dermatologic, and gynecological emergencies in pediatric ED are lacking. No consideration is given to the child's psychiatric and psychological needs in the ED. Specialists are usually on call and attend pediatric patients only when called - this adversely impacts care due to lack of access to adequately-trained subspecialists. Expertise and skills related to basic life- and limb-saving procedures such as the use of and access to alternate emergency airways, foreign body removal, thoracostomy, suturing, and splinting, to name a few, are not being taught. Defined protocols for standardized evidence-based evaluation, management, and disposition of children treated in EDs are lacking. Preparedness for multiple casualties and disasters is another domain that is under-emphasized and hence, under-resourced with many institutions being under-prepared.
Academic model for pediatric emergency training in India
After the initiation of MCI recognized residency programs in the discipline of EM (MD in EM), it is essential for the MCI to recognize the need for a superspeciality in PEM. Rising patient volume in pediatric emergency centers across the country reemphasizes the importance of starting DM and DNB programs (3 years, including examination) in PEM in recognized medical colleges and hospitals. Such institutions with diverse and high-volume patient population are the ideal sites in India for initiating DM programs in PEM.
The Academic College of Emergency Experts in India (ACEE-INDIA) is an INDO-US Emergency and Trauma Collaborative initiative that has started a 1-year capacity building training program in PEM, with the objective of introducing the concepts of PEM for those providers who may be interested in pursuing PEM as a career. The essential qualification for this program is MD/DNB in Pediatrics, MD/DNB in EM or a Fellow of ACEE-INDIA. The College is actively working toward its vision of starting DM and DNB in PEM. The Joint Working Group of ACEE-INDIA proposes the guidelines for development of such a program. A MD/DNB program in PEM should have Tthe following components:
Knowledge–Imparted though departmental teaching activities such as seminars, lectures, journal clubs, and self-directed learning
Clinical skills–Imparted through the apprentice model and rotational postings in different disciplines
Communication skills–Imparted though formal trainings and rotational postings in day-to-day practice
Undertaking research by undertaking thesis–Protocol writing in the first year, research and thesis completion in the second year
Encouraging publication of research work
Scholarship and excellence in professional work.
Eligibility criteria
It has been proposed that a medical graduate who has completed a 3-year course of MD/DNB in Pediatrics or MD/DNB in EM shall be eligible for DM or DNB course in PEM.[29]
Core curriculum and rotations
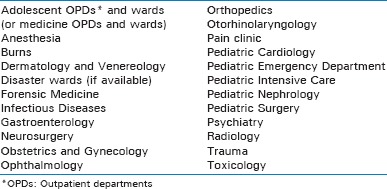
The accredited programs should develop specific residency rotations and predefined aims and learning objectives. Suggested core content for the residency program has been given in Table 1. The curriculum should be directly influenced by the epidemiology of pediatric emergencies in India. For instance, the toxicology curriculum will need to focus on locally prevalent ingestions such as organophosphates and hydrocarbons (kerosene) rather than tricyclic antidepressants, which are more common in the USA. Infectious diseases, which constitute a large and diverse volume in children should have a tropical perspective. Pediatric trauma and unintentional injuries, largely a neglected domain, constitute a huge burden of morbidity and mortality.[30] The rotations should include residency training in trauma and pediatric surgery wards and the gaining of expertise in managing various trauma mechanisms such as motor vehicle crashes, falls, and blunt and orthopedic injuries. Burns and electrocution injuries are also common in both urban and rural settings; hence, rotations should include burns and plastic surgery wards too.[31,32] Adolescents are a specialized group of the population who have different needs altogether. Gynecological problems in females as well as sexually transmitted diseases and psychiatric and psychological problems need to be recognized; hence, a rotation in the departments of obstetrics and gynecology and psychiatry becomes mandatory. Child maltreatment and sexual abuse are prevalent in society and often go unrecognized in pediatric emergencies.[33] Sensitization of pediatric emergency residents to these conditions and rotation in psychiatry medicine also need to be incorporated in the curriculum.
Table 1.
Suggested disciplines in pediatric emergency curriculum
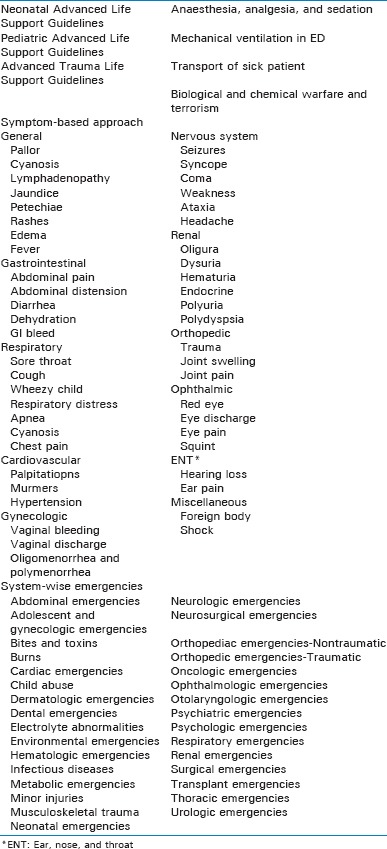
The 3-year curriculum in PEM should include rotations in various departments as shown in Table 2. Specific objectives need to be developed and validated for each rotation. A few examples of these objectives are depicted in Table 3. An objective evaluation of skills should be required in the form of maintainence of a procedure “logbook” for all trainees. Along with a record of participation in the teaching activities in the department, presentations made, case-record maintenance, procedures learnt and performed, counseling skills and the right attitude toward patients and relatives should be kept. Table 4 gives the description of the topics that need to be incorporated in PEM DM curriculum. The core text book for PEM should be Fleisher and Ludwig's Textbook of Pediatric Emergency Medicine. Apart from this, Tintinalli's Textbook of Emergency Medicine, and Goldfrank's Toxicologic Emergencies should be used as reference books. However, these will need to be supplemented with other pertinent texts, especially those written for Indian conditions.
Table 2.
Suggested rotations for a 3-year residency program

Table 3.
Objectives in various rotations
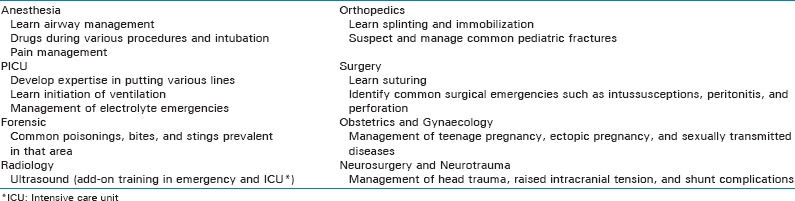
Table 4.
The 3-year curriculum for PEM DM training program
Research
Research in the form of thesis should be a mandatory requirement for partial fulfillment of the DM course. Apart from that, acceptance or publication of at least one paper in journals and one presentation in conference should be part of the eligibility criteria for appearing in the examination. This is being done for MD courses too. Setting of such high academically-oriented standards will help future emergency pediatricians to have the aptitude of research.[34,35]
Faculty/staff
A minimum of three faculty members, namely, a professor, an associate professor, and an assistant professor would be required for starting the DM program. A similar staff and academic criteria need to be evolved for DNB program. Since the specialty is still in the evolving stage, special consideration may be given with regard to the qualification for the faculty posts, e.g., for the post of Assistant Professor, 3 years of post-PG experience out of which 2 years in managing pediatric emergencies from a recognized medical college should suffice. Detailed guidelines for each post need to be adopted keeping in view the roadmap for program development.
Faculty development should include exchange programs with established centers in the developed world and distance learning by telemedicine and teleconferencing. INDO-US Emergency and Trauma Collaborative provides an excellent opportunity for pediatricians who wish to establish and pursue PEM in the public and private sectors as exchange programs.
Infrastructure
Bed strength
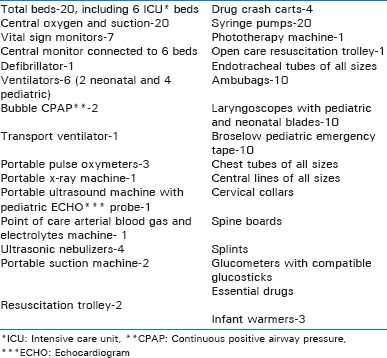
As per the existing norms of recognition to start a DM program, a pediatric emergency unit with a minimum of 20 beds should be available for PEM.
Equipment
Table 5 gives a comprehensive list of the equipments needed in a setup providing DM course in PEM for the purpose of patient care, training, and research.
Table 5.
List of equipments in pediatric emergency medicine
Mandatory courses and skills
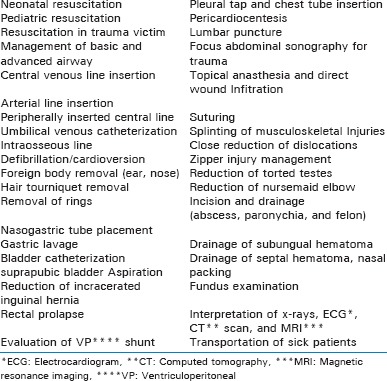
As ED is constantly dealing with sick patients, the development of resuscitative skills becomes important. Certification in Neonatal Advanced Life Support (NALS), Pediatric Advanced Life Support (PALS), Advanced Trauma Life Support (ATLS), and Advanced Cardiac Life Support (ACLS) should be a mandatory part of the training program. Equivalent courses from India Neonatal Resuscitation Program by the National Neonatology Forum of India, Indian Academy of Pediatrics-Advanced Life Support should be recognized for the residency program. During their rotations in the concerned specialties, PEM residents should receive training in skills such as airway management, vascular access, wound management, incision and drainage, foreign body removal, and suturing and splinting. Table 6 enlists the competencies that a DM candidate pursuing the training should acquire during his or her 3-year training program.
Table 6.
Procedural skills in pediatric emeregency medicine
Ultrasound in emergency, a noninvasive bedside test, is a useful adjunct for airway management, central line placement, identification of fluid and air in various cavities requiring emergency management such as the pneumothorax, pericardial tamponade, and hemoperitoneum.[36,37,38] A few standardized courses are available in India, and collaboration with such skill schools is needed to provide training in ED ultrasound for establishing the diagnosis and performing therapeutic procedures.
Assessment
Formative assessment should be carried out during the 3 years of training program, which should be made a part of internal assessment. Summative assessment of both theory and clinical practice should be done at the end of 3 years. The grading or marking system may be used for successful completion of the course.
Theory examination should consist of three question papers. These should be:
Paper I: Basic Sciences as applied to PEM
Paper II: Systemic PEM (abdominal, gastrointestinal, respiratory, cardiac, renal, and endocrinologic emergencies)
Paper III: Systemic PEM (orthopedic, ophthalmic, ear, nose, and throat (ENT), surgical, hematologic, oncologic, phychiatric, and behavioral emergencies).
The distribution of these three papers may be made on organ systems and procedures/highly focused areas only. In each paper, 10% weightage may be given to recent advances.
The practical examination should have:
Objective structured clinical examination (OSCE)
Cases (four).
Cases should focus on communication, management, and demonstartion of clinical skills so as to examine all the four domains of education.
The practical examination should incorporate assessment tools that offer high reliability and validity.
Tables with viva voce on procedures, instruments, x-rays, electrocardiogram (ECG), arterial blood gases, and clinical photographs
Procedures on simulators.
Assessors
A minimum of four examiners with experience of imparting teaching, training, and assessment of postgraduates in EM and pediatric emergencies from MCI/NBE recognized colleges should be assessing the candidate. Ideally, all examiners should have prior exposure and formal training in the assessment tools. As it is a new specialty, qualified faculty might not be available in the initial years; efforts be made to create a pool of examiners/assessors with 8 years of post-PG standing in teaching and training and in imparting formal training in assessment.
KEY RECOMMENDATIONS
The Joint Working Group of the Academic College of Emergency Experts in India (JWG ACEE-INDIA) proposes the following recommendations to start MCI-recognized DM/DNB course in PEM in India. The aim is to produce trained and skilled pediatric emergency physicians to provide the standard of care that is at par with the Western world and to improve overall childhood mortality and morbidity.
PEM should be recognized as a superspeciality per provisions of the Indian Medical Council Act and a 3-year MD/DNB program in PEM should be started in recognized medical colleges and institutes
MD/DNB pediatrics or MD/DNB in EM should be considered as an essential qualification to be eligible of this course
A 20-bedded pediatric emergency unit should be earmarked where resuscitation and treatment of sick patients may be carried out
Faculty requirement should be a minimum of three faculty members, namely, a professor, an associate professor, and an assistant professor for starting a PEM MD/DNB program
Since the faculty fulfilling the mandatory teaching requirement may not be available in the initial stages, relaxation may be given to begin with. For example, 3 years of post-PG experience out of which 2 years in managing pediatric emergencies from a recognized medical college should suffice for the post of Assistant Professor
Faculty should be a fulltime faculty dedicated to pediatric ED
Adequate infrastructure and equipment as enlisted should be available for starting the course
Residents pursuing DM course in PEM should have a defined rotational plan to have an exposure to all the related specialities
Residents should acquire the mandatory procedural skills and a logbook should be maintained by the department for the same
To promote research among residents, thesis should be a mandatory requirement toward fulfilling the DM/DNB course
Assessment of theoretical as well as clinical skills should be done by at least three formative assessments during the residency training and a final summative assessment at the end of three years by a panel of assessors.
CONCLUSION
The Academic College of Emergency Experts in India (ACEE-INDIA) is working incessantly to strengthen EM training in India. The MCI has recognized MD in EM as a specialty and now, it is time to move a step ahead. The Joint Working Group of ACEE INDIA proposes to start DM/DNB course in PEM as superspeciality in MCI-recognized medical colleges. Through this paper, a structured curriculum has been provided to start such a course so that well-trained, competent, and skilled pediatric emergency physicians are produced who can manage all the types of pediatric emergencies.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Editor's Note: This policy paper is being published simultaneously in ‘International Journal of Critical Illness and Injury Science’ (IJCIIS. 2015;5:247-55) and ‘Indian Pediatrics’ (Indian Pediatr. 2015;52:1061-71).
REFERENCES
- 1.Millenium Development Goals and Beyond. [Last accessed on 2014 Oct 6]. Available from: http://www.un.org/millenniumgoals/
- 2.Clark M, Spry E, Daoh K, Baion D, Skordis-Worrall J. Reductions in inpatient mortality following interventions to improve emergency hospital care in Freetown, Sierra Leone. PLoS One. 2012;7:e41458. doi: 10.1371/journal.pone.0041458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gove S. Integrated management of childhood illness by outpatient health workers: Technical basis and overview. The WHO Working Group on Guidelines for Integrated Management of the Sick Child. Bull World Health Organ. 1997;75(Suppl 1):7–24. [PMC free article] [PubMed] [Google Scholar]
- 4.Bursch B, Breezy J, Shaw R. Emergency department satisfaction: What matters most? Ann Emerg Med. 1993;22:586–91. doi: 10.1016/s0196-0644(05)81947-x. [DOI] [PubMed] [Google Scholar]
- 5.Molyneux E, Ahmad S, Robertson A. Improved triage and emergency care for children reduces inpatient mortality in a resource constrained setting. Bull World Health Organ. 2006;84:314–9. doi: 10.2471/blt.04.019505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singhi S, Singhi S, Gupta G. Comparison of pediatric emergency patients in a tertiary care hospital vs a community hospital. Indian Pediatr. 2004;41:67–72. [PubMed] [Google Scholar]
- 7.Roy N, Murlidhar V, Chowdhury R, Patil SB, Supe PA, Vaishnav PD, et al. Where there are no emergency medical services-prehospital care for the injured in Mumbai, India. See comment in PubMed Commons belowPrehosp Disaster Med. 2010;25:145–51. doi: 10.1017/s1049023x00007883. [DOI] [PubMed] [Google Scholar]
- 8.Verma S, Lal N, Lodha R, Murmu L. Childhood trauma profile at a tertiary care hospital in India. Indian Pediatr. 2009;46:168–71. [PubMed] [Google Scholar]
- 9.Ramanujam P, Aschkenasy M. Identifying the need for pre-hospital and emergency care in the developing world: A case study in Chennai, India. J Assoc Physicians India. 2007;55:491–5. [PubMed] [Google Scholar]
- 10.Pallavisarji U, Gururaj G, Girish RN. Practice and perception of first aid among lay first responders in a southern district of India. Arch Trauma Res. 2013;1:155–60. doi: 10.5812/atr.7972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joshi A, Rajhans P, Galwankar S, Arquilla B, Swaroop M, Stawicki S, et al. Academic college of emergency experts in India's INDO-US joint working group (JWG) white paper on the integrated emergency communication response service in India: Much more than just a number! J Emerg Trauma Shock. 2013;6:216–23. doi: 10.4103/0974-2700.115354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rowe BH, Villa-Roel C, Guo X, Bullard MJ, Ospina M, Vandermeer B, et al. The role of triage nurse ordering on mitigating overcrowding in emergency departments: A systematic review. Acad Emerg Med. 2011;18:1349–57. doi: 10.1111/j.1553-2712.2011.01081.x. [DOI] [PubMed] [Google Scholar]
- 13.Mwaniki MK, Nokes DJ, Ignas J, Munywoki P, Ngama M, Newton CR, et al. Emergency triage assessment for hypoxaemia in neonates and young children in a Kenyan hospital: An observational study. Bull World Health Organ. 2009;87:263–70. doi: 10.2471/BLT.07.049148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Choi J, Claudius I. Decrease in emergency department length of stay as a result of triage pulse oximetry. Pediatr Emerg Care. 2006;22:412–4. doi: 10.1097/01.pec.0000221340.26873.2f. [DOI] [PubMed] [Google Scholar]
- 15.Gupta MA, Chakrabarty A, Halstead R, Sahni M, Rangasami J, Puliyel A, et al. Validation of “Signs of Inflammation in Children that Kill” (SICK) score for immediate non-invasive assessment of severity of illness. Ital J Pediatr. 2010;36:35. doi: 10.1186/1824-7288-36-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bains HS, Soni RK. A simple clinical score “TOPRS” to predict outcome in pediatric emergency department in a teaching hospital in India. Iran J Pediatr. 2012;22:97–101. [PMC free article] [PubMed] [Google Scholar]
- 17.Olenes K, Bhave SY. Children in disasters. Indian Pediatr. 2005;42:873–5. [PubMed] [Google Scholar]
- 18.Bhave SY, Chaoudhary P, Pemde H, Mathur YC. IAP Task Force on Child at Risk. IAP workshop on disaster management practices: Recommendations and IAP plan of action. Indian Pediatr. 2005;42:887–903. [PubMed] [Google Scholar]
- 19.Morse TS. Formal training in pediatric emergency medicine: The surgeon's contribution. J Pediatr Surg. 1978;13(6D):690–2. doi: 10.1016/s0022-3468(78)80115-8. [DOI] [PubMed] [Google Scholar]
- 20.Pediatric Emergency Medicine (PEM) Fellowship Curriculum Statement. Curriculum Subcommittee, Section of Emergency Medicine, American Academy of Pediatrics. Pediatr Emerg Care. 1993;9:60–6. doi: 10.1097/00006565-199302000-00019. [DOI] [PubMed] [Google Scholar]
- 21.Modification of the PEM Fellowship Curriculum Statement for Emergency Medicine Resident Graduates (EMRGs). TERIPEM Committee of the Section of Emergency Medicine of the American Academy of Pediatrics. Pediatr Emerg Care. 1995;11:142–9. doi: 10.1097/00006565-199504000-00021. [DOI] [PubMed] [Google Scholar]
- 22.Shaw KN, Schunk J, Ledwith C, Lockhart G. Pediatric Emergency Medicine (PEM) fellowship: Essentials of a three-year academic curriculum. Three-Year Academic Subcommittee of the PEM Fellowship Committee of the Section of Emergency Medicine, American Academy of Pediatrics. Pediatr Emerg Care. 1997;13:77–81. [PubMed] [Google Scholar]
- 23.“Pediatric Emergency Medicine Overview” American Board of Emergency Medicine. [Last accessed on 2014 Dec 9]. Available from: https://www.abem.org/public/superspeciality-certification/pediatric-emergency-medicine/pediatric-emergency-medicine.overview .
- 24.Report. Emergency Care for Children: Growing Pains. [Last accessed on 2014 Dec 9]. Available from: http://www.iom.edu/Reports/2006/Emergency-Care-for-Children-Growing-Pains.aspx .
- 25.ACGME Accreditation Council for Graduate Medical Education. ACGME program requirements for graduate medical education in pediatric emergency medicine. [Last accessed on 2014 Dec 9]. Available from: https://www.acgme.org/acgmeweb/tabid/143/ProgramandInstitutionalAccreditation/MedicalSpecialties/Pediatrics.aspx .
- 26.Accidental death and disability: The neglected disease of modern society; Division of medical sciences at national academy of science and medical research council. 1966. [Last accessed on 2014 Dec 9]. Available from: http://www.ems.gov/pdf/1997-reproduction-accidentaldeathdissability.pdf .
- 27.Harvey JC. The emergency medical service systems act of 1973. JAMA. 1974;230:1139–40. [PubMed] [Google Scholar]
- 28.Seidel JS, Hornbein M, Yoshiyama K, Kuznets D, Finklestein JZ, St Geme JW., Jr Emergency medical services and the pediatric patient: Are the needs being met? Pediatrics. 1984;73:769–72. [PubMed] [Google Scholar]
- 29.Post Graduate Medical Education Regulations 2000. [Last accessed on 2014 Dec 9]. Available from: http://www.mciindia.org/RulesandRegulations/PGMedicalEducationRegulations2000.aspx .
- 30.Vashishtha VM. World Report on child injury prevention: An ignored component of child survival! Indian Pediatr. 2009;46:152–3. [PubMed] [Google Scholar]
- 31.Bagri N, Saha A, Chandelia S, Dubey NK, Bhatt A, Rai A, et al. Fireworks injuries in children: A prospective study during the festival of lights. Emerg Med Australas. 2013;25:452–6. doi: 10.1111/1742-6723.12114. [DOI] [PubMed] [Google Scholar]
- 32.Rai A, Khalil S, Batra P, Gupta SK, Bhattacharya S, Dubey NK, et al. Electrical injuries in urban children in New Delhi. Pediatr Emerg Care. 2013;29:342–5. doi: 10.1097/PEC.0b013e3182852f71. [DOI] [PubMed] [Google Scholar]
- 33.Krishnakumar P, Satheesan K, Geeta MG, Sureshkumar K. Prevalence and spectrum of sexual abuse among adolescents in Kerala, South India. Indian J Pediatr. 2014;81:770–4. doi: 10.1007/s12098-013-1260-z. [DOI] [PubMed] [Google Scholar]
- 34.Lerner EB, Dayan PS, Brown K, Fuchs S, Leonard J, Borgialli D, et al. Pediatric Emergency Care Applied Research Network (PECARN). Characteristics of the pediatric patients treated by the pediatric emergency care applied research network's affiliated EMS agencies. Prehosp Emerg Care. 2014;18:52–9. doi: 10.3109/10903127.2013.836262. [DOI] [PubMed] [Google Scholar]
- 35.Chamberlain JM, Shaw KN, Lillis KA, Mahajan PV, Ruddy RM, Lichenstein R, et al. Pediatric Emergency Care Applied Research Network. Creating an infrastructure for safety event reporting and analysis in a multicenter pediatric emergency department network. Pediatr Emerg Care. 2013;29:125–30. doi: 10.1097/PEC.0b013e31828043a5. [DOI] [PubMed] [Google Scholar]
- 36.Gallagher RA, Levy J, Vieira RL, Monuteaux MC, Stack AM. Ultrasound assistance for central venous catheter placement in a pediatric emergency department improves placement success rates. Acad Emerg Med. 2014;21:981–6. doi: 10.1111/acem.12460. [DOI] [PubMed] [Google Scholar]
- 37.Tessaro MO, Salant EP, Arroyo AC, Haines LE, Dickman E. Tracheal rapid ultrasound saline test (T.R.U.S.T) for confirming correct endotracheal tube depth in children. Resuscitation. 2015;89:8–12. doi: 10.1016/j.resuscitation.2014.08.033. [DOI] [PubMed] [Google Scholar]
- 38.Bhoi S, Chandra A, Galwankar S. Ultrasound-guided nerve blocks in the emergency department. J Emerg Trauma Shock. 2010;3:82–8. doi: 10.4103/0974-2700.58655. [DOI] [PMC free article] [PubMed] [Google Scholar]


