Abstract
Intrahospital transportation of critically ill patients is associated with significant complications. In order to reduce overall risk to the patient, such transports should well organized, efficient, and accompanied by the proper monitoring, equipment, and personnel. Protocols and guidelines for patient transfers should be utilized universally across all healthcare facilities. Care delivered during transport and at the site of diagnostic testing or procedure should be equivalent to the level of care provided in the originating environment. Here we review the most common problems encountered during transport in the hospital setting, including various associated adverse outcomes. Our objective is to make medical practitioners, nurses, and ancillary health care personnel more aware of the potential for various complications that may occur during patient movement from the intensive care unit to other locations within a healthcare facility, focusing on risk reduction and preventive strategies.
Keywords: Complications, critically ill patient population, intrahospital patient transfers, patient safety, never events
INTRODUCTION
Intrahospital transport (IHT) consists of the movement of a patient from one physical location within the hospital to another. Such transfers may be temporary (e.g., to obtain diagnostic imaging) or for a longer term (e.g., transfer from inpatient ward to an intensive care unit), and are critical transitions in which complications and death may occur.[1,2,3,4] Risks associated with IHT have been suggested to be independent of the duration of hospitalization.[5] Of interest, the distance travelled between locations may affect care delivery, quality and outcomes.[6,7]
The benefits of IHT must outweigh the risks, and a triage-like process should be instituted and followed in order to optimize the risk-benefit ratio for each IHT.[8] No patient should be transported for a test or procedure that is unlikely to alter care. Guidelines have been promulgated by the Society of Critical Care Medicine for the intrahospital transport of critically ill patients,[9] and, more recently, by French critical care societies.[10] The availability of checklists and/or the presence of specially trained personnel may mitigate complications and untoward outcomes.[1,11,12,13] Physicians must be aware that such transfers may be time consuming for nurses and require significant team effort and specific knowledge.[14,15] Finally, whenever a point-of-care alternative of similar clinical utility is available, such option should be considered (e.g., as part of established clinical pathways) before exposing the patient to the risk of IHT.[16,17,18,19,20]
Many issues related to IHT can be attributed to difficulties with equipment and/or clinical management of patients.[21] These factors combine with environmental factors related to IHT origin and destination settings, contributing to a unique and difficult to predict risk profile [Figures 1 and 2]. A concise review of common physiologic insults arising during IHT is lacking and would be of value for implementation of targeted strategies to ameliorate IHT related complications. Herein, we assess the impact of IHT on the respiratory system, hemodynamics (including loss of intravenous access), traumatic injury, nosocomial infections, acid-base homeostasis, glucose regulation, among other aspects. The purpose of this review is to provide a high-level overview of key complications associated with IHTs, allowing the reader to use it both as a clinical guide and a reference source for further research.
Figure 1.
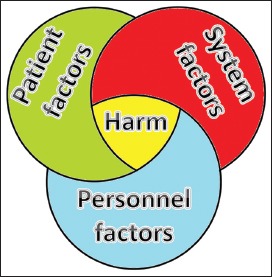
Schematic representation of key factors associated with patient harm during intrahospital transfers. A number of patient factors (e.g., acuity of illness/severity of injury); system factors (e.g., environment change, lack of safety procedures, inadequate facilities, equipment deficiencies or failures); and personnel factors (e.g., poor communication, inadequate training, insufficient staffing, lack of supervision). The above factors frequently interact in a synergistic fashion to result in potential or actual patient harm
Figure 2.
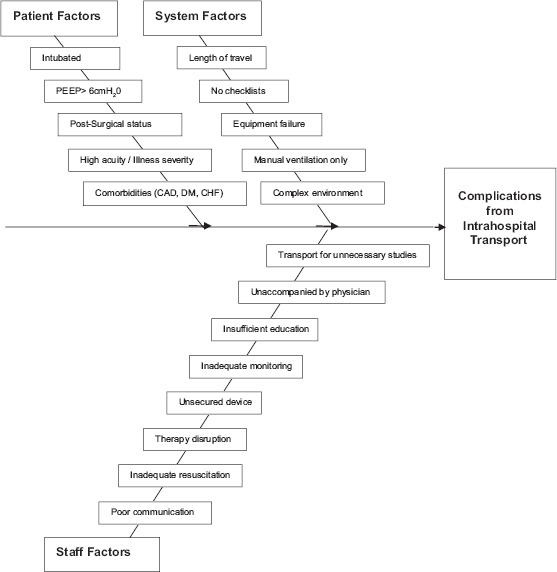
Factors contributing to complications during intrahospital transports. Fishbone diagram with patient, staff, and systems factors contributing to complications from intrahospital transport. Coronary artery disease (CAD), injury severity score (ISS), diabetes mellitus (DM)
PULMONARY COMPLICATIONS INCLUDING AIRWAY LOSS
Airway-related and pulmonary complications can occur during IHT, especially in the intensive care unit (ICU), trauma, and perioperative settings where a relatively high proportion of patients require mechanical ventilation thereby leading to an added complexity of the transport process. Symptomatic pneumothorax and atelectasis occur at an increased frequency in patients undergoing IHT.[1] In fact, the risk of pneumothorax may be elevated more than 2-fold while the occurrence of atelectasis may be increased nearly 3-fold in patients undergoing IHT.[1,22,23] Furthermore, there may be increased risk of developing deep vein thrombosis in transported patients (odds ratio of 4.5), which may subsequently lead to increased incidence of pulmonary embolism.[1]
Airway displacement risk may also be significant, yet it often is an under-recognized problem. Extrapolating from out-of-hospital transfers involving 77 pediatric and neonatal intubated patients, post-intubation chest roentgenograms demonstrated that the endotracheal tube was malpositioned in nearly half of the cases.[24] Although risk of similar occurrences during IHT may be lower, it is likely not negligible, and patient movement/transportation is likely to cause airway positioning challenges. Parmentier-Decruq et al.[5] examined a cohort of 262 mechanically ventilated patients who underwent IHT. Of all adverse events, 0.4% included accidental extubation, 8.8% involved oxygen desaturation, and 17.6% were incidents involving airway-related equipment.[5] Of note, risk factors for oxygen desaturation included positive end-expiratory pressure (PEEP) of >6 cmH2O as well as the use of treatment modification(s) for transport. In the aforementioned study, the largest sub-group of adverse events were equipment related incidents, including improper alarm settings and battery issues related to airway monitoring devices.[5] Of note, the presence of anesthesia trainees during patient transport activities was associated with fewer equipment related events, likely due to better familiarity with equipment and the ability to anticipate potential problems. In another report, Venkategowda et al.[25] examined a cohort of 254 ICU patients and again demonstrated that the majority of unexpected events during IHT were related to equipment malfunction. Unexpected events occurred in 139 patients, and 64% of adverse events were related to equipment issues such as oxygen probe displacement.[25] Furthermore, oxygen desaturation accounted for 10.8% of recorded adverse events.
In a study by Papson et al.[26] intrahospital transports involving 297 critically ill patients were characterized by as many as 640 unexpected events (e.g., 2.15 events per patient). Thirty events were considered significant, including 4 necessitating securing of the airway. Oxygen desaturation comprised 2.3% of unexpected events while equipment related events (probe disconnection, ventilator circuit leaks and ventilator failure) accounted for 11.3%. Furthermore, accidental extubation has been estimated to occur in nearly 1% of transports involving 1,659 ventilated patients in another study.[1] Although a rarity, attention should be given to accidental extubation as the risk of rapid patient demise without prompt intervention is inherent. Targeted prevention measures and experienced staff capable of providing ventilation and performing emergent airway intubation are invaluable during transport to prevent airway loss and reducing delays in reestablishing a definitive airway.
Outcomes with manual ventilation have also been compared to mechanical ventilation. One prospective study[27] examined transfers of 36 ventilator-dependent patients, of whom 20 received manual ventilation with a ventilatory bag while 16 patients were transported using portable mechanical ventilators. Fourteen out of the 20 manually ventilated patients experienced changes in parameters on arterial blood gas analysis (e.g., changes in pCO2 > 10 mmHg or changes in pH >0.05). There were significantly fewer alterations in the group that received mechanical ventilation compared to manual ventilation (P < 0.01).[27]
In summary, pulmonary complications associated with IHT are often attributed to equipment related issues and may be increased with manual ventilation relative to mechanical ventilation. This understanding should form the framework for the development of systematic solutions to circumvent and/or prevent such problems. Furthermore, experienced team members accompanying the transported patient can (and should) facilitate prevention, early recognition and definitive treatment of potential respiratory/pulmonary complications that may occur during IHT.
HEMODYNAMIC COMPLICATIONS
Hemodynamic alterations during IHT are always a reason for concern and require a great deal of vigilance. In a study involving 35 patients transported from an ICU, with vital signs measured at nine separate time points[11] and the majority of patients (77%) intubated, a substantial decrease in blood pressure was noted in 19 patients (54%). In addition, one patient developed significant hypotension (systolic blood pressure <90 mmHg).[11] Another study of 37 IHTs in mechanically ventilated patients demonstrated evidence of non-trivial heart rate increases during patient transports.[28]
Specific patient populations appear to be more vulnerable to hemodynamic alterations than others. One study of patients with coronary artery disease reported arrhythmias in 84% of patients transported from the ICU.[29] Likewise, a high incidence of cardiac instability was found in postoperative patients during intrahospital transports.[30]
Cardiac arrest remains a serious concern for critically ill patients undergoing IHT. The incidence of this dreaded complication is between 0.34% and 1.6%.[21,26,31,32] This variability might be partly attributed to inadequate monitoring during transportation, particularly when staff members with limited experience or less preparation are involved.[5]
Cumulatively, the above studies provide evidence for the risk of tachycardia, hypotension, and cardiac complications during IHT. Cardiac arrest occurs at a lower frequency but the consequences can be so devastating that it might be considered by some a “never event”. A great deal of attention should be devoted to vulnerable populations such as those with coronary artery disease and post-surgical patients as the potential for cardiac related problems is magnified in those groups.
INFECTION
Nosocomial infections are among the leading causes of morbidity and mortality in non-cardiac ICU patients.[33] Notably, IHT has been suggested as a potential risk factor for infection [Tables 1 and 2]. Such risk may be present for both the patient being transported and for others who might potentially be exposed to the transported patient (e.g., in cases of highly contagious or resistant infectious agents).[34,35] One study involving 521 patients on mechanical ventilation demonstrated that transport out of the ICU was independently associated with nearly 4-fold increase in odds of ventilator-associated pneumonia (VAP).[36] Severity of illness, patient gender, diagnosis, and potential risk factors for VAP including antibiotic administration, APACHE II score, bronchoscopy, and tracheostomy were all controlled for in the study design.[36] These findings were supported by another matched-cohort study where intra-hospital transport was associated with over a 3-fold increase in odds of VAP.[37] The largest study investigating this important topic in the context of IHT reported a nearly 1.4-fold increase in odds of VAP in a cohort of 6,242 patients.[1] Overall, the evidence supports the hypothesis that IHT is a quantifiable risk factor for the development of VAP. At the same time, the increased risk of infection associated with IHT should not become an impediment to obtaining medically indicated diagnostic tests and performing medically necessary procedures.
Table 1.
Studies investigating the association between intra-hospital transport and ventilator associated pneumonias
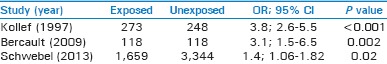
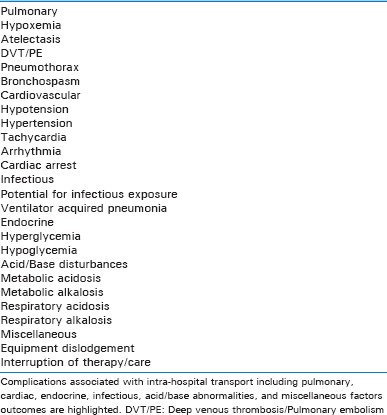
Table 2.
Complications of intrahospital transport
TRANSPORTING CRITICALLY INJURED PATIENTS
One frequently overlooked risk of transporting injured patients is the low, but very real, probability that an existing injury may be exacerbated in the process. This particular scenario can affect a variety of patients, but is especially important to consider in orthopaedic (e.g., extremity fractures) and neurosurgical patients (e.g., spine and/or brain injury), where various traction, monitoring and/or stabilization devices must be perfectly aligned and secured or patient functional outcomes may be affected.[38] Moreover, there is little to no room for error during such transports.
Spinal injury is among the most critical items on the list necessitating special attention. Minor patient manipulation without proper precautions may result in propagation of a sole skeletal related injury into one involving the spinal cord or other vital neurologic and vascular structures.[39] Specialized airway and stabilization equipment should be readily available for patients with cervical spine injuries, especially when potential respiratory or airway issues are present.[40]
Orthopedic traction or splinting devices, including traction pins and casts do not completely immobilize fractures.[41] This, in turn, may result in secondary injury via distraction, misalignment, neurovascular damage, or other types of soft tissue injury.[42] Consequently, providers caring for these patients, across all healthcare settings, should exercise extreme caution when performing patient manipulation outside of minimal activities, supervised mobilization, and/or repositioning. Effective multi-disciplinary team approach is crucial to successful care of multiply injured orthopaedic patients.[43]
Finally, the importance of the safe IHT of the brain-injured patient cannot be overemphasized. Picetti et al. followed 288 transports of brain-injured patients whose mean transport time was approximately 31 minutes.[13] Although >80% of the transports were scheduled and planned, there were 103/288 (36%) of patients who experienced complications (intracranial hypertension, oxygen saturation <90%, bronchospasm, ventilator dyssynchrony, hypertension or hypotension requiring intervention, and arrhythmias). In brain-injured patients, higher injury severity scores also place individuals at a greater risk of secondary insults during transportation. Adequate resuscitation prior to transport may help reduce the number of such secondary insults.[44,45]
INTERRUPTION OF CRITICAL OR SPECIALTY THERAPIES
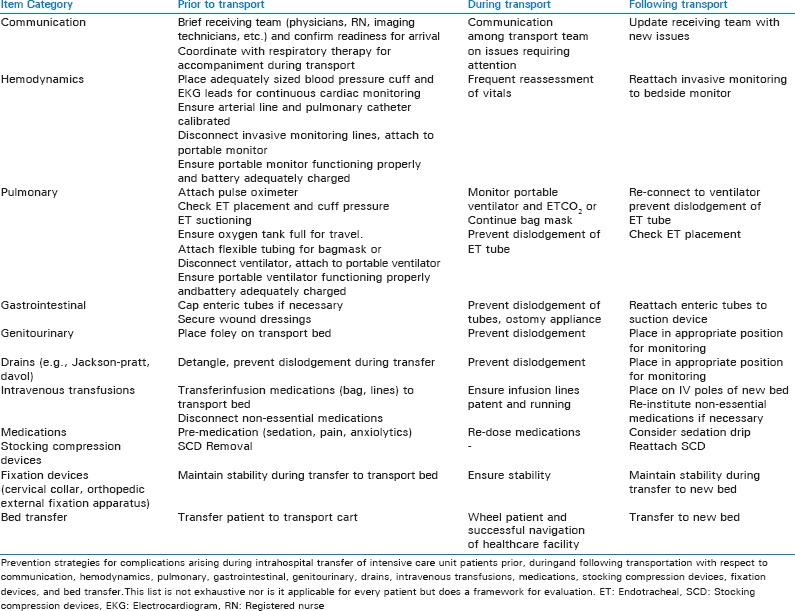
In addition to the potential for interruption in vital infusions (e.g., sedation, analgesia, vasopressor, inotrope)[26] and the ever-present potential for medication errors[46] during patient transports, there are various other therapies that must be maintained uninterrupted during IHT.[47] For example, a negative pressure wound therapy (NPWT) device intended to provide temporary abdominal coverage in patients with open abdomens should not be interrupted for more-than-minimal amount of time needed to exchange the fluid collection canister. If there is insufficient battery power or the canister overfills during patient transport, and cannot be readily replaced, the failure may result in unanticipated evisceration, need for unscheduled NPWT dressing change, or potentially emergent surgical intervention. Finally, a seemingly simple event as the loss of intravenous access can cause potentially serious problems.[12] Some of the complexities of patient transport considerations, including various continous therapies and life-saving devices, are schematically outlined in Figure 3.
Figure 3.
Complexities of Transferring Intensive Care Unit Patients. Representative setup and important suggested equipment prior to patient arrival in a modern intensive care bed (a) Demonstrative considerations necessary for transport teams of patients with various medical equipment/apparatus (with suggested appropriate action in brackets) in order to minimize unintended harm (b-f) Intracranial pressure (ICP), Continuous renal replacement therapy (CRRT), Intravenous (IV), Left ventricular assist device (LVAD)
HYPOGLYCEMIA AND HYPERGLYCEMIA
Derangements of glucose homeostasis and its management can occur during IHT. Schwebel et al.[1] examined over 3,000 IHTs for complications, including adverse events such as alterations in glucose. Hyperglycemia during IHT was nearly 2.3 times more likely when compared to control patients.[1] Likewise, the odds of IHT leading to an episode of hypoglycemia were elevated by a similar margin.[1] Glucose dysregulation may be related, in part, to transport practices such as discontinuation of insulin pumps and alterations in intravenous fluid infusions during transport. Because the degree of glycemic control and the associated glycemic variability both correlate with patient outcomes,[48,49] close attention should be paid to glucose regulation during all phases of patient care, including IHTs.[50] It is advisable for clinical teams to include glycemic control as an integral part of pre-IHT debriefing.
ACID/BASE DISORDERS
Ventilator changes, alterations in intravenous fluid infusions, interruptions in vasoactive drug administration, as well as altered circulatory dynamics and end-organ perfusion can result in perturbations in systemic acid-base milieu during IHTs. Acidotic conditions may alter vasopressor effectiveness and predispose patients to arrhythmias. Braman et al.[27] evaluated arterial pH and PaCO2 in critically ill patients transported on a mechanical ventilator compared to manual ventilation. Changes of magnitude greater than 10 mm Hg PaCO2 and 0.05 pH units were used as cutoff points. Patients on mechanical ventilation experienced significantly fewer variations in PaCO2 and pH compared to patients receiving manual ventilation (P < 0.01); fluctuations of arterial pH correlated with cardiac arrhythmias and cardiac arrest.[27] Zuchelo and Chiavone explored alterations of arterial pH (a change in arterial pH was defined as pH change >0.07 during transport) in 58 IHT patients and found that 17% of patients met this criterion, 8 patients had increased pH while 2 had decreased pH values.[51] After examining PaCO2 values, it was discovered that four patients had decreased PaCO2, while one had increased PaCO2. These data suggest that IHT may result in non-trivial changes in pH and PaCO2 with the associated potential for alterations in patient physiology.[51]
PERSONNEL AND EQUIPMENT CONSIDERATIONS DURING PATIENT TRANSFERS
There cannot be a discourse on the complications of IHT without addressing the importance of equipment and personnel. While IHTs should be reserved for diagnostic tests and procedures that are more likely to directly affect care, of equal importance is the presence of appropriately trained personnel, properly functioning equipment, adequate documentation, and pertinent checklists.[1,5,11,12,13,21,52,53,54,55] Frequent patient and equipment checks are vital, as is the scrupulous pre-IHT preparation of the patient.[9,21,26,56,57,58] Significant proportion of problems that occur during IHTs are related to equipment or monitoring.[52] Choi et al.[52] documented ECG lead failure (23%), monitor power failure (14%), combination of these two (10%), intravenous access (9%) or disconnection of medication infusion (5%), and ventilator disconnections (3%). Oftentimes these events were discovered at the destination site, before or after the intended test or procedure, but not during transportation. Choi et al. implemented two interventions that together played a major role in decreasing adverse events during IHT. The first was training of the transport staff in the potential hazards through a formal 4-hour course, and the second intervention involved the use of a checklist before transportation. Some organizations actually have built special transfer boards to which equipment can be attached to reduce the likelihood of adverse events,[59] which can be used as part of a “safe platform” for moving patients. It is evident that effective communication and well-trained, properly prepared staff all play an important role,[9,12,21] as well as having a viable plan at the trip destination.[60] Along the same lines, there may be additional logistical issues to solve during trips to highly restricted areas, such as the Magnetic Resonance Imaging (MRI) suite, where mechanically ventilated patients must be placed on special ventilators that do not contain magnetically sensitive components.[61] Finally, certain monitoring capabilities may be lost for brief periods of time as patients undergo specialized testing (e.g., MRI scanning).[62]
EMERGENT/UNEXPECTED SITUATIONS DURING INTRAHOSPITAL TRANSFERS
Team coordination, communications, and resources availability are vital should emergency or unexpected situations occur during IHT. Examples of some of the complexities associated with transferring critically ill patients are provided in Figure 3, with focus on different types of equipment and considerations inherent to pre-transfer planning. It is important that a formal, written protocol for IHT is developed by a multidisciplinary team and evaluated by a quality improvement process of each institution. Transport protocols should include requirements for routine checks and maintenance of equipment used during transport and at destination.[63] Organization and collaboration with other health care providers in the receiving destination should be undertaken prior to the transport. The receiving team should confirm their readiness of receiving the patient for immediate procedure or testing before the transport commences. The keys to ensuring a smooth and safe IHT include, a coordinated assumption of team management responsibility for the patient on arrival, physician-to-physician and/or nurse-to-nurse communication to review patient condition, the treatment plan, and resources availability during emergency/unexpected situation. The receiving team must be familiar with the equipment used on the transport and be experienced with management of emergency airways, ventilation, and resuscitation. The Joint Commission requires that handoff communication between licensed providers during IHT be standardized and implemented for the safe patient transfer.[64] Handoff communication should address issues related to patient monitoring, assessment, and potential intervention should it be required in case of emergency or when the unexpected occurs.[4] Should an emergency or unexpected event occur during IHT or at the receiving destination, emergent management according to the order of ABCs (i.e., airway, breathing, and circulation) should be initiated. According to the guidelines of American College of Critical Care Medicine, a blood pressure monitor, pulse oximetry, and cardiac monitor/defibrillator should accompany every high-acuity IHT without exception, in addition to equipment for emergency airway management and an oxygen source to provide for projected needs plus an extra 30-minute reserve.[9] In patients with specialty-specific needs (e.g., trauma, respiratory failure, neurocritical care), capnometry, and further monitoring (e.g., intracranial pressure monitor) may be beneficial, as appropriate. The minimal requirements in IHT destination locations include suction device, an oxygen source, accessible electric connections, monitoring devices of equal caliber to the ICU, and a readily available “crash cart”.[37,65]
In terms of basic resuscitation drugs for cardiac arrest or arrhythmia, inotropes, vasopressors, and anti-arrhythmic medications should be available for the transport. In addition, a more complete array of commonly used pharmaceuticals, such as sedatives and narcotic analgesics, calcium, and bicarbonate should be available for transportation, and at the receiving location. An ample supply of appropriate intravenous fluids and continuous drip medications should also be ensured. Since most of critically ill patients are on mechanical ventilation, mechanical ventilation equipment should be available at the receiving location as mentioned above. Comprehensive listings of potential risk factors and preventive measures for IHT-related complications are provided in Tables 3 and 4.
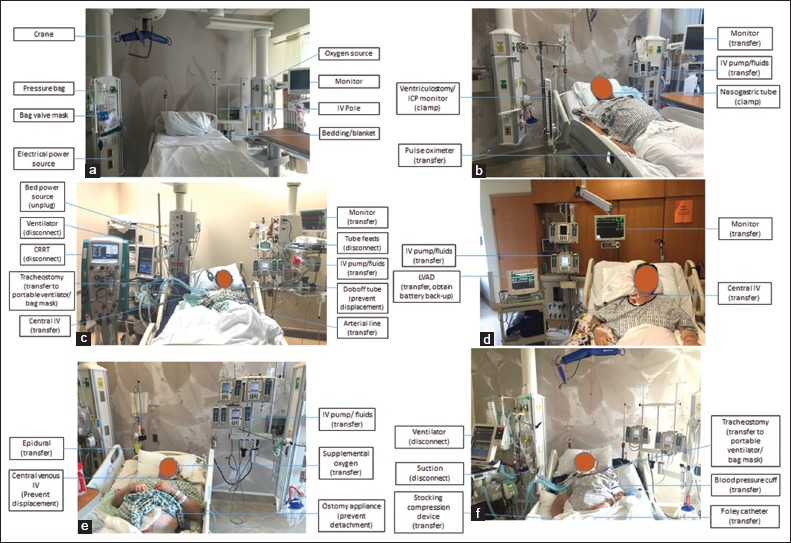
Table 3.
Risk factors for complications during intrahospital transportation
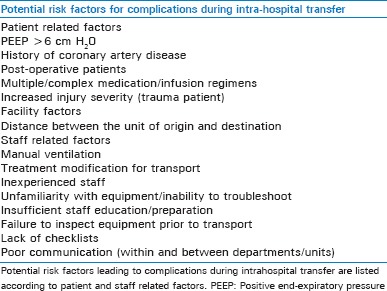
Table 4.
Prevention strategies for complications arising during intrahospital transport of intensive care unit patients
CONCLUSION
During IHT patients are at risk for significant adverse events, such as airway/pulmonary complications, hemodynamic perturbations (including cardiac arrest), nosocomial infections, acid/base disturbances, and glucose abnormalities. True mortality estimates from IHT are challenging because mortalities resulting from IHT often cannot distinguished from those of the general ICU population.[1,2] Transportation of critically ill patients should only occur when the benefits of a procedure or diagnostic test outweigh the risks. Moving these patients should only happen when there is appropriate monitoring and other necessary equipment in the presence of trained personnel who are familiar with the care of such patients.
We encourage societies, hospital systems, and departments to promulgate guidelines for IHT-specific care of critically ill patients. Further research on best practices for IHT of these patients should be pursued, thereby allowing for the implementation of targeted prevention and treatment strategies during IHT.[52,53] Such efforts will ultimately improve overall patient safety and potentially reduce healthcare associated costs arising from preventable complications.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Schwebel C, Clec’h C, Magne S, Minet C, Garrouste-Orgeas M, Bonadona A, et al. OUTCOMEREA Study Group. Safety of intrahospital transport in ventilated critically ill patients: A multicenter cohort study*. Crit Care Med. 2013;41:1919–28. doi: 10.1097/CCM.0b013e31828a3bbd. [DOI] [PubMed] [Google Scholar]
- 2.Szem JW, Hydo LJ, Fischer E, Kapur S, Klemperer J, Barie PS. High-risk intrahospital transport of critically ill patients: Safety and outcome of the necessary “road trip”. Crit Care Med. 1995;23:1660–6. doi: 10.1097/00003246-199510000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Waddell G. Movement of criticall ill patients within hospital. Br Med J. 1975;2:417–9. doi: 10.1136/bmj.2.5968.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stawicki SP, Galwankar SC, Papadimos TJ, Moffatt-Bruce SD. Gurgaon, Haryana, India: Wolters Kluwer Health (India) Pvt. Ltd; 2014. Fundamentals of Patient Safety in Medicine and Surgery; pp. 5–78. [Google Scholar]
- 5.Parmentier-Decrucq E, Poissy J, Favory R, Nseir S, Onimus T, Guerry MJ, et al. Adverse events during intrahospital transport of critically ill patients: Incidence and risk factors. Ann Intensive Care. 2013;3:10. doi: 10.1186/2110-5820-3-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pascual JL, Blank NW, Holena DN, Robertson MP, Diop M, Allen SR, et al. There's no place like home: Boarding surgical ICU patients in other ICUs and the effect of distances from the home unit. J Trauma Acute Care Surg. 2014;76:1096–102. doi: 10.1097/TA.0000000000000180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nuckols TK. Reducing the risks of intrahospital transport among critically ill patients*. Crit Care Mede. 2013;41:2044–5. doi: 10.1097/CCM.0b013e31828fd714. [DOI] [PubMed] [Google Scholar]
- 8.Stawicki SP, Pryor JP, Hyams ES, Gupta R, Gracias VH, Schwab CW. The surgeon and the intensivist: Reaching consensus in intensive care triage. J SurgEduc. 2007;64:289–93. doi: 10.1016/j.jsurg.2007.05.008. [DOI] [PubMed] [Google Scholar]
- 9.Warren J, Fromm RE, Jr, Orr RA, Rotello LC, Horst HM. American College of Critical Care Medicine. Guidelines for the inter- and intrahospital transport of critically ill patients. Crit Care Med. 2004;32:256–62. doi: 10.1097/01.CCM.0000104917.39204.0A. [DOI] [PubMed] [Google Scholar]
- 10.Quenot JP, Milési C, Cravoisy A, Capellier G, Mimoz O, Fourcade O, et al. Intrahospital transport of critically ill patients (excluding newborns) recommendations of the SociétédeRéanimationdeLangueFrançaise (SRLF), the SociétéFrançaised’AnesthésieetdeRéanimation (SFAR), and the SociétéFrançaisedeMédecined’Urgence (SFMU) Ann Intensive Care. 2012;2:1. doi: 10.1186/2110-5820-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nakayama DK, Lester SS, Rich DR, Weidner BC, Glenn JB, Shaker IJ. Quality improvement and patient care checklists in intrahospital transfers involving pediatric surgery patients. J Pediatr Surg. 2012;47:112–8. doi: 10.1016/j.jpedsurg.2011.10.030. [DOI] [PubMed] [Google Scholar]
- 12.Stearley HE. Patients’ outcomes: Intrahospital transportation and monitoring of critically ill patients by a specially trained ICU nursing staff. Am J Crit Care. 1998;7:282–7. [PubMed] [Google Scholar]
- 13.Picetti E, Antonini MV, Lucchetti MC, Pucciarelli S, Valente A, Rossi I, et al. Intra-hospital transport of brain-injured patients: A prospective, observational study. Neurocrit Care. 2013;18:298–304. doi: 10.1007/s12028-012-9802-1. [DOI] [PubMed] [Google Scholar]
- 14.Blay N, Duffield CM, Gallagher R, Roche M. A systematic review of time studies to assess the impact of patient transfers on nurse workload. Int J NursPract. 2014;20:662–73. doi: 10.1111/ijn.12290. [DOI] [PubMed] [Google Scholar]
- 15.Shields J, Overstreet M, Krau SD. Nurse knowledge of intrahospital transport. NursClin North Am. 2015;50:293–314. doi: 10.1016/j.cnur.2015.03.005. [DOI] [PubMed] [Google Scholar]
- 16.Stawicki SP, Stoltzfus JC, Aggarwal P, Bhoi S, Bhatt S, Kalra OP, et al. Academic College of Emergency Experts in India's INDO-US Joint Working Group and OPUS12 Foundation Consensus Statement on Creating A Coordinated, Multi-Disciplinary, Patient-Centered, Global Point-of-Care Biomarker Discovery Network. Int J CritIlln Inj Sci. 2014;4:200–8. doi: 10.4103/2229-5151.141398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peace K, Maloney-Wilensky E, Frangos S, Hujcs M, Levine J, Kofke WA, et al. Portable head CT scan and its effect on intracranial pressure, cerebral perfusion pressure, and brain oxygen. Journal of neurosurgery. 2011;114:1479–84. doi: 10.3171/2010.11.JNS091148. [DOI] [PubMed] [Google Scholar]
- 18.Leong CS, Cascade PN, Kazerooni EA, Bolling SF, Deeb GM. Bedside chest radiography as part of a postcardiac surgery critical care pathway: A means of decreasing utilization without adverse clinical impact. Crit Care Med. 2000;28:383–8. doi: 10.1097/00003246-200002000-00016. [DOI] [PubMed] [Google Scholar]
- 19.Stawicki SP, Seamon MJ, Meredith DM, Chovanes J, Paszczuk A, Kim PK, et al. Transthoracic echocardiography for suspected pulmonary embolism in the intensive care unit: Unjustly underused or rightfully ignored? J Clin Ultrasound. 2008;36:291–302. doi: 10.1002/jcu.20461. [DOI] [PubMed] [Google Scholar]
- 20.Stawicki SP, Seamon MJ, Kim PK, Meredith DM, Chovanes J, Schwab CW, et al. Transthoracic echocardiography for pulmonary embolism in the ICU: Finding the “right” findings. J Am Coll Surg. 2008;206:42–7. doi: 10.1016/j.jamcollsurg.2007.06.293. [DOI] [PubMed] [Google Scholar]
- 21.Beckmann U, Gillies DM, Berenholtz SM, Wu AW, Pronovost P. Incidents relating to the intra-hospital transfer of critically ill patients. An analysis of the reports submitted to the Australian Incident Monitoring Study in Intensive Care. Intensive Care Med. 2004;30:1579–85. doi: 10.1007/s00134-004-2177-9. [DOI] [PubMed] [Google Scholar]
- 22.de Lassence A, Timsit JF, Tafflet M, Azoulay E, Jamali S, Vincent F, et al. OUTCOMEREA Study Group. Pneumothorax in the intensive care unit: Incidence, risk factors, and outcome. Anesthesiology. 2006;104:5–13. doi: 10.1097/00000542-200601000-00003. [DOI] [PubMed] [Google Scholar]
- 23.GarrousteOrgeas M, Timsit JF, Soufir L, Tafflet M, Adrie C, Philippart F, et al. Outcomerea Study Group. Impact of adverse events on outcomes in intensive care unit patients. Crit Care Med. 2008;36:2041–7. doi: 10.1097/CCM.0b013e31817b879c. [DOI] [PubMed] [Google Scholar]
- 24.Sanchez-Pinto N, Giuliano JS, Schwartz HP, Garrett L, Gothard MD, Kantak A, et al. The impact of postintubation chest radiograph during pediatric and neonatal critical care transport. Pediatr Crit Care Med. 2013;14:e213–7. doi: 10.1097/PCC.0b013e3182772e13. [DOI] [PubMed] [Google Scholar]
- 25.Venkategowda PM, Rao SM, Mutkule DP, Taggu AN. Unexpected events occurring during the intra-hospital transport of critically ill ICU patients. Indian J Crit Care Med. 2014;18:354–7. doi: 10.4103/0972-5229.133880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Papson JP, Russell KL, Taylor DM. Unexpected events during the intrahospital transport of critically ill patients. Acad Emerg Med. 2007;14:574–7. doi: 10.1197/j.aem.2007.02.034. [DOI] [PubMed] [Google Scholar]
- 27.Braman SS, Dunn SM, Amico CA, Millman RP. Complications of intrahospital transport in critically ill patients. Ann Intern Med. 1987;107:469–73. doi: 10.7326/0003-4819-107-4-469. [DOI] [PubMed] [Google Scholar]
- 28.Mazza BF, Amaral JL, Rosseti H, Carvalho RB, Senna AP, Guimarães HP, et al. Safety in intrahospital transportation: Evaluation of respiratory and hemodynamic parameters. A prospective cohort study. Sao Paulo Med J. 2008;126:319–22. doi: 10.1590/S1516-31802008000600005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taylor JO, Chulay, Landers CF, Hood W, Jr, Abelman WH. Monitoring high-risk cardiac patients during transportation in hospital. Lancet. 1970;2:1205–8. doi: 10.1016/s0140-6736(70)92176-8. [DOI] [PubMed] [Google Scholar]
- 30.Geevarghese KP. Postoperative care of the patient undergoing neurological surgery. Int Anesthesiol Clin. 1977;15:309–20. [PubMed] [Google Scholar]
- 31.Damm C, Vandelet P, Petit J, Richard JC, Veber B, Bonmarchand G, et al. Complications during the intrahospital transport in critically ill patients. Ann Fr Anesth Reanim. 2005;24:24–30. doi: 10.1016/j.annfar.2004.10.026. [DOI] [PubMed] [Google Scholar]
- 32.Gillman L, Leslie G, Williams T, Fawcett K, Bell R, McGibbon V. Adverse events experienced while transferring the critically ill patient from the emergency department to the intensive care unit. Emerg Med J. 2006;23:858–61. doi: 10.1136/emj.2006.037697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vincent JL, Rello J, Marshall J, Silva E, Anzueto A, Martin CD, et al. International study of the prevalence and outcomes of infection in intensive care units. JAMA. 2009;302:2323–9. doi: 10.1001/jama.2009.1754. [DOI] [PubMed] [Google Scholar]
- 34.Kalra S, Kelkar D, Galwankar SC, Papadimos TJ, Stawicki SP, Arquilla B, et al. The emergence of ebola as a global health security threat: From ‘lessons learned’ to coordinated multilateral containment efforts. J Glob Infect Dis. 2014;6:164–77. doi: 10.4103/0974-777X.145247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schmidt JM. Stopping the chain of infection in the radiology suite. RadiolTechnol. 2012;84:31–51. [PubMed] [Google Scholar]
- 36.Kollef MH, Von Harz B, Prentice D, Shapiro SD, Silver P, St John R, et al. Patient transport from intensive care increases the risk of developing ventilator-associated pneumonia. Chest. 1997;112:765–73. doi: 10.1378/chest.112.3.765. [DOI] [PubMed] [Google Scholar]
- 37.Bercault N, Wolf M, Runge I, Fleury JC, Boulain T. Intrahospital transport of critically ill ventilated patients: A risk factor for ventilator-associated pneumonia--a matched cohort study. Crit Care Med. 2005;33:2471–8. doi: 10.1097/01.ccm.0000185644.54646.65. [DOI] [PubMed] [Google Scholar]
- 38.Fried LC. Cervical spinal cord injury during skeletal traction. JAMA. 1974;229:181–3. [PubMed] [Google Scholar]
- 39.Conrad BP, Rossi GD, Horodyski MB, Prasarn ML, Alemi Y, Rechtine GR. Eliminating log rolling as a spine trauma order. SurgNeurolInt. 2012;3(Suppl 3):S188–97. doi: 10.4103/2152-7806.98584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hastings RH, Marks JD. Airway management for trauma patients with potential cervical spine injuries. AnesthAnalg. 1991;73:471–82. doi: 10.1213/00000539-199110000-00019. [DOI] [PubMed] [Google Scholar]
- 41.Poole GV, Miller JD, Agnew SG, Griswold JA. Lower extremity fracture fixation in head-injured patients. J Trauma. 1992;32:654–9. doi: 10.1097/00005373-199205000-00019. [DOI] [PubMed] [Google Scholar]
- 42.Van Meter JW, Branick RI. Bilateral genu recurvatum after skeletal traction. A case report. J Bone Joint Surg Am. 1980;62:837–9. [PubMed] [Google Scholar]
- 43.Bach JA, Leskovan JJ, Scharschmidt T, Boulger CT, Papadimos TJ, Russell S, et al. The right team at the right time: Multidisciplinary approach to multi-trauma patient with orthopedic injuries. OPUS 12 Scientist. 2012;6:6–10. doi: 10.4103/IJCIIS.IJCIIS_5_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Andrews PJ, Piper IR, Dearden NM, Miller JD. Secondary insults during intrahospital transport of head-injured patients. Lancet. 1990;335:327–30. doi: 10.1016/0140-6736(90)90614-b. [DOI] [PubMed] [Google Scholar]
- 45.Wisler JR, Beery PR, 2nd, Steinberg SM, Stawicki SP. Rijeka, Croatia: InTech; 2012. Competing Priorities in the Brain Injured Patient: Dealing with the Unexpected. Brain Injury: Pathogenesis, Monitoring, Recovery and Management; pp. 341–54. [Google Scholar]
- 46.Stawicki SP, Gerlach AT. Polypharmacy and medication errors: Stop, listen, look, and analyze. OPUS 12 Scientist. 2009;3:6–10. [Google Scholar]
- 47.Cipolla J, Baillie DR, Steinberg SM, Martin ND, Jaik NP, Lukaszczyk JJ, et al. Negative pressure wound therapy: Unusual and innovative applications. OPUS 12 Scientist. 2008;2:15–29. [Google Scholar]
- 48.Stawicki SP, Schuster D, Liu JF, Kamal J, Erdal S, Gerlach AT, et al. The glucogram: A new quantitative tool for glycemic analysis in the surgical intensive care unit. Int J CritIlln Inj Sci. 2011;1:5–12. doi: 10.4103/2229-5151.79275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pappada SM, Cameron BD, Tulman DB, Bourey RE, Borst MJ, Olorunto W, et al. Evaluation of a model for glycemic prediction in critically ill surgical patients. PloS One. 2013;8:e69475. doi: 10.1371/journal.pone.0069475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Raghavan M, Marik PE. Management of sepsis during the early “golden hours”. J Emerg Med. 2006;31:185–99. doi: 10.1016/j.jemermed.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 51.Zuchelo LT, Chiavone PA. Intrahospital transport of patients on invasive ventilation: Cardiorespiratory repercussions and adverse events. J Bras Pneumol. 2009;35:367–74. doi: 10.1590/s1806-37132009000400011. [DOI] [PubMed] [Google Scholar]
- 52.Choi HK, Shin SD, Ro YS, Kim do K, Shin SH, Kwak YH. A before- and after-intervention trial for reducing unexpected events during the intrahospital transport of emergency patients. Am J Emerg Med. 2012;30:1433–40. doi: 10.1016/j.ajem.2011.10.027. [DOI] [PubMed] [Google Scholar]
- 53.Berube M, Bernard F, Marion H, Parent J, Thibault M, Williamson DR, et al. Impact of a preventive programme on the occurrence of incidents during the transport of critically ill patients. Intensive Crit Care Nurs. 2013;29:9–19. doi: 10.1016/j.iccn.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 54.Jarden RJ, Quirke S. Improving safety and documentation in intrahospital transport: Development of an intrahospital transport tool for critically ill patients. Intensive Crit Care Nurs. 2010;26:101–7. doi: 10.1016/j.iccn.2009.12.007. [DOI] [PubMed] [Google Scholar]
- 55.Brunsveld-Reinders AH, Arbous MS, Kuiper SG, de Jonge E. A comprehensive method to develop a checklist to increase safety of intra-hospital transport of critically ill patients. Crit Care. 2015;19:214. doi: 10.1186/s13054-015-0938-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lovell MA, Mudaliar MY, Klineberg PL. Intrahospital transport of critically ill patients: Complications and difficulties. Anaesth Intensive Care. 2001;29:400–5. doi: 10.1177/0310057X0102900412. [DOI] [PubMed] [Google Scholar]
- 57.Shirley PJ, Bion JF. Intra-hospital transport of critically ill patients: Minimising risk. Intensive Care Med. 2004;30:1508–10. doi: 10.1007/s00134-004-2293-6. [DOI] [PubMed] [Google Scholar]
- 58.Lahner D, Nikolic A, Marhofer P, Koinig H, Germann P, Weinstabl C, et al. Incidence of complications in intrahospital transport of critically ill patients--experience in an Austrian university hospital. Wien Klin Wochenschr. 2007;119:412–6. doi: 10.1007/s00508-007-0813-4. [DOI] [PubMed] [Google Scholar]
- 59.Matsumura Y, Nakada TA, Hayashi Y, Oshima T, Oda S. Intrahospital transport of mechanically ventilated intensive care patients using new equipment attached to a transfer board. Acute Medicine and Surgery. 2015;2:219–22. doi: 10.1002/ams2.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ott LK, Pinsky MR, Hoffman LA, Clarke SP, Clark S, Ren D, et al. Patients in the radiology department may be at increased risk of developing critical instability. J Radiol Nurs. 2015;34:29–34. doi: 10.1016/j.jradnu.2014.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Feldman JM, Kalli I. Equipment and environmental issues for nonoperating room anesthesia. Curr Opin Anaesthesiol. 2006;19:450–2. doi: 10.1097/01.aco.0000236148.90988.36. [DOI] [PubMed] [Google Scholar]
- 62.Karlik SJ, Heatherley T, Pavan F, Stein J, Lebron F, Rutt B, et al. Patient anesthesia and monitoring at a 1.5-T MRI installation. Magn Reson Med. 1988;7:210–21. doi: 10.1002/mrm.1910070209. [DOI] [PubMed] [Google Scholar]
- 63.Australasian College for Emergency Medicine, Australian and New Zealand College of Anaesthetists; Joint Faculty of Intensive Care Medicine. Minimum standards for intrahospital transport of critically ill patients. Emerg Med (Fremantle) 2003;15:202–4. [PubMed] [Google Scholar]
- 64.The Joint Commission. Hand-off Communication FAQs. [Last accessed on 2015 Oct 1]. Available from: http://www.centerfortransforminghealthcare.org/faq.aspx?CategoryId=51#1115 .
- 65.McLenon M. Use of a specialized transport team for intrahospital transport of critically ill patients. Dimens Crit Care Nurs. 2004;23:225–9. doi: 10.1097/00003465-200409000-00008. [DOI] [PubMed] [Google Scholar]


