Abstract
Background:
Post traumatic osteonecrosis of a vertebral body occurring in a delayed fashion was first described by the German doctor Kümmell in 1895. Several studies have reported percutaneous vertebroplasty (PVP), or percutaneous kyphoplasty (PKP) for Kümmell's disease achieves good outcomes. However, it is unknown whether a technique is superior for the treatment of this disease. The objective of the study is to compare the efficacy of PVP and PKP for the treatment of Kümmell's disease.
Materials and Methods:
A retrospective review was conducted for 73 patients with Kümmell's disease. PVP was performed in 38 patients and PKP in 35 patients. Visual analogue score (VAS) was used to evaluate pain. The anterior vertebral height was measured. The operative time, the incidence of cement leakage and the costs were recorded.
Results:
In both PVP group and PKP group, the VAS and anterior vertebral height significantly improved at 1-day postoperatively (P < 0.05), and the improvement sustained at the final followup (P > 0.05). Between the PVP and PKP groups, there were no significant differences in VAS and the anterior vertebral height at 1-day postoperatively and at the final followup (P > 0.05). The operating time and expense in the PKP group were higher than the PVP group (P < 0.001). Cement leakages in the PKP group were fewer than PVP group (P < 0.05).
Conclusions:
PVP is a faster, less expensive option that still provides a comparable pain relief and restoration of vertebral height to PKP for the treatment of Kümmell's disease. PKP has a significant advantage over PVP in term of the fewer cement leakages.
Keywords: Intravertebral cleft, intravertebral vacuum phenomenon, Kümmell's disease, kyphoplasty, vertebroplasty
Mesh terms: Osteonecrosis, aseptic necrosis of bone, avascular necrosis of bone, vertebrae, vertebroplasty, bone cements
INTRODUCTION
The intravertebral vacuum phenomenon (IVP), also termed “intravertebral vacuum cleft,” is an uncommon condition that was first reported by Maldague et al.1 It refers to a prominent gaseous radiolucency within a collapsed vertebral body seen on computed tomography (CT) scan or a plain radiograph. IVP visualized on plain radiograph is highly suggestive of Kümmell's disease, which is an eponymous term used to describe avascular necrosis of a vertebral body that occurred in a delayed fashion after a minor trauma. It is distinguished from typical osteoporotic fractures because the symptoms develop in a delayed fashion.
Gas noted on plain radiographs is expected to be hypointense on both T1 and T2 magnetic resonance imaging (MRI) sequences. The authors have reported that the vacuum cleft is observed as hypointense signal on T1-weighted images. However, on T2-weighted images, this area may be either hypointense or hyperintense.2 In a report by Malghem et al.2 patients with the vacuum sign were serially imaged. Initially, MRI demonstrated a hypointense gas-filled cleft; however, following prolonged supine positioning, a hyperintense signal appeared on the T2 sequences, indicating the presence of fluid. Reports suggest that the presence of IVP is highly suggestive of a benign sign,1,3,4 but IVP occurs rarely in patients with spinal infections and spinal malignancies, for examples, multiple myeloma,5 the non-Hodgkin's lymphoma.6
Several studies have reported percutaneous vertebroplasty (PVP)7,8 or percutaneous kyphoplasty (PKP)9,10 for Kümmell's disease achieves good outcomes. However, it is unknown whether a technique is superior. The objectives of this study were to evaluate and compare the efficacy of PVP and PKP for the treatment of Kümmell's disease.
MATERIALS AND METHODS
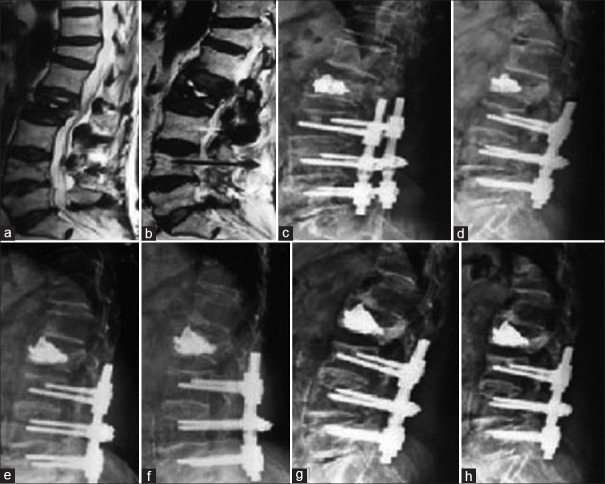
73 patients who were admitted between October 2005 and February 2013 were retrospectively reviewed. Inclusion criteria involved, single level vertebrae with IVP, in plain radiogram or CT or MRI. Exclusion criteria included patients with clinical evidence of neoplasm or infection involving the affected vertebral body, patients with neurological symptoms. PVP was performed in 38 patients, PKP was performed in 35 patients. A biopsy and tissue histopathological examination was performed for each of the cases. Most common vertebrae affected were in the thoracolumbar region (T10-L1) [Figure 1]. There was no significant difference between two groups (X2 = 0.228, P > 0.05). There were no significant differences regarding mean followup time and preoperative general clinical data in the age, gender, mean duration of symptom, preoperative visual analogue score (VAS) and preoperative anterior vertebral height between the two groups (P > 0.05) [Table 1].
Figure 1.
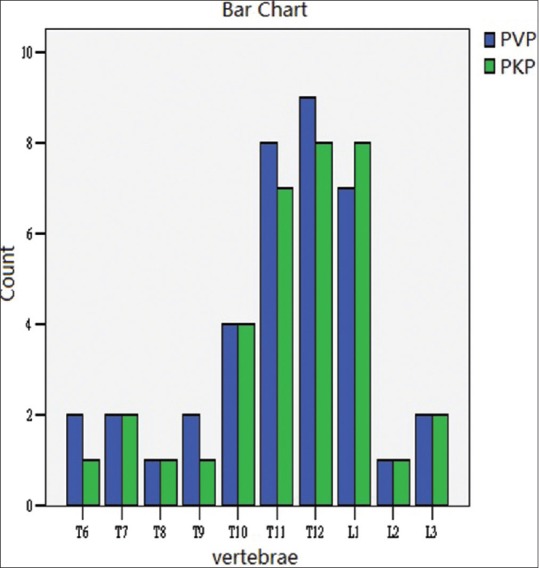
Bar diagram showing the distribution of fractures with intravertebral vacuum phenomenon. PVP = Percutaneous vertebroplasty, PKP = Percutaneous kyphoplasty
Table 1.
Demographics of patients

Operative procedure
Polymethylmethacrylate (PMMA) was injected at low viscosity directly into the cancellous bone in the PVP technique. PKP differs from PVP in that a contrast filled, inflatable balloon is inserted into the vertebral body, allowing a degree of fracture reduction and leaving a cavity behind, after withdrawal of balloon which is filled with high viscosity PMMA.
PVP was performed in an extended posture using fluoroscopic guidance under local anesthesia. Pillows were used to support the upper chest and pelvis, and the operating table was adjusted to enable maximum extension of the spinal column. First, a 4 mm (diameter) bone needle was used for puncturing. Spinal canal violation was avoided by ensuring that the medial pedicle cortex (in the anteroposterior projection) was not crossed before the posterior vertebral wall had been reached (in the lateral projection). When the needle passed the posterior vertebral wall, the stylet was removed from the trocar, which served as a working cannula. Next, a 3.5 mm (diameter) biopsy needle, which was connected to a 10 ml syringe, was used to suction out specimen and fluid. Then, a 3.5 mm pushing rod pushed PMMA bone cement into the vertebra.
Steps for performing PKP were similar to PVP as described above. However, following biopsy and additional step was performed. A deflated balloon was placed into the channel and inflated to elevate the endplates and restore the height of the vertebral body by reducing the fracture. The balloon was then deflated and withdrawn, and then PMMA was manually injected under fluoroscopic guidance. After operation, antiosteoporotic drug (including calcitonin 600 mg/day, 1α-hydroxy vitamin D3 0.5 μg/day and alendronate 70 mg weekly tablet) were used regularly for 2 years.(the longest followup duration of the study is 2 years).
A VAS that ranged from 0 (no pain) to 10 (maximal pain) was used to assess pain severity preoperatively, postoperatively and at the final followup. Preoperative imaging included standing anteroposterior and lateral radiographs, CT scans, and MRI. After surgery, all patients underwent standing anteroposterior and lateral radiographs. The vertebral height was measured in millimeters along the anterior of the fractured vertebral body. Two independent, experienced orthopedists measured the radiological variable 2 times, with an internal time of 3 days. The inter- and intra-observer reproducibility of the radiological variable is good.
The rate of cement leakages and refracture were determined postoperatively using radiographs. The costs, amounts of cement injected and operating time of the two procedures were recorded.
Statistical analysis
SPSS 19.0 statistical software (SPSS, Inc., Chicago, IL, USA) was used for analysis. Comparisons were made before and at each followup appointment after PVP or PKP. Independent samples t-tests were performed to compare the age, mean followup time, mean duration of symptoms, anterior vertebral height, VAS, costs, cement volume, operating time between two groups, paired t-tests were performed to compare the anterior vertebral height and VAS in the same group. Chi-squared tests were performed to compare the rates of cement leakages and refracture, gender, the distribution of the affected vertebrae with IVP. P < 0.05 was considered as statistically significant.
RESULTS
Intraoperative biopsies from all cases confirms bone necrosis. In the PVP group, the average anterior vertebral body heights increased from 11.66 mm preoperatively to 19.50 mm at the 1-day postoperatively, 19.02 mm at the final followup. In the PKP group, the average anterior vertebral body heights increased from 10.65 mm preoperatively to 20.94 mm at the 1-day postoperatively, 20.52 mm at the final followup (mean 17 month, range 12 -24 month). There were significant improvements in both groups P < 0.001) in the anterior vertebral body heights at the 1-day postoperatively and at the final followup compared with the preoperative values [Table 2], this improvement was maintained at the finial followup (P > 0.05). However, there were no differences in terms of the anterior vertebral body heights at the 1-days postoperatively and at the final followup between the PVP group and PKP groups (P > 0.05) [Table 2].
Table 2.
VAS and anterior vertebral height before and after operation
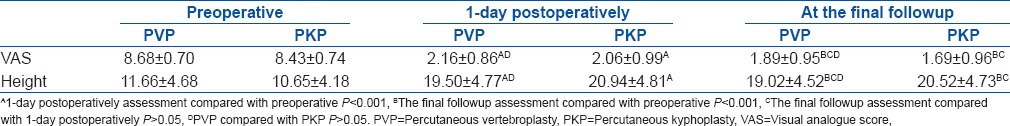
In the PVP group, the mean VAS decreased from 8.68 preoperatively to 2.16 at the 1-day postoperatively, 1.89 at the final follow up. In the PKP group, the mean VAS decreased from 8.43 preoperatively to 2.06 at the 1-day postoperatively, 1.69 at the final follow up. There were significant improvements in both groups P < 0.001) in the VAS at the 1-day postoperatively and the final followup compared with the preoperative values, this improvement was maintained at the finial followup (P > 0.05). However, no differences (P > 0.05) were found between the two groups with respect to the VAS at the one day postoperatively and at the final followup [Table 2].
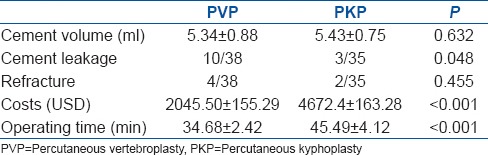
The mean amount of cement used in PVP group 5.34 ml, PKP 5.43 ml, and no significant differences were found (P > 0.05) [Table 3]. Cement leakages were observed in 10 cases in the PVP group (26.3%) and in 3 cases in the PKP group (8.6%), all were asymptomatic, this difference was statistically significant (P < 0.05). During mean 17 months followup, there were four new osteoporotic vertebral fractures in PVP group and two new osteoporotic vertebral fractures in PKP group, this difference was not statistically significant (P > 0.05). Of these new fractures, one vertebra in PVP group and one vertebrae in PKP group were fractures in adjacent vertebrae, others were fractures in remote vertebrae. The mean cost in PVP group was 2045.5 USD, however, the cost in PKP group was 4672.4 USD. The cost in PKP was higher than PVP, this difference was statistically significant P < 0.001). The mean operating time in PVP group was 34.68 min range (31-41 min), however, the mean operating time in PKP group was 45.49 min (range 31-54 min). The mean operating time was significantly reduced using the PVP technique, this difference was statistically significant P < 0.001).
Table 3.
The amounts of cement injected, the rate of cement leakage, the rate of refracture, costs, operating time
DISCUSSION
In 1895, Kümmell presented a series of six patients who had sustained “vertebral body collapse” after seemingly minor trauma.11 With the advent of radiography, it was attributed to a delayed posttraumatic vertebral compression fracture. Recently, multiple synonymous terms have been used to describe Kümmell's disease, including intravertebral vacuum cleft,2,3,6,12,13,14 intravertebral cleft,15,16,17,18 intravertebral pseudoarthrosis,7,19 vertebral osteonecrosis,8 vertebral fluid collection associated with vertebral collapse20 and delayed posttraumatic vertebral collapse.21,22 Maldague et al.1 first reported the IVP sign on X-ray, which was described as pathognomonic for Kümmell's disease. Later, some articles have the same result.1,3,4 However, others have reported that IVP occurs rarely in patients with spinal infection and in patients with tumor.5 We had reported one patient with IVP was diagnosed as non-Hodgkin's lymphoma.6 Hence, IVP is not pathognomonic for Kümmell's disease, only highly suggestive of this disease. In this study, according to the duration of symptom, the cleft sign, postoperative pathological result, all patients were diagnosed with Kümmell's disease.
Treatment of symptomatic Kümmell's disease depends on the severity of the patient's pain and the presence of any neurological deficits. In patients without any neurological symptoms, PVP7,8 or PKP9,10 is used. Both have been shown to restore vertebral height and alleviate pain markedly. Pain relief is thought to be due to the elimination of motion at the fracture site by cementing.16,17,18 We agree that filling the entire cleft with cement is important to ensure a pain free postoperative period.16,17,18 In our study, one patient required a second PVP due to persistent pain and incomplete filling following an initial PVP at another hospital. Following the second PVP, the cleft opacified completely and the pain alleviated [Figure 2]. For all the other patients in both PVP group and PKP group, the cleft was opacified completely, at the 1-day postoperatively pain was markedly relieved. After the mean followup of 17 months, the pain relief and vertebral height were maintained in both groups. These results suggest that once cleft opacification is completely achieved, PMMA provides stabilization and pain relief.
Figure 2.
82-year-old female with lumbar decompression and pedicle screw fixation 8 years ago, with severe lumbar pain since 3 months, especially when changing positions (a-b) Preoperative magnetic resonance imaging showing intravertebral vacuum phenomenon at L2. (c-d) After PVP in another hospital, cleft is not opacified completely, flexion extension lateral film shows L2 is unstable (e-f) After repeated PVP in our hospital, flexion extension lateral film shows L2 is stable. (g-h) After 1-year followup, there is callus along the anterior margin of L1 and L2 with no cement dislodgement
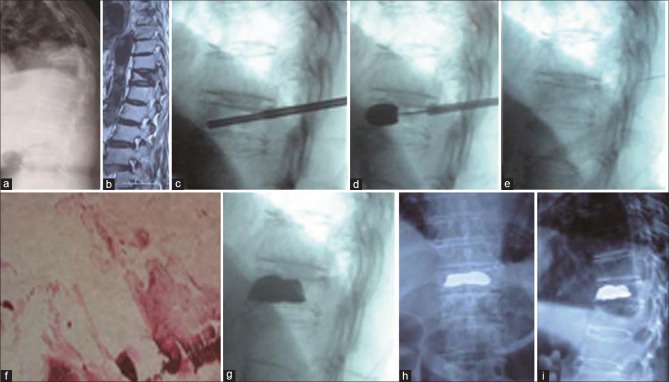
Compared to PVP, PKP has been shown to be more effective at reducing the kyphosis and restoring the height of the vertebral body, as well as reducing the risk of cement extravasation.10Jan g et al.7 reported that, the mean corrected vertebral height between pre and post treatment was 7.0 mm when they used PVP for treatment of intervertebral pseudarthrosis. Yang et al.10 reported in their 21 Kümmell's patients, after kyphoplasty, the anterior height of the vertebrae was restored from 63.5% ±8.9% to 84.4% ±11.2%. In this study, at the 1-day postoperatively, we found the restoration of the anterior vertebral height was from 11.66 ± 4.68 mm to 19.50 ± 4.77 mm in PVP group, from 10.65 ± 4.18 mm to 20.94 ± 4.81 mm in PKP group, there was no statistically difference (P > 0.05). The reason is related to the entity of Kümmell's disease. For Kümmell's disease, the vertebral height varies with postural changes because of the cleft (pseudarthrosis) and thus the anterior vertebral height can be significantly corrected in an extended posture [Figures 2 and 3]. The most common complication of PVP and PKP is cement leakage. Krauss et al.23 reported during PVP, cement leakage occurred in 18.2% of clefts and 46% of regular osteoporotic fractures. The cement leakage rate was significantly lower in the cleft group P < 0.001), they thought, the reason might be that an intravertebral cleft is surrounded by a fibrocartilaginous membrane. For patients with cleft, we had the higher rate of cement leakage (26.3%) during PVP than Krauss et al.22 Maybe, the reason was that we injected more amount of cement (mean, 5.34 ml) than Krauss et al.22 (mean, 3.1 ml). Wang et al.24 reported that in their 27 patients with cleft, 2 cases (7.4%) occurred cement leakage during PKP. In our study, although the amount of cement injected was no significant difference between PKP group (mean, 5.43 ml) and PVP group (mean, 5.34 ml), PKP group had fewer cement leakages (8.6%) than PVP group (26.3%), and there was a significant difference between two groups (P < 0.05). Maybe, the expansion of the balloon tamp compacting cancellous bone in the intravertebral cavity can reduce the rate of cement leakage.
Figure 3.
71 year old female had a compression fracture of T11. (a) Standing lateral radiograph showing T11 fracture and local kyphosis (b) Magnetic resonance imaging showing the coexistence of both air and fluid in the T11 (c-d) Intraoperative fluoroscopy showing balloon inflated (e) Intraoperative fluoroscopy showing restoration of height of D11 (f) Histopathological report showing necrotic tissue. (g) Postoperative lateral fluoroscopy view showing well filled cement (h-i) Followup (18 months) x-rays anteroposterior and lateral views dorsal spine showing well filled cement and no dislodgement after surgery
In our study, the mean cost in the PVP group was 2045.5 USD. In contrast, the mean cost in the PKP group was 4672.4 USD. It seems that PVP has an advantage over PKP, considering the higher cost of PKP. In our study, the mean operating time in PVP group was 34.68 min, the mean operating time in PKP group was 45.49 min, PVP group has a lower operating time than PKP group P < 0.001). Hence, PVP is a faster, less expense option than PKP for the treatment of Kümmell's disease. A previous study hypothesized that the osteolysis rate among patients with Kümmell's disease is greater than the rate of bone callus formation.25 Following PVP or PKP, accelerated osteolysis occurs and may displace the bone cement.26,27 No cement dislodgement was observed in our study, maybe it was related to regular usage of the antiosteoporotic drug postoperatively.
The limitations of this study were that it was a retrospective study and has the short followup period. Due to the small incidence of this disease, the numbers of patients were relatively small. A prospective large study with long term followup is needed to verify the conclusion.
To conclude, both PVP and PKP are effective for Kümmell's disease. There were no statistically significant differences in pain relief and restoration of vertebral height between the two methods for the treatment of this disease. PVP is a faster, less expense option than PKP, PKP has a significant advantage over PVP in term of the fewer cement leakages for the treatment of this disease.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Maldague BE, Noel HM, Malghem JJ. The intravertebral vacuum cleft: A sign of ischemic vertebral collapse. Radiology. 1978;129:23–9. doi: 10.1148/129.1.23. [DOI] [PubMed] [Google Scholar]
- 2.Malghem J, Maldague B, Labaisse MA, Dooms G, Duprez T, Devogelaer JP, et al. Intravertebral vacuum cleft: Changes in content after supine positioning. Radiology. 1993;187:483–7. doi: 10.1148/radiology.187.2.8475295. [DOI] [PubMed] [Google Scholar]
- 3.Bhalla S, Reinus WR. The linear intravertebral vacuum: A sign of benign vertebral collapse. AJR Am J Roentgenol. 1998;170:1563–9. doi: 10.2214/ajr.170.6.9609175. [DOI] [PubMed] [Google Scholar]
- 4.Libicher M, Appelt A, Berger I, Baier M, Meeder PJ, Grafe I, et al. The intravertebral vacuum phenomen as specific sign of osteonecrosis in vertebral compression fractures: Results from a radiological and histological study. Eur Radiol. 2007;17:2248–52. doi: 10.1007/s00330-007-0684-0. [DOI] [PubMed] [Google Scholar]
- 5.Feng SW, Chang MC, Wu HT, Yu JK, Wang ST, Liu CL. Are intravertebral vacuum phenomena benign lesions? Eur Spine J. 2011;20:1341–8. doi: 10.1007/s00586-011-1789-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang GQ, Gao YZ, Zheng J, Luo JP, Tang C, Chen SL, et al. Posterior decompression and short segmental pedicle screw fixation combined with vertebroplasty for Kümmell's disease with neurological deficits. Exp Ther Med. 2013;5:517–22. doi: 10.3892/etm.2012.833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jang JS, Kim DY, Lee SH. Efficacy of percutaneous vertebroplasty in the treatment of intravertebral pseudarthrosis associated with noninfected avascular necrosis of the vertebral body. Spine (Phila Pa 1976) 2003;28:1588–92. [PubMed] [Google Scholar]
- 8.Do HM, Jensen ME, Marx WF, Kallmes DF. Percutaneous vertebroplasty in vertebral osteonecrosis (Kummell's spondylitis) Neurosurg Focus. 1999;7:e2. doi: 10.3171/foc.1999.7.1.4. [DOI] [PubMed] [Google Scholar]
- 9.Becker S, Tuschel A, Chavanne A, Meissner J, Ogon M. Balloon kyphoplasty for vertebra plana with or without osteonecrosis. J Orthop Surg (Hong Kong) 2008;16:14–9. doi: 10.1177/230949900801600104. [DOI] [PubMed] [Google Scholar]
- 10.Yang H, Gan M, Zou J, Mei X, Shen X, Wang G, et al. Kyphoplasty for the treatment of Kümmell's disease. Orthopedics. 2010;33:479. doi: 10.3928/01477447-20100526-07. [DOI] [PubMed] [Google Scholar]
- 11.Kümmell H. Die rarefizierende Ostitis der Wirbelkrper. Dtsch Med. 1985;21:180–1. [Google Scholar]
- 12.Theodorou DJ. The intravertebral vacuum cleft sign. Radiology. 2001;221:787–8. doi: 10.1148/radiol.2213991129. [DOI] [PubMed] [Google Scholar]
- 13.Peh WC, Gelbart MS, Gilula LA, Peck DD. Percutaneous vertebroplasty: Treatment of painful vertebral compression fractures with intraosseous vacuum phenomena. AJR Am J Roentgenol. 2003;180:1411–7. doi: 10.2214/ajr.180.5.1801411. [DOI] [PubMed] [Google Scholar]
- 14.Mirovsky Y, Anekstein Y, Shalmon E, Peer A. Vacuum clefts of the vertebral bodies. AJNR Am J Neuroradiol. 2005;26:1634–40. [PMC free article] [PubMed] [Google Scholar]
- 15.Lee SH, Cho DC, Sung JK. Catastrophic intramedullary hematoma following Kümmell's disease with large intravertebral cleft. Spine J. 2008;8:1007–10. doi: 10.1016/j.spinee.2007.07.397. [DOI] [PubMed] [Google Scholar]
- 16.Lane JI, Maus TP, Wald JT, Thielen KR, Bobra S, Luetmer PH. Intravertebral clefts opacified during vertebroplasty: Pathogenesis, technical implications, and prognostic significance. AJNR Am J Neuroradiol. 2002;23:1642–6. [PMC free article] [PubMed] [Google Scholar]
- 17.McKiernan F, Faciszewski T. Intravertebral clefts in osteoporotic vertebral compression fractures. Arthritis Rheum. 2003;48:1414–9. doi: 10.1002/art.10984. [DOI] [PubMed] [Google Scholar]
- 18.Mathis JM. Vertebroplasty for vertebral fractures with intravertebral clefts. AJNR Am J Neuroradiol. 2002;23:1619–20. [PMC free article] [PubMed] [Google Scholar]
- 19.Hasegawa K, Homma T, Uchiyama S, Takahashi H. Vertebral pseudarthrosis in the osteoporotic spine. Spine (Phila Pa 1976) 1998;23:2201–6. doi: 10.1097/00007632-199810150-00011. [DOI] [PubMed] [Google Scholar]
- 20.Dupuy DE, Palmer WE, Rosenthal DI. Vertebral fluid collection associated with vertebral collapse. AJR Am J Roentgenol. 1996;167:1535–8. doi: 10.2214/ajr.167.6.8956592. [DOI] [PubMed] [Google Scholar]
- 21.Lee CS, Yu JW, Chung SS, Suh YL, Ahn G, Ahn JM. Delayed Posttraumatic Vertebral Collapse: MR Categorization and MR-Pathology Correlation. Asian Spine J. 2007;1:32–7. doi: 10.4184/asj.2007.1.1.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Osterhouse MD, Kettner NW. Delayed posttraumatic vertebral collapse with intravertebral vacuum cleft. J Manipulative Physiol Ther. 2002;25:270–5. doi: 10.1067/mmt.2002.123164. [DOI] [PubMed] [Google Scholar]
- 23.Krauss M, Hirschfelder H, Tomandl B, Lichti G, Bär I. Kyphosis reduction and the rate of cement leaks after vertebroplasty of intravertebral clefts. Eur Radiol. 2006;16:1015–21. doi: 10.1007/s00330-005-0056-6. [DOI] [PubMed] [Google Scholar]
- 24.Wang G, Yang H, Chen K. Osteoporotic vertebral compression fractures with an intravertebral cleft treated by percutaneous balloon kyphoplasty. J Bone Joint Surg Br. 2010;92:1553–7. doi: 10.1302/0301-620X.92B11.24671. [DOI] [PubMed] [Google Scholar]
- 25.Laredo JD. Expert's comment concerning Grand Rounds case entitled “Kümmell's disease: Delayed posttraumatic osteonecrosis of the vertebral body” (by R.Ma, R. Chow, F. H. Shen) Eur Spine J. 2010;19:1071–2. doi: 10.1007/s00586-009-1204-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wagner AL, Baskurt E. Refracture with cement extrusion following percutaneous vertebroplasty of a large interbody cleft. AJNR Am J Neuroradiol. 2006;27:230–1. [PMC free article] [PubMed] [Google Scholar]
- 27.Wang HS, Kim HS, Ju CI, Kim SW. Delayed bone cement displacement following balloon kyphoplasty. J Korean Neurosurg Soc. 2008;43:212–4. doi: 10.3340/jkns.2008.43.4.212. [DOI] [PMC free article] [PubMed] [Google Scholar]