Abstract
Background:
Hip resurfacing arthroplasty (HRA) is primarily indicated for young, active patients with disabling coxarthrosis who wish to remain active and return to sports after surgery. Relatively few prospective studies have assessed return to sporting activity and impact of gender and age on this.
Materials and Methods:
Seventy-nine consecutive patients treated with HRA were included. Patients were reviewed clinically and radiologically. Function was assessed using the modified University of California Los Angeles (UCLA) activity score. The Oxford, Harris and WOMAC hip scores were calculated.
Results:
Average age at the time of surgery was 54.9 years (range 34.5–73.6 years). Average preoperative and postoperative UCLA scores were 4 and 7.6 respectively. Patients were involved in 2 (0–4) sporting activities preoperatively and 2 (0–5) postoperatively. Preoperative and postoperative Oxford Hip Scores, Harris Hip Score and WOMAC scores were 40, 46 and 51 and 16, 94 and 3 respectively (P < 0.0001). Patients returned to sports at an average of 3 months postoperatively.
Conclusion:
Patients were able to return to sports by 3 months and perform the same number of activities at preoperative intensity. Activity levels are maintained up to the medium term with few complications.
Keywords: Activity, gender, hip, resurfacing, sport
Mesh terms: Arthroplasty, replacement, hip, arthritis
INTRODUCTION
The average age of patients being treated with total hip arthroplasty (THA) is decreasing.1 This younger, more active group often wish to return to sporting activity after their procedure.2 Survival of conventional THA has been least encouraging in this patient population.3 Modern metal on metal hip resurfacing arthroplasty (MoM HRA) was introduced specifically to address this active, demanding group of patients.4 Proposed advantages of HRA in this patient population include improved stability and a reduced risk of dislocation as a result of using a large diameter bearing, improved proprioception and preservation of bone stock, particularly on the femoral side.4
In the United Kingdom, the average age of patients undergoing MoM HRA is 11 years less than those receiving uncemented THA and 19 years less than those treated with cemented THA.5 This young, active group expect to return to sporting pursuits post-surgery.6
Complications associated with hip resurfacing prostheses have also been reported in the medical literature as well as the media.6,7 These have ranged from pain to large soft tissue destructive lesions (pseudotumors). Several of these complications have been thought to be design specific.8 This has led to the withdrawal of at least one product from the market.9 The Birmingham hip resurfacing (BHR) Arthroplasty was designed and is most commonly used in the United Kingdom. Good clinical outcomes have been reported with this prosthesis in the short and medium term10 but return to sporting activity has not been specifically addressed. Although it is thought that HRA will allow resumption of an active lifestyle, up to 61% of asymptomatic patients avoid activities such as jogging postoperatively due to anxiety about their prosthesis suggesting more evidence is needed in this area to guide patients.11
This study examines the return to sporting activity after hip resurfacing using the BHR prosthesis in the medium term, timing of the return to sporting activity and the impact of age and gender on return to sport.
MATERIALS AND METHODS
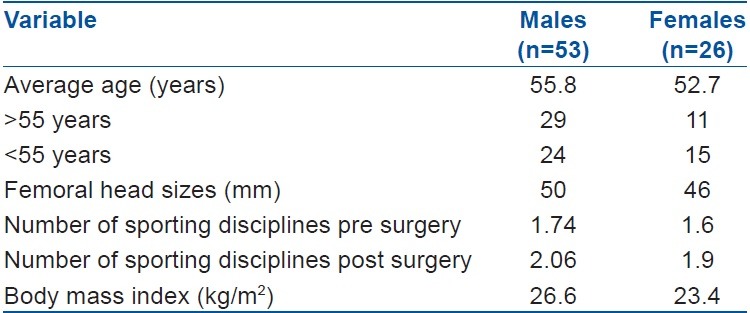
79 consecutive patients treated with the BHR prosthesis between August 2000 and October 2003 years in our unit were enrolled in this prospective study. Patients were selected for this procedure based on their age (<60 years for males and <55 years for females), level of activity, their desire to maintain an active lifestyle after the procedure and also whether they specifically requested this procedure. Patient demographics are shown in Table 1. Patients who had metal allergies, those who had osteoporosis or large cystic lesions within the femoral head on radiographic imaging and females of childbearing age were excluded from the study.
Table 1.
Demographics of the patients
Informed consent was obtained from each patient. All procedures were performed by a single surgeon using the BHR prosthesis (Smith and Nephew, UK). Bilateral simultaneous replacement was done in 1 patient. The second surgery of the bilateral procedures was performed after an intervening period of 3 months.
All procedures were performed with the patient in the lateral decubitus position via a posterior approach. At the end of each procedure the short external rotators were reattached to their previous insertion sites via drill holes placed in the greater trochanter in order to restore the patient's normal anatomy as much as possible and minimize any loss of function as a result of the surgical approach.
All patients were mobilized on the 1st day post surgery and allowed to full weight bearing based on their level of comfort. Activities that required hip flexion beyond 90°, for example sitting in low chairs, tying shoe laces, and low toilet seats, as well as sporting activities, were prohibited for the initial 6 weeks postoperative period. During this period activities resulting in adduction and internal rotation of the hips such as crossing of legs, were also prohibited.
Supervised physiotherapy was started on the 1st post operative day. Initial emphasis was placed on strengthening the hip flexors and gluteal muscles. Supervised mobilization was performed during which patients were encouraged to climb and descend stairs as well as walk on level surfaces, sit and rise from a seated position and get into and out of the car. These sessions continued twice daily until discharge.
Patients were seen in followup at 6 weeks, 12 weeks, 6 months and then yearly. At each visit they were examined to assess their range of movement and level of comfort, questioned about pain and specific enquiry was made into their levels of daily function as well as sporting activity. Objective, quantitative scoring was performed using the University of California Los Angeles (UCLA) activity scores, as well as the Oxford Hip Score (OHS). Satisfaction levels were assessed using a visual analog score with 1 and 10 representing the least and most satisfied patients respectively.
Return to sporting activity
Low impact activities such as exercise, walking on soft surfaces and non competitive swimming were allowed from 6th week post surgery while higher impact activities such as using the cross trainer and chipping and putting (for those who played golf) were allowed between 6 and 12 weeks. Patients were allowed to resume normal activities within their level of tolerance after 3 months. At each stage, they were advised to progress gradually and refrain from activities that caused pain in their operated hip. Examples of gradual progression included playing doubles tennis before returning to the singles game and becoming comfortable playing 9 holes prior to returning to a full round of golf.
At each review, a routine assessment was performed. This included taking a detailed history focusing on the level of mobility and function attainable as well as the level of pain at rest and during activity. Enquires were also made about relief of preoperative pain and their ability to return to activities they performed prior to the onset of their symptoms. Clinical examination included assessment of gait, observation for wasting of gluteal and thigh muscle bulk and review of the surgical scar.
Statistical analysis
All data was recorded and tabulated on a spreadsheet using Microsoft Excel software (Redmond, WA, USA). Statistical analysis was performed using the Student's t-test.
Radiological analysis
Anteroposterior (AP) and lateral radiographs were obtained at each visit to assess implant position and the structure of the surrounding bone as well as for changes in the position of the acetabular and femoral components which might suggest loosening. While not specifically relating to activity levels this formed part of our routine assessment protocol. The pelvic images were obtained with the beam centered on the pubic symphysis at a distance of 100 cm from the patient. This pre-calculated distance resulted in a magnification of 20% that facilitated preoperative planning with the systems used in our unit. The femoral component was examined specifically for changes in position of the ball or the stem using the zones described by Amstutz et al.2 Signs of loosening of the acetabular components were graded as according to the zones described by DeLee and Charnley.5
RESULTS
Eighty procedures were performed in 79 patients between 2000 and 2003. Twenty six females and 53 males were included. One male patient had bilateral procedures performed 3 months apart. Average duration of followup was 8.5 years (range 8–10 years). The average age of our cohort was 54.9 years (range 34.5–73.6 years). The mean age of the male and female groups was 55.8 years (range 35.1–73.6 years) and 52.7 years (range 34.5–64.9 years) respectively. The patient who had bilateral procedures was 55 years old. The average body mass index (BMI) was 25.2 (range 19.8–31.9). All patients involved in this study had advanced symptomatic osteoarthritis affecting their hips. Primary osteoarthritis was the indication for surgery in 74 cases (93.7%). Six patients had osteoarthritis secondary to avascular necrosis with associated collapse of the femoral head [Table 1]. No patients were lost to followup. Mean femoral component size in the male and female populations was 50 mm (range 46–54 mm) and 46 mm (range 38–46 mm) respectively.
Sporting activity
Each patient or cohort performed an average of 1.7 sports (range 1–4 sports). Forty-three patients (44 hips) (55%) played >1 sport. A similar number walked >4 miles a day. The most popular sport was swimming (n = 17) followed by tennis (n = 11) while only one patient played squash [Table 2]. Four swimmers and six cyclists were club athletes while one swimmer competed nationally on the master's circuit. The remainder of this population played sport recreationally. None of these patients participated in extreme sports.
Table 2.
Sporting activities performed by our cohort
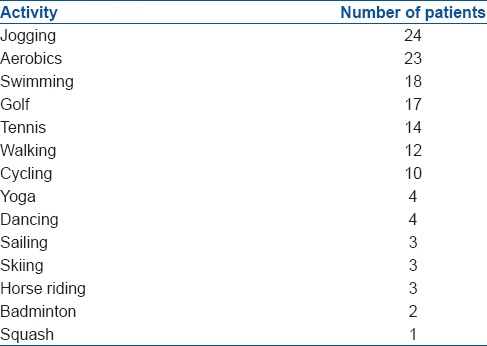
Patients mobilized from day 1 and were discharged at an average of 5 days post surgery (range 4–9 days). By 6 weeks, patients had returned to walking and low impact activities. By 3 months, 85% had returned to jogging and doubles tennis as well as swimming. At the 6 months post surgery review all patients reported being back to their usual sporting activities [Figure 1]. At this stage each patient participated in an average of two sporting activities (range 1–5 activities). Two patients discontinued all sports after surgery. This was due to new onset lower back pain which had been diagnosed as being of a spinal origin (by separate doctors) and was unrelated to their hip arthroplasty procedures. They were, however, prevented from participating in sporting activity due to this pain.
Figure 1.
Sporting activities performed before and after surgery based on their popularity
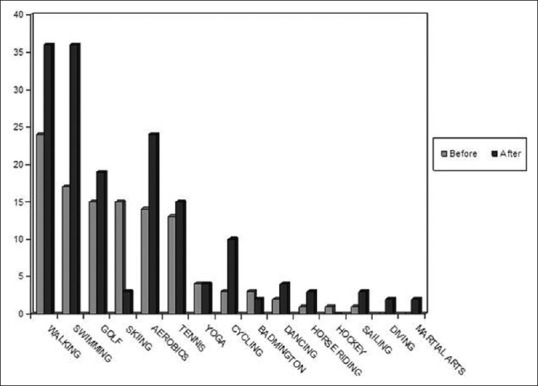
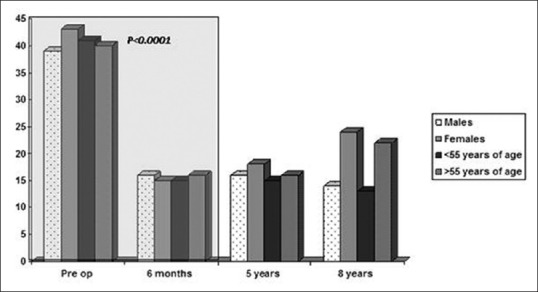
With the exception of skiing, all activities were performed >3 times/week with each session lasting 60–90 min. Twenty nine patients (19 males, 10 females) took up a total of 36 new sports in addition to their preoperative activities. These new sports included skiing, walking and riding and in each case placed them into a higher UCLA category. The average preoperative UCLA score was 4 (range 1–9) compared to 7.6 (range 2–10) postoperatively (P < 0.0001) [Figure 2].
Figure 2.
Changes in University of California Los Angeles activity scores in our patient subgroups over the duration of this study. Statistically significant changes were noted at the 6 months post operatively
We also grouped patients based on their age and gender. This enabled comparison with the designer surgeons’ results in patients under 55 years of age. It also addressed the issue of sporting activity based on gender in an attempt to specifically quantify any improvement experienced by our female cohort. While much has been published on the failure rates of HRA in females, there is, to our knowledge, no prospective data on the amount of benefit they receive relative to male patients.
Sporting activity based on gender
Males
Fifty-two male patients were included in this study. Their average age was 55.8 years (range 35.1-73.6 years). Average BMI of this group was 26.6 (range 21.1–31.9). Prior to their surgery, each patient participated in an average of 1.7 sporting activities (range 0–4). The mean preoperative OHS and UCLA scores were 38.7 (range 24–57) and 4.4 (range 2–9) respectively.
Post surgery members of this cohort participated in a mean of 2 sports (range 0–5) and took up at least 1 new activity (range 1–4). Their mean post surgery OHS and UCLA scores were 14 (range 12–24) and 7.7 (range 6–10) (P < 0.0001 for both scores respectively).
Females
Twenty-seven females were included in this cohort with an average of 52.7 years (range 34.5–64.9 years). The mean BMI of this group was 23.4 (range 19.8–27.4). Each member of this group participated in an average of 1.6 sporting activities prior to their procedure (range 0–4) and their mean preoperative UCLA score was 3.4 (range 1–8). Their average preoperative OHS score was 43.2 (range 26–57). Postoperatively the mean OHS was 24.2 (range 12–32) (P = 0.0007) and the average UCLA score was 7.4 (range 2–10) (P < 0.0001). Each member of this group played 1.98 sports on average and took up a mean of 1.3 new sports after their procedure.
Sporting activity based on age
Age <55 years
Thirty six patients (9 males, 27 females) were <55 years of age at the time of their surgery. The average age of this cohort was 48.7 years (range 34.5–54.9 years). Sixteen members of this cohort (44%) were <40 years of age. Average BMI of this group was 25.1 (range 19.8–30.1). Each member participated in a mean of 1.7 sporting activities preoperatively (range 0–4) which increased to 2 sports postoperatively (P = 0.0657). This was not statistically significant. Pre operative and postoperative OHS and UCLA scores in this cohort were 41 (range 26–53) and 3.9 (range 2–8) and 13.3 (range 12–19) and 7.7 (range 6–10) (P < 0.0001) respectively. Overall patients in this group took up an additional 1.6 new activities along with previous sports.
Age >55 years
Forty three patients (32 males, 11 females) were included in this group. The average age of this cohort was 60.5 years (range 55.1–73.6 years). Their mean BMI was 25.6 (range 20.1–31.9). Members of this group participated in an average of 1.8 sports prior to their surgery and a mean of 2 sports postoperatively (P = 0.6255). Pre and postoperative UCLA score were 4.3 (range 1–6) and 7.4 (range 2–10) respectively (P < 0.0001). Similarly, the pre and postoperative OHS scores were 39.6 (range 24–57) and 21.9 (range 12–32) respectively (P < 0.0001). Two patients discontinued sporting activities post surgery. Although their mobility improved significantly, they had progressive back pain due to preexisting medical issues which precluded them from sporting activity.
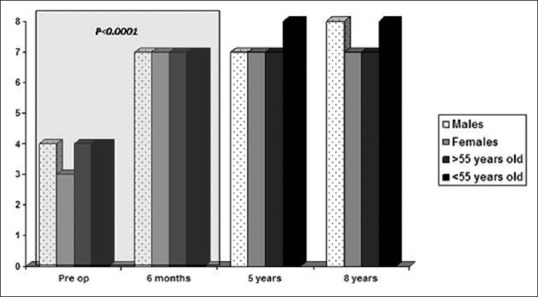
Clinical scores
Oxford Hip Scores were calculated for each patient both pre and postoperatively. The average preoperative OHS was 40.4 (range 24–57) and the average postoperative score was 15.6 (range 12–40) (P < 0.0001). There were significant improvements in the pain component of the OHS as well as in activities in daily living [Figure 3].
Figure 3.
Changes in Oxford Hip Scores over the course of this study. Statistically significant changes were noted at the 6 months post operatively
Radiological review
Each patient had a standardized AP pelvic radiograph at each followup visit. These were reviewed by two separate assessors to ascertain any signs of loosening of the acetabular or femoral component. The femoral components were examined specifically for signs of varus/valgus alignment within the neck as well as for radiolucent lines around the femoral stem. On the acetabular side, there was no evidence of component loosening. Average abduction angle was 47° (range 30–50°). On the femoral side, no cases of varus malpositioning were noted. There were radiolucent lines around the femoral components in 6 patients and signs of neck thinning in 3 patients. These patients were all asymptomatic clinically.
Complications
One male patient suffered a fracture of his right femoral neck 7 years after his index procedure on the side that was resurfaced. This occurred secondary to a fall from his pushbike. The fracture included the region of bone in which the femoral component was fixed hence this was revised to a stemmed prosthesis. The acetabular component was retained. There were no deep infections or cases of impending revisions at the time of last follow up.
DISCUSSION
There has been an overall increase in patient expectations. Patients now expect to resume sporting and an active lifestyle.2 Such high levels of activity has been associated with increased wear and unacceptable failure rates of traditional THA in the active population.3 Modern MoM HRA was introduced to address this group and large marketing campaigns involving manufactures, physicians and high level athletes have claimed improved return to sporting activity after hip resurfacing).12
It has been shown that up to 98% of patients who engage in sports preoperatively are able to return to sports after HRA13 and up to 91.6% return to high-impact activities such as jogging.14 Several factors have been proposed to favor this return to high levels of function. These include improved stability, low wearing bearing surfaces and improved proprioception15 although it has been suggested that return to sporting activity post lower limb arthroplasty surgery is mainly determined by presurgical activity levels, BMI and age.16
Patients treated with HRA have been shown to have faster-walking speeds17,18 and higher UCLA activity scores when compared to those with conventional THA.19 The association between these findings and return to sporting activity in the medium term has not been discussed.
Abe et al.11 found that only 12.8% of patients returned to jogging at a mean of 4.8 years after HRA in the absence of pain or other post surgical complication, suggesting that activity levels decrease up to this period.
The average age for patients having Hip resurfacing Arthroplasty (HRA) in the United Kingdom is 54.7 years of age compared to 65.5 years for those having uncemented THA and 73 years for those having cemented THA.20 The ideal patient for HRA was considered to be a young, active male who engages in vigorous activity.4 As a result, it is performed twice as much in males compared to females.21 Female patients treated with resurfacing are often younger than males, reflecting a cautious approach to patients with potentially osteopenic bone and suboptimal proximal bone stock. These factors are reflected in our patient cohort.
Most complications of HR reported in the literature have occurred within the first 5 years. Hence, we chose to review patients after this period as revision surgery is likely to affect activity level. Patients in this consecutive series performed on average 1.7 sports before their surgical procedures [Table 1]. Ten patients (7.9%) were club level competitors. By 3 months post surgery 85% had returned to their preoperative activity levels and by 6 months all patients were performing sports at their pre-symptom levels. At this stage each patient participated in a mean of 2 sporting disciplines. This is in contrast to Banerjee et al.3 who found a small reduction in sports participation post surgery as well as Naal et al.19 who reported that only 50% of their had returned to sporting activity at the 3 months stage with an overall decrease in the number of sporting discipline performed by each patient.
Thirty-seven percent of our cohort participated in a larger number of sporting activities post surgery compared to before their procedure. This potentially reflects previously reported observations that patients receiving HRA are not only more active preoperatively, but expect to participate in sports after surgery.22 It also possibly reflects a subjective perception of a stable joint with preserved proprioception25 that facilitates a faster return to sporting activity.
Not all authors agree that HRA allows patients to return to sport more effectively than conventional THA.23,24 Lavigne et al.24 found no difference in return to sport when they prospectively compared THA and HRA. Their study was not restricted to the BHR prosthesis however.
There was no difference in the level of functional improvement experienced by patients under or over 55 years or when separated by gender. All age groups and both genders showed improved Oxford and UCLA activity scores while maintaining their expected levels of sporting activity. This contrasts with previous findings that older patients seem to return to sport at a higher intensity and for a longer duration than patients <60 years old.25
A higher failure and revision rate of HR in female patients has been reported.20 The demographics of our female cohort are similar to the United Kingdom NJR. Female patients in this study exhibited similar improvements in UCLA and OHS scores when compared to male patients. They returned to a similar level of sporting activity and participated in a similar number of new sporting disciplines as males after their procedure and differs from previous reports suggesting that male sex correlates with return to sporting activity postoperatively.11 These results suggest that females experience similar functional improvements and clinical benefits to those exhibited by male patients and while they need to be carefully selected, they could possibly experience a similar degree of improvement in their activity levels as male patients after having this procedure.
Significant improvements were noted in the OHS at final followup. Resolution of pain and overall improvement in daily physical function, as well as activities of daily living, were experienced by all patient categories. Survival at the time of final followup was 99.8% with failure considered as a revision for any reason. The acetabular component was retained. He subsequently returned to riding his bike. There were no cases of unexplained femoral neck fractures, and no patients had symptoms of the adverse reaction to metal debris (ARMD) up to the last followup.
The limitations of our study are that this cohort is relatively small, but it does represent a prospective consecutive non designer surgeon series and reflects activity levels in a population of patients in the United Kingdom. To the best of our knowledge, it is also a report of the return to sporting function with the longest followup using this prosthesis. Surgeons have generally lost confidence in using MoM HR due to concerns about ARMD. The results of this series show that results can be encouraging in the young, active group of patients, and they can achieve a high level of function and satisfaction with this procedure. This in keeping with other published opinion.21,22,25
CONCLUSION
These results suggest that preoperative sporting activity can be restored in the medium term with the BHR prosthesis, likewise pain relief and activities of daily living can be maintained.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Amstutz HC, Beaulé PE, Dorey FJ, Le Duff MJ, Campbell PA, Gruen TA. Metal-on-metal hybrid surface arthroplasty: Two to six-year followup study. J Bone Joint Surg Am. 2004;86-A:28–39. [PubMed] [Google Scholar]
- 2.Amstutz HC, Le Duff MJ, Campbell PA, Wisk LE, Takamura KM. Complications after metal-on-metal hip resurfacing arthroplasty. Orthop Clin North Am. 2011;42:207–30, viii. doi: 10.1016/j.ocl.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 3.Banerjee M, Bouillon B, Banerjee C, Bäthis H, Lefering R, Nardini M, et al. Sports activity after total hip resurfacing. Am J Sports Med. 2010;38:1229–36. doi: 10.1177/0363546509357609. [DOI] [PubMed] [Google Scholar]
- 4.Daniel J, Pynsent PB, McMinn DJ. Metal-on-metal resurfacing of the hip in patients under the age of 55 years with osteoarthritis. J Bone Joint Surg Br. 2004;86:177–84. doi: 10.1302/0301-620x.86b2.14600. [DOI] [PubMed] [Google Scholar]
- 5.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976:20–32. [PubMed] [Google Scholar]
- 6.Gore DR, Murray MP, Gardner GM, Sepic SB. Hip function after total vs. surface replacement. Acta Orthop Scand. 1985;56:386–90. doi: 10.3109/17453678508994353. [DOI] [PubMed] [Google Scholar]
- 7.Haddad FS, Benjamin-Laing H. Commentary - Key advantages and indications for metal-on-metal hip resurfacing should not be dismissed. Orthopaedics Today Europe. 2012;15:4. [Google Scholar]
- 8.Herberts P, Karrholm J, Garellik G. The Swedish National Hip Arthroplasty Register, Annual Report. 2010. [Last accessed 2014 Jun 10]. Available from: http://www.shpr.se/en/Publications/DocumentsReports.aspx .
- 9.Langton DJ, Joyce TJ, Jameson SS, Lord J, Van Orsouw M, Holland JP, et al. Adverse reaction to metal debris following hip resurfacing: The influence of component type, orientation and volumetric wear. J Bone Joint Surg Br. 2011;93:164–71. doi: 10.1302/0301-620X.93B2.25099. [DOI] [PubMed] [Google Scholar]
- 10.Kobayashi S, Eftekhar NS, Terayama K, Joshi RP. Comparative study of total hip arthroplasty between younger and older patients. Clin Orthop Relat Res. 1997;140:51. doi: 10.1097/00003086-199706000-00019. [DOI] [PubMed] [Google Scholar]
- 11.Abe H, Sakai T, Nishii T, Takao M, Nakamura N, Sugano N. Jogging after total hip arthroplasty. Am J Sports Med. 2014;42:131–7. doi: 10.1177/0363546513506866. [DOI] [PubMed] [Google Scholar]
- 12. [Last accessed 2014 Jun 10]. Available from: http://www.surfacehippy.info/athletes.php .
- 13.Girard J, Miletic B, Deny A, Migaud H, Fouilleron N. Can patients return to high-impact physical activities after hip resurfacing?. A prospective study. Int Orthop. 2013;37:1019–24. doi: 10.1007/s00264-013-1834-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fouilleron N, Wavreille G, Endjah N, Girard J. Running activity after hip resurfacing arthroplasty: A prospective study. Am J Sports Med. 2012;40:889–94. doi: 10.1177/0363546511434564. [DOI] [PubMed] [Google Scholar]
- 15.Szymanski C, Thouvarecq R, Dujardin F, Migaud H, Maynou C, Girard J. Functional performance after hip resurfacing or total hip replacement: A comparative assessment with non-operated subjects. Orthop Traumatol Surg Res. 2012;98:1–7. doi: 10.1016/j.otsr.2011.10.006. [DOI] [PubMed] [Google Scholar]
- 16.Jassim SS, Douglas SL, Haddad FS. Athletic activity after lower limb arthroplasty: A systematic review of current evidence. Bone Joint J. 2014;96-B:923–7. doi: 10.1302/0301-620X.96B7.31585. [DOI] [PubMed] [Google Scholar]
- 17.McBryde CW, Theivendran K, Thomas AM, Treacy RB, Pynsent PB. The influence of head size and sex on the outcome of Birmingham hip resurfacing. J Bone Joint Surg Am. 2010;92:105–12. doi: 10.2106/JBJS.I.00197. [DOI] [PubMed] [Google Scholar]
- 18.Mont MA, Seyler TM, Ragland PS, Starr R, Erhart J, Bhave A. Gait analysis of patients with resurfacing hip arthroplasty compared with hip osteoarthritis and standard total hip arthroplasty. J Arthroplasty. 2007;22:100–8. doi: 10.1016/j.arth.2006.03.010. [DOI] [PubMed] [Google Scholar]
- 19.Naal FD, Maffiuletti NA, Munzinger U, Hersche O. Sports after hip resurfacing arthroplasty. Am J Sports Med. 2007;35:705–11. doi: 10.1177/0363546506296606. [DOI] [PubMed] [Google Scholar]
- 20. [Last accessed 2014 Jun 10]. Available from http://www.new.njrcentre.org.uk/NjrCentre/Portals/0/Documents/NJR%208th%20Annual%20Report%202011.pdf .
- 21.Narvani AA, Tsiridis E, Nwaboku HC, Bajekal RA. Sporting activity following Birmingham hip resurfacing. Int J Sports Med. 2006;27:505–7. doi: 10.1055/s-2006-924199. [DOI] [PubMed] [Google Scholar]
- 22.Wylde V, Blom A, Dieppe P, Hewlett S, Learmonth I. Return to sport after joint replacement. J Bone Joint Surg Br. 2008;90:920–3. doi: 10.1302/0301-620X.90B7.20614. [DOI] [PubMed] [Google Scholar]
- 23.Pollard TC, Baker RP, Eastaugh-Waring SJ, Bannister GC. Treatment of the young active patient with osteoarthritis of the hip. A five- to seven-year comparison of hybrid total hip arthroplasty and metal-on-metal resurfacing. J Bone Joint Surg Br. 2006;88:592–600. doi: 10.1302/0301-620X.88B5.17354. [DOI] [PubMed] [Google Scholar]
- 24.Lavigne M, Therrien M, Nantel J, Roy A, Prince F, Vendittoli PA. The John Charnley Award: The functional outcome of hip resurfacing and large-head THA is the same: A randomized, double-blind study. Clin Orthop Relat Res. 2010;468:326–36. doi: 10.1007/s11999-009-0938-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Treacy RB, McBryde CW, Shears E, Pynsent PB. Birmingham hip resurfacing: A minimum followup of ten years. J Bone Joint Surg Br. 2011;93:27–33. doi: 10.1302/0301-620X.93B1.24134. [DOI] [PubMed] [Google Scholar]


