Abstract
Background
Medication non-adherence increases the risk of hospitalization and poor outcomes, particularly among patients with cardiovascular disease (CVD).
Purpose
To examine characteristics associated with medication non-adherence among adults hospitalized for CVD.
Methods
Patients in the Vanderbilt Inpatient Cohort Study who were admitted for acute coronary syndromes or heart failure completed validated assessments of self-reported medication adherence (the Adherence to Refills and Medications Scale [ARMS]), demographic characteristics, health literacy, numeracy, social support, depressive symptoms, and health competence. We modeled the independent predictors of non-adherence before hospitalization, standardizing estimated effects by each predictor’s interquartile range (IQR).
Results
Among 1967 patients studied, 70.7% indicated at least some degree of medication non-adherence leading up to their hospitalization. Adherence was significantly lower among patients with lower health literacy (0.18 point change in adherence score per IQR change in health literacy), lower numeracy (0.28), lower health competence (0.30), and more depressive symptoms (0.52), and those of younger age, non-White race, male gender, or less social support.
Conclusions
Medication non-adherence in the period before hospitalization is more prevalent among patients with lower health literacy, numeracy, or other intervenable psychosocial factors. Addressing these factors in a coordinated care model may reduce hospitalization rates.
Keywords: medication adherence, cardiovascular patients
INTRODUCTION
Medication adherence is the degree to which patients take their medications as prescribed (Osterberg, 2005). For patients with cardiovascular disease, adherence to medications is necessary to achieve control of hypertension, hyperlipidemia, and diabetes and reduce the risk of adverse outcomes such as stroke, heart failure, renal failure, and myocardial infarction. Non-adherence to medication regimens is a significant contributor to Emergency Department (ED) visits and hospitalization rates, as well as higher health care costs and mortality (Bitton, Choudhry, Matlin, Swanton, & Shrank, 2013; Davis, Jandrisevits, Iles, Weber, & Gallo, 2012; Fitzgerald et al., 2011; Ho et al., 2006; Jackevicius, Li, & Tu, 2008; Roebuck, Liberman, Gemmill-Toyama, & Brennan, 2011). A better understanding of the factors associated with non-adherence at the time patients are hospitalized may provide intervention targets for care coordination and population health management programs which seek to reduce excess health care utilization.
Prior research has shown that medication non-adherence is related to sociodemographic characteristics, but the associations are weak and vary among studies (Osterberg, 2005; Steiner et al., 2009). In cardiovascular patients, lower medication adherence is associated with non-White races, the extremes of age, less education, and lower income/socioeconomic status (SES); these findings, however, have been inconsistent (Ali et al., 2009; Chan et al., 2010; Cohen et al., 2012; Lewey et al., 2013; Marcum et al., 2013; Melloni et al., 2009). Medication adherence is likely affected by other psychosocial factors, such as health literacy, numeracy, self-efficacy, social support, and depression, but again findings are contradictory, and little research has considered these factors together. This leads to an incomplete understanding of the independent predictors of medication non-adherence and may hamper intervention efforts.
For example, research on health literacy and adherence to cardiovascular medications reveals some studies finding no association, while others found positive and even an inverse relationship (Gazmararian et al., 2006; Loke, Hinz, Wang, & Salter, 2012; Noureldin et al., 2012). Finally, research is ongoing to more fully elucidate the relationship between numeracy—i.e., “the ability to use and understand numbers in daily life” (Rothman et al., 2006)—and medication adherence. We have demonstrated an association between low health numeracy and post-discharge medication errors (Mixon et al., 2014). Low health numeracy affects medication self-management and has been associated with increased odds of unplanned healthcare utilization in patients with heart failure (McNaughton et al., 2013).
Several studies have found associations between self-efficacy and adherence behavior (Burke, 1997; Krall Scherer, 2001; Ni, 1999; Sarkar, 2006). A review of cardiovascular disease prevention strategies concluded that self-efficacy enhancement was among the most successful strategies in improving adherence (Burke, 1997). Other studies revealed that pragmatic social support (e.g., helping patients accomplish daily tasks) led to improved medication adherence as compared to emotional or no social support (DiMatteo, 2004a, 2004b; Kripalani, Henderson, Jacobson, & Vaccarino, 2008). Additionally, depressed patients are generally less adherent to medications than non-depressed patients (Kronish, 2006; Osterberg, 2005). Davis et al. (2012) found that psychological factors, such as health attitudes and beliefs, anxiety and depression, social support and locus of control, all predicted medication adherence in ED patients with hypertension, diabetes or seizure disorders to a greater extent than demographic or socioeconomic factors.
Because medication non-adherence is a risk factor for preventable hospitalization, we sought to develop a more complete understanding of factors associated with non-adherence leading up to hospitalization for acute cardiovascular events. We hypothesized that medication non-adherence would be independently associated with lower health literacy and numeracy, lower education and income, less social support, more depressive symptoms, and lower perceived health competence.
METHODS
Study setting and design
The Vanderbilt Inpatient Cohort Study (VICS) is a prospective cohort study of patients admitted to Vanderbilt University Hospital in Nashville, Tennessee or Williamson Medical Center in Franklin, Tennessee with acute coronary syndromes (ACS) or acute decompensated heart failure (ADHF). The purpose of the study is to examine the relationships between social determinants of health and outcomes after hospital discharge. The rationale and design of VICS, including the conceptual framework which guided the overall study and selection of measures, are detailed elsewhere (Meyers et al., 2014). Participants completed a baseline interview and 3 follow-up calls in the 3 months following hospital discharge. All data are collected and managed using Vanderbilt University’s Research Electronic Data Capture (REDCap) tool (Harris, 2009). The study was approved by the Vanderbilt University Institutional Review Board.
Participants
In these analyses, we included VICS participants enrolled from October 2011 to September 2014. To be eligible for VICS, patients must be at least 18 years old and meet study criteria for ACS or ADHF as determined by a physician’s review of the electronic medical record. The main exclusion criteria are being too ill to complete the in-hospital interview, cognitive impairment, lack of reliable contact information for follow-up, inability to communicate in English, unstable psychiatric illness, or being in hospice care. Patients who denied taking any medications prior to admission were excluded from the present analyses, as we could not assess their pre-hospital medication adherence.
Measures
All variables analyzed herein were obtained in the baseline interview which was administered by trained research assistants (RAs) at the patient’s bedside, generally within 24 hours of hospitalization. The structured interview included sociodemographic information such as age, gender, educational attainment (in years), marital status, household income, financial strain, and self-reported race. Household income was reported using a modification of the strata from the Behavioral Risk Factor Surveillance System (BRFSS) questionnaire ((CDC), 2010). Financial strain was assessed by a single, 4-point question asking “How difficult is it for you (and your family) to pay your monthly bills” (“Not at all difficult” to “Very difficult”). Race was dichotomized into White vs. all other races, and marital status was dichotomized to living with a partner/spouse vs. not married/partnered.
The primary outcome, medication adherence prior to hospitalization, was measured using a shortened, 7-item version of the Adherence to Refills and Medications Scale (ARMS), which correlates very highly (0.95) with the full 12-item measure (Kripalani, Risser, Gatti, & Jacobson, 2009). The ARMS is a reliable and validated instrument that was developed among patients with cardiovascular disease. Each of the items allows patients to express on a 4-point scale how often they do not take or refill their medications under different circumstances. Scores on the ARMS-7 range from 7 to 28, with higher values indicating better adherence. Scores less than 28 indicate some degree of non-adherence (Kripalani, 2008). In prior research, the ARMS correlated more strongly with medication refills than did the widely used 4-item scale by Morisky and colleagues (Spearman’s rho = 0.32 vs. 0.22, p<0.01)(Kripalani et al., 2009; Morisky, Green, & Levine, 1986). The ARMS has also demonstrated predictive validity with blood pressure control and glycemic control (Kripalani et al., 2009; Mayberry, Gonzalez, Wallston, Kripalani, & Osborn, 2013; McNaughton, Jacobson, & Kripalani, 2014). Cronbach’s alpha for the ARMS-7 in this sample was 0.82.
Health literacy was assessed with the Brief Health Literacy Screen (BHLS) (Chew, 2004; Wallston et al., 2014). The 3-item measure asks patients to report their level of confidence filling out medical forms, need for assistance in reading hospital materials, and their understanding of written medical information, each on a 5-point response scale. Scores for this measure can range from 3 to 15, with higher scores representing higher subjective health literacy.
Numeracy was assessed by a shortened 3-item version of the Subjective Numeracy Scale (SNS) that aims to quantify the participants’ perceived quantitative abilities and comfort with numbers (Fagerlin et al., 2007; Zikmund-Fisher, Smith, Ubel, & Fagerlin, 2007). Specifically, the items ask patients to rate their own math skills and preferences for numerical information on a 6-point response scale. The SNS-3 score is reported as the mean of the 3 items and ranges from 1 to 6, with higher scores reflecting higher subjective numeracy. The SNS-3 is at least as valid as the full 8-item version (McNaughton, Cavanaugh, Kripalani, Rothman, & Wallston, 2015). In this sample, Cronbach’s alpha for the SNS-3 was 0.80.
Health competence (also referred to in the literature as generalized health self-efficacy (Wallston, 2001)) was assessed with 2 of the 8 items of the Perceived Health Competence Scale (PHCS) (Smith, Wallston, & Smith, 1995). The items were “It is difficult for me to find effective solutions for health problems that come my way” and “I am able to do things for my health as well as most other people.” Both PHCS items use a 5-point Likert response scale. After reverse-scoring the first item the total summed score can range from 2 to 10. Higher PHCS-2 scores reflect an increased belief in one’s capability to do whatever is necessary to optimize health outcomes.
Social support was assessed using the ENRICHD Social Support Inventory (ESSI) (Berkman, 2003). Participants were asked 6 questions regarding emotional and instrumental support, each of which had a 5-point response scale (range 6–30), where higher scores indicate increased social support.
Depression during the 2 weeks prior to hospitalization was assessed using the 8-item version of the Patient Health Questionnaire (PHQ-8) (Kroenke, 2009). The sum of the questions ranges from 0 to 24, where higher scores indicate more depressive symptoms.
Statistical Analyses
To describe our patient sample, we summarized categorical variables with percentages and continuous variables with percentiles (i.e., 5th, 25th, 50th, 75th, 95th). For the primary outcome of pre-hospital medication non-adherence, ARMS-7 scores were treated as a continuous variable. In unadjusted analyses, we examined factors associated with non-adherence using the Kruskal-Wallis and Wilcoxon tests for the categorical variables and the Spearman correlation coefficient test for the ordered categorical and continuous variables.
We then used multivariable linear regression to characterize the independent predictors of non-adherence, including all pre-specified variables in the model and allowing for non-linear effects. When fitting the model, the functional form for the continuous variable effects was initially allowed to be very flexible as we used restricted cubic splines with four knots (Harrell, 2001). However, if the likelihood ratio tests for the non-linear terms showed little to no evidence of improved model fit over standard linear effects (p > 0.20 for the 2 degree of freedom non-linear effect test), then for ease of interpretation, we reported the estimate on the linear scale. By using a large p-value as the criterion for significance of the non-linear terms, we erred on the side of including richer functional forms for covariate effects and avoided excluding non-linear effects whose p-values were only slightly above the standard 0.05 significance level. Continuous variables modeled with linear functional forms were scaled by the interquartile range (IQR) to facilitate effect size comparisons. Associated regression parameter estimates may therefore be interpreted as the expected change in the ARMS-7 score per IQR change in the independent variable. To avoid casewise deletion of records with missing covariates we employed multiple imputation with 5 imputation samples using predictive mean matching. Based on the available sample size, regression models were able to accommodate 98 degrees of freedom, using a 20:1 rule. All analyses were conducted using R version 3.1.0.
RESULTS
Among 8,926 patient hospitalizations for ACS and/or ADHF, 2,654 completed screening and were found to be eligible for the study. The most common reasons for exclusion, aside from being unavailable or declining screening, were being too ill to complete an in-hospital interview (e.g., on a mechanical ventilator for several days), cognitive impairment, communication difficulties, or lack of reliable contact information for follow-up interviews (Figure 1). Among screened eligible patients, 2,079 (78.3%) provided informed consent and were enrolled in the study.
Figure 1.
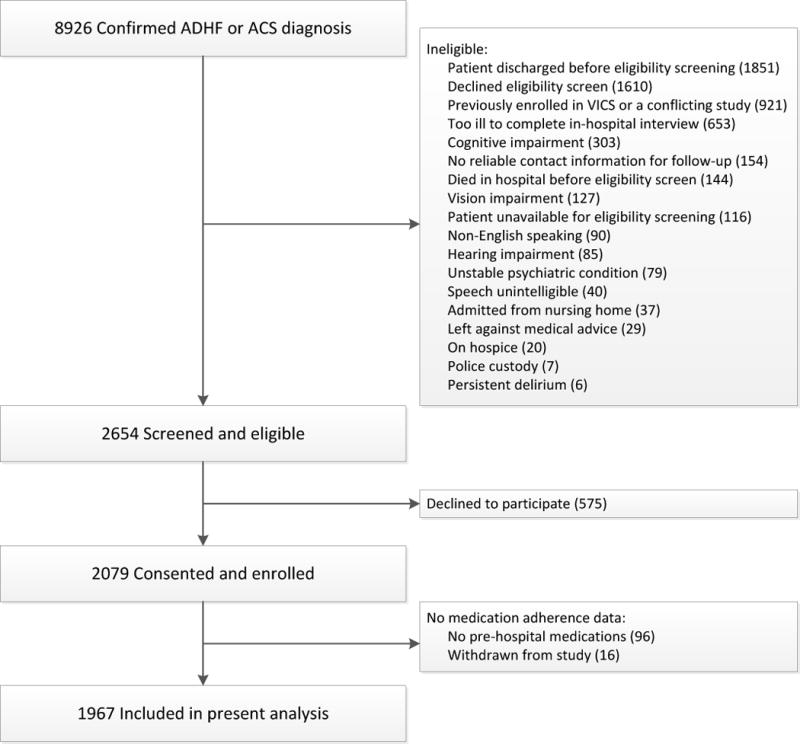
Study flow diagram.
Medication adherence scores were available for 1,967 enrolled patients (94.6%). The median score was 26 (IQR: 24 to 28), and 70.7% of patients admitted some degree of non-adherence prior to hospitalization (i.e., ARMS-7 score < 28).
As shown in Table 1, 61%, 32%, and 7% of patients were hospitalized with ACS, ADHF, or both ACS and ADHF, respectively; 43% were female, 83% percent were White, and 60% lived with their spouse or partner. The median age was 61 years (IQR: 52 to 69), and the median years of educational attainment was 13 years (IQR: 12 to 16). The median annual household income fell into the $35,000 to $49,999 category, and nearly half (46.7%) of patients reported difficulty paying bills. Patients had a median health literacy score of 12 (IQR: 10 to 14) and a median subjective numeracy score of 5 (IQR: 3 to 5). Despite acknowledging both emotional and instrumental support from other persons, most patients also reported occasionally experiencing some depressive symptoms, and had a median health competence score of 8 (IQR: 6 to 10). In unadjusted analyses (Table 1), all patient characteristics tested except for gender and diagnosis were associated with the pre-hospital medication adherence score (p<0.05 for each comparison).
Table 1.
Descriptive statistics and unadjusted associations with medication adherence.
| Summary* | Unadjusted Association with Medication Adherence Score (ARMS-7)** | ||
|---|---|---|---|
| Distribution (N) | Measure | p-value | |
| Medication Adherence (ARMS) | 21: 24: 26: 28: 28 (1967) | – | – |
| Diagnosis† | 0.2412 | ||
| ACS only | 60.9% (1197) | 21: 24: 26: 28: 28 | |
| ADHF only | 32.2% (634) | 21: 24: 26: 28: 28 | |
| ACS and ADHF | 6.9% (136) | 21: 24: 26: 28: 28 | |
| Gender | 0.7461 | ||
| Male | 57.0% (1122) | 21: 24: 26: 28: 28 | |
| Female | 43.0% (845) | 21: 24: 26: 28: 28 | |
| Marital Status | 0.0021 | ||
| Not living with spouse | 40.1% (788) | 20: 24: 26: 28: 28 | |
| Living with spouse | 59.9% (1179) | 21: 25: 27: 28: 28 | |
| Race | <0.0011 | ||
| White | 83.2% (1633) | 21: 25: 27: 28: 28 | |
| Non-white | 16.8% (329) | 19: 23: 25: 27: 28 | |
| Difficulty Paying Bills | <0.0012 | ||
| Very difficult | 17.5% (342) | 20: 23: 25: 27: 28 | |
| Somewhat difficult | 29.2% (570) | 21: 24: 26: 27: 28 | |
| Not very difficult | 19.3% (377) | 21: 24: 26: 28: 28 | |
| Not at all difficult | 34.0% (664) | 22: 26: 27: 28: 28 | |
| Age | 39: 53: 61: 69: 81 (1967) | 0.243 | <0.0013 |
| Education | 9: 12: 13: 16: 18 (1967) | 0.103 | <0.0013 |
| Income†† | 1: 4: 6: 7: 9 (1887) | 0.161 | <0.0013 |
| Social Support | 16: 24: 27: 30: 30 (1965) | 0.213 | <0.0013 |
| Depression | 1: 4: 7: 12: 19 (1957) | −0.265 | <0.0013 |
| Health Competence | 3: 6: 8: 10: 10 (1955) | 0.207 | <0.0013 |
| Brief Health Literacy | 5: 10: 12: 14: 15 (1967) | 0.129 | <0.0013 |
| Subjective Numeracy | 2: 3: 5: 5: 6 (1961) | 0.182 | <0.0013 |
For summary statistics: Continuous variables are displayed as the 5th: 25th: 50th: 75th: 95th percentiles and (N). Categorical variables are summarized with the percentage and (N).
For associations with categorical variables, the distribution of the adherence score is displayed for each category of the independent variable. For continuous variables, the Spearman’s rho correlation with adherence score is displayed.
ACS=acute coronary syndrome; ADHF=acute decompensated heart failure
Income levels: 1=<$10,000; 2=$10,000–14,999; 3=$15,000–19,999; 4=$20,000–24,999; 5=$25,000–$34,999; 6=$35,000–49,999; 7=$50,000–74,999; 8=$75,000–99,999; 9=$100,000+
Wilcoxon test
Kruskal-Wallis test
Spearman correlation
Results from the multivariable linear regression are displayed in Figure 2 with the y-axis depicting the change in the mean medication adherence score associated with changes in independent variables. Non-linear continuous covariate associations with adherence are shown in individual panels. Linear continuous variable associations and categorical variable associations are shown in the bottom panel. For linear relationships between adherence and continuous variables, the magnitude of change in adherence is expressed per IQR change in the independent variable. Collectively, these independent variables explained 20% of the variance in medication adherence scores (p<0.001). We observed that pre-hospital medication adherence was significantly lower among patients with lower health literacy or numeracy. Specifically, the estimated medication adherence score differed by 0.18 (95% CI 0.02 to 0.34) points per 4 point change in health literacy and 0.28 (95% CI 0.10 to 0.46) points per 2 point change in subjective numeracy. Psychosocial risk factors, namely lower levels of social support or perceived health competence, and greater levels of depressive symptoms, were also associated with more non-adherence. Sociodemographic characteristics such as male gender, non-White race, and education, also predicted non-adherence. Two variables that appeared to be related to medication adherence in the unadjusted analyses (income and marital status) did not exhibit associations with adherence scores after adjustment for other variables.
Figure 2.
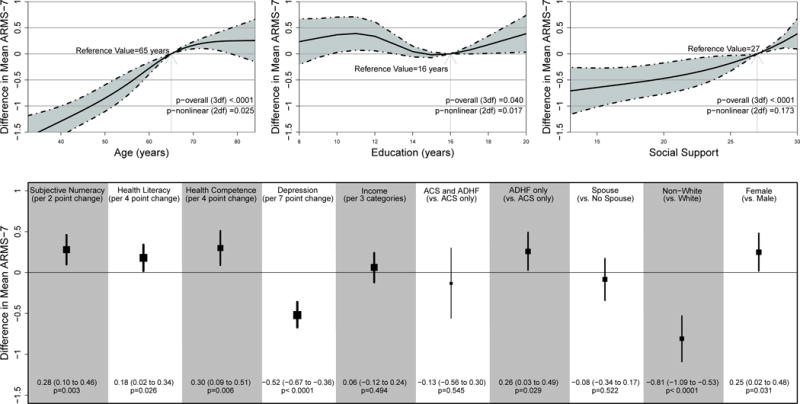
Multivariable analysis of factors associated with pre-hospital medication adherence.
The effect sizes for subjective numeracy, health literacy, health competence, depression, and income are expressed in terms of a change of one interquartile range in the value of the predictor variable. This scaling is done to facilitate effect size comparisons across continuous variables with different scoring ranges.
Three independent variables, age, education, and social support, exhibited at least some evidence of non-linear associations with medication adherence (Figure 2). For example, age less than 65 was associated with more non-adherence, whereas the opposite was seen for ages between 65 and 75; beyond age 75, the effect of age on medication adherence was not statistically significant. Interestingly, the association of education with adherence shows at least some evidence of a U-shape. That is, those with 12 or 20 years of education are expected to have higher levels of adherence than those with 16 years of education.
DISCUSSION
This study examined the factors associated with medication non-adherence leading up to hospitalization for acute cardiovascular conditions. We found that low health literacy and numeracy were significantly associated with non-adherence, as were non-White race, younger age, male gender, lower health competence, less social support, and more depressive symptoms. Several of these individual associations are consistent with prior findings, and it is important to note that these patient attributes remained significant independent predictors in the multivariable model when adjusting for these and other factors.
Prior research has demonstrated that, on average, only 50% of patients take their medications as prescribed (Osterberg, 2005). Medication non-adherence plays an important role in acute exacerbations of chronic conditions such as heart failure and coronary heart disease, resulting in emergency department visits and hospitalizations. In this study, we found several risk factors for non-adherence (i.e., health literacy, numeracy, social support, health competence, and depression) that represent potentially intervenable targets for outpatient disease management. Comprehensive outpatient care coordination that provides attention to these factors with educational, behavioral, and social interventions has the potential to improve chronic disease control and prevent some hospitalizations related to non-adherence.
We hypothesized that lower health literacy and numeracy would be associated with medication non-adherence, and our findings confirmed this. This research adds to a relatively small body of adherence studies that have examined health literacy and numeracy concurrently (Apter et al., 2013; Osborn et al., 2011; Osborn et al., 2013; Waldrop-Valverde, Jones, Gould, Kumar, & Ownby, 2010). Low health literacy may exert an effect on adherence by affecting patients’ ability to read and understand the text component of medication instructions, whereas numeracy could have an effect on patients’ handling of daily dosage, quantity dispensed, and refill dates. Overall, the prior literature on health literacy and adherence has demonstrated inconsistent findings, but this may be due in part to methodological limitations (Loke et al., 2012). Many prior studies were relatively small and categorized variables for ease of interpretation, but at the expense of data loss. Our large study had sufficient sample size for modeling a robust set of continuous predictor variables which were allowed to have linear and non-linear effects. We thus believe our findings to have a high level of rigor for addressing the longstanding question of whether health literacy and numeracy are independently associated with medication adherence.
We observed lower medication adherence among non-White patients, the majority of whom in our sample were Black. This finding is consistent with other research (Dickson, McCarthy, Howe, Schipper, & Katz, 2013; Heidenreich, 2014; Wu et al., 2010; Zhang & Baik, 2014), and it is noteworthy that the difference between the two racial groups was maintained in the multivariate analysis that controlled for health literacy, numeracy and the other covariates. Other research has shown that health literacy or numeracy may mediate racial disparities in medication adherence, but that did not wholly occur here, indicating that more research is needed to clarify this issue (Osborn et al., 2011; Waldrop-Valverde, Osborn, et al., 2010). Low medication adherence on the part of Black patients may partially explain racial discrepancies in health status, and if it is mediated by health literacy or numeracy, this could offer an intervention target.
In our analyses, age had both a significant linear and non-linear relationship to medication adherence. In general, younger cardiovascular patients reported less adherence with their medication regimens than did older patients, which corresponded to findings from other studies; this trend, however, changed once patients reached their mid-70’s. The age at which adherence appears to decline in our sample is approximately 10 years later than in the study by Akerblad et al., but this could be due to differences in the type of medical condition (cardiovascular vs. major depression) or the country in which the two studies were conducted (United States vs. Sweden)(Akerblad, Bengtsson, Holgersson, von Knorring, & Ekselius, 2008; Bender, Pedan, & Varasteh, 2006; Rolnick, Pawloski, Hedblom, Asche, & Bruzek, 2013).
It was not surprising that education also had both a linear and non-linear relationship with medication adherence in our analyses. We would expect that patients with more schooling would be exposed to more information about the role of medication adherence and health. What was surprising, however, was the shape of the lower part of the tail for education in the adjusted analysis where it appeared that patients with only a high school diploma were more adherent than those with a college degree. More research is required in order to validate this perhaps counter-intuitive result.
As a group, the strongest predictors of medication adherence in this study were the psychosocial variables, specifically perceived health competence, depressive mood, and social support. Our results support the findings of prior work (Burke, 1997; Davis et al., 2012; DiMatteo, 2004a, 2004b; Krall Scherer, 2001; Kripalani, 2008; Kronish, 2006; Molassiotis, 2002; Ni, 1999; Osterberg, 2005; Sarkar, 2006), but what is unique about our study is the demonstration that all three of these constructs independently influence adherence, even when adjusting for other factors and each other. Cardiovascular patients who believe themselves capable of taking care of their own health, who exhibit few symptoms of depression, and/or who perceive support from other people in their lives are less likely to exhibit medication non-adherence. Like numeracy and health literacy, these psychosocial factors are addressable in the outpatient setting. The clinical and health system implications of these findings are that population health programs which successfully address these targets through educational and behavioral interventions could yield downstream health benefits including reduced ED visits and hospitalization, as well as lower cardiovascular morbidity and mortality.
Among the strengths of this study are its large sample size, little missing data, and rigorous statistical methods, including multiple imputation and examination of nonlinear effects. Also, inclusion of three known psychosocial predictors of adherence in the same analysis with health literacy, numeracy, and the other covariates allowed us to see whether each of them remain significant in the presence of the others.
Nevertheless, this study had several limitations. First, generalizability may be limited by the focus on acute cardiovascular hospitalizations and most of the patients having been recruited from two hospitals in Middle Tennessee, although they were referred to those hospitals from a wide geographical area. Second, health literacy and medication adherence were measured by patient self-report, which may be influenced by social desirability bias and a ceiling effect. Third, patients were asked to report their recent (pre-hospital) medication adherence and other variables were collected concurrently. The cross-sectional nature of the analysis limits causal inferences. Fourth, we did not specifically assess the extent to which medication non-adherence contributed to the patients’ hospitalization, as this would have required detailed clinical review that was beyond the scope of the study.
CONCLUSION
Medication non-adherence is common prior to cardiovascular hospitalization. This study identified several factors that are independently associated with non-adherence, including low health literacy, numeracy, social support, perceived health competence, and greater depressive symptoms, which represent potential targets for intervention in population health management. Future research should directly test interventions that identify and address these factors through educational, behavioral, and social interventions in both inpatient and outpatient settings, and assess the effect on disease control and hospitalization rates.
Acknowledgments
We acknowledge the following additional members of the VICS research team who contributed to the study design or conduct: Susan P. Bell, MD, MSCI; Courtney Cawthon, MPH; Catherine Couey; Katharine M. Donato, PhD; Vanessa Fuentes; Frank E. Harrell, PhD; Blake Hendrickson; Cardella Leak, MPH; Daniel Lewis; Abby G. Meyers, MD; Russell L. Rothman, MD, MPP; John F. Schnelle, PhD; Eduard E. Vasilevskis, MD, MPH; Kelly H.S. Wright, MA.
Funded by the National Heart, Lung, and Blood Institute (R01 HL109388) and in part by the National Center for Advancing Translational Sciences (2 UL1 TR000445-06). Additional funding includes K12HL109019 and K23 HL125670. The content is solely the responsibility of the authors and does not necessarily represent official views of the National Institutes of Health. The authors’ funding sources did not participate in the planning, collection, analysis or interpretation of data or in the decision to submit for publication.
References
- (CDC), Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Survey Questionnaire. Atlanta, Georgia: 2010. [Google Scholar]
- Akerblad AC, Bengtsson F, Holgersson M, von Knorring L, Ekselius L. Identification of primary care patients at risk of nonadherence to antidepressant treatment. Patient Prefer Adherence. 2008;2:379–386. doi: 10.2147/ppa.s3511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali RC, Melloni C, Ou FS, Schmader K, Ohman EM, Roe MT, Alexander KP. Age and persistent use of cardiovascular medication after acute coronary syndrome: results from medication applied and sustained over time. J Am Geriatr Soc. 2009;57(11):1990–1996. doi: 10.1111/j.1532-5415.2009.02483.x. [DOI] [PubMed] [Google Scholar]
- Apter AJ, Wan F, Reisine S, Bender B, Rand C, Bogen DK, Morales KH. The association of health literacy with adherence and outcomes in moderate-severe asthma. J Allergy Clin Immunol. 2013;132(2):321–327. doi: 10.1016/j.jaci.2013.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bender BG, Pedan A, Varasteh LT. Adherence and persistence with fluticasone propionate/salmeterol combination therapy. J Allergy Clin Immunol. 2006;118(4):899–904. doi: 10.1016/j.jaci.2006.07.002. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Blumenthal J, Burg M, Carney RM, Catellier D, Cowan MJ, Czajkowski SM, DeBusk R, Hosking J, Jaffee A, Kaufmann PG, Mitchell P, Norman J, Powell LH, Raczynski JM, Schneiderman N. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: The Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) randomized trial. JAMA: Journal of the American Medical Association. 2003;289(23):3106–3116. doi: 10.1001/jama.289.23.3106. [DOI] [PubMed] [Google Scholar]
- Bitton A, Choudhry NK, Matlin OS, Swanton K, Shrank WH. The impact of medication adherence on coronary artery disease costs and outcomes: a systematic review. Am J Med. 2013;126(4):357 e357–357 e327. doi: 10.1016/j.amjmed.2012.09.004. [DOI] [PubMed] [Google Scholar]
- Burke LE, Dunbar-Jacob JM, Hill MN. Compliance with cardiovascular disease prevention strategies: A review of the research. Annals of Behavioral Medicine. 1997;19(3):239–263. doi: 10.1007/BF02892289. [DOI] [PubMed] [Google Scholar]
- Chan DC, Shrank WH, Cutler D, Jan S, Fischer MA, Liu J, Choudhry NK. Patient, physician, and payment predictors of statin adherence. Med Care. 2010;48(3):196–202. doi: 10.1097/MLR.0b013e3181c132ad. [DOI] [PubMed] [Google Scholar]
- Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Family Medicine. 2004;36(8):558–594. [PubMed] [Google Scholar]
- Cohen MJ, Shaykevich S, Cawthon C, Kripalani S, Paasche-Orlow MK, Schnipper JL. Predictors of medication adherence postdischarge: the impact of patient age, insurance status, and prior adherence. J Hosp Med. 2012;7(6):470–475. doi: 10.1002/jhm.1940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis DP, Jandrisevits MD, Iles S, Weber TR, Gallo LC. Demographic, socioeconomic, and psychological factors related to medication non-adherence among emergency department patients. J Emerg Med. 2012;43(5):773–785. doi: 10.1016/j.jemermed.2009.04.008. [DOI] [PubMed] [Google Scholar]
- Dickson VV, McCarthy MM, Howe A, Schipper J, Katz SM. Sociocultural influences on heart failure self-care among an ethnic minority black population. J Cardiovasc Nurs. 2013;28(2):111–118. doi: 10.1097/JCN.0b013e31823db328. [DOI] [PubMed] [Google Scholar]
- DiMatteo MR. Social Support and Patient Adherence to Medical Treatment: A Meta-Analysis. 2004a;23:207–218. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- DiMatteo MR. Variations in patients’ adherence to medical recommendations: A quantitative reivew of 50 years of research. Med Care. 2004b;42(3):200–209. doi: 10.1097/01.mlr.0000114908.90348.f9. [DOI] [PubMed] [Google Scholar]
- Fagerlin A, Zikmund-Fisher BJ, Ubel PA, Jankovic A, Derry HA, Smith DM. Measuring numeracy without a math test: development of the Subjective Numeracy Scale. Med Decis Making. 2007;27(5):672–680. doi: 10.1177/0272989X07304449. [DOI] [PubMed] [Google Scholar]
- Fitzgerald AA, Powers JD, Ho PM, Maddox TM, Peterson PN, Allen LA, Havranek EP. Impact of medication nonadherence on hospitalizations and mortality in heart failure. J Card Fail. 2011;17(8):664–669. doi: 10.1016/j.cardfail.2011.04.011. [DOI] [PubMed] [Google Scholar]
- Gazmararian JA, Kripalani S, Miller MJ, Echt KV, Ren J, Rask K. Factors associated with medication refill adherence in cardiovascular-related diseases: a focus on health literacy. J Gen Intern Med. 2006;21(12):1215–1221. doi: 10.1111/j.1525-1497.2006.00591.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell Frank E. Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis. New York: Springer; 2001. [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)- A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heidenreich PA. Capsule commentary on Zhang et al., Race/ethnicity, disability, and medication adherence among medicare beneficiaries with heart failure. J Gen Intern Med. 2014;29(4):648. doi: 10.1007/s11606-013-2736-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho PM, Spertus JA, Masoudi FA, Reid KJ, Peterson ED, Magid DJ, Rumsfeld JS. Impact of medication therapy discontinuation on mortality after myocardial infarction. Arch Intern Med. 2006;166(17):1842–1847. doi: 10.1001/archinte.166.17.1842. [DOI] [PubMed] [Google Scholar]
- Jackevicius CA, Li P, Tu JV. Prevalence, predictors, and outcomes of primary nonadherence after acute myocardial infarction. Circulation. 2008;117(8):1028–1036. doi: 10.1161/CIRCULATIONAHA.107.706820. [DOI] [PubMed] [Google Scholar]
- Krall Scherer Y, Bruce S. Knowledge, attitudes, and self-efficacy and compliance with medical regimen, number of emergency department visits, and hospitalizations in adults with asthma. Heart & Lung. 2001;30(4):250–257. doi: 10.1067/mhl.2001.116013. [DOI] [PubMed] [Google Scholar]
- Kripalani S, Henderson LE, Jacobson TA, Vaccarino V. Medication use among inner-city patients after hospital discharge: patient-reported barriers and solutions. Mayo Clin Proc. 2008;83(5):529–535. doi: 10.4065/83.5.529. [DOI] [PubMed] [Google Scholar]
- Kripalani S, Henderson LE, Jacobson TA, Vaccarino V. Medication use among inner-city patients after hospital discharge: Patient-reported barriers and solutions. Mayo Clinic Proceedings. 2008;83(5):529–535. doi: 10.4065/83.5.529. [DOI] [PubMed] [Google Scholar]
- Kripalani S, Risser J, Gatti ME, Jacobson TA. Development and evaluation of the Adherence to Refills and Medications Scale (ARMS) among low-literacy patients with chronic disease. Value Health. 2009;12(1):118–123. doi: 10.1111/j.1524-4733.2008.00400.x. [DOI] [PubMed] [Google Scholar]
- Kroenke K, et al. The PHQ-8 as a measure of current depression in the general population. Jounral of Affective Disorders. 2009;114:163–173. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- Kronish IM, Rieckmann N, Halm EA, Shimbo D, Vorchheimer D, Haas DC, Davidson KW. Persistent depression affects adherence to secondary prevention behaviors after acute coronary syndromes. Journal of General Internal Medicine. 2006;21:1178–1183. doi: 10.1111/j.1525-1497.2006.00586.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewey J, Shrank WH, Bowry AD, Kilabuk E, Brennan TA, Choudhry NK. Gender and racial disparities in adherence to statin therapy: a meta-analysis. Am Heart J. 2013;165(5):665–678. 678–e661. doi: 10.1016/j.ahj.2013.02.011. [DOI] [PubMed] [Google Scholar]
- Loke YK, Hinz I, Wang X, Salter C. Systematic review of consistency between adherence to cardiovascular or diabetes medication and health literacy in older adults. Ann Pharmacother. 2012;46(6):863–872. doi: 10.1345/aph.1Q718. [DOI] [PubMed] [Google Scholar]
- Marcum ZA, Zheng Y, Perera S, Strotmeyer E, Newman AB, Simonsick EM, Hanlon JT. Prevalence and correlates of self-reported medication non-adherence among older adults with coronary heart disease, diabetes mellitus, and/or hypertension. Res Social Adm Pharm. 2013 doi: 10.1016/j.sapharm.2012.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayberry LS, Gonzalez JS, Wallston KA, Kripalani S, Osborn CY. The ARMS-D out performs the SDSCA, but both are reliable, valid, and predict glycemic control. Diabetes Res Clin Pract. 2013;102(2):96–104. doi: 10.1016/j.diabres.2013.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNaughton CD, Cavanaugh KL, Kripalani S, Rothman RL, Wallston KA. Validation of a Short, 3-Item Version of the Subjective Numeracy Scale. Med Decis Making. 2015 doi: 10.1177/0272989X15581800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNaughton CD, Collins SP, Kripalani S, Rothman R, Self WH, Jenkins C, Storrow AB. Low numeracy is associated with increased odds of 30-day emergency department or hospital recidivism for patients with acute heart failure. Circ Heart Fail. 2013;6(1):40–46. doi: 10.1161/CIRCHEARTFAILURE.112.969477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNaughton CD, Jacobson TA, Kripalani S. Low literacy is associated with uncontrolled blood pressure in primary care patients with hypertension and heart disease. Patient Educ Couns. 2014;96(2):165–170. doi: 10.1016/j.pec.2014.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melloni C, Alexander KP, Ou FS, LaPointe NM, Roe MT, Newby LK, Peterson ED. Predictors of early discontinuation of evidence-based medicine after acute coronary syndrome. Am J Cardiol. 2009;104(2):175–181. doi: 10.1016/j.amjcard.2009.03.013. [DOI] [PubMed] [Google Scholar]
- Meyers AG, Salanitro A, Wallston KA, Cawthon C, Vasilevskis EE, Goggins KM, Kripalani S. Determinants of health after hospital discharge: rationale and design of the Vanderbilt Inpatient Cohort Study (VICS) BMC Health Serv Res. 2014;14:10. doi: 10.1186/1472-6963-14-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mixon AS, Myers AP, Leak CL, Lou Jacobsen JM, Cawthon C, Goggins KM, Kripalani S. Characteristics associated with postdischarge medication errors. Mayo Clin Proc. 2014;89(8):1042–1051. doi: 10.1016/j.mayocp.2014.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molassiotis A, Nahas-Lopez V, Chung WYR, Lam SWC, Li CKP, Lau TFJ. Factors associated with adherence to antiretroviral medication with HIV-infected patients. International Journal of STD & AIDS. 2002;13:301–310. doi: 10.1258/0956462021925117. [DOI] [PubMed] [Google Scholar]
- Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- Ni H, Nauman D, Burgess D, Wise K, Crispell K, Hershberger RE. Factors influencing knowledge of and adherence to self-care among patients with heart failure. Archives of Internal Medicine. 1999;159:1613–1619. doi: 10.1001/archinte.159.14.1613. [DOI] [PubMed] [Google Scholar]
- Noureldin M, Plake KS, Morrow DG, Tu W, Wu J, Murray MD. Effect of health literacy on drug adherence in patients with heart failure. Pharmacotherapy. 2012;32(9):819–826. doi: 10.1002/j.1875-9114.2012.01109.x. [DOI] [PubMed] [Google Scholar]
- Osborn CY, Cavanaugh K, Wallston KA, Kripalani S, Elasy TA, Rothman RL, White RO. Health literacy explains racial disparities in diabetes medication adherence. J Health Commun. 2011;16(Suppl 3):268–278. doi: 10.1080/10810730.2011.604388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osborn CY, Wallston KA, Shpigel A, Cavanaugh K, Kripalani S, Rothman RL. Development and validation of the General Health Numeracy Test (GHNT) Patient Educ Couns. 2013;91(3):350–356. doi: 10.1016/j.pec.2013.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osterberg L, Blaschke T. Adherence to medication. The New England Journal of Medicine. 2005;353:487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- Roebuck MC, Liberman JN, Gemmill-Toyama M, Brennan TA. Medication adherence leads to lower health care use and costs despite increased drug spending. Health Aff (Millwood) 2011;30(1):91–99. doi: 10.1377/hlthaff.2009.1087. [DOI] [PubMed] [Google Scholar]
- Rolnick SJ, Pawloski PA, Hedblom BD, Asche SE, Bruzek RJ. Patient characteristics associated with medication adherence. Clin Med Res. 2013;11(2):54–65. doi: 10.3121/cmr.2013.1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothman RL, Housam R, Weiss H, Davis D, Gregory R, Gebretsadik T, Elasy TA. Patient understanding of food labels: the role of literacy and numeracy. Am J Prev Med. 2006;31(5):391–398. doi: 10.1016/j.amepre.2006.07.025. [DOI] [PubMed] [Google Scholar]
- Sarkar U, Fisher L, Schillinger D. Is self-efficacy associated with diabetes self-management across race/ethnicity and health literacy? Diabetes Care. 2006;29(4):823–829. doi: 10.2337/diacare.29.04.06.dc05-1615. [DOI] [PubMed] [Google Scholar]
- Smith MS, Wallston KA, Smith CA. The development and validation of the Perceived Health Competence Scale. Health Educ Res. 1995;10(1):51–64. doi: 10.1093/her/10.1.51. [DOI] [PubMed] [Google Scholar]
- Steiner JF, Ho PM, Beaty BL, Dickinson LM, Hanratty R, Zeng C, Estacio RO. Sociodemographic and clinical characteristics are not clinically useful predictors of refill adherence in patients with hypertension. Circ Cardiovasc Qual Outcomes. 2009;2(5):451–457. doi: 10.1161/CIRCOUTCOMES.108.841635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldrop-Valverde D, Jones DL, Gould F, Kumar M, Ownby RL. Neurocognition, health-related reading literacy, and numeracy in medication management for HIV infection. AIDS Patient Care STDS. 2010;24(8):477–484. doi: 10.1089/apc.2009.0300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldrop-Valverde D, Osborn CY, Rodriguez A, Rothman RL, Kumar M, Jones DL. Numeracy skills explain racial differences in HIV medication management. AIDS Behav. 2010;14(4):799–806. doi: 10.1007/s10461-009-9604-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallston KA. Conceptualization and operationalization of perceived control. In: Baum TRA, Singer JE, editors. The Handbook of Health Psychology. Mahway, NJ: Erlbaum; 2001. pp. 49–58. [Google Scholar]
- Wallston KA, Cawthon C, McNaughton CD, Rothman RL, Osborn CY, Kripalani S. Psychometric properties of the brief health literacy screen in clinical practice. J Gen Intern Med. 2014;29(1):119–126. doi: 10.1007/s11606-013-2568-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu JR, Lennie TA, De Jong MJ, Frazier SK, Heo S, Chung ML, Moser DK. Medication adherence is a mediator of the relationship between ethnicity and event-free survival in patients with heart failure. J Card Fail. 2010;16(2):142–149. doi: 10.1016/j.cardfail.2009.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Baik SH. Race/Ethnicity, disability, and medication adherence among medicare beneficiaries with heart failure. J Gen Intern Med. 2014;29(4):602–607. doi: 10.1007/s11606-013-2692-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zikmund-Fisher BJ, Smith DM, Ubel PA, Fagerlin A. Validation of the Subjective Numeracy Scale: effects of low numeracy on comprehension of risk communications and utility elicitations. Med Decis Making. 2007;27(5):663–671. doi: 10.1177/0272989X07303824. [DOI] [PubMed] [Google Scholar]


