Abstract
Chlamydiae are obligate intracellular pathogens that replicate within a membrane-bound compartment (the inclusion) and are associated with important human diseases, such as trachoma, pneumonia, and atherosclerosis. We have examined the interaction of the host autophagic pathway with Chlamydia trachomatis serovar L2 by using the specific autophagosomal stain monodansylcadaverine, antibodies to autophagosome-associated markers, and traditionally used autophagic inhibitors, particularly 3-methyladenine and amino acids. Chlamydial inclusions did not sequester monodansylcadaverine, suggesting absence of fusion with autophagosomes. Interestingly, exposure of cultures infected for 19 h to 3-methyladenine or single amino acids until the end of infection (44 h) caused various degrees of abnormalities in the inclusion maturation and in the progeny infectivity. Incubation of host cells with chemicals throughout the entire period of infection modulated the growth of Chlamydia even more dramatically. Remarkably, autophagosomal markers MAP-LC3 and calreticulin were redistributed to the inclusion of Chlamydia, a process that appears to be sensitive to 3-methyladenine and some amino acids. The present data indicate the lack of autophagosomal fusion with the inclusion because it was devoid of monodansylcadaverine and no distinct rim of autophagosomal protein-specific staining around the inclusion could be observed. However, high sensitivity of Chlamydia to conditions that could inhibit host autophagic pathway and the close association of MAP-LC3 and calreticulin with the inclusion membrane still suggest a potential role of host autophagy in the pathogenesis of Chlamydia.
Chlamydiae are obligate intracellular bacterial pathogens that infect eukaryotic cells and live within a cytoplasmic vacuole or an inclusion (42, 43). Chlamydiae consist of several species that undergo a biphasic developmental cycle over a period of 44 to 72 h, depending on the chlamydial strain. Infection of eukaryotic host cells is initiated by the metabolically inactive and the infectious elementary bodies (EBs). Through largely unknown mechanisms, EBs attach to and induce their internalization by host cells. Within the first few hours postinfection (p.i.), EBs differentiate to the larger and more pleomorphic reticulate bodies (RBs), which are metabolically active, noninfectious, and replicative. At the end of a successful developmental cycle, the cell lyses, releasing the EBs (42, 43).
One of the important species of Chlamydia is Chlamydia trachomatis responsible for several significant human diseases, including trachoma, the leading cause of infectious blindness worldwide. It is also the most common cause of sexually transmitted diseases (51, 55). This species consists of several strains or serovars: lymphogranuloma venereum (LGV) strains (serovars L1, L2, and L3) and non-LGV strains (serovars A to K) (54).
It has been speculated that chlamydiae obtain metabolic precursors, which are required for growth and multiplication, such as amino acids, glycolytic and tricarboxylic substrates, and nucleotides from host pools (21, 24, 25, 31, 38, 61). Several mechanisms of nutrient acquisition used by intracellular pathogens were excluded in the case of Chlamydia. For example, these bacteria do not have access to nutrients present in lysosomes, since chlamydial inclusion avoids fusion with these nutrient-laden organelles (3, 27). Further, the chlamydial inclusion does not allow free exchange of molecules as small as 520 Da across its membrane (26). However, it appears to be freely permeable to cytoplasmic ions (21). Another source of nutrients for the replicating chlamydiae may be provided by the interaction with early endosomes (4, 62), which significantly accumulate close to the inclusion, or by fusion with vesicles derived from the Golgi (12). Another possibility, not yet been documented, is that the inclusion membrane possesses specific active transport systems for the uptake of free amino acids, nucleotides, and other nutrients from the intracytoplasmic pool.
Since chlamydiae rely on nutrients from the host cell, any deviation in the levels of nutrients available to Chlamydia would markedly affect the normal chlamydial development. Indeed, in vitro evidence demonstrates that limiting availability of metabolites such as amino acids, glucose, and iron induced the production of aberrant chlamydial forms with reduced infectivity (1, 2, 4, 13, 14, 23, 52). However, increasing levels of the soluble metabolites by reintroduction of metabolites into starved cultures or by adding the eukaryotic protein synthesis repressor cycloheximide into infected cell cultures starved or grown under standard conditions recovers or improves the growth and the infectivity of chlamydiae (1, 4, 24, 40, 52). These findings emphasize the competition between host and pathogen for the intracytoplasmic pool of nutrients (24, 42).
There are at least three possible sources for the soluble essential metabolites available in the cytoplasm of the host cell: (i) through the entry of a wide range of extracellular nutrients and solutes through the host cell membrane by means of diffusion and transport systems; (ii) through the release of metabolites from nutrient-rich vesicles of the endosomal-lysosomal endocytic pathway that is involved in the fluid phase uptake (heterophagy); and (iii) through the release of biosynthetic precursors resulted from the degradation of endogenous cellular components by a process known as autophagy, a pathway that is widely used for the maintenance of cellular homeostasis (16, 17, 29, 57, 60). Autophagic degradation is initiated when organelles and portions of cytoplasm are sequestered in vacuoles called nascent autophagosomes (early autophagosomes) that are not acidic and do not have lysosomal hydrolases or lysosome-associated membrane proteins associated with them. These vacuoles acquire degradative enzymes upon fusion with lysosomes and then mature to autophagolysosomes (late autophagosomes), in which the vacuolar content is degraded and released into the cytosol (45, 48). Therefore, autophagic proteolysis is considered an important determinant of the intracellular biosynthetic precursor content (8, 34, 60).
A possible interaction of chlamydial inclusions with the autophagic pathway of the host cell may provide a source of nutrients for the replicating organisms. In the present study, in order to investigate whether the inclusion has autophagosomal characteristics, fluorescence microscopy of HEp-2 cells infected with C. trachomatis serovar L2 was carried out by using the specific autophagosomal fluorescent stain monodansylcadaverine (MDC) and antibodies against the autophagosome-associated markers microtubule-associated protein light chain 3 (MAP-LC3) and calreticulin. Further, some autophagic inhibitors such as 3-methyladenine (3-MA) and exogenously added individual amino acids were used combined with phase-contrast, confocal microscopy and electron microscopy (EM) and infectivity studies. Although we detected no MDC in the chlamydial inclusion, aggregates of MAP-LC3 and calreticulin were closely associated with the inclusion. The use of excess amino acids and 3-MA had dramatic effects on the progress of infection and the development of bacteria.
MATERIALS AND METHODS
Chemicals and antibodies.
RPMI medium was purchased from Invitrogen GmbH (Karlsruhe, Germany). Fetal bovine serum (FBS) was from Biochrom KG (Berlin, Germany). Cycloheximide, 3-MA, and the autofluorescent MDC were purchased from Sigma-Aldrich (Steinheim, Germany). Amino acids in the l configuration were from Sigma-Aldrich Merck (Darmstadt, Germany) or Fluka (Buchs, Germany). Rabbit polyclonal antibodies specific against the genus Chlamydia and human calreticulin were supplied from Milan Analytica AG (La Roche, Switzerland) and Affinity BioReagents (Golden, Colo.), respectively. Goat polyclonal antibodies to human MAP-LC3 were from Santa Cruz Biotechnology (Santa Cruz, Calif.). The IMAGEN kit for chlamydial detection was purchased from Dako (Hamburg, Germany). Secondary antibodies conjugated with fluorochromes were obtained from Molecular Probes (Leiden, The Netherlands). Cytotoxicity reagent WST-1 was from Roche (Mannheim, Germany). Glutaraldehyde and OsO4 were from Sigma-Aldrich. Polybed was obtained from Polysciences (Washington, D.C.).
Growth and purification of chlamydial stocks.
C. trachomatis LGV serovar L2 was routinely propagated in the human laryngeal epithelial HEp-2 cells (ATCC CCL23) grown in cell growth medium (CGM), which consists of RPMI medium supplemented with 2 mM glutamine, 25 mM HEPES, 10% (vol/vol) FBS, and 10 μg of gentamicin/ml. Stock organisms were prepared essentially as described previously (3, 4).
Preparation of infection media supplied with excess individual amino acids or 3-MA.
Autophagic inhibition can be already achieved by using adenine analogues and excess amino acids at millimolar concentrations (9, 16, 17, 19, 29, 37, 39, 47, 49, 56, 57). Chemicals used in the present study were 3-MA, three representatives of the nonessential amino acids (namely, l-asparagine [Asn], l-arginine [Arg], and l-tyrosine [Tyr]), and all essential amino acids except l-tryptophan. The essential amino acids examined here include l-lysine (Lys; dihydrochloride), l-valine (Val), l-histidine (His), l-threonine (Thr), l-phenylalanine (Phe), l-methionine (Met), l-isoleucine (Ile), and l-leucine (Leu). Chemicals were individually dissolved in the infection medium (IM), which is composed of RPMI supplemented with 2 mM glutamine, 25 mM HEPES, 5% (vol/vol) FBS, and 10 μg of gentamicin/ml. Concentrations prepared for Lys or 3-MA were 5 mM and for other amino acids were 10 mM. In addition, 30 mM concentration of Asn was used as recommended by Hoyvik et al. (29) and Schaible et al. (56). At these concentrations, neither inhibitor appeared to compromise host cell viability and morphology nor cause detachment (see below). The pH value of amino acid- or 3-MA-containing IM was adjusted to 7.28 by addition of 1.0 N HCl (Gibco-BRL, Paisley, Scotland). Solutions were then filter sterilized and stored at 4°C. Where required, lower concentrations of chemicals were prepared by diluting the 5 or 10 mM solutions in IM.
Cell cultures, infection, and treatment with amino acids and 3-MA.
HEp-2 cells were grown in six-well plates in CGM and incubated overnight at 5% CO2 and 37°C to allow adherence. To examine effects of excess free amino acids and 3-MA on the progress of infection, host cells were infected and chemicals were administered as follows: C. trachomatis L2 EBs were suspended in IM and added directly to the cells at a multiplicity of infection (MOI) of ∼1. The cultures were incubated at 5% CO2 and 35°C for 2 h. At the end of the incubation, infected cells were washed twice with IM and further incubated at similar conditions. At 19 h p.i., old medium was aspirated from the plates and replaced with 2 ml of IM containing one of the additives/well. For each treatment, two wells were assigned. As controls, infected cells in two wells were exposed to fresh IM without additives. Treated and untreated cells were allowed to incubate under conditions mentioned above until the end of the experiment (44 h p.i.).
In another number of experiments, host cells seeded in six-well plates were pretreated with IM plus one of the additives for 30 min before infection. EBs (MOI ∼1) diluted in IM containing the respective chemical were added to the cells and allowed to adsorb for 2 h at 5% CO2 and 35°C. The cells were rinsed two times and subsequently loaded with IM plus the respective chemical and further incubated until 44 h p.i., unless otherwise indicated. Control untreated cells were similarly infected and maintained in IM without extra amino acids or 3-MA.
Morphology of chlamydial inclusions and particles.
Development of infection and morphological changes in inclusions treated with autophagic inhibitors were visually determined by using either phase-contrast microscopy, immunofluorescence confocal microscopy, or EM. Treated and untreated infected cells seeded on plates were examined by Olympus IX50 phase-contrast microscope equipped with a video imaging system, and images were directly printed by using a Sony video graphic printer. For confocal microscopy, infected cells grown on coverslips were stained by using the IMAGEN Chlamydia kit as recommended by the manufacturer. The specimens were mounted with Mowiol and visualized on a Leica TCS-SP laser scanning confocal microscope with a krypton/argon laser. Images were processed by using Adobe Photoshop 6.0 and Microsoft PowerPoint.
To reveal ultrastructural features of inclusions in untreated control cells and in cells exposed to chemicals, cells infected for indicated times were washed with phosphate-buffered saline (PBS; pH 7.4) and fixed in 2.5% glutaraldehyde for 30 min. Cells were postfixed with 1% OsO4, dehydrated, and then embedded in Polybed. Specimens were then viewed in LEO 906E (A Carl Zeiss SMT AG Company, Oberkochen, Germany) transmission electron microscope.
Titration of infectivity yield of chlamydial inclusions.
Treated and untreated control cells were removed with sterile glass beads and the cells suspended in IM alone (controls) or with the respective chemicals were pooled and homogenized by vortexing with glass beads. Lysates were stored at −75°C or freshly utilized for the infectivity titer determination. The infectivity titer, expressed as the number of inclusion-forming units (IFU) per milliliter, was estimated as described elsewhere (4).
Labeling of cell cultures with MDC and detection of autophagosomal markers.
Autophagic vacuoles were detected with MDC according to the methods of Biederbick et al. (7) and Pizzaro-Cerdá et al. (46). Cell cultures infected for either 24 h or 48 h and grown on coverslips in the absence of autophagic inhibitors were incubated with IM without FBS and glutamine for 30 min to 2 h to increase autophagy. Cells were then incubated with serum- and glutamine-free IM containing a 0.05 mM concentration of the vital stain MDC for 30 min to 3 h. After two washes with PBS, the cells were inverted onto microscopic slides and examined immediately with a Leica epifluorescence microscope equipped with a 365-nm excitation filter and a 545-nm barrier filter and connected to a digital camera. Immunofluorescence staining to visualize MAP-LC3 or calreticulin was performed as previously described (3, 4). The images were processed with Adobe Photoshop 6.0 and Microsoft PowerPoint.
Cytotoxicity test and estimation of host cell proliferation.
The effect of excess amino acids and 3-MA on the proliferation capacity of HEp-2 cells was estimated as follows: equal numbers of uninfected host cells suspended in CGM were seeded in six-well plates and incubated overnight in a humidified cell chamber at 35°C and 5% CO2. On the next day and just prior to exposure to various chemicals, cells from two different wells were washed with sterile PBS (pH 7.2), treated with trypsin, and then diluted in a total volume of 1 ml per well with sterile PBS. The cell count in each well was immediately estimated by using an automatic cell counter (Schärfe System GmbH, Reutlingen, Germany). Average of cell numbers determined here would represent the initial number of cells per well just before exposure to chemicals. Subsequently, cells in two wells were exposed to one chemical and incubated as previously mentioned for an additional 48 h, at which time the cells were treated with trypsin, the cells per well were counted as described above, and the average of cell numbers obtained from each treatment was determined. The fold increase in cell number resulting from cell multiplication in the presence of each chemical was determined by dividing average number of cells per milliliter counted 48 h posttreatment with that chemical by the initial average number of cells per milliliter present in each well just prior to treatment (determined earlier). Cell monolayers unexposed to exogenous chemicals were included as controls.
To assess the effects of supply with excess free amino acids or with 3-MA on cell viability and metabolic activity, a WST-1 colorimetric assay was carried out. The assay is based on cleavage of the tetrazolium salt WST-1 by active mitochondria to produce a soluble colored formazan salt. HEp-2 cells were plated in 96-well plates in CGM. The next day, the medium was removed and replaced with 200 μl of IM alone (control) per well or with 200 μl of IM containing one of the chemicals per well; plates were then incubated for 2 days at 5% CO2 and 35°C. Next, 50 μl of the cell proliferation reagent WST-1 was added into each well. The cells were incubated for 2 h at 35°C in a humidified cell atmosphere with 5% CO2. The microplates were thoroughly shaken for 1 min, and the absorbance was measured at 450 nm by using a Spectra MAX 250 enzyme-linked immunosorbent assay plate reader (Molecular Devices, Calif.). The data were obtained from eight wells exposed to each chemical and were expressed subsequently as the mean percent metabolic activity (i.e., the mean of the optical densities of treated versus control untreated cultures multiplied by 100) ± the standard deviation from the mean.
For experiments in which host cells were incubated with chemicals for periods of up to 5 days, the viability of cells was determined at 3, 4, or 5 days by using MitoTracker staining (4).
Statistical analysis.
All experiments were done at least two times with similar outcomes. The data are presented as means ± the standard deviation from the means. In WST-1 test, statistical comparisons between groups were assessed by using the Student t test. The difference was considered significant when the P value is <0.05.
RESULTS
Effects of autophagic inhibitors on the maturation of C. trachomatis inclusion.
Autophagy can be inhibited by presence of excess amino acids and by adenine analogues. Thus, to further investigate any possible involvement of autophagy in chlamydial infection, we tested the action of 3-MA, three nonessential amino acids (Asn, Arg, and Tyr), and eight essential amino acids (Lys, Val, His, Thr, Phe, Met, Ile, and Leu). Host cells were treated with chemicals in two different ways. First, cells were infected and at 19 h p.i., time at which the number of C. trachomatis L2 RBs is maximized and already started reverting back to EBs (21, 44), 3-MA or specified amino acids were added until the end of the developmental cycle (44 h p.i.). In another set of experiments, cells were pretreated for 30 min with 3-MA or amino acids and then infected for 44 h in the continuous presence of respective chemicals.
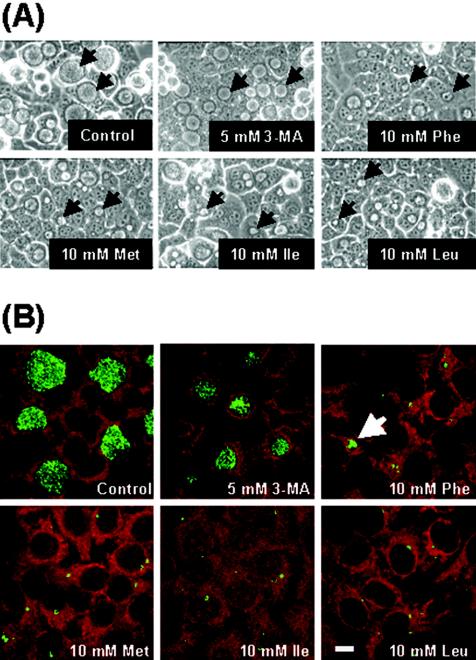
Qualitatively, examination by phase-contrast microscopy demonstrated that Lys, Asn, Arg, His, Tyr, and Thr had little or no effect on the inclusion size when they were introduced into infected cultures at 19 h p.i. until the end of the experiment (data not shown). However, similar treatments of infected monolayers with 3-MA, Phe, Met, Ile, or Leu dramatically arrested the inclusion growth, generating smaller inclusions than those in untreated infected cells (Fig. 1A, arrows).
FIG. 1.
Effect of excess individual amino acids and 3-MA on C. trachomatis L2 inclusion growth. (A) Cell monolayers were infected for 19 h and then exposed to IM containing exogenous individual amino acids or 3-MA. Microscopic examination was performed 44 h p.i., and phase-contrast images were obtained under the same magnification (×400). Inclusions are indicated by arrows. (B) Host cells were pretreated for 30 min with amino acids or 3-MA and then infected in the presence of respective chemicals until the end of the infection period (44 h). Cells were stained for Chlamydia (green) by using IMAGEN kit and examined by confocal microscopy. Bar, 10 μm.
Administration of 3-MA or the amino acids Lys, Asn, Arg, His, Tyr, or Thr 30 min before and during the infection led to similar effects on the maturation of inclusions, compared to those receiving the same chemicals at 19 h p.i. until the end of the infection (data not shown). Unexpectedly, very small aberrant inclusions developed in cells exposed to Phe, Met, Ile, and Leu that were only detected by immunofluorescence staining (Fig. 1B, green).
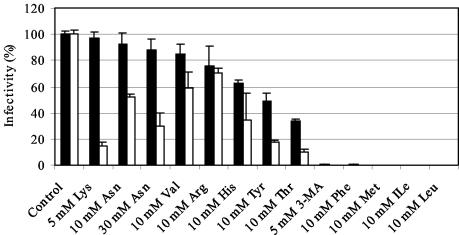
Effects of autophagic inhibitors on the infectivity of C. trachomatis.
Next, the production of infectious EBs developed in the presence of autophagic inhibitors was assessed by routinely used infectivity titration assays. The level of infectivity reduction was grouped into four categories: minimal (negligible) reduction (1 to 25% inhibition in IFU per milliliter); moderate reduction (26 to 50% reduction in infectivity); strong inhibition (51 to 75% reduction in infectivity); and a very strong reduction (76 to 100% reduction in infectivity). In experiments in which chemicals were added 19 h p.i. until the end of the infection course (44 h p.i.), Lys, Asn, Val, and Arg minimally inhibited the production of infectious EBs (Fig. 2, solid bars). In contrast, reduction in progeny infectivity was moderate in cells treated with His, whereas infectivity was strongly inhibited by Tyr and Thr. Interestingly, exposure to either 3-MA, Phe, Met, Ile, or Leu very strongly diminished the production of infectious chlamydial forms (>99% reduction), as shown in Fig. 2 (solid bars).
FIG. 2.
Effect of excess amino acids and 3-MA on C. trachomatis L2 infectivity in vitro. Chemicals were added 19 h p.i. until the end of the infection course (44 h) (▪). In another set of experiments, chemicals were present in the cell monolayers 30 min before infection and also during infection (□). At 44 h p.i., cells were lysed and passaged onto fresh HEp-2 cells for determination of the infectious progeny yield. The percent infectivity is a reflection of the reduction in the titer (in IFU/milliliter) in infected cultures exposed to each chemical compared to the titer in control unexposed cell cultures. The results are expressed as the means of the percentage of infectivity ± the averages of the absolute deviations from the means for two different experiments.
The inhibition of progeny infectivity obtained with amino acid and 3-MA treatments started at 19 h p.i. was dramatically different when the treatment was continuous. For instance, when continuously present in infected cell monolayers, Lys very strongly reduced the production of infectious chlamydiae by >85% (Fig. 2, open bar), compared to negligible inhibition in the infectivity when added 19 h p.i. The effect on the progeny infectivity was also pronounced in other treatments. Asn, Val, and Arg, which minimally inhibited the infectivity when added 19 h p.i., resulted in a moderate to strong inhibition of the progeny infectivity, as demonstrated in Fig. 2 (open bars). Moreover, continuous treatments with 3-MA, Met, Ile, or Leu during the infection completely diminished the infectivity of chlamydiae. In contrast, the continuous presence of Phe did not completely prevent infectious forms being produced, which could be attributed to occasionally seen relatively large inclusions (Fig. 1B, arrow).
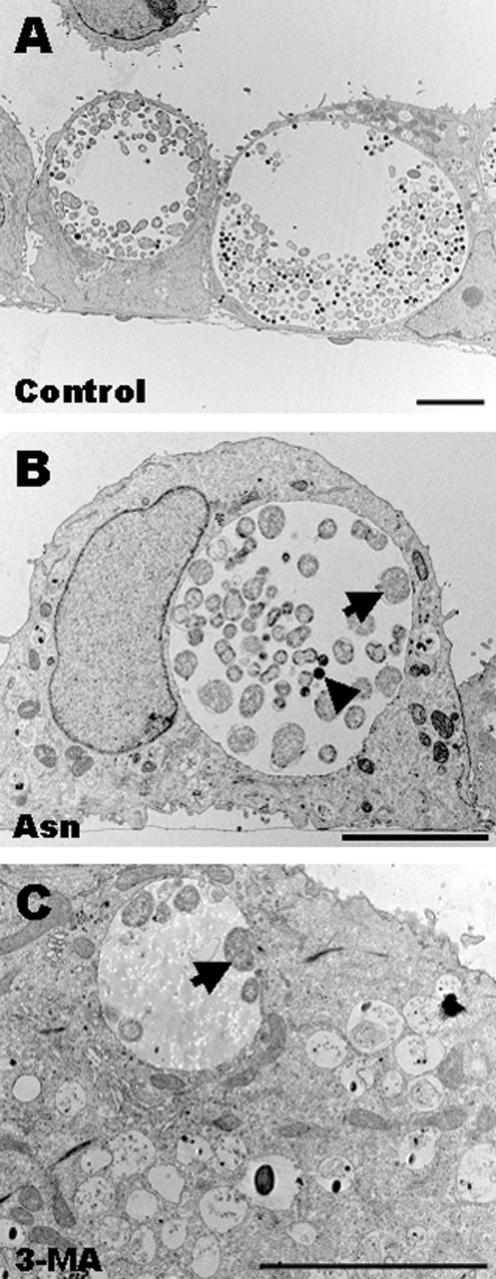
Effects of autophagic inhibitors on morphology of organisms.
The decrease in the chlamydial progeny infectivity, particularly in cells continuously exposed to autophagic inhibitors, could correlate with a delay in the developmental cycle and/or the formation of aberrant chlamydial forms. Hence, EM was used to examine chlamydiae grown in the continuous presence of amino acids and 3-MA. In 30 mM Asn-treated cells infected for 32 h, EM revealed the presence of morphologically unaltered chlamydiae that were mostly RBs (Fig. 3B, arrow). The presence of EBs was also observed but was infrequent (Fig. 3B, arrowhead) compared to control untreated cell cultures infected for the similar time period (Fig. 3A), indicating that Asn could delay the maturation of bacteria. In contrast, ultrastructural analysis of 3-MA-treated cells infected for 32 h confirmed the presence of small inclusions containing small number of RB forms (Fig. 3C, arrow).
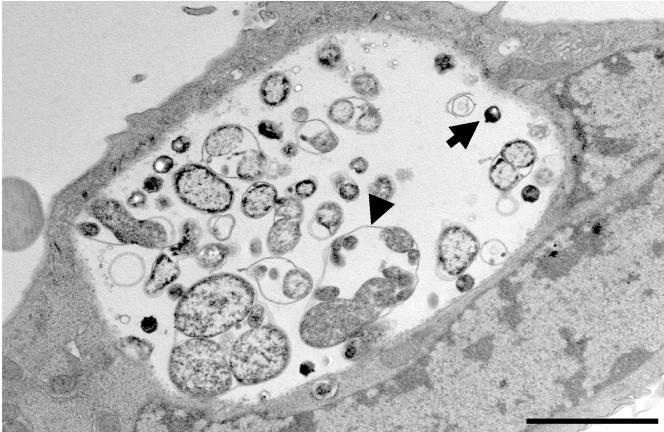
FIG. 3.
C. trachomatis L2 inclusions in cell monolayers exposed to 3-MA or exogenous excess Asn, as viewed by EM. Host cells were pretreated with one of the chemicals for 30 min and then infected for 32 h in the presence of the respective chemical. (A) Control inclusions developed for 32 h in medium without additives contained normal forms of chlamydiae. (B) Inclusions developed in the presence of 30 mM Asn. Inclusions here are less mature and contain mostly RBs (arrow) compared to control inclusions (see panel A). Few EBs were observed (arrowhead). (C) Inclusions grown in the presence of 5 mM 3-MA contained low number of chlamydial forms, which were exclusively RBs (arrow). Bars, 5 μm.
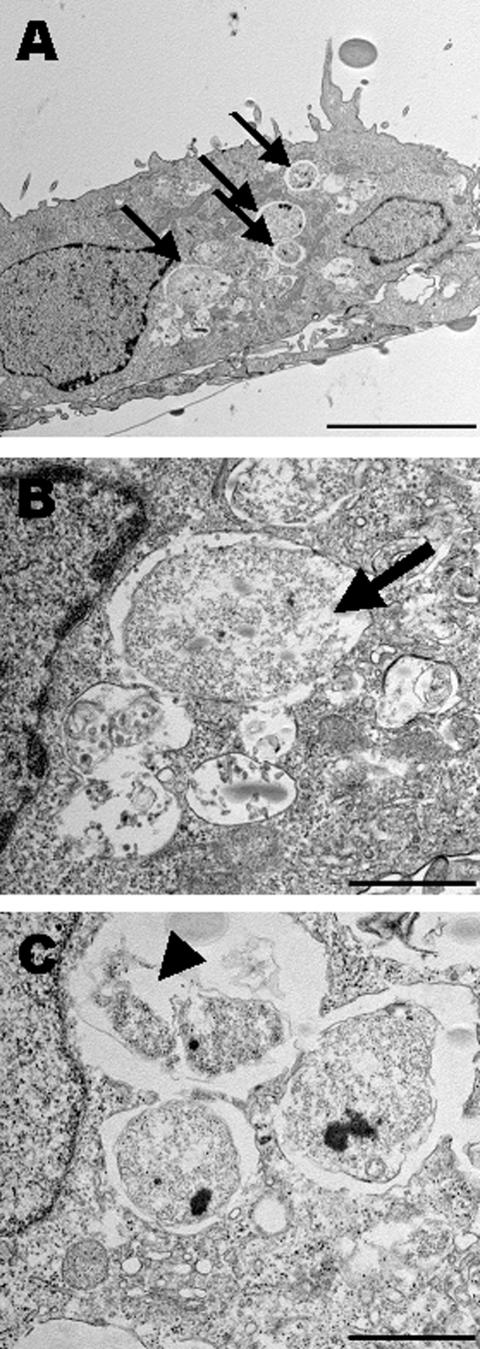
The addition of Leu, Ile, Met, and Phe before and during the infection produced very small aberrant inclusions (Fig. 1B). To characterize the morphology of developed inclusions, cell monolayers exposed to Met and then infected for 48 h with C. trachomatis at an MOI of ∼10 were selected to be processed for EM. Ultrathin sections revealed the presence of multiple very small inclusions per host cell that contained morphologically typical single RBs (Fig. 4A, arrows). In addition, continuous exposure to Met led to a partial destruction and distortion of some internalized bacteria (Fig. 4B and C, respectively). Interestingly, some of the observed inclusions were still in the process of homotypic fusion (Fig. 4C), a characteristic of C. trachomatis that should be completed within the first 24 h of infection.
FIG.4.
EM examination of chlamydial inclusions grown under conditions of a high Met concentration. Host cells pretreated with 10 mM Met were infected for 48 h with C. trachomatis L2 at an MOI ∼10 in the presence of Met. (A) Ultrathin sections revealed that Met led to a complete growth arrest of inclusions. Moreover, multiple inclusions per infected host cell were detected (arrows). Most of the inclusions contained single typical RBs. (B and C) In addition, EM provided evidence of abnormalities in some of the formed RBs. Some RBs were partially degraded (arrow in panel B), whereas others were atypical and distorted (arrowhead in C). Bars, 5 μm (A) and 1 μm (B and C).
Lys, when added at 19 h p.i., did not affect the size of inclusions (data not shown) and negligibly inhibited the yield of progeny infectivity (Fig. 2, closed bar). Interestingly, however, the presence of Lys before and during the infection very strongly diminished the infectivity yield (Fig. 2, open bar), despite the absence of any noticeable decrease in the inclusion size, compared to that of untreated inclusions (data not shown). To explain the dramatic effect observed on infectivity but not on the inclusion growth, the morphology of chlamydiae developed in host cells continuously exposed to Lys was defined by EM. Lys treatment was associated with a unique appearance of aggregates of RB-like forms of different sizes that were enclosed together within a loosened single membrane, possibly the bacterial outer membrane (Fig. 5, arrowhead). EB-like forms were also present (arrow). This unusual restraint of multiple bacteria in a common membrane indicated that binary fission is disrupted, in which the bacterial cells could divide but could not separate from each other, hindering possibly the transformation of daughter cells to infective EBs.
FIG. 5.
Morphology of C. trachomatis L2 inclusions developed in host cells exposed to 5 mM Lys 30 min before infection and until 48 h after infection. The major characteristic observed was the frequent presence of multiple RB-like forms that were enveloped, together with a single outer membrane. Notice the obvious loosening of the outer membrane (arrowhead). EB-like forms were also present (arrow). Bar, 2 μm.
Withdrawal of Leu, Ile, Met, and Phe restores chlamydial growth.
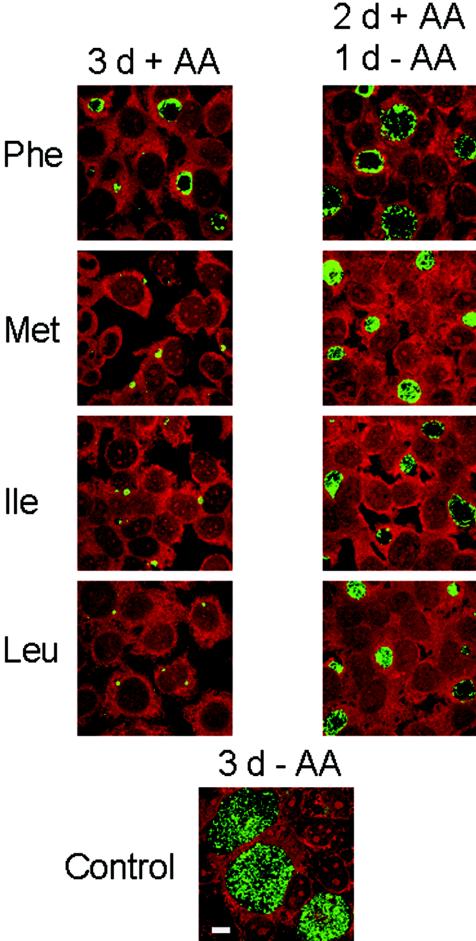
To determine whether inhibitory effects of Leu, Ile, Met, and Phe on the growth of chlamydiae are reversible, infected host cells were incubated for 2 days in the presence of either amino acids (10 mM each) and for an additional day in new IM without extra amino acids. As shown in Fig. 6, removal of extra amino acids restored the growth of chlamydiae, as revealed by the considerable increase in the inclusion size shown in the right panels, in contrast to inclusions grown for 72 h in IM containing extra amino acids that remained delayed in their maturation (Fig. 6, left panels). Of note, inclusions grown for 72 h in the presence of either Leu, Ile, Met, and Phe showed a slight increase in the inclusion size compared to those incubated for only 44 h in the presence of respective amino acids (e.g., compare inclusions in Phe-treated cells in Fig. 1B with those in Fig. 6). Importantly, inclusion size did not further increase if treated cultures were incubated for periods longer than 72 h.
FIG. 6.
Growth-inhibitory effects of excess Phe, Met, Ile, or Leu on C. trachomatis L2 can be simply reversed by additive removal. Left panels represent infected cell cultures that were continuously exposed to one of the additives for 72 h. Right panels represent infected cells that were incubated for 48 h with medium supplied with exogenous amino acids and for additional 24 h without additives in an attempt to restore the growth of inclusions. Replacement of medium generated an apparent recovery of inclusions (green). Bar, 10 μm.
Inclusions recovered by the removal of excess amino acids contained a mixture of morphologically normal chlamydial forms: RBs, some of which are dividing, intermediate bodies, and dense EBs, as revealed by EM (data not shown). Overall, these findings indicate that detrimental effects of certain exogenous amino acids on chlamydial growth can be reversed by restoring normal IM.
As mentioned above, prolonged treatments of infected cells with Leu, Ile, Met, or Phe very strongly or totally diminished the bacterial infectivity (Fig. 2, open bars). To determine whether infectious progeny can be formed in continuously treated cells over time, cell cultures were infected in the presence of 10 mM concentrations of either Leu, Ile, Met, or Phe for several intervals of times, as indicated in Table 1, and subsequently subpassaged onto fresh untreated cells to determine the chlamydial infectivity yield. Infectivity assessments indicated no recovery of EBs in infected cells incubated with either Leu, Ile, or Met for 1, 2, 3, 4, or 5 days (specimens 4 to 8). Similarly, long exposure of infected cells to Phe depressed the infectivity, which remained negligible and decreased over time. Collectively, these findings suggest that C. trachomatis cannot complete its developmental cycle when these amino acids are continuously present in the infected cell cultures.
TABLE 1.
Influence of prolonged exposures to either Leu, Ile, Met, or Phe on the production of infectious EBs and rescue of infectivity of C. trachomatis L2 by withdrawal of excess amino acidsa
| Specimen | Treatment duration (days)b | No. of IFU/ml harvested from infected cell cultures exposed to:
|
||||
|---|---|---|---|---|---|---|
| None | Leu | Ile | Met | Phe | ||
| 1 | 1 (−AA) | 4.16 × 103 | ||||
| 2 | 2 (−AA) | 2.61 × 108 | ||||
| 3 | 3 (−AA) | 3.98 × 107 | ||||
| 4 | 1 (+AA) | 0 | 0 | 0 | 0 | |
| 5 | 2 (+AA) | 0 | 0 | 0 | 3.22 × 104 | |
| 6 | 3 (+AA) | 0 | 0 | 0 | 4.51 × 103 | |
| 7 | 4 (+AA) | 0 | 0 | 0 | 1.37 × 103 | |
| 8 | 5 (+AA) | 0 | 0 | 0 | 1.15 × 103 | |
| 9 | 1 (+AA) | 5.88 × 107 | 6 × 107 | 6 × 107 | 4.22 × 107 | |
| 2 (−AA) | ||||||
| 10 | 2 (+AA) | 3.15 × 106 | 1.84 × 106 | 1.07 × 106 | 3.56 × 106 | |
| 2 (−AA) | ||||||
| 11 | 3 (+AA) | 2.38 × 105 | 3.86 × 104 | 2.14 × 104 | 5.64 × 105 | |
| 2 (−AA) | ||||||
| 12 | 4 (+AA) | 1.78 × 103 | 2.38 × 103 | 5.94 × 102 | 2.97 × 105 | |
| 2 (−AA) | ||||||
| 13 | 5 (+AA) | n | n | n | 4.16 × 105 | |
| 2 (−AA) | ||||||
Host cells were preincubated for 30 min with IM containing 10 mM Leu, Ile, Met, or Phe (specimens 4 to 13) and were then infected for various time intervals in the presence of respective amounts of amino acids. For some specimens (specimens 9 to 13), excess amino acid-containing medium was replaced with IM without exogenous amino acids, and then the cells were incubated for an additional 2 days in an attempt to rescue the bacterial infectivity. As controls, host cells were infected and incubated in IM without any exogenous amino acid for either 1, 2, or 3 days (specimens 1, 2, and 3, respectively). Each specimen was represented by two wells of six-well plates. At the end of the indicated time points, all specimens were harvested, disrupted, serially diluted, and inoculated onto fresh HEp-2 cells to determine the IFU/ml. n, Negligible.
−AA, without added amino acid; +AA, with added amino acid.
The question still remained as to whether the infectivity suppressed by these amino acids can be reverted by removal of excess amino acids. To address this question, cell cultures were infected in the presence of these amino acids for either 1, 2, 3, 4, or 5 days (Table 1, specimens 9 to 13). At these time points, culture IM containing the respective amino acids was replaced with fresh IM without additives, and the cell cultures were incubated for additional 2 days to allow the rescue of chlamydiae. The cells were then lysed and inoculated onto fresh HEp-2 cells for infectivity yield assessments. Table 1 generally confirms that replacement of IM containing exogenous amino acids at 1, 2, 3, 4, or 5 days posttreatment led to a recovery, although sometimes negligible, of bacterial infectivity (specimens 9 to 13). The time of amino acid removal seems to be critical, since restoration of infectious bacterial progeny was more efficient at earlier times of medium replacement compared to the infectivity yield obtained at later times. Overall, the data obtained suggest that the inhibition of the chlamydial infectivity induced by Leu, Ile, Met, and Phe can be simply reversed by the removal of excess amino acids and that the degree of rescue of chlamydial development is dramatically affected by prolonged exposures to amino acids.
Effect of lower doses of Leu, Ile, Met, Phe, and 3-MA on inclusion development and on infectivity of C. trachomatis serovar L2.
The growth-inhibitory effects of Leu, Ile, Met, Phe, and 3-MA, demonstrated previously, were determined by using high concentrations of chemicals that ranged from 5 (for 3-MA) to 10 mM (for amino acids). Here, we designed experiments to examine the effect of decreasing concentrations on inclusion growth and EB production. Chemicals were used at 1, 2.5, or 5 mM and were added 30 min before the infection and throughout the infection period (44 h). Inclusions developed in the presence of 1 mM Phe, Met, or 3-MA were the same size as the control untreated inclusions, whereas inclusions present in cultures exposed to 1 mM Leu or Ile appeared smaller by immunofluorescence microscopy (data not shown). However, inclusions generated by additions of chemicals at 2.5 and 5 mM were considerably smaller compared to the controls (data not shown). Most importantly, the size of inclusions decreased in a dose-dependent manner, according to the results obtained here and those indicated in Fig. 1B with 10 mM concentrations.
The development of infectious C. trachomatis progeny in cell cultures exposed to various concentrations of 3-MA, Leu, Ile, Met, and Phe was also reduced in a dose-dependent fashion (Table 2). Importantly, concentrations of Leu, Ile, and Met as low as 1 mM reduced the infectivity yield by >92%, despite a noticeable increase in the inclusion size, whereas 1 mM Phe or 3-MA was relatively less effective in inhibiting formation of infectious progeny. In addition, when chemicals used at higher concentrations (2.5 or 5 mM), development of infectious EBs was reduced by >96% or totally eliminated (Table 2).
TABLE 2.
Reduction in the production of infectious C. trachomatis L2 by exogenous amino acids and 3-MA is dose dependenta
| Chemical | Concn (mM)b | % Infectivity ± the SDc |
|---|---|---|
| None (control) | 100 ± 20.96 | |
| Leu | 1 | 2.54 ± 0.12 |
| 2.5 | 0.01 ± 0.005 | |
| 5 | 0 | |
| Ile | 1 | 2.13 ± 0.2 |
| 2.5 | 0.01 ± 0.003 | |
| 5 | 0 | |
| Met | 1 | 7.74 ± 0.7 |
| 2.5 | 0.04 ± 0.03 | |
| 5 | 0 | |
| Phe | 1 | 45.04 ± 11.52 |
| 2.5 | 3.24 ± 0.12 | |
| 5 | 0.23 ± 0.06 | |
| 3-MA | 1 | 25.01 ± 11.3 |
| 2.5 | 1.08 ± 0.14 |
The experiment was performed on two different occasions.
Host cells were preincubated for 30 min with exogenous amino acids at concentrations ranging from 1 to 5 mM or with either 1 or 2.5 mM 3-MA. Cells were subsequently infected with C. trachomatis L2 and incubated for an additional 44 h in the presence of respective amounts of the additives.
The percent infectivity of C. trachomatis L2 in each treatment was determined by dividing the IFU/milliliter estimated for that treatment by the IFU/milliliter of the control cell monolayers unexposed to exogenous amino acids or 3-MA multiplied by 100. The percent infectivity was expressed as the means for two different experiments ± the standard deviation from the means. The IFU/ml value was estimated as described in the legend for Table 1.
Chlamydial inclusions do not accumulate with the autophagosomal stain MDC.
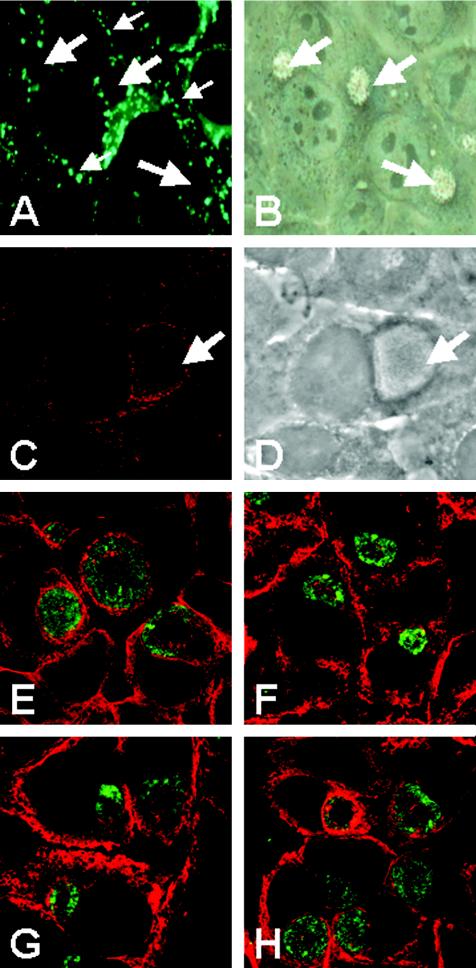
A possible interaction of chlamydial inclusions with autophagosomes was investigated by using MDC, an autofluorescent autophagosome-specific marker. This marker was used successfully in examining possible involvement of autophagy in bacterial infections such as Brucella (46), Porphyromonas (15), and Coxiella (6) infections. MDC colocalized with small vesicles distributed throughout the cytoplasm of cells infected for 24 h (Fig. 7A, small arrows) but not with the chlamydial inclusion (Fig. 7A, large arrows). Similar results were obtained with cells infected for 48 h (data not shown), indicating that the inclusion does not fuse with autophagosomes.
FIG. 7.
Distribution of the autophagosome-associated markers in cell monolayers infected with C. trachomatis. (A and B) Fluorescence localization of the autofluorescent marker MDC in HEp-2 cells as visualized by conventional epifluorescence microscopy. MDC (small arrows) did not accumulate in chlamydial inclusions (large arrows). The corresponding phase-contrast image of panel A is shown in panel B. (C and D) MAP-LC3 distribution in cell cultures infected for 43 h. Confocal images revealed concentration of MAP-LC3-positive structures (red) adjacent to the inclusion (arrow). Panel D is a phase-contrast image of panel C. (E to H) Confocal images showing the distribution of calreticulin in cells infected for 43 h in the absence of additives (E) or in the presence of 1 mM Leu (F), Ile (G), or 3-MA (H). Chemicals were added at 19 h p.i. for additional 24 h. Cells were then fixed and stained with suitable antibodies.
Autophagosome-associated proteins are found at the periphery of the chlamydial inclusion.
Next, we examined the distribution of MAP-LC3, an essential protein for autophagy that is associated with autophagosomal membranes (65). In uninfected cells, immunofluorescence of this protein showed a fine granular distribution pattern throughout the cytoplasm (data not shown). In infected cells, interestingly, MAP-LC3-containing structures remarkably concentrated (Fig. 7C, red) at the periphery of the inclusion (Fig. 7C, arrows). A distinct fluorescence rim was not apparent around the inclusion, suggesting that MAP-LC3 was not incorporated into the inclusion membrane.
Majeed et al. (36) have shown that endoplasmic reticulum (ER) proteins, particularly SERCA2 and calreticulin, are intimately associated with chlamydial inclusions. Since it has been proposed that the membrane source of autophagosomes may be from the ER membranes (18), accumulation of these markers, in addition to MAP-LC3, adjacent to the inclusion may strengthen the hypothesis that a potential interaction of the autophagic pathway with the inclusion may exist. Here, we demonstrated again the notable localization of calreticulin (Fig. 7E, red) around the inclusion (Fig. 7E, green). To examine whether calreticulin presence near the inclusion is probably sensitive to chemicals used in the present study, we infected cells for 19 h and then incubated them for an additional 24 h with 1 mM 3-MA, Leu, Ile, or Met, chemicals that showed maximal growth-inhibitory effects, or with 1 mM Arg, an amino acid that exhibited minimal adverse effects on the inclusion size and infectivity. Changes in calreticulin distribution in response to the additives were studied by using confocal microscopy and compared to untreated infected cell cultures. In untreated infected cells, ca. 87% of cells showed strong labeling of calreticulin around inclusions (consistent with findings shown in reference 36) compared to ∼35, 61, 31, and 67% in Leu-, Met-, Ile-, and 3-MA-treated cells, respectively. However, Arg slightly reduced number of infected cells (∼83%), showing the typical strong calreticulin staining in the vicinity of the inclusion (Fig. 7E to H [images for cells treated with Met and Arg are not shown]). Unfortunately, we were not able to estimate sensitivity of MAP-LC3 accumulation to chemicals used due to the relatively low intensity staining of this protein in the treated and untreated infected cells compared to that of calreticulin. Taken together, the capacity of 3-MA, Leu, Ile, and Met, but not Arg, to appreciably prevent the redistribution of calreticulin to bacterial inclusions could provide a link between the inhibitory effects of these chemicals on chlamydial growth and autophagy modulation.
Effect of 3-MA and excess amino acids on host cells.
Initial experiments were performed on uninfected HEp-2 cells to determine toxicity of chemicals used and their effects on host cell viability and growth rate. Cell cultures were incubated for 48 h in IM supplied with the highest concentrations of individual free amino acids used in the present study. In addition, cell monolayers were treated with 3-MA at concentrations ranging from 1 to 5 mM. When treated cell cultures were examined by light microscopy, these concentrations appeared to be well tolerated by HEp-2 cell monolayers, which remained intact. Host cell viability was not affected as detected by the fluorescent MitoTracker (data not shown). Some chemicals had no effect on the rate of cell duplication (data not shown). However, other chemicals slowed, but did not halt, host cell replication. These results were corroborated by the WST-1 colorimetric assay used to analyze the metabolic activity of treated cells (data not shown), reflecting the proliferation rate and viability of cell cultures.
For some experiments where host cells were incubated with amino acids for periods up to 5 days (Table 1), the viability of cells was determined at 3, 4, or 5 days by using MitoTracker staining. Long-term amino acid exposure did not compromise the cell viability as detected by immunofluorescence microscopy (data not shown).
DISCUSSION
Autophagy is a major pathway for turnover of cytoplasmic components including mitochondria, peroxisomes, smooth and rough membranes, proteins, glycogen, neutral lipids, RNA, and ribosomes (16, 17, 34, 41, 53, 57). Autophagy is initiated by sequestration of cytoplasmic organelles or cytoplasmic fractions into an early autophagosome that is transformed in a late autophagosome, where the internalized materials are degraded. In the present study, autophagosomal fusion with the chlamydial inclusion is excluded, since the autophagosomal specific marker MDC was not delivered into the inclusion and MAP-LC3 and calreticulin staining revealed discontinuous distribution pattern around the inclusion. Schaible et al. (56) found that dextrans introduced into the host cell cytosol can be transferred into the parasitophorous vacuole of Leishmania mexicana and this process was sensitive to autophagic modulators (adenine, 3-MA, and Asn), suggesting that parasitophorous vacuoles gain access to nutrients by autophagosomes. The transfer of dextrans from the cytoplasm into the Leishmania vacuole via autophagosomes is consistent with previous studies on the sequestration of endogenous or introduced cytoplasmic constituents into autophagosomal vacuoles (11, 28, 30, 50, 59). Heinzen and Hackstadt (26), who directly introduced dextrans into the cytoplasm of C. trachomatis-infected cells by microinjection or transfection, found the inclusion membrane passively impermeable to these molecules. If we assume that introduced dextrans will be partially sequestered into autophagosomes, we can also conclude that autophagosomes do not fuse with chlamydial inclusions, corroborating our findings obtained in the present study.
Although fusion of autophagosomes with the chlamydial inclusion is unlikely to occur, our findings suggest the existence of a potential link to autophagy. C. trachomatis was extremely sensitive to classic autophagic regulators, such as amino acids and 3-MA. Individually added chemicals markedly affected at least one of the following: the inclusion size, morphology of chlamydial forms, and development of infectious progeny. Generally, as determined by microscopy techniques and infectivity assays, various degrees of chlamydial growth abnormality were produced by additives used. Differences in susceptibility of chlamydiae to these chemicals may be correlated, at least in part, with different efficiencies of these chemicals to suppress autophagy (8, 22, 41, 57, 58). Another evidence for the presence of a potential involvement of autophagy with Chlamydia is obtained from the close association of the autophagosomal proteins MAP-LC3 and calreticulin, which accumulate around the inclusion by a process seems to be sensitive to amino acids and 3-MA.
Of the amino acids tested here, only four—Leu, Ile, Met, and Phe—notably arrested inclusion maturation. Moreover, these chemicals led to a very strong or a complete suppression of the production of infectious chlamydiae, depending on the time at which the amino acid was added. Complete infectivity inhibition by Met, Ile, and Leu is apparently attributed to the presence of inclusions containing RBs that failed to multiply and transform back into EBs (Fig. 4). This transformation seems likely not to take place over time, since no infectious EBs were recovered from infected cell monolayers incubated with chemicals for up to 5 days (Table 1). Interestingly, bacteria developed in amino acid-exposed host cells could restore their growth simply by withdrawal of excess amino acids. This infectivity recovery was markedly effective, when additives were removed 1 or 2 days after treatment compared to the negligible infectivity obtained from cultures treated for periods as long as 5 days (Table 1). We are currently performing experiments to determine the long-term effects of amino acid treatment on Chlamydia infection in vitro.
Earlier in vitro studies conducted in the past two decades have demonstrated that the developmental cycle of C. psittaci, C. trachomatis, and C. pneumoniae is adversely affected by omission of all or single amino acids from the cell cultures (1, 2, 13, 14, 35) or by small changes in external amino acid concentrations (23). Paradoxically, the present study showed that excess amino acid supply led to more dramatic changes in the development of C. trachomatis, particularly when Leu, Ile, Met, or Phe were introduced. The markedly aberrant growth observed in our study using high amounts of amino acids and in the studies of other groups using restricted amounts of amino acids suggests that concentrations of amino acids available for bacteria should be tightly regulated to provide a favorable environment for a chlamydial productive infection and that any disturbance in the levels of extracellular or intracellular amino acids could adversely affect chlamydial development. In this context, since in vitro experiments with chlamydiae rely exclusively on cell culturing systems with commercial cell growth media that differ in amino acid composition and concentrations, the nutritional requirements for Chlamydia in these media, especially for amino acids, should be revised and defined.
In summary, our data suggest a potential involvement of autophagy in the growth of Chlamydia based on (i) the extreme sensitivity of bacteria to 3-MA and amino acids, traditionally known to modulate autophagy, and (ii) the considerable accumulation of autophagosome-linked proteins (MAP-LC3 and ER markers) around the inclusion, a phenomenon that can notably be disrupted by chemicals used. Host cells regulate synthetic precursor pools in their cytoplasm, in part, by degradation of endogenous materials via autophagy. Since chlamydiae are obligate intracellular pathogens that rely on their host for synthetic precursors and metabolites, this degradation pathway could be a source of these building blocks needed by developing bacteria, especially when the amounts of exogenous precursors are limited (insufficient). Therefore, it is plausible to hypothesize that manipulation of autophagy as a major source of endogenous metabolites, available in some way for chlamydiae, by using 3-MA and amino acids may adversely affect the development of bacteria in host cells. To support this hypothesis, further studies are required to elucidate the potential of these chemicals to modulate autophagy in the cell system used here. In addition to their anticatabolic activities, other mechanisms by which 3-MA and amino acids could modulate chlamydial infections are not excluded. These agents can possibly gain access to the inclusion lumen and directly affect chlamydiae. Moreover, amino acids act as metabolic signals involved in many host transduction pathways, and recent in vivo and in vitro work has revealed a number of components of the translational machinery that can be regulated by amino acids (5, 32, 33). On the other hand, 3-MA has been reported to inhibit autophagy by its capacity to specifically inhibit phosphatidylinositol 3-kinase (10), a key enzyme that regulates numerous cellular processes, including cell growth, proliferation, survival, cytoskeletal remodeling, and the trafficking of intracellular organelles (20, 63, 64). Taken together, it is possible that 3-MA and amino acids could inhibit chlamydial growth by activating other molecular mechanisms that modulate, together with autophagy inhibition, chlamydial pathogenesis.
Acknowledgments
We thank Marco Kachler and Beatrix Fauler for excellent technical support. We also thank the other members of our Chlamydia group, namely, Agnes Szczepek, Wolfgang Wehrl, André Mäurer, Dagmar Heuer, Nicole Paland, Marion Rother, Joscha Gussmann, and Peter Braun, for valuable discussions.
Editor: J. N. Weiser
REFERENCES
- 1.Allan, I., and J. H. Pearce. 1983. Differential amino acid utilization by Chlamydia psittaci (strain guinea pig inclusion conjunctivitis) and its regulatory effect on chlamydial growth. J. Gen. Microbiol. 129:1991-2000. [DOI] [PubMed] [Google Scholar]
- 2.Allan, I., T. P. Hatch, and J. H. Pearce. 1985. Influence of cysteine deprivation on chlamydial differentiation from reproductive to infective life-cycle forms. J. Gen. Microbiol. 131:3171-3177. [DOI] [PubMed] [Google Scholar]
- 3.Al-Younes, H. M., T. Rudel, and T. F. Meyer. 1999. Characterization and intracellular trafficking pattern of vacuoles containing Chlamydia pneumoniae in human epithelial cells. Cell. Microbiol. 1:237-247. [DOI] [PubMed] [Google Scholar]
- 4.Al-Younes, H. M., T. Rudel, V. Brinkmann, A. J. Szczepek, and T. F. Meyer. 2001. Low iron availability modulates the course of Chlamydia pneumoniae infection. Cell. Microbiol. 3:427-437. [DOI] [PubMed] [Google Scholar]
- 5.Avruch, J., C. Belham, Q. Wenig, K. Hara, and K. Yonezawa. 2001. The p70 S6 kinase integrates nutrient and growth signals to control translational capacity. Prog. Mol. Subcell. Biol. 26:115-154. [DOI] [PubMed] [Google Scholar]
- 6.Beron, W., M. G. Gutierrez, M. Rabinovitch, and M. I. Colombo. 2002. Coxiella burnetii localizes in a Rab7-labeled compartment with autophagic characteristics. Infect. Immun. 70:5816-5821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Biederbick, A., H. F. Kern, and H. P. Elsasser. 1995. Monodansylcadaverine (MDC) is a specific in vivo marker for autophagic vacuoles. Eur. J. Cell Biol. 66:3-14. [PubMed] [Google Scholar]
- 8.Blommaart, E. F., J. J. Luiken, and A. J. Meijer. 1997. Autophagic proteolysis: control and specificity. Histochem. J. 29:365-385. [DOI] [PubMed] [Google Scholar]
- 9.Blommaart, E. F., J. J. Luiken, P. J. Blommaart, G. M. van Woerkom, and A. J. Meijer. 1995. Phosphorylation of ribosomal protein S6 is inhibitory for autophagy in isolated rat hepatocytes. J. Biol. Chem. 270:2320-2326. [DOI] [PubMed] [Google Scholar]
- 10.Blommaart, E. F., U. Krause, J. P. Schellens, H. Vreeling-Sindelarova, and A. J. Meijer. 1997. The phosphatidylinositol 3-kinase inhibitors wortmannin and LY294002 inhibit autophagy in isolated rat hepatocytes. Eur. J. Biochem. 243:240-246. [DOI] [PubMed] [Google Scholar]
- 11.Bridges, K. R. 1987. Ascorbic acid inhibits lysosomal autophagy of ferritin. J. Biol. Chem. 262:14773-14778. [PubMed] [Google Scholar]
- 12.Carabeo, R. A., D. J. Mead, and T. Hackstadt. 2003. Golgi-dependent transport of cholesterol to the Chlamydia trachomatis inclusion. Proc. Natl. Acad. Sci. USA 100:6771-6776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coles, A. M., and J. H. Pearce. 1987. Regulation of Chlamydia psittaci (strain guinea pig inclusion conjunctivitis) growth in McCoy cells by amino acid antagonism. J. Gen. Microbiol. 133:701-708. [DOI] [PubMed] [Google Scholar]
- 14.Coles, A. M., D. J. Reynolds, A. Harper, A. Devitt, and J. H. Pearce. 1993. Low-nutrient induction of abnormal chlamydial development: a novel component of chlamydial pathogenesis? FEMS Microbiol. Lett. 106:193-200. [DOI] [PubMed] [Google Scholar]
- 15.Dorn, B. R., W. A. Dunn, Jr., and A. Progulske-Fox. 2002. Bacterial interactions with the autophagic pathway. Cell. Microbiol. 4:1-10. [DOI] [PubMed] [Google Scholar]
- 16.Dunn, W. A., Jr. 1990. Studies on the mechanisms of autophagy: formation of the autophagic vacuole. J. Cell Biol. 110:1923-1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dunn, W. A., Jr. 1990. Studies on the mechanisms of autophagy: maturation of the autophagic vacuole. J. Cell Biol. 110:1935-1945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dunn, W. A., Jr. 1994. Autophagy and related mechanisms of lysosome-mediated protein degradation. Trends Cell Biol. 4:139-143. [DOI] [PubMed] [Google Scholar]
- 19.Fengsrud, M., N. Roos, T. Berg, W. Liou, J. W. Slot, and P. O. Seglen. 1995. Ultrastructural and immunocytochemical characterization of autophagic vacuoles in isolated hepatocytes: effects of vinblastine and asparagine on vacuole distributions. Exp. Cell Res. 221:504-519. [DOI] [PubMed] [Google Scholar]
- 20.Fruman, D. A., R. E. Meyers, and L. C. Cantley. 1998. Phosphoinositide kinases. Annu. Rev. Biochem. 67:481-507. [DOI] [PubMed] [Google Scholar]
- 21.Grieshaber, S., J. A. Swanson, and T. Hackstadt. 2002. Determination of the physical environment within the Chlamydia trachomatis inclusion using ion-selective ratiometric probes. Cell. Microbiol. 4:273-283. [DOI] [PubMed] [Google Scholar]
- 22.Grinde, B., and P. O. Seglen. 1981. Effects of amino acid analogues on protein degradation in isolated rat hepatocytes. Biochim. Biophys. Acta 676:43-50. [DOI] [PubMed] [Google Scholar]
- 23.Harper, A., C. I. Pogson, M. L. Jones, and J. H. Pearce. 2000. Chlamydial development is adversely affected by minor changes in amino acid supply, blood plasma amino acid levels, and glucose deprivation. Infect. Immun. 68:1457-1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hatch, T. P. 1975. Competition between Chlamydia psittaci and L cells for host isoleucine pools: a limiting factor in chlamydial multiplication. Infect. Immun. 12:211-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hatch, T. P. 1975. Utilization of L-cell nucleoside triphosphates by Chlamydia psittaci for ribonucleic acid synthesis. J. Bacteriol. 122:393-400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Heinzen, R. A., and T. Hackstadt. 1997. The Chlamydia trachomatis parasitophorous vacuolar membrane is not passively permeable to low-molecular-weight compounds. Infect. Immun. 65:1088-1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Heinzen, R. A., M. A. Scidmore, D. D. Rockey, and T. Hackstadt. 1996. Differential interaction with endocytic and exocytic pathways distinguish parasitophorous vacuoles of Coxiella burnetii and Chlamydia trachomatis. Infect. Immun. 64:796-809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hernandez-Yago, J., E. Knecht, A. Martinez-Ramon, and S. Grisolia. 1980. Autophagy of ferritin incorporated into the cytosol of HeLa cells by liposomes. Cell Tissue Res. 205:303-309. [DOI] [PubMed] [Google Scholar]
- 29.Hoyvik, H., P. B. Gordon, T. O. Berg, P. E. Stromhaug, and P. O. Seglen. 1991. Inhibition of autophagic-lysosomal delivery and autophagic lactolysis by asparagine. J. Cell Biol. 113:1305-1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hultcrantz, R., and H. Glaumann. 1987. Intracellular fate of ferritin in HeLa cells following microinjection. Exp. Cell Res. 171:203-212. [DOI] [PubMed] [Google Scholar]
- 31.Kalman, S., W. Mitchell, R. Marathe, C. Lammel, J. Fan, R. W. Hyman, L. Olinger, J. Grimwood, R. W. Davis, and R. S. Stephens. 1999. Comparative genomes of Chlamydia pneumoniae and C. trachomatis. Nat. Genet. 21:385-389. [DOI] [PubMed] [Google Scholar]
- 32.Kimball, S. R., and L. S. Jefferson. 2002. Control of protein synthesis by amino acid availability. Curr. Opin. Clin. Nutr. Metab. Care 5:63-67. [DOI] [PubMed] [Google Scholar]
- 33.Kimball, S. R. 2002. Regulation of global and specific mRNA translation by amino acids. J. Nutr. 132:883-886. [DOI] [PubMed] [Google Scholar]
- 34.Klionsky, D. J., and S. D. Emr. 2000. Autophagy as a regulated pathway of cellular degradation. Science 290:1717-1721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kuo, C. C., and J. T. Grayston. 1990. Amino acid requirements for growth of Chlamydia pneumoniae in cell cultures: growth enhancement by lysine or methionine depletion. J. Clin. Microbiol. 28:1098-1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Majeed, M., K. H. Krause, R. A. Clark, E. Kihlstrom, and O. Stendahl. 1999. Localization of intracellular Ca2+ stores in HeLa cells during infection with Chlamydia trachomatis. J. Cell Sci. 112:35-44. [DOI] [PubMed] [Google Scholar]
- 37.May, M. E., and M. G. Buse. 1989. Effects of branched-chain amino acids on protein turnover. Diabetes Metab. Rev. 5:227-245. [DOI] [PubMed] [Google Scholar]
- 38.McClarty, G. 1994. Chlamydiae and the biochemistry of intracellular parasitism. Trends Microbiol. 2:157-164. [DOI] [PubMed] [Google Scholar]
- 39.Meijer, A. J., L. A. Gustafson, J. J. Luiken, P. J. Blommaart, L. H. Caro, G. M. van Woerkom, C. Spronk, and L. Boon. 1993. Cell swelling and the sensitivity of autophagic proteolysis to inhibition by amino acids in isolated rat hepatocytes. Eur. J. Biochem. 215:449-454. [DOI] [PubMed] [Google Scholar]
- 40.Morgan, H. R. 1956. Latent viral infection of cells in tissue culture. I. Studies on latent infection of chick embryo tissues with psittacosis virus. J. Exp. Med. 103:34-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mortimore, G. E., B. R. Lardeux, and S. J. Heydrick. 1989. Mechanism and control of protein and RNA degradation in the rat hepatocyte: two modes of autophagic sequestration. Revis. Biol. Celular. 20:79-96. [PubMed] [Google Scholar]
- 42.Moulder, J. W. 1991. Interaction of chlamydiae and host cells in vitro. Microbiol. Rev. 55:143-190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Moulder, J. W. 1974. Intracellular parasitism: life in an extreme environment. J. Infect. Dis. 130:300-306. [DOI] [PubMed] [Google Scholar]
- 44.Nicholson, T. L., L. Olinger, K. Chong, G. Schoolnik, and R. S. Stephens. 2003. Global stage-specific gene regulation during the developmental cycle of Chlamydia trachomatis. J. Bacteriol. 185:3179-3189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pillay, C. S., E. Elliott, and C. Dennison. 2002. Endolysosomal proteolysis and its regulation. Biochem. J. 363:417-429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pizarro-Cerdá, J., S. Meresse, R. G. Parton, G. van der Goot, A. Sola-Landa, I. Lopez-Goni, E. Moreno, and J. P. Gorvel. 1998. Brucella abortus transits through the autophagic pathway and replicates in the endoplasmic reticulum of nonprofessional phagocytes. Infect. Immun. 66:5711-5724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Punnonen, E. L., and H. Reunanen. 1990. Effects of vinblastine, leucine, and histidine, and 3-methyladenine on autophagy in Ehrlich ascites cells. Exp. Mol. Pathol. 52:87-97. [DOI] [PubMed] [Google Scholar]
- 48.Punnonen, E. L., S. Autio, V. S. Marjomaki, and H. Reunanen. 1992. Autophagy, cathepsin L transport, and acidification in cultured rat fibroblasts. J. Histochem. Cytochem. 40:1579-1587. [DOI] [PubMed] [Google Scholar]
- 49.Punnonen, E. L., V. S. Marjomaki, and H. Reunanen. 1994. 3-Methyladenine inhibits transport from late endosomes to lysosomes in cultured rat and mouse fibroblasts. Eur. J. Cell Biol. 65:14-25. [PubMed] [Google Scholar]
- 50.Rabouille, C., G. J. Strous, J. D. Crapo, H. J. Geuze, and J. W. Slot. 1993. The differential degradation of two cytosolic proteins as a tool to monitor autophagy in hepatocytes by immunocytochemistry. J. Cell Biol. 120:897-908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Raulston, J. E. 1995. Chlamydial envelope components and pathogen-host cell interactions. Mol. Microbiol. 15:607-616. [DOI] [PubMed] [Google Scholar]
- 52.Raulston, J. E. 1997. Response of Chlamydia trachomatis serovar E to iron restriction in vitro and evidence for iron-regulated chlamydial proteins. Infect. Immun. 65:4539-4547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Reggiori, F., and D. J. Klionsky. 2002. Autophagy in the eukaryotic cell. Eukaryot. Cell 1:11-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schachter, J., and H. D. Caldwell. 1980. Chlamydiae. Annu. Rev. Microbiol. 34:285-309. [DOI] [PubMed] [Google Scholar]
- 55.Schachter, J. 1999. Infection and disease epidemiology, p. 139-169. In R. S. Stephens (ed.), Chlamydia: intracellular biology, pathogenesis, and immunity. American Society for Microbiology, Washington, D.C.
- 56.Schaible, U. E., P. H. Schlesinger, T. H. Steinberg, W. F. Mangel, T. Kobayashi, and D. G. Russell. 1999. Parasitophorous vacuoles of Leishmania mexicana acquire macromolecules from the host cell cytosol via two independent routes. J. Cell Sci. 112:681-693. [DOI] [PubMed] [Google Scholar]
- 57.Seglen, P. O., and P. Bohley. 1992. Autophagy and other vacuolar protein degradation mechanisms. Experientia 48:158-172. [DOI] [PubMed] [Google Scholar]
- 58.Seglen, P. O., P. B. Gordon, and A. Poli. 1980. Amino acid inhibition of the autophagic/lysosomal pathway of protein degradation in isolated rat hepatocytes. Biochim. Biophys. Acta 630:103-118. [DOI] [PubMed] [Google Scholar]
- 59.Stacey, D. W., and V. G. Allfrey. 1977. Evidence for the autophagy of microinjected proteins in HeLa cells. J. Cell Biol. 75:807-817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Stromhaug, P. E., and D. J. Klionsky. 2001. Approaching the molecular mechanism of autophagy. Traffic 2:524-531. [DOI] [PubMed] [Google Scholar]
- 61.Tipples, G., and G. McClarty. 1993. The obligate intracellular bacterium Chlamydia trachomatis is auxotrophic for three of the four ribonucleoside triphosphates. Mol. Microbiol. 8:1105-1114. [DOI] [PubMed] [Google Scholar]
- 62.van Ooij, C., G. Apodaca, and J. Engel. 1997. Characterization of the Chlamydia trachomatis vacuole and its interaction with the host endocytic pathway in HeLa cells. Infect. Immun. 65:758-766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wymann, M. P., and L. Pirola. 1998. Structure and function of phosphoinositide 3-kinases. Biochim. Biophys. Acta 1436:127-150. [DOI] [PubMed] [Google Scholar]
- 64.Wymann, M. P., M. Zvelebil, and M. Laffargue. 2003. Phosphoinositide 3-kinase signalling: which way to target? Trends Pharmacol. Sci. 24:366-376. [DOI] [PubMed] [Google Scholar]
- 65.Yoshimori, T. 2004. Autophagy: a regulated bulk degradation process inside cells. Biochem. Biophys. Res. Commun. 313:435-458. [DOI] [PubMed] [Google Scholar]