Abstract
Waterpipe (hookah, narghile) tobacco smoking (WTS) is becoming prevalent worldwide and is one of the most popular forms of tobacco use among youth. WTS prevalence has increased dramatically among youth in the United States within the past decade. Misperceived as less harmful than cigarette smoking, WTS is associated with many of the same chronic health effects such as lung cancer, chronic obstructive pulmonary disease, cardiovascular disease, bronchitis, and asthma. Much of this risk is due to the fact that a single WTS session exposes users to large volumes of smoke that contain toxic chemicals such as carbon monoxide, cancer-causing polycyclic aromatic hydrocarbons, and volatile aldehydes. Unlike cigarette smoking, WTS poses unique risks of acute negative health outcomes including carbon monoxide poisoning and the spread of communicable diseases such as herpes and tuberculosis. Because waterpipe tobacco smoke contains the addictive chemical nicotine, youth who smoke tobacco from a waterpipe may be at risk for dependence. As a result, many youth may initiate WTS and continue to use despite negative health effects. Considering many of the potential negative health effects associated with WTS affect the pulmonary system, pulmonologists and primary care providers may treat patients who are waterpipe tobacco smokers and should be aware of the risk associated with WTS. The purpose of this review is to describe a waterpipe, the prevalence and correlates of WTS, the toxicants found in waterpipe tobacco smoke, the health effects of WTS, and implications for pulmonologists and other clinicians.
Keywords: Waterpipe tobacco smoking, youth, prevalence and correlates, smoke toxicants, health effects
Introduction
Nearly all health practitioners in the United States are aware of the dangers associated with tobacco use, with almost half a million deaths each year in the U.S. attributed to cigarette smoking [1]. Most of these deaths are caused by diseases of the lung or cardiovascular system [1]. However, many clinicians may be unaware of a growing tobacco use trend that poses similar risks: tobacco smoking using a waterpipe (also known as hookah, narghile, or shisha). Waterpipe tobacco smoking (WTS) is increasing in prevalence, especially among adolescents and young adults. Health practitioners should be aware of the potential dangers associated with WTS so that they can help to prevent morbidity and mortality associated with it, just as they do with cigarette smoking. The purpose of this review is to provide a basic overview of WTS, describe current youth trends and why youth are attracted to WTS, describe the toxicants found in waterpipe tobacco smoke, and discuss the acute and chronic health effects associated with WTS, including implications for pulmonologists.
Waterpipe Tobacco Smoking Overview
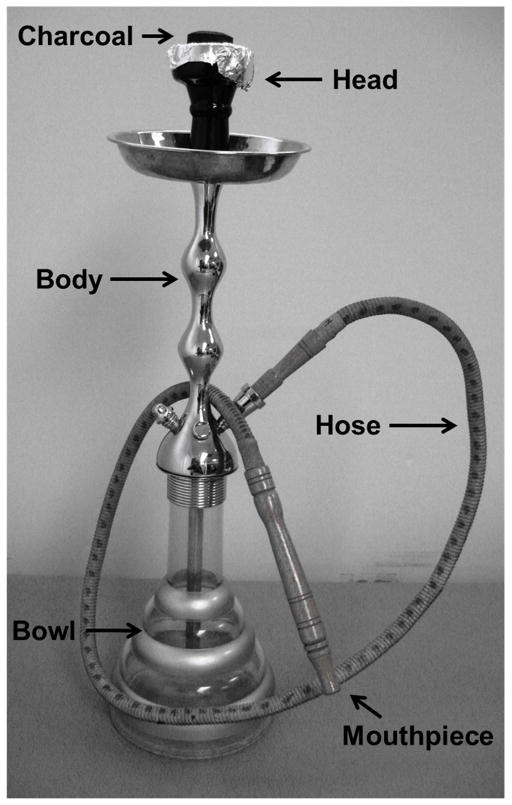
A waterpipe has four main components: the head, body, bowl, and hose/mouthpiece assembly (Figure 1). A waterpipe is prepared for tobacco smoking by filling the head with 10–20g of a moist, sweetened, and flavored tobacco mixture (called ma’assel or shisha). Virtually any flavor is available, and fruit (e.g., apple, peach, strawberry, watermelon), drink (e.g., margarita, piña colada), or candy flavors (e.g., chocolate, vanilla, white gummi bear) are common. The tobacco-filled head is covered with perforated aluminum foil onto which a lit piece of charcoal is placed. Charcoal is used in WTS because the moistness of the tobacco mixture in the head does not allow for self-sustained combustion. Rather, when the waterpipe smoker inhales on the hose/mouthpiece assembly, charcoal-heated air is drawn across the tobacco, thus producing the mainstream aerosol. This aerosol then passes through the body of the pipe, bubbles through the water in the bowl, travels the length of the hose, and the user inhales the resulting smoke.
Figure 1.
Waterpipe tobacco smoking assembly.
Prevalence of WTS
While tobacco smoking using a waterpipe commonly is associated with the Eastern Mediterranean Region (EMR), it is now a common practice globally, though few countries regularly conduct surveillance on WTS [2]. As a result, determining up-to-date WTS prevalence rates in many countries can be challenging. With respect to the EMR, current adult WTS rates of 15% have been reported in Lebanon [3], 8.6% in Jordan [4], 44.6% exclusive WTS (no other tobacco product used) in Kuwait [5], and 3.3–6% in Egypt [6,7]. Adolescent WTS is also common in the EMR. A study examining data on WTS among 13–15 year old adolescents from the Global Tobacco Survey reported current other tobacco use (primarily WTS in the EMR region) rates of 15% in Bahrain, 16% in Kuwait, 9% in Oman, 14% in Qatar, 15% in the United Arab Emirates, and 15% in Yemen [8]. Current WTS rates among university students in the EMR include 28% in Lebanon [9], 8–14.6% in Saudi Arabia [10–11], 6% in the United Arab Emirates [12], and 33% in Pakistan [13]. With respect to the rest of the world, ever WTS rates include 7.8% in Scotland and 12.0% in England [14], and current WTS has been reported among 8% college students in the United Kingdom [15], 10% among adolescents in Germany [16], 6.4% of adults aged 15 and older in Vietnam [17], and 30% of university students in Malaysia [18]. This global trend of increasing popularity of WTS has also made its way to North America.
Though WTS in the United States is a relatively recent trend, it has increased in popularity rapidly, particularly among adolescents and young adults. Young adults in the U.S. report current (past 30 day) WTS rates ranging from 7.2% to 20.3% [19–25], past-year WTS rates of 12.1% to 43.4% [19,20,23,26,27] and lifetime use rates ranging from 10% to 48.4% [19,20,23,25,26]. In one study [19], more participants reported past year WTS than past year cigarette smoking (46.4% vs. 42.1%) and in another study [23], lifetime WTS smoking was more common than lifetime cigarette smoking (41.0% vs. 39.6%).
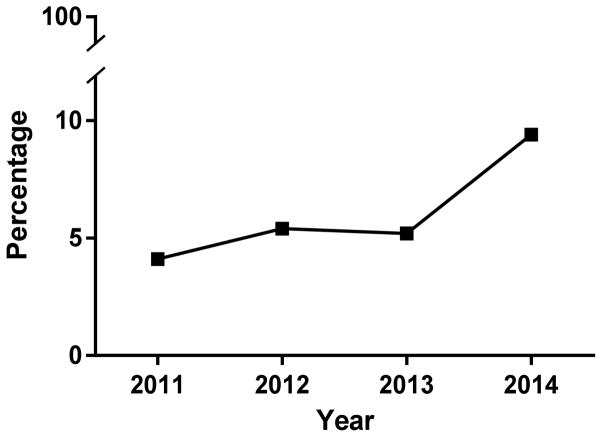
WTS smoking is not only becoming increasingly common among college students and young adults, but younger populations as well. Despite being illegal for individuals under the age of 18 in the U.S., many studies report WTS among middle and high school students with rates increasing over time. For instance, two studies [28,29] examining lifetime WTS among high school students in Florida reported that in 2007 11% of high school students had tried WTS [28]. In 2012, this number had increased to 16.7%[29]. Studies from other states and nationally representative samples report consistent findings. A survey of New Jersey high school students in 2008 found that 9.7% of high school students were current waterpipe tobacco smokers [30]. A study of 5,540 high school seniors from across the United States found that 18% of the sample reported WTS in the past year [31]. Additionally, while some of these numbers may represent experimentation or infrequent WTS, some adolescents progress to continued use. A study examining WTS using 2011 data from the National Youth Tobacco Survey reported adolescent ever WTS at 7.3% and current WTS at 2.6% [32]. Using data from the same survey one year later, 1.3% of middle school students and 5.4% of high school students reported current WTS [33] which represented significant increases from WTS current use rates in 2011. These rates continued to increase and in 2014, current WTS was reported by 2.5% of middle school students and 9.4% of high school students [34] (See Figure 3). In fact, in 2014 the only tobacco product more popular among adolescents than WTS was electronic cigarettes [34]. The current evidence from the U.S. and elsewhere around the world indicates that WTS is more than a passing fad and that many youth are at risk for WTS.
Figure 3.
Volume of smoke generated in a single waterpipe tobacco smoking session compared to a single cigarette.
Youth Appeal and Correlates of WTS
Understanding the correlates of WTS may help us learn about what youth subgroups are most likely to engage in it. One of the most commonly reported and most problematic correlates of youth WTS is the perception that WTS is associated with less harm potential, especially when compared to combustible cigarette smoking [20,23,25,35–40]. Many young adults perceive that WTS is associated with less nicotine, tar, and carcinogen exposure, less harmful secondhand smoke, a lower likelihood of causing addiction, and a lower likelihood of causing both short term and long term harm including cancer [41]. Some of these perceptions could be a result of the numerous social media outlets that often portray WTS in a positive light [42] or misleading packaging that may cause waterpipe tobacco smokers to believe waterpipe tobacco smoke to be less harmful than cigarette smoke [43]. WTS is also perceived by youth as a more attractive and acceptable behavior compared to other forms of tobacco use [44]. There are many aspects of WTS that may be attractive to youth, especially the highly social dynamic associated with WTS. A qualitative study of 49 young adults reported that social acceptance, peer influence, socializing with friends, and looking “cool” were main reasons for WTS [45]. These results are supported by a larger survey of 438 young adults [46]. Of those respondents who reported hookah use, 29% reported socializing/partying and 27% reported peer influence as motivating factors for WTS [46]. Additionally, many youth may be attracted to attending the waterpipe cafes that have increased in number dramatically [47]. These cafes may be appealing to youth and young adults because they provide an attractive social atmosphere [48] especially for those wanting to attend bars or nightclubs but are not of legal drinking age [49,50] but are still old enough to gain access (legally or illegally) to venues where WTS occurs and alcohol is not served.
With some variations depending on sample characteristics, common demographic and behavioral correlates of WTS include: sex (males) [15,22,25,28,31,36,51–56], younger age (i.e., young adults) [25,28,52,53], Arab ethnicity [15,30,36], non-Hispanic white race [22,31,53,56], higher household income [31,52,57], tobacco use including cigarettes and cigar use [15,21,22,25,28,30,31,36,41,46,52–56], substance use including alcohol use and marijuana use [21,25,31,41,46,52–56], binge drinking [46,52,55], and sensation seeking personality characteristics [55]. There are several important points to understand regarding common correlates. First, the extent to which these common WTS correlates can be applied to different populations may differ substantially depending on cultural norms. For example, while WTS may be more common among those who report alcohol use and binge drinking in the U.S., in countries and cultures where alcohol use is not as common (e.g., EMR countries), alcohol use is not a strong correlate. Second, while many studies have identified behavioral correlates of WTS, few longitudinal studies have examined behavioral predictors of WTS. That is, much of the current body of evidence does not allow causal inferences to be made regarding WTS initiation. Third, while Arab ethnicity has been identified as a correlate of WTS, the majority of young waterpipe tobacco smokers in the U.S. are of non-Arab ethnicity. However, the current evidence does indicate that many adolescents and young adults globally are at risk for WTS (for a more detailed discussion of the epidemiology of WTS, see [58]).
Toxicants in Waterpipe Tobacco Smoke
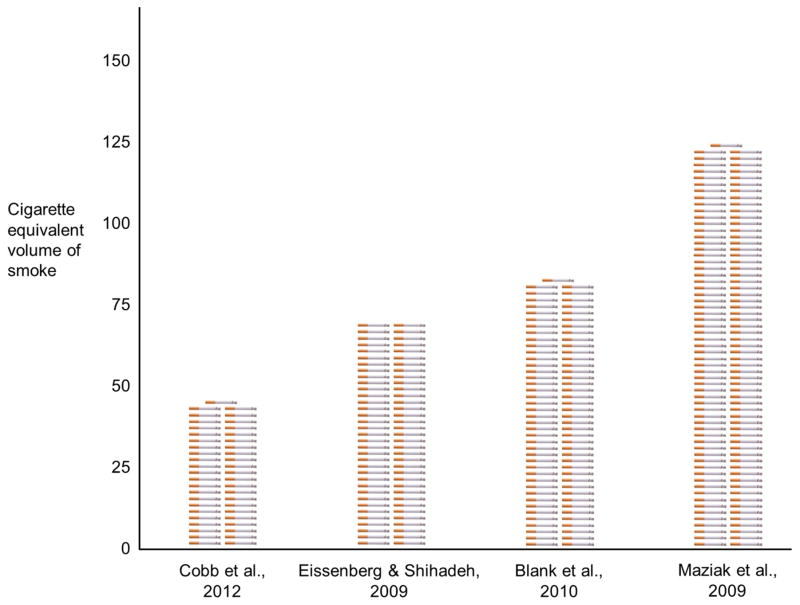
One especially problematic quality of WTS is the large volume of toxicant-laden smoke inhaled during a WTS session. The large volume is a product of long session durations and the large number of high volume puffs taken during each session. With regard to session length, a typical WTS session may last 45 minutes or more [59], much longer than the approximately 5 minutes taken to consume a tobacco cigarette. During this time, waterpipe users will take as many as 78–269 puffs [61,62], as compared to approximately 10 from a tobacco cigarette that is usually smoked in about 5 minutes (e.g., [63]. Moreover, each puff from a waterpipe involves inhalation of approximately 768–899 ml of smoke, compared to approximately 50 ml for a tobacco cigarette [61,64]. As a result of each of these factors (time, puff number, puff volume), waterpipe smokers may inhale 31 to 86 liters of smoke in a typical WTS session [62,64,65,66], and potentially more for extended WTS sessions. Given that cigarette smokers typically inhale on average 0.5 to 0.8 liters of smoke per cigarette [67–69], waterpipe tobacco smokers may inhale anywhere between 39 and 172 times the volume of smoke in a single WTS session compared to smoking a single cigarette (Figure 3).
There is much evidence demonstrating that waterpipe tobacco smoke contains many of the same lethal smoke toxicants as cigarette smoke that are known to cause disability, disease, and death. These toxicants include carbon monoxide (CO; [64,70,71]), polycyclic aromatic hydrocarbons (PAHs) [70,72–74], volatile aldehydes [75–77], and nicotine [64,71]. Exposure to these toxicants is associated with a variety of adverse health consequences including cardiovascular disease, cancer, and pulmonary disease, and nicotine/tobacco dependence.
Many of the toxicants found in waterpipe tobacco smoke generated from a single session are found in significantly higher concentrations than in smoke generated from a single cigarette. For example, in one laboratory study examining PAHs in waterpipe tobacco smoke generated using a smoking protocol modeled after smokers observed in waterpipe cafés, a single WTS session produced an average of 2.5 times more phenanthrene, 8.2 times more fluoranthene, and 5.0 times more chrysene compared to the amount of toxins found in the smoke from a single cigarette [71]. Using similar methods, another study found that a single WTS session produced 16.6 times higher formaldehyde in the mainstream smoke than what is produced from smoking a single tobacco cigarette [75]. In no case is the amount of any toxicant contained in the smoke from a single WTS session ever less than the amount of that toxicant contained in the smoke from a single cigarette.
There is ample evidence that these toxicants reach the waterpipe tobacco smokers’ lungs and blood. In one study, carboxyhemoglobin levels among participants who engaged in a WTS session increased from 0.8% to 4.5% compared to 0.8% to 1.1% after smoking a single cigarette [61]. Field studies have also reported increased expired air CO after WTS. These studies report mean expired air CO concentration of patrons exiting waterpipe cafes of 34.7–58.2 ppm [15,78,79]. Metabolites of carcinogenic tobacco specific nitrosamines (TSNAs) such as NNAL have also been found in waterpipe tobacco smokers. Non-smokers have lower NNAL concentrations (0.7 pg/mL) than exclusive waterpipe daily waterpipe smokers (8.4 pg/mL) and exclusive daily cigarette smokers (10.7 pg/mL) [80] (see also [81]). Several studies have shown increases in plasma nicotine concentrations after WTS. These studies report mean increases in plasma nicotine concentration of 3.1–6.8 ng/ml [62,65,66,82]. Finally, CO and nicotine measured in waterpipe tobacco smoke generated from a smoking machine that is programmed to replicate exactly the individual puffing behavior of actual waterpipe smokers is correlated strongly with those smokers’ exposure to CO (r > 0.78) and nicotine (r > 0.76; [83]). This result means that waterpipe tobacco smokers are likely exposed to other toxicants such as aldehydes and PAHs that are measured in waterpipe tobacco smoke but have not yet been measured yet in waterpipe tobacco smokers (for a more detailed discussion of waterpipe smoke toxicant content see [84]).
One final note about toxicants in waterpipe smoke and in waterpipe tobacco smokers is in order. Many waterpipe smokers will point to labeling on waterpipe tobacco that indicates “0% tar”, and “0.05% nicotine” or “0.5% nicotine””. This labeling is misleading. “Tar” is a tobacco smoke constituent, legally defined as “nicotine free, dry particulate matter” [85]. Because “tar” is a smoke constituent, any labeling on a container of non-burning tobacco is technically accurate that there is no “tar” in the tobacco, just as an unlit cigarette also contains no tar. However, once the tobacco is heated to produce smoke, tar is formed and is contained in the smoke. In fact, the smoke from a single waterpipe session produces approximately 802 mg of tar, compared to 11.2 mg from a single cigarette – more than 71 times greater tar produced [71]. While the content of the tar found in waterpipe smoke may differ from that of cigarette smoke, the fact that there is tar in waterpipe smoke is irrefutable. The nicotine labeling is also misleading. In one study, 110 waterpipe tobacco users smoked one of three brands of tobacco from a waterpipe [43]. These tobacco products were contained in packaging that listed nicotine content as 0.5% (brand 1) or 0.05% nicotine (brands 2 and 3). Peak plasma nicotine concentrations associated with these tobacco products were 9.8 ng/ml for Brand 1, 11.4 ng/ml for Brand 2, and 5.8 ng/ml for Brand 3 [43]. In other words, product labeling was not predictive of actual nicotine exposure. Not only does WTS deliver high concentrations of dangerous and dependence causing toxicants to smokers, but waterpipe tobacco packaging may cause smokers to believe they are getting low or even no exposure to these toxicants.
Health Effects of Waterpipe Smoking
A growing body of research identifies the acute and long-term health effects associated with WTS [86,87]. In terms of acute effects, WTS can, in some cases, cause CO intoxication. Numerous cases of CO poisoning have been reported in the literature [88–96]. In one of these reports [88], a 21 year old man presented to the emergency department due to an episode of syncope. The patient reported smoking tobacco from a waterpipe earlier in the day and during the physical examination, the patient had a carboxyhemoglobin (COHb) level of 15.3%. Cigarette smokers who smoke 40 or more cigarettes per day (>2 packs per day) typically have COHb levels of 8%–9% [88]. CO poisoning is a potential risk of WTS because of the high concentrations of CO found in mainstream and sidestream waterpipe tobacco smoke and greater volumes of smoke inhaled per puff and per session (relative to other combustible tobacco products). Symptoms associated with increased CO concentration in the body include dizziness or feeling lightheaded. Some waterpipe tobacco smokers enjoy physiological effects associated with WTS including dizziness, relaxation, or feeling a head rush [45]. One study used a placebo control to disentangle the differences in effects resulting from exposure to nicotine and other smoke toxicant exposure [65]. In this study, occasional waterpipe tobacco smokers engaged in WTS in two double-blind sessions that differed by the product placed in the waterpipe head: the participants’ preferred flavor/brand of waterpipe tobacco or a flavor matched, herbal waterpipe product that contained no tobacco and no nicotine (placebo). Participants in both conditions reported feelings of dizziness. Given that there was no nicotine in one condition, some of the dizziness may be attributable to CO inhalation. Ironically, the dizziness which is likely in part due to exposure to harmful CO may be perceived as a positive physiological effect associated with WTS.
In addition to CO intoxication, WTS has been implicated with the spread of certain communicable diseases including herpes and tuberculosis, likely due to sharing of the same hose/mouthpiece assembly during use [97,98]. WTS has also been shown to cause acute increases in respiratory rate [99–101], decreased forced expiratory flow [99,100], and decreased peak expiratory flow rate [99,102].
In terms of the health effects associated with longer-term use, WTS is associated with many of the same chronic health effects as cigarette smoking. One of the most important is likely nicotine dependence, because dependence helps maintain WTS over the long-term. Like dependent cigarette smokers, at least some long-term waterpipe tobacco smokers report cravings for WTS [6,15,61,103]. Also like cigarette smokers, some frequent waterpipe tobacco smokers report WTS within the first hour after waking, smoking a waterpipe even when feeling ill, and finding abstaining from WTS even for less than a day between sessions difficult [6]. These studies support the notion that WTS supports nicotine/tobacco dependence, and that many waterpipe tobacco smokers may continue WTS despite experiencing adverse health consequences (for a detailed review of this literature, see [104]).
Indeed, a variety of adverse health consequences of WTS have been documented including chronic pulmonary health conditions, though this literature could be more robust [86]. WTS has been linked with lung cancer [105,106,107]. In a study of Lebanese adult hospital patients, being a former waterpipe tobacco smoker was associated with a 6 times greater risk of lung cancer compared to non-former waterpipe tobacco smokers [105]. Chronic obstructive pulmonary disease (COPD) has also been linked with WTS [108–111]. One study of 2201 adults reported that waterpipe tobacco smokers were 2.5 times as likely as non-waterpipe smokers to have COPD [111]. Additionally, WTS is associated generally with “decreased respiratory quality of life” [112]. More dependent waterpipe tobacco smokers may be at increased risk for certain chronic health conditions. A case-control study of 274 individuals with chronic bronchitis and 559 controls reported that compared to individuals who were not dependent on WTS, dependent waterpipe tobacco smokers were 3.7 times more likely to have chronic bronchitis [113]. Youth waterpipe tobacco smokers have been found to be at greater risk for asthma. In a 2012 study of 36,578 Florida high school students, approximately 20% had a lifetime diagnoses of asthma. Though the nature of the study does not allow causal inferences, the participants with a lifetime asthma diagnosis were approximately 1.5 times more likely to report ever WTS [38]. Secondhand waterpipe tobacco smoke may also negatively affect the respiratory system even among non-smokers. More so than second hand cigarette smoke, exposure to second hand WTS has been found to be associated with chronic cough [114].
WTS has also been associated with cardiovascular disease. One study reported that participants with 40 years of WTS experience had a three times greater risk of coronary artery disease compared to non-waterpipe smokers [115]. The increased risk of cardiovascular disease among waterpipe tobacco smokers is likely a product of the increased stress placed on the cardiovascular system due to the large amounts of CO to which waterpipe tobacco smokers are exposed [116]. An important point to note is that establishing a causal link between WTS and chronic health conditions presents many challenges including the inability to differentiate between negative health outcomes caused by WTS alone and those that may be influenced by other factors such as exposure to cigarette smoke or environmental toxicants. Despite this limitation, the literature linking WTS and chronic health conditions continues to grow (for a detailed review of this literature, see [87]).
Implications for Pulmonologists and Primary Care Providers
A growing body of research demonstrates that WTS is a dependence-inducing behavior that is linked with severe acute and long term negative health outcomes. Despite the dangers, WTS has become a highly prevalent behavior, especially among youth and young adults across the globe. As a result, pulmonologists and primary care providers may treat patients presenting with conditions that have resulted from or are exacerbated by WTS. However, standard assessments of tobacco use may not include asking patients about their WTS. Furthermore, when patients are asked if they are “smokers,” some waterpipe tobacco smokers may interpret this question as referring to cigarette smoking only and not WTS and therefore would not reveal their WTS. For this reason, many young waterpipe tobacco smokers who are at risk for significant negative health effects may not receive appropriate counseling and/or treatment. Therefore, when assessing tobacco use behaviors, especially with younger populations, pulmonologists and primary care providers should ask patients about all forms of tobacco use, including WTS, specifically. Similarly, when providing smoking cessation recommendations or instructions to patients to limit or prevent negative health effects associated with smoking, pulmonologists and primary care providers should extend these recommendations and instructions to their patients who engage in WTS.
Because WTS is more prevalent among young adults and adolescents compared to older individuals, pediatricians need to ask specifically about WTS as part of their routine prevention of smoking initiation. While cigarette smoking is currently more prevalent among individuals with lower socioeconomic status [117], evidence suggests that in the U.S., WTS may be more common among non-Hispanic whites from families with higher household income than non-whites individuals with a lower socioeconomic status (with the exception of individuals with Arab ethnicity). This demographic difference between waterpipe tobacco smokers and cigarettes smokers suggests that the group most at risk for WTS is not being counseled adequately.
Achieving cigarette smoking cessation in adolescents is an important preventive care goal for pediatric primary care providers because only a minority quit without intervention, despite the fact that the majority of adolescent smokers want to quit [118]. Waterpipe tobacco smokers may not exhibit similar desire to quit because of the perception that WTS is associated with less harm potential than cigarette smoking. This perception may pose more challenges for the clinician when addressing cessation with waterpipe tobacco smoking patients. The peer influences associated with smoking plus the socializing aspect of hookah bars and cafes, and the more lenient smoking WTS regulations (or lack thereof) in many jurisdictions may support waterpipe smokers to continue smoking.
For adults who have been smoking for years, clinicians have a method to assess the amount of cigarettes smoked in a year by multiplying the number of packs smoked per day with the number of days spent smoking. For lifelong waterpipe smokers there is no such method to quantify their lifetime smoke exposure. The absence of such a method is concerning in light of the higher number of puffs per smoking session, and the larger volumes of smoke inhaled with each puff by waterpipe smokers compared to cigarette smokers. Furthermore the pack-year quantification of cigarette smoking is used to guide the starting dose and duration of nicotine replacement pharmacotherapy for smoking cessation. Recently the U.S. Preventive Services Task Force recommended that individuals aged 55 through 80 years with 30 or more pack-years’ exposure to smoking get annual CT screening for lung cancer [119]. At the present time clinicians are not able to compare WTS to cigarette smoking as it relates to the amount a person smokes over a long period of time. As WTS continues to become more prevalent, such quantification will be important for waterpipe tobacco smokers because their risk of developing lung cancer may be much higher than estimated using a metric developed for cigarette smokers.
Conclusion
Waterpipe tobacco smoking is becoming increasingly popular, particularly among youth and young adults. Evidence suggests that WTS is associated with dependence and acute and long-term negative health outcomes similar to those of cigarette smoking. Pulmonologists and primary care providers should assess for WTS in addition to other forms of tobacco use and explain to patients that there is no indication that WTS is less risky than cigarette smoking. Based on clinical judgment, patients who report any form of tobacco use, including WTS, should be advised that abstaining from all forms of tobacco will limit their risks of negative health outcomes.
Figure 2.
Trends in past 30 day (current) waterpipe tobacco smoking among US high school student from 2011–2014. Data from [33,34].
Footnotes
Compliance with Ethics Guidelines
Human and Animal Rights and Informed Consent
This article contains no studies with human or animal subjects performed by the author.
Conflicts of Interest
Drs Soule, Lipato, Eissenberg work was supported by the National Institute on Drug Abuse of the National Institutes of Health under Award Number P50DA036105 and the Center for Tobacco Products of the U.S. Food and Drug Administration. The content is solely the responsibility of the authors and does not necessarily represent the views of the NIH or the FDA.
Contributor Information
Eric K. Soule, Email: eksoule@vcu.edu, Virginia Commonwealth University, Department of Psychology, Center for the Study of Tobacco Products, PO Box 980205, Richmond, VA 23298, USA, Phone: 804-827-3562
Thokozeni Lipato, Email: tlipato@vcu.edu, Virginia Commonwealth University, School of Medicine, PO Box 980102, Richmond, VA 23298, USA, Phone: 804-628-3626.
Thomas Eissenberg, Email: teissenb@vcu.edu, Virginia Commonwealth University, Department of Psychology, Center for the Study of Tobacco Products, PO Box 980205, Richmond, VA 23298, Phone: 804-827-4617, Fax: 804-828-7862.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of great importance
- 1.U. S. Department of Health and Human Services. The health consequences of smoking – 50 years of progress: a report of the Surgeon General. Atlanta: U. S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Accessed 21 Feb 2015]. [Google Scholar]
- 2.Akl EA, Gunukula SK, Aleem S, Obeid R, Jaoude PA, Honeine R, Irani J. The prevalence of waterpipe tobacco smoking among the general and specific populations: a systematic review. BMC Public Health. 2011;11:244. doi: 10.1186/1471-2458-11-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baddoura R, Wehbeh-Chidiac C. Prevalence of tobacco use among the adult Lebanese population. East Mediterr Health J. 2001;7(4–5):819–28. [PubMed] [Google Scholar]
- 4.Jaghbir M, Shreif S, Ahram M. Pattern of cigarette and waterpipe smoking in the adult population in Jordan. 2014;20(9):529–37. [PubMed] [Google Scholar]
- 5.Mohammed HR, Zhang Y, Newman IM, Shell DF. Waterpipe smoking in Kuwait. East Mediterr Health J. 2010;1(11):1115–20. [PubMed] [Google Scholar]
- 6.Auf RA, Radwan GN, Loffredo CA, El Setouhy M, Israel E, Mohamed MK. Assessment of tobacco dependence in waterpipe smokers in Egypt. Int J Tuberc Lung Dis. 2012;16(1):132–7. doi: 10.5588/ijtld.11.0457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fouad H, Awa FE, Naga RA, Emam AH, Labib S, Palipudi KM, Andes LJ, Asma S, Talley B. Prevalence of tobacco use among adults in Egypt, 2009. Glob Health Promot. 2013 doi: 10.1177/1757975913499801. [epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 8.Moh’d Al-Mulla A, Abdou Helmy S, Al-Lawati J, Al Nasser S, Ali Abdel Rahman S, Almutawa A, Abi Saab B, Al-Bedah AM, Al-Rabeah AM, Ali Bahaj A, El-Awa F, Waren CW, Jones NR, Asma S. Prevalence of tobacco use among students aged 13–15 years in Health Ministers’ Council/Gulf Cooperation Council Member States, 2001–2004. J Sch Health. 2008;78(6):337–43. doi: 10.1111/j.1746-1561.2008.00311.x. [DOI] [PubMed] [Google Scholar]
- 9.Chaaya M, El-Roueiheb Z, Chemaitelly H, Azar G, Nasr J, Al-Sahab B. Argileh smoking among university students: a new tobacco epidemic. Nicotine Tob Res. 2004;6(3):457–63. doi: 10.1080/14622200410001696628. [DOI] [PubMed] [Google Scholar]
- 10.Al-Turki YA. Smoking habits among medical students in Central Saudi Arabia. Saudi Med J. 2006;27(5):700–3. [PubMed] [Google Scholar]
- 11.Al-Mohamed HI, Amin TT. Pattern and prevalence of smoking among students at King Faisal University, Al Hassa, Saudi Arabia. East Mediterr Health J. 2010;16(1):56–64. [PubMed] [Google Scholar]
- 12.Mandil A, Hussein A, Omer H, Turki G, Gaber I. Characteristics and risk factors of tobacco consumption among University of Sharjah students, 2005. East Mediterr Health J. 2007;13(6):1449–58. doi: 10.26719/2007.13.6.1449. [DOI] [PubMed] [Google Scholar]
- 13.Jawaid A, Zafar AM, Rehman TU, Nazir MR, Ghafoor ZA, Afzal O, Khan JA. Knowledge, attitudes and practice of university students regarding waterpipe smoking in Pakistan. Int J Tuberc Lung Dis. 2008;12(9):1077–84. [PubMed] [Google Scholar]
- 14.Grant A, Morrison R, Dockrell MJ. Prevalence of waterpipe (Shisha, Narghille, Hookah) use among adults in Great Britain and factors associated with waterpipe use: data from cross-sectional Online Surveys in 2012 and 2013. Nicotine Tob Res. 2014;16(7):931–8. doi: 10.1093/ntr/ntu015. [DOI] [PubMed] [Google Scholar]
- 15.Jackson D, Aveyard P. Waterpipe smoking in students: prevalence, risk factors, symptoms of addiction, and smoke intake. Evidence from one British university. BMC Public Health. 2008;8:174. doi: 10.1186/1471-2458-8-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Waterpipe (shisha) smoking among adolescents in Germany: Results of the KiGGS study: first follow-up (KiGGS Wave 1) Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2015;58(4–5):467–73. doi: 10.1007/s00103-015-2128-3. [DOI] [PubMed] [Google Scholar]
- 17.Xuan le TT, Van Minh H, Giang KB, Nga PT, Hai PT, Minh NT, Hsia J. Prevalence of waterpipe tobacco smoking among population aged 15 years or older, Vietnam, 2010. Prev Chronic Dis. 2013;10:E57. doi: 10.5888/pcd10.120100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Water pipe (shisha) smoking and associated factors among Malaysian university students. Asian Pac J Cancer Prev. 2011;12(11):3041–7. [PubMed] [Google Scholar]
- 19.Barnett TE, Smith T, He Y, Soule EK, Curbow BA, Tomar SL, McCarty C. Evidence of emerging hookah use among university students: a cross-sectional comparison between hookah and cigarette use. 2013;13:302. doi: 10.1186/1471-2458-13-302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eissenberg T, Ward KD, Smith-Simone S, Maziak W. Waterpipe tobacco smoking on a U.S. College campus: prevalence and correlates. J Adolesc Health. 2008;42(5):526–9. doi: 10.1016/j.jadohealth.2007.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goodwin RD, Grinberg A, Shapiro J, Keith D, McNeil MP, Taha F, Jiang B, Hart CL. Hookah use among college students: prevalence, drug use, and mental health. Drug Alcohol Depend. 2014;141:16–20. doi: 10.1016/j.drugalcdep.2014.04.024. [DOI] [PubMed] [Google Scholar]
- 22.Rahman S, Chang L, Hadgu S, Salinas-Miranda AA, Corvin J. Prevalence, knowledge, and practices of hookah smoking among university students, Florida, 2012. Prev Chronic Dis. 2014;11:E214. doi: 10.5888/pcd11.140099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Primack BA, Sidani J, Agarwal AA, Shadel WG, Donny EC, Eissenberg TE. Prevalence of and associations with waterpipe tobacco smoking among U.S. university students. Ann Behav Med. 2008;36(1):81–6. doi: 10.1007/s12160-008-9047-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Primack BA, Fertman CI, Rice KR, Adachi-Mejia AM, Fine MJ. Waterpipe and cigarette smoking among college athletes in the United States. J Adolesc Health. 2010;46(1):45–51. doi: 10.1016/j.jadohealth.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sutfin EL, McCoy TP, Reboussin BA, Wagoner KG, Spangler J, Wolfson M. Prevalence and correlates of waterpipe tobacco smoking by college students in North Carolina. Drug Alcohol Depend. 2011;115(1–2):131–6. doi: 10.1016/j.drugalcdep.2011.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grekin ER, Ayna D. Argileh use among college students in the United States: an emerging trend. J Stud Alcohol Drugs. 2008;69(3):472–5. doi: 10.15288/jsad.2008.69.472. [DOI] [PubMed] [Google Scholar]
- 27.Jarret T, Blosnich J, Tworek C, Horn K. Hookah use among U.S. college students: results from the National College Health Assessment II. Nicotine Tob Res. 2012;14(10):1145–1153. doi: 10.1093/ntr/nts003. [DOI] [PubMed] [Google Scholar]
- 28.Barnett TE, Curbow BA, Weitz JR, Johnson TM, Smith-Simone SY. Water pipe tobacco smoking among middle and high school students. Am J Public Health. 2009;99(11):2014–9. doi: 10.2105/AJPH.2008.151225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barnett TE, Forrest JR, Porter L, Curbow BA. A multiyear assessment of hookah use prevalence among Floridian high school students. Nicotine Tob Res. 2014;16(3):373–7. doi: 10.1093/ntr/ntt188. [DOI] [PubMed] [Google Scholar]
- 30.Jordan HM, Delnevo CD. Emerging tobacco products: hookah use among New Jersey youth. Prev Med. 2010;51(5):394–6. doi: 10.1016/j.ypmed.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 31.Palamar JJ, Zhou S, Sherman S, Weitzman M. Hookah use among U.S. high school seniors. Pediatrics. 2014;134(2):227–34. doi: 10.1542/peds.2014-0538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Amrock SM, Gordon T, Zelikoff T, Weitzman M. Hookah use among adolescents in the United States: results of a national survey. Nicotine Tob Res. 2014;16(2):231–7. doi: 10.1093/ntr/ntt160. [DOI] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention. Tobacco product use among middle and high school students—United States, 2011 and 2012. MMWR Morb Mortal Wkly Rep. 2013;62(45):893–7. [PMC free article] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention. Tobacco use among middle and high school students – United States, 2011–2014. MMWR Morb Mortal Wkly Rep. 2015;64(14):381–5. [PMC free article] [PubMed] [Google Scholar]
- 35.Amin TT, Amr MA, Zaza BO, Suleman W. Harm perception, attitudes and predictors of waterpipe (shisha) smoking among secondary school adolescents in Al-Hassa, Saudi Arabia. Asian Pac J Cancer Prev. 2010;11(2):293–301. [PubMed] [Google Scholar]
- 36.Grekin ER, Ayna D. Waterpipe smoking among college students in the United States: a review of the literature. J Am Coll Health. 2012;60(3):244–9. doi: 10.1080/07448481.2011.589419. [DOI] [PubMed] [Google Scholar]
- 37.Lipkus IM, Eissenberg T, Schwartz-Bloom RD, Prokhorov AV, Levy J. Affecting perceptions of harm and addiction among college waterpipe tobacco smokers. Nicotine Tob Res. 2011;13(7):599–610. doi: 10.1093/ntr/ntr049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Martinasek MP, Gibson-Young L, Forrest J. Hookah smoking and harm perception among asthmatic adolescents: findings from the Florida youth tobacco survey. J Sch Health. 2014;84(5):334–41. doi: 10.1111/josh.12153. [DOI] [PubMed] [Google Scholar]
- 39.Smith SY, Curbow B, Stillman FA. Harm perception of nicotine products in college freshmen. Nicotine Tob Res. 2007;9(9):977–82. doi: 10.1080/14622200701540796. [DOI] [PubMed] [Google Scholar]
- 40.Smith JR, Novotny TE, Edland SD, Hofstetter CR, Lindsay SP, Al-Delaimy WK. Determinants of hookah use among high school students. Nicotine Tob Res. 2011;13(7):565–72. doi: 10.1093/ntr/ntr041. [DOI] [PubMed] [Google Scholar]
- 41.Heinz AJ, Giedgowd GE, Crane NA, Veilleux JC, Conrad M, Braun AR, Olejarska NA, Kassel JD. A comprehensive examination of hookah smoking in college students: use patterns and contexts, social norms and attitudes, harm perception, psychological correlates and co-occurring substance use. Addict Behav. 2013;38(11):2751–60. doi: 10.1016/j.addbeh.2013.07.009. [DOI] [PubMed] [Google Scholar]
- 42.Carroll MV, Shensa A, Primack BA. A comparison of cigarette- and hookah-related videos on YouTube. Tob Control. 2013;22(5):319–23. doi: 10.1136/tobaccocontrol-2011-050253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vansickel AR, Shihadeh A, Eissenberg T. Waterpipe tobacco products: nicotine labelling versus nicotine delivery. Tob Control. 2012;21(3):377–9. doi: 10.1136/tc.2010.042416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Smith-Simone SY, Curbow BA, Stillman FA. Differing psychosocial risk profiles of college freshmen waterpipe, cigar, and cigarette smokers. Addict Behav. 2008;33(12):1619–24. doi: 10.1016/j.addbeh.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 45.Sharma E, Clark PI, Sharp KE. Understanding psychosocial aspects of waterpipe smoking among college students. Am J Health Behav. 2014;38(3):440–7. doi: 10.5993/AJHB.38.3.13. [DOI] [PubMed] [Google Scholar]
- 46.Braun RE, Glassman T, Wohlwend J, Whewell A, Reindl DM. Hookah use among college students from a Midwest University. J Community Health. 2012;37(2):294–8. doi: 10.1007/s10900-011-9444-9. [DOI] [PubMed] [Google Scholar]
- 47.Cobb C, Ward KD, Maziak W, Shihadeh AL, Eissenberg T. Waterpipe tobacco smoking: an emerging health crisis in the United States. Am J Health Behav. 2010;34(3):275–85. doi: 10.5993/ajhb.34.3.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Carroll MV, Chang J, Sidani JE, Barnett TE, Soule EK, Balbach E, Primack BA. Reigniting tobacco ritual: waterpipe tobacco smoking establishment culture in the United States. Nicotine Tob Res. 2014;16(12):1549–58. doi: 10.1093/ntr/ntu101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Maziak K. The global epidemic of waterpipe smoking. Addict Behav. 2011;36(1–2):1–5. doi: 10.1016/j.addbeh.2010.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.World Health Organization. Waterpipe Tobacco Smoking: Health Effects, Research Needs and Recommended Actions by Regulators. Geneva, Switzerland: World Health Organization; 2005. TobReg Advisory Note. [Google Scholar]
- 51.Baheiraei A, Hamzehgardeshi Z, Mohammadi MR, Nedjat S, Mohammadi E. Lifetime and current waterpipe use among adolescents in Tehran, Islamic Republic of Iran. [PubMed] [Google Scholar]
- 52.Dugas E, Tremblay M, Low NC, Cournoyer D, O’Loughlin J. Water-pipe smoking among North American youths. Pediatrics. 2010;125(6):1184–9. doi: 10.1542/peds.2009-2335. [DOI] [PubMed] [Google Scholar]
- 53.Jarrett T, Blosnich J, Tworek C, Horn K. Hookah use among U.S. college students: results from the National College Health Assessment II. Nicotine Tob Res. 2012;14(10):1145–53. doi: 10.1093/ntr/nts003. [DOI] [PubMed] [Google Scholar]
- 54.Jawad M, McIvver C, Iqbal Z. Prevalence and correlates of lifetime waterpipe, cigarette, alcohol and drug use among secondary school students in Stoke-on-Trent, UK: a post hoc cross-sectional analysis. J Public Health (Oxf) 2014;36(4):615–21. doi: 10.1093/pubmed/fdu002. [DOI] [PubMed] [Google Scholar]
- 55.Lipkus IM, Reboussin BA, Wolfson M, Sutfin EL. Assessing and predicting susceptibility to waterpipe tobacco use among college students. Nicotine Tob Res. 2015 doi: 10.1093/ntr/ntu336. [epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sterling KL, Mermelstein R. Examining hookah smoking among a cohort of adolescent ever smokers. Nicotine Tob Res. 2011;13(12):1202–9. doi: 10.1093/ntr/ntr146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Azab M, Khabour MF, Alkaraki AK, Eissenberg T, Alzoubi KH, Primack BA. Water pipe tobacco smoking among university students in Jordan. Nicotine Tob Res. 2010;12(6):606–12. doi: 10.1093/ntr/ntq055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Maziak W. Rise of waterpipe smoking. BMJ. 2015;350:h1991. doi: 10.1136/bmj.h1991. [DOI] [PubMed] [Google Scholar]
- 59.Shihadeh A, Azar S, Antonios C, Haddad A. Towards a topographical model of narghile water-pipe café smoking: a pilot study in a high socioeconomic status neighborhood of Beirut, Lebanon. Pharmacol Biochem Behav. 2004;79(1):75–82. doi: 10.1016/j.pbb.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 60.Djordjevic MV, Stellman SD, Zang E. Doses of nicotine and lung carcinogens delivered to cigarette smokers. J Natl Cancer Inst. 2000;92(2):106–11. doi: 10.1093/jnci/92.2.106. [DOI] [PubMed] [Google Scholar]
- 61.Cobb CO, Shihadeh A, Weaver MF, Eissenberg T. Waterpipe tobacco smoking and cigarette smoking: a direct comparison of toxicant exposure and subjective effects. Nicotine Tob Res. 2011;13(2):78–87. doi: 10.1093/ntr/ntq212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Maziak W, Rastam S, Ibrahim I, Ward KD, Shihadeh A, Eissenberg T. CO exposure, puff topography, and subjective effects in waterpipe tobacco smokers. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Breland AB, Kleykamp BA, Eissenberg T. Clinical laboratory evaluation of potential reduced exposure products for smokers. Nicotine Tob Res. 2006;8(6):727–38. doi: 10.1080/14622200600789585. [DOI] [PubMed] [Google Scholar]
- 64.Eissenberg T, Shihadeh A. Waterpipe tobacco and cigarette smoking: direct comparison of toxicant exposure. Am J Prev Med. 2009;37(6):518–23. doi: 10.1016/j.amepre.2009.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Blank MD, Cobb CO, Kilgalen B, Austin J, Weaver MF, Shihadeh A, Eissenberg T. Acute effects of waterpipe tobacco smoking: a double-blind, placebo-control study. Drug Alcohol Depend. 2011;116(1–3):102–9. doi: 10.1016/j.drugalcdep.2010.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cobb CO, Sahmarani K, Eisseneberg T, Shihadeh A. Acute toxicant exposure and cardiac autonomic dysfunction from smoking a single narghile waterpipe with tobacco and with a “healthy” tobacco-free alternative. Toxicol Lett. 2012;215(1):70–5. doi: 10.1016/j.toxlet.2012.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Grainge MJ, Shahab L, Hammond D, O’Connor RJ, McNeill A. First cigarette on waking and time of day as predictors of puffing behavior in UK adult smokers. Drug Alcohol Depend. 2009;101(3):191–5. doi: 10.1016/j.drugalcdep.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 68.Perkins KA, Karelitz JL, Giedgowd GE, Conklin CA. The reliability of puff topography and subjective responses during ad lib smoking of a single cigarette. 2012;14(4):490–4. doi: 10.1093/ntr/ntr150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.O’Connor RJ, Rees VW, Norton KJ, Cummings KM, Connolly GN, Alpert HR, Sjödin A, Romanoff L, Li Z, June KM, Giovino GA. Does switching to reduced ignition propensity cigarettes alter smoking behavior or exposure to tobacco smoke constituents? Nicotine Tob Res. 2010;12(10):1011–8. doi: 10.1093/ntr/ntq139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Monzer B, Sepetdjian E, Saliba N, Shihadeh A. Charcoal emissions as a source of CO and carcinogenic PAH in mainstream narghile waterpipe smoke. Food Chem Toxicol. 2008;46(9):2991–5. doi: 10.1016/j.fct.2008.05.031. [DOI] [PubMed] [Google Scholar]
- 71.Shihadeh A, Saleh R. Polycyclic aromatic hydrocarbons, carbon monoxide, “tar”, and nicotine in the mainstream smoke aerosol of the narghile water pipe. Food Chem Toxicol. 2005;43(5):655–61. doi: 10.1016/j.fct.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 72.Nguyen T, Hlangothi D, Martinez RA, 3rd, Jacob D, Anthony K, Nance H, Saleh MA. Charcoal burning as a source of polyaromatic hydrocarbons in waterpipe smoking. J Environ Sci Health B. 2013;48(12):1097–102. doi: 10.1080/03601234.2013.824300. [DOI] [PubMed] [Google Scholar]
- 73.Sepetdjian E, Shihadeh A, Saliba NA. Measurement of 16 polycyclic aromatic hydrocarbons in narghile waterpipe tobacco smoke. Food Chem Toxicol. 2008;46(5):1582–90. doi: 10.1016/j.fct.2007.12.028. [DOI] [PubMed] [Google Scholar]
- 74.Sepetdjian E, Saliba N, Shihadeh A. Carcinogenic PAH in waterpipe charcoal products. Food Chem Toxicol. 2010;48(11):3242–5. doi: 10.1016/j.fct.2010.08.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Al Rashidi M, Shihadeh A, Saliba NA. Volatile aldehydes in the mainstream smoke of the narghile waterpipe. Food Chem Toxicol. 2008;46(11):3546–9. doi: 10.1016/j.fct.2008.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Schubert J, Bewersdorff J, Luch A, Schulz TG. Waterpipe smoke: a considerable source of human exposure against furanic compounds. Anal Chim Acta. 2012;709:105–12. doi: 10.1016/j.aca.2011.10.012. [DOI] [PubMed] [Google Scholar]
- 77.Schubert J, Heinke V, Bewersdorff J, Luch A, Schulz TG. Waterpipe smoking: the role of humectants in the release of toxic carbonyls. Arch Toxicol. 2012;86(8):1309–16. doi: 10.1007/s00204-012-0884-5. [DOI] [PubMed] [Google Scholar]
- 78.Barnett TE, Curbow BA, Soule EK, Tomar SL, Thombs DL. Carbon monoxide levels among patrons of hookah cafes. Am J Prev Med. 2011;40(3):324–8. doi: 10.1016/j.amepre.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 79.Martinasek MP, Ward KD, Calvanese AV. Change in carbon monoxide exposure among waterpipe bar patrons. Nicotine Tob Res. 2014;16(7):1014–9. doi: 10.1093/ntr/ntu041. [DOI] [PubMed] [Google Scholar]
- 80.Al Ali R, Rastam S, Ibrahim I, Bazzi A, Fayad S, Shihadeh AL, Zaatari GS, Maziak W. A comparative study of systemic carcinogen exposure in waterpipe smokers, cigarette smokers and non-smokers. Tob Control. 2015;24(2):125–7. doi: 10.1136/tobaccocontrol-2013-051206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Radwan G, Hecht SS, Carmella SG, Loffredo CA. Tobacco-specific nitrosamine exposures in smokers and nonsmokers exposed to cigarette or waterpipe tobacco smoke. Nicotine Tob Res. 2013;15(1):130–8. doi: 10.1093/ntr/nts099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Cobb CO, Blank MD, Morlett A, Shihadeh A, Jaroudi E, Karaoghlanian N, Kilgalen B, Austin J, Weaver MF, Eissenberg T. Comparison of puff topography, toxicant exposure, and subjective effects in low- and high-frequency waterpipe users: a double-blind, placebo-control study. Nicotine Tob Res. 2015;17(6):667–74. doi: 10.1093/ntr/ntu196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Shihadeh AL, Eissenberg TE. Significance of smoking machine toxicant yields to blood-level exposure in water pipe tobacco smokers. Cancer Epidemiol Biomarkers Prev. 2011;20(11):2457–60. doi: 10.1158/1055-9965.EPI-11-0586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Shihadeh A, Schubert J, Klaiany J, El Sabban M, Luch A, Saliba NA. Toxicant content, physical properties and biological activity of waterpipe tobacco smoke and its tobacco-free alternatives. Tob Control. 2015;24 (Suppl 1):i22–i30. doi: 10.1136/tobaccocontrol-2014-051907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.International Organization of Standardization. [Accessed 21 Jul 2015];Cigerettes – Determination of nicotine-free dry particulate matter and nicotine in sidestream smoke. 2013 https://www.iso.org/obp/ui/#iso:std:iso:20773:ed-2:v1:en.
- 86.Akl EA, Gaddamm S, Gunukula SK, Honeine R, Jaoude PA, Irani J. The effects of waterpipe tobacco smoking on health outcomes: a systematic review. Int J Epidemiol. 2010;39(3):834–57. doi: 10.1093/ije/dyq002. [DOI] [PubMed] [Google Scholar]
- 87.El-Zaatari ZM, Chami HA, Zaatari GS. Health effects associated with waterpipe smoking. Tob Control. 2015;24 (Suppl 1):i31–i43. doi: 10.1136/tobaccocontrol-2014-051908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ashurst JV, Urquhart M, Cook MD. Carbon monoxide poisoning secondary to hookah smoking. J Am Osteopath Assoc. 2012;112(10):686–8. [PubMed] [Google Scholar]
- 89.Cavus UY, Rehber ZH, Ozeke O, Ilkay E. Carbon monoxide poisoning associated with narghile use. Emerg Med J. 2010;27(5):406. doi: 10.1136/emj.2009.077214. [DOI] [PubMed] [Google Scholar]
- 90.Clarke SF, Stephens C, Farhan M, Ward P, Keshishian C, Murray V, Zenner D. Multipe patients with carbon monoxide toxicity from water-pipe smoking. Prehosp Disaster Med. 2012;27(6):612–4. doi: 10.1017/S1049023X12001227. [DOI] [PubMed] [Google Scholar]
- 91.Karaca Y, Eryigit U, Aksut N, Turkmen S. Syncope associated with water pipe smoking. BMJ Case Rep. 2013 doi: 10.1136/bcr-2013-009526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.La Fauci G, Weiser G, Steiner IP, Shavit I. Carbon monoxide poisoning in narghile (water pipe) tobacco smokers. CJEM. 2012;14(1):57–9. doi: 10.2310/8000.2011.110431. [DOI] [PubMed] [Google Scholar]
- 93.Lim BL, Lim GH, Seow E. Case of carbon monoxide poisoning after smoking shisha. Int J Emerg Med. 2009;2(2):121–2. doi: 10.1007/s12245-009-0097-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ozkan S, Ozturk T, Ozmen Y, Durukan P. Syncope associated with carbon monoxide poisoning due to narghile smoking. Case Rep Emerg Med. 2013;2013:796857. doi: 10.1155/2013/796857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Türkmen S, Eryigit U, Sahin A, Yeniocak S, Turedi S. Carbon monoxide poisoning associated with water pipe smoking. Clin Toxicol (Phila) 2011;49(7):697–8. doi: 10.3109/15563650.2011.598160. [DOI] [PubMed] [Google Scholar]
- 96.von Rappard J, Schönenberger M, Býrlocher L. Carbon monoxide poisoning following use of a water pipe/hookah. Dtsch Arztebl Int. 2014;111(40):674–9. doi: 10.3238/arztebl.2014.0674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.American Lung Association. [Accessed 21 Jul 2015];Hookah smoking: a growing threat to public health. 2015 20 http://www.lung.org/stop-smoking/tobacco-control-advocacy/reports-resources/cessation-economic-benefits/reports/hookah-policy-brief.pdf. [Google Scholar]
- 98.Knishkowy B, Amitai Y. Water-pipe (narghile) smoking: an emerging health risk behavior. Pediatrics. 2005;116(1):e113–9. doi: 10.1542/peds.2004-2173. [DOI] [PubMed] [Google Scholar]
- 99.Hakim F, Hellou E, Goldbart A, Katz R, Bentur Y, Bentur L. The acute effects of water-pipe smoking on the cardiorespiratory system. Chest. 2011;139(4):775–81. doi: 10.1378/chest.10-1833. [DOI] [PubMed] [Google Scholar]
- 100.Hawari FI, Obeidat NA, Ayub H, Ghonimat I, Eissenberg T, Dawahrah S, Beano H. The acute effects of waterpipe smoking on lung function and exercise capacity in a pilot study of health participants. Inhal Toxicol. 2013;25(9):492–7. doi: 10.3109/08958378.2013.806613. [DOI] [PubMed] [Google Scholar]
- 101.Shaikh RB, Vijayaraghavan N, Sulaiman AS, Kazi S, Shafi MS. The acute effects of waterpipe smoking on the cardiovascular and respiratory systems. J Preve Med Hyg. 2008;49(3):101–7. [PubMed] [Google Scholar]
- 102.Bentur L, Hellou E, Goldbart A, Pillar G, Monovich E, Salameh M, Scherb I, Bentur Y. Laboratory and clinical acute effects of active and passive indoor group water-pipe (narghile) smoking. Chest. 2014;145(4):803–9. doi: 10.1378/chest.13-0960. [DOI] [PubMed] [Google Scholar]
- 103.Jawad M, Jawad S, Mehdi A, Sardar A, Jawad AM, Hamilton FL. A qualitative analysis among regular waterpipe tobacco smokers in London universities. Int J Tuberc Lung Dis. 2013;17(10):1364–9. doi: 10.5588/ijtld.12.0923. [DOI] [PubMed] [Google Scholar]
- 104.Aboaziza E, Eissenberg T. Waterpipe tobacco smoking: what is the evidence that it supports nicotine/tobacco dependence? Tob Control. 2015;24 (Suppl 1):i44–i53. doi: 10.1136/tobaccocontrol-2014-051910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Aoun J, Saleh N, Waked M, Salamé J, Salameh P. Lung cancer correlates in Lebanese adults: a pilot case—control study. J Epidemiol Glob Health. 2013;3(4):235–44. doi: 10.1016/j.jegh.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Gupta D, Boffetta P, Gaborieau V, Jindal SK. Risk factors of lung cancer in Chandigarh, India. Indian J Med Res. 2001;113:142–50. [PubMed] [Google Scholar]
- 107.Koul PA, Hajni, Sheikh MA, Khan UH, Shah A, Khan Y, Ahangar AG, Tasleem RA. Hookah smoking and lung cancer in the Kashmir valley of the Indian subcontinent. Asian Pac J Cancer Prev. 2011;12(2):519–24. [PubMed] [Google Scholar]
- 108.Mohammad Y, Shaaban R, Al-Zahab BA, Khaltaev N, Bousquet J, Dubaybo B. Impact of active and passive smoking as risk factors for asthma and COPD in women presenting in primary care in Syria: first report by the WHO-GARD survey group. Int J Chron Obstruct Pulmon Dis. 2013;8:473–82. doi: 10.2147/COPD.S50551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Rammah M, Dandachi F, Salman R, Shihadeh A, El-Sabban M. In vitro cytotoxicity and mutagenicity of mainstream waterpipe smoke and its functional consequences on alveolar type II derived cells. Toxicol Lett. 2012;211(3):220–31. doi: 10.1016/j.toxlet.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Tageldin MA, Nafti S, Khan JA, Nejjari C, Beji M, Mahboub B, Obeidat NM, Uzaslan E, Sayiner A, Wali S, Rashid N, El Hasnaoui A BREATHE Study Group. Distribution of COPD-related symptoms in the Middle East and North Africa: results of the BREATHE study. Respir Med. 2012;106 (Suppl 2):S25–32. doi: 10.1016/S0954-6111(12)70012-4. [DOI] [PubMed] [Google Scholar]
- 111.Waked M, Khayat G, Salameh P. Chronic obstructive pulmonary disease prevalence in Lebanon: a cross-sectional descriptive study. Clin Epidemiol. 2011;3:315–23. doi: 10.2147/CLEP.S26350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Joseph S, Pascale S, Georges K, Mirna W. Cigarette and waterpipe smoking decrease respiratory quality of life in adults: results from a national cross-sectional study. Pulm Med. 2012;2012:868294. doi: 10.1155/2012/868294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Salameh P, Waked M, Khoury F, Akiki Z, Abou Abbass L, Dramaix M Chronic Bronchitis Study Group. Waterpipe smoking and dependence are associated with chronic bronchitis: a case-control study in Lebanon. East Mediterr Health J. 2012;18(10):996–1004. doi: 10.26719/2012.18.10.996. [DOI] [PubMed] [Google Scholar]
- 114.Zeidan RK, Rachidi S, Awada S, El Hajje A, El Bawab W, Salamé J, Bejjany R, Salameh P. Carbon monoxide and respiratory symptoms in young adult passive smokers: a pilot study comparing waterpipe to cigarette. Int J Occup Med Environ Health. 2014;27(4):571–82. doi: 10.2478/s13382-014-0246-z. [DOI] [PubMed] [Google Scholar]
- 115.Sibai AM, Tohme RA, Almedawar MM, Itani T, Yassine SI, Nohra EA, Isma’eel HA. Lifetime cumulative exposure to waterpipe smoking is associated with coronary artery disease. Atherosclerosis. 2014;234(2):454–60. doi: 10.1016/j.atherosclerosis.2014.03.036. [DOI] [PubMed] [Google Scholar]
- 116.Jukema JB, Bagnasco DE, Jukema RA. Waterpipe smoking: not necessarily less hazardous than cigarette smoking: possible consequences for (cardiovascular) disease. Neth Heart J. 2014;22(3):91–9. doi: 10.1007/s12471-013-0501-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Harrell JS, Bangdiwala SI, Deng S, Webb JP, Bradley C. Smoking initiation in youth: the roles of gender, race, socioeconomics, and developmental status. J Adolesc Health. 1998;23(5):271–9. doi: 10.1016/s1054-139x(98)00078-0. [DOI] [PubMed] [Google Scholar]
- 118.Centers for Disease Control and Prevention (CDC). . High school students who tried to quit smoking cigarettes--United States, 2007. MMWR Morb Mortal Wkly Rep. 2009;58(16):428–31. [PubMed] [Google Scholar]
- 119.de Koning HJ, Mexa R, Plevritis SK, ten Haaf K, Munshi VN, Jeon J, Erdogan SA, Kong CY, Han SS, van Rosmalen J, Choi SE, Pinsky PF, Berrington de Gonzalez A, Berg CD, Black WC, Tammemýgi MC, Hazelton WD, Feuer EJ, McMahon PM. Benefits and harms of computed tomography lung cancer screening strategies: a comparative modeling study for the U.S. Preventive Services Task Force. Ann Intern Med. 2014;160(5):311–20. doi: 10.7326/M13-2316. [DOI] [PMC free article] [PubMed] [Google Scholar]