Abstract
Context
Psychiatric problems are among the most common health problems of childhood.
Objective
To test whether these health problems adversely affect adult functioning even if the problems themselves do not persist.
Design
Prospective, population-based study of 1420 participants assessed with structured interviews up to 6 times in childhood (ages 9 to 16; 6674 observations) for common psychiatric diagnoses and subthreshold psychiatric problems.
Setting and population
Community sample.
Main outcome measure
Participants were then assessed 3 times in young adulthood (ages 19, 21, and 24–26; 3215 observations of 1273 subjects) for adverse outcomes related to health, legal, financial, and social functioning.
Results
Participants with a childhood disorder had 6 times higher odds of at least one adverse adult outcome as compared to those with no history of psychiatric problems and 9 times higher odds of 2 or more such indicators (1 indicator: 59.5% vs. 19.9%, p <0.001; 2+ indicators: 34.2% vs. 5.6%, p <0.001). These associations persisted after statistically controlling for childhood psychosocial hardships and adult psychiatric problems. Risk was not limited to those with a diagnosis: participants with subthreshold psychiatric problems had 3 times higher odds of adult adverse outcomes and 5 time higher odds of 2 or more outcomes (1 indicator: 41.9% vs. 19.9%, p <0.001; 2+ indicators: 23.2% vs. 5.6%, p <0.001). The best diagnostic predictor of adverse outcomes was cumulative childhood exposure to psychiatric disorders.
Conclusions
Common, typically moderately-impairing, childhood psychiatric problems are associated with a disrupted transition to adulthood even if the problems do not persist into adulthood and even if the problems are subthreshold. Such problems provide potential target for public health efforts to ameliorate adult suffering and morbidity.
Keywords: Childhood, psychiatric disorders, depression, conduct problems, adult outcomes
Introduction
In the 2010 global burden of disease analysis, neuropsychiatric disorders in youth ages 10 to 24 were the leading cause of disease burden1. Unlike many chronic physical health problems, most psychiatric disorders are first diagnosed in childhood2–4. This allows such disorders and their sequelae to affect the entire lifespan. Some portion of this burden is due to a few rare, but highly impairing, chronic psychiatric disorders (e.g., schizophrenia, pervasive developmental disorders)1. The vast majority of this burden, however, is due to more common (point prevalence >1%), typically moderately impairing emotional and behavioral disorders. These common disorders create a substantial burden within childhood5. Here we report on how these common childhood disorders affect adverse functional outcomes during the transition to adulthood.
Prospective studies that follow children into early adulthood and retrospective studies of adults confirm that most adults with psychiatric disorders previously had a disorder in childhood2, 4, 6. Optimal adult functioning, however, includes much more than psychiatric status. A successful transition to adulthood involves a bevy of developmental challenges: staying healthy, avoiding health risk behaviors, completing one’s education, getting and maintaining a job, avoiding or desisting illegal behavior, and developing and maintaining a social support network7. Failure in any area can be a major barrier to a successful transition to adulthood. In the UK’s National Child Development Study, any recorded psychological problem predicted adult incomes and marriage stability at age 508. Other studies have looked at long-term functional outcomes of individual childhood disorders9–11. These apparent long-term effects may simply be accounted for by continued psychiatric problems. This study uses a prospective, longitudinal community sample to test 1) whether childhood psychiatric problems predict adverse health, legal, financial, and social functioning in early adulthood, and 2) whether any such effects persist when adjusting for adult psychiatric status.
Studying only children meeting full criteria for psychiatric disorders, however, may severely underestimate the burden. Subthreshold problems do not meet full diagnostic criteria, but often are significantly impairing12, 13. As many as half of clinically referred child psychiatric patients do not meet criteria for a well-specified DSM diagnosis14, 15. This is not a minor problem. A complete understanding of the burden of childhood psychiatric problems must include such subthreshold cases. This study defines subthreshold cases as individuals with significant impairment resulting from psychiatric symptoms that do not meet full DSM criteria for a disorder3, 12.
Which early psychiatric problems have the most severe long-term consequences? Some specific childhood disorders may have a worse prognosis than others (specificity hypothesis)9, 10. However, recent work suggests that the propensity to common psychiatric disorders may be summarized by a few (or one) underlying dimensions16–19. This is not surprising given the shared genetic liability commonly observed among common psychiatric disorders20, the non-specific patterns of familial transmission of psychiatric problems21, and the considerable concurrent and sequential co-morbidity of psychiatric diagnoses22. Alternatively, the accumulation of multiple/repeated exposures to psychiatric distress throughout childhood (the cumulative exposure hypothesis) may be more important than specific disorders themselves.
Methods
Participants
The Great Smoky Mountains Study is a longitudinal, representative study of children in 11 predominantly-rural counties of North Carolina (see23). Three cohorts of children, ages 9, 11, and 13 years, were recruited from a pool of some 12,000 children using a two-stage sampling design, resulting in N = 1,420 participants (49% female; see also23). The two-stage sampling design involved oversampling of participants at risk for psychopathology. In addition, American Indians were also oversampled to constitute 25% of the sample. Sampling weights are applied to adjust for differential probability of selection.
Annual assessments were completed on the 1420 children until age 16 and then again at ages 19, 21, and 25 for a total of 9941 assessments. Interviews were completed by a parent figure and the subject to age 16, and by the participant only thereafter. Before all interviews, parent and child signed informed consent/assent forms. The study protocol and consent forms have been approved by the Duke University Medical Center Institutional Review Board.
Childhood/Adolescent Psychiatric Status
Psychiatric disorders were assessed using the structured Child and Adolescent Psychiatric Assessment (CAPA) until age 1624. A 3-month primary period is used to assess psychiatric symptoms. A symptom was counted as present if reported by either parent or child or both. Scoring programs written in SAS combine information about the date of onset, duration, and intensity of each symptom to create DSM-IV diagnoses. A two-week test-retest reliability study of CAPA diagnoses in children aged 10 through 18 found kappa values ranged from 0.5 for conduct disorder to K = 1.0 for substance dependence25. CAPA diagnoses are associated with higher scores on well-established behavioral scales, higher levels of psychosocial impairments, and use of specialty mental health services24.
Common childhood psychiatric disorders assessed included anxiety disorders (separation anxiety, generalized anxiety, social phobia, specific phobia, agoraphobia, panic disorder, obsessive-compulsive disorder, and posttraumatic stress disorder), mood disorders (major depression, dysthymia, mania, and hypomania), conduct disorder, oppositional defiant disorder, ADHD, and substance disorders.
Childhood impairment was assessed in 17 areas of functioning using definitions and rules specified in the CAPA glossary and the interview schedule. Areas of functioning assessed included self-care, completion of household chores, completion of homework, academic performance, school suspension, and relationships with parents, sibling, peers or teachers. A positive rating required a description of some decrement in actual function (see26 for a full description). After completing the symptom part of the interview, the interviewer reviews all areas of positive symptomatology. The participant is questioned about whether those symptoms have resulted in any of the 17 impairment categories (each impairment category is reviewed separately). Symptomatic impairment is met when individuals displayed impairment resulting from psychiatric symptoms but did not meet full diagnostic criteria. The test-retest intraclass correlation coefficient for level of psychosocial impairment by child self-report was 0.7726. Previous work found that children with symptomatic impairment were positive for multiple markers of “caseness” including risk for a psychiatric diagnosis one year later12. Symptomatic impairment status was used to identify subthreshold cases.
Childhood covariates
To clarify that the effects of childhood psychiatric status are independent of other childhood psychosocial factors, all models account for the following family and individual hardship variables: low socioeconomic status (SES), including family poverty, low parental educational attainment, and low parental occupational prestige; unstable family structure including single parent family, divorce, parental separation, presence of step-parent, or change in parent structure; family dysfunction including inadequate parental supervision, domestic violence, parental over involvement, maternal depression, marital relationship characterized by apathy, indifference, or high conflict, and high conflict between parent and child; and maltreatment including physical abuse, sexual abuse, and parental neglect. A full description of these variables is available in a previous publication27 and also in supplemental materials.
Adult health, legal, financial, and social outcomes
Our aim was to identify a broad range of outcomes that that typically a) impede functioning for an extended period of time, b) across many domains, and c) for most individuals. These outcomes covered four domains: health, legal, financial, and social functioning. Table 1 provides a full list of outcomes, their definitions and prevalence. All outcomes except where noted (e.g., official criminal records) were assessed using the Young Adult Psychiatric Assessment (YAPA),28 an upward extension of the CAPA interview administered to the participants themselves. In most cases, an individual was positive for outcomes if it was reported at any adult assessment. In some cases, the thresholds for indicators were self-evident (e.g., dropping out of high school). Where such thresholds were not available, indicators were defined to identify approximately 5% of participants or fewer (e.g., unable to keep a job defined as fired from 3+ jobs) to insure the outcome was deviant. Additional information about outcomes is available in supplemental table 1.
Table 1.
Definitions and prevalence of young adult outcomes
| Definition | Prevalence | |
|---|---|---|
| % | ||
| Health | ||
| Multiple psych problems | Meeting full criteria for 2 or more different DSM disorders across all adult assessments. | 3.9% |
| Multiple addictions | Meeting full criteria for DSM substance dependence for 2 or more substances across all adult assessments | 5.3% |
| Suicidality | Reporting recurrent thoughts of death (not just fear of dying), recurrent ideation, a suicide attempt, or specific plan for committing suicide | 7.1% |
| Serious physical event | Diagnosis with serious physical illness, involved in serious accident or death. Physical illness and accidents had to involve risk of death or chronic disability. | 3.4% |
| Legal | ||
| Serious criminal activity | Official record of felony charge between ages 16 and 25 | 7.7% |
| Incarceration | Participant reported time spent in jail or prison across adult assessments | 3.3% |
| Financial | ||
| High school dropout | Had not received high school diploma, equivalent degree, or GED by last adult observation | 12.4% |
| Unable to keep job | Participant reported being fired from 3+ jobs over the course of adult observations | 6.6% |
| Residential instability | Moved 6 or more times in 5 years | 5.2% |
| Social | ||
| Early parenthood | Participant reported becoming a parent prior to age of majority or legal adulthood (age 18) | 4.6% |
| No social support | Participant reported no best friend/confidante, little to no relationship with parents, and rare contact with peers across all adult observations | 3.0% |
| Relational instability | Multiple divorces | 4.8% |
All percentages are weighted.
Adult covariates
To clarify that the long-term effects of childhood psychiatric status are independent of adult psychiatric status, all models account for adult psychiatric disorder status and subthreshold status. Adult psychiatric and subthreshold status was assessed using the YAPA28 as described above. Adult subthreshold status was defined exactly as it was for childhood (positive for symptom-related impairment), but the impairment categories were adapted to apply to adult relationships and functioning in the home, school, employment and community settings.
Analytic strategy
Childhood diagnostic status was based on 6674 assessments of the 1420 GSMS participants between ages 9 and 16. Participants were coded as psychiatric cases if they met criteria for a childhood psychiatric disorder at any assessment. If they never met criteria for a psychiatric disorder in childhood but met criteria for symptomatic impairment at some assessment, then they were coded as subthreshold cases. Remaining subjects had never met criteria for either a psychiatric disorder or symptomatic impairment (noncases). Sampling weights were applied in all analyses to insure that results represent unbiased estimates for the original sample population. Consistent with common conventions, all percentages provide in the results are weighted percentages and Ns/sample sizes are unweighted. Weighted regression models were used to look at differences between these three groups on adult outcomes. All models used SAS PROC GENMOD with robust variance (sandwich type) estimates derived from generalized estimating equations to adjust the standard errors for the stratified design. A Bonferroni correction was applied to unadjusted models to account for the number of adult outcomes. After bivariate models were tested, adjusted models tested group differences while accounting for sex, race, childhood family hardship variables, and adult psychiatric and subthreshold status.
Results
Descriptive Information
Of the total sample of 1420 subjects, 26.2% (unweighted N=527) met criteria for a common behavioral or emotional disorder at some point in childhood/adolescence (ages 9 to 16), 31.0% (N=466) displayed subthreshold psychiatric problems only, and 42.7% (N=427) never met criteria for a disorder or subthreshold problems. For the purposes of this analysis, we did not include children or adolescents meeting criteria for a tic or elimination disorder – two categories of disorders that are relatively common and have been included in past analyses. Follow-up rates into adulthood (ages 19, 21, and 24–26) were similar across groups (psychiatric cases: 475 of 527 or 90.1%; subthreshold only cases: 423 of 466 or 90.7%; non-cases: 375 of 427 or 87.8%) with no differences between the case group follow-up rates and either other control group (cases vs. noncases, p = 0.23; impairment cases vs. noncase controls, p = 0.18). Childhood psychiatric cases were more likely to be male, American Indian and to have all types of family adversities as compared to noncases (supplemental table 2). A similar pattern was observed for subthreshold- versus non-cases. There were no demographic differences between subthreshold and psychiatric cases, but full cases had higher levels of family dysfunction and maltreatment.
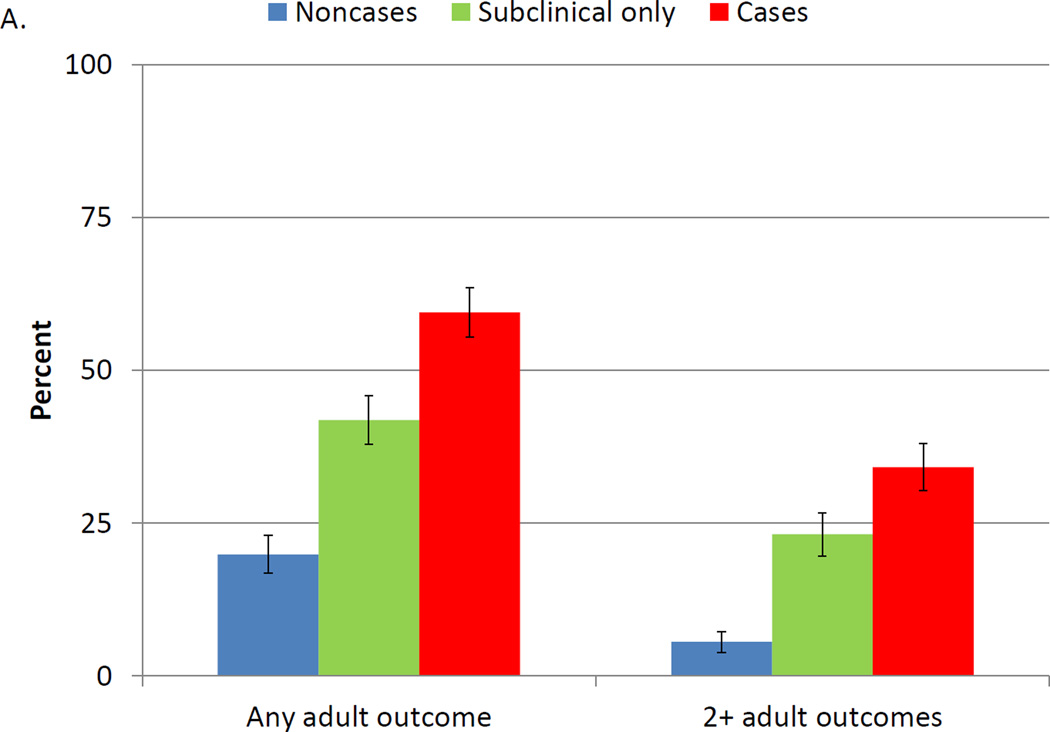
Childhood psychiatric status and adult indicators
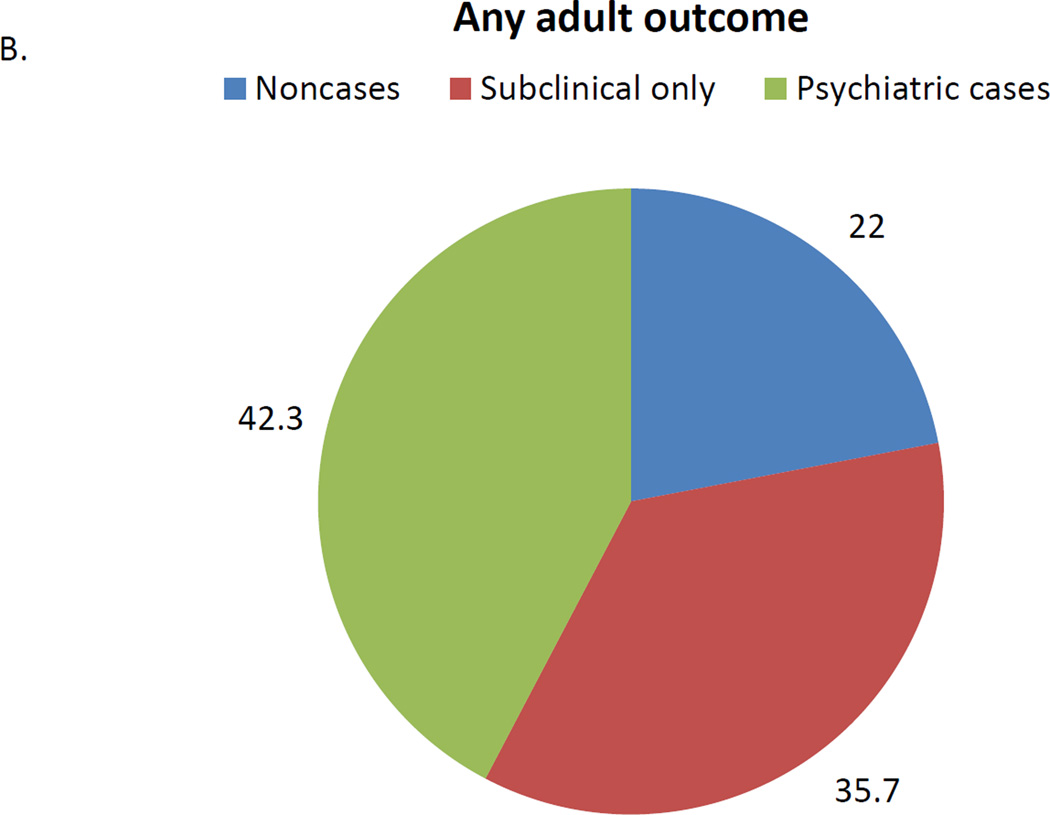
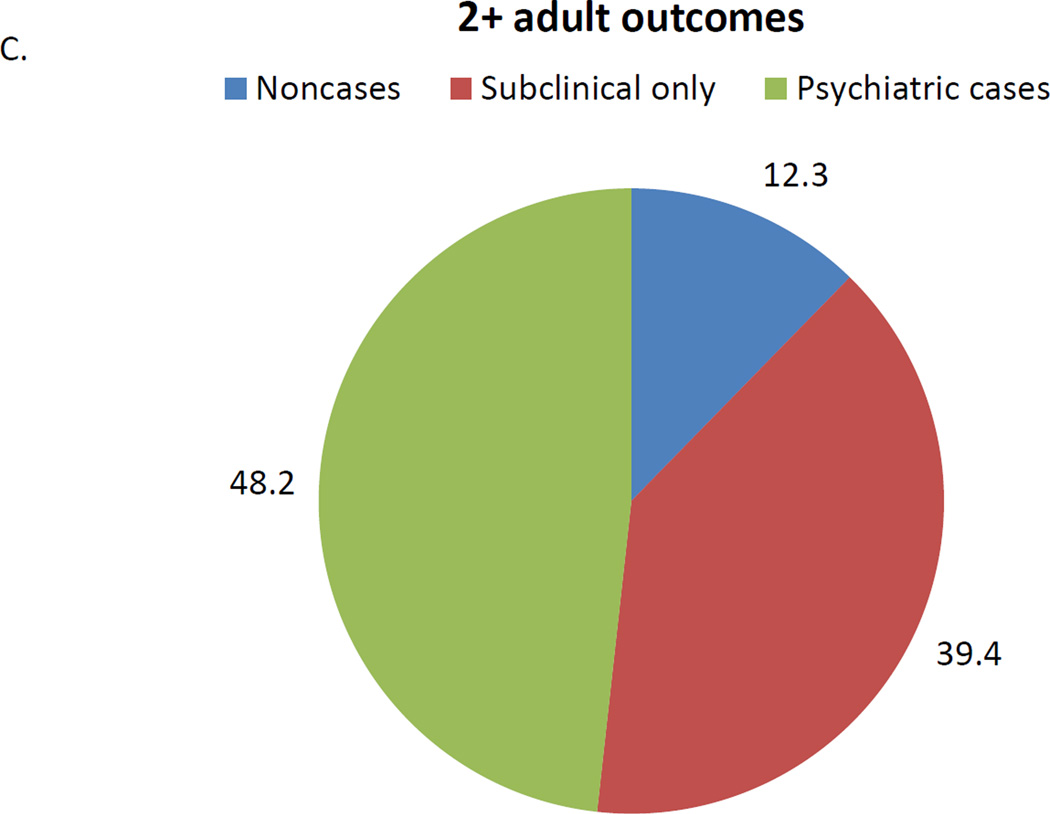
Rates of individual outcomes and between group comparisons are available in table 2. Of psychiatric noncases, 19.9% reported an adult outcome, suggesting that it is not rare to experience one of these indicators (see figure 1a). This compared to 41.5% of participants who were subthreshold cases only and 59.5% of psychiatric cases. Both subthreshold and psychiatric cases were significantly more likely to report an adult indicator as compared to noncases, and psychiatric cases had higher levels than subthreshold cases. A similar pattern was observed for the likelihood of having 2 or more indicators. Psychiatric and subthreshold cases made up close to 80% of participants with an adult indicator and close to 90% of participants with 2 or more such indicators (figures 1b and c).
Table 2.
Prevalence and unadjusted associations between childhood diagnostic groups and young adult outcomes.
| Noncases | Subthreshold cases |
Psychiatric cases |
Cases vs. Noncases | Impair. only vs. Noncases | Cases vs. Impair. only | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | % | % | OR | CI | p | OR | CI | p | OR | CI | p | |
| Any outcome | 19.9 | 41.9 | 59.5 | 5.9 | 3.6–9.7 | <0.001 | 2.9 | 1.8–4.8 | <0.001 | 2.0 | 1.3—3.2 | 0.002 |
| Multiple outcomes | 5.6 | 23.2 | 34.2 | 8.7 | 4.3–17.8 | <0.001 | 5.1 | 2.4–10.7 | <0.001 | 1.7 | 1.0–2.9 | 0.04 |
| Health | ||||||||||||
| Multiple psychiatric | 1.9 | 1.6 | 10.0 | 5.8 | 1.7–20.3 | 0.006 | 0.9 | 0.2–4.5 | 0.86 | 6.8 | 1.8–25.5 | 0.005 |
| Multiple addictions | 1.6 | 5.4 | 11.1 | 7.8 | 2.0–30.4 | 0.003 | 3.5 | 0.8–14.9 | 0.09 | 2.2 | 0.9–5.4 | 0.08 |
| Suicidality | 4.3 | 6.6 | 11.9 | 3.0 | 1.2–7.8 | 0.02 | 1.6 | 0.6–4.5 | 0.40 | 1.9 | 0.8–4.7 | 0.16 |
| Serious physical event | 2.1 | 1.1 | 8.4 | 4.2 | 1.4–12.8 | 0.01 | 0.5 | 0.2–1.5 | 0.21 | 8.5 | 3.8–18.6 | <0.001 |
| Legal | ||||||||||||
| Serious criminality | 2.9 | 10.6 | 12.2 | 4.7 | 1.9–12.1 | 0.001 | 4.1 | 1.5–10.9 | 0.006 | 1.2 | 0.6–2.2 | 0.64 |
| Incarceration | 0.4 | 5.3 | 5.3 | 13.8 | 5.2–36.6 | <0.001 | 13.5 | 4.7–38.9 | <0.001 | 1.0 | 0.4–2.4 | 0.97 |
| Financial | ||||||||||||
| High School dropout | 3.4 | 19.4 | 18.0 | 6.2 | 2.7–14.0 | <0.001 | 6.8 | 2.9–15.5 | <0.001 | 0.9 | 0.5–1.6 | 0.75 |
| Unable to keep job | 1.9 | 8.6 | 11.4 | 6.5 | 2.0–21.6 | 0.002 | 4.8 | 1.4–16.7 | 0.01 | 1.4 | 0.6–2.9 | 0.43 |
| Residential Instability | 1.4 | 4.8 | 11.7 | 9.4 | 2.8–31.6 | <0.001 | 3.6 | 0.9–13.9 | 0.06 | 2.6 | 1.0–6.7 | 0.04 |
| Social | ||||||||||||
| Early parenthood | 1.6 | 5.6 | 8.2 | 5.7 | 1.6–19.7 | 0.006 | 3.7 | 1.0–13.9 | 0.05 | 1.5 | 0.6–3.9 | 0.38 |
| No social support | 1.0 | 2.1 | 7.4 | 7.9 | 1.5–40.3 | 0.01 | 2.1 | 0.4–11.9 | 0.40 | 3.7 | 1.2–11.6 | 0.02 |
| Relational instability | 4.0 | 3.5 | 7.9 | 2.1 | 0.8–5.4 | 0.14 | 0.9 | 0.3–2.6 | 0.80 | 2.4 | 1.0–6.0 | 0.06 |
All percentages are weighted. Bolded values are significant at Bonferroni corrected alpha level (0.05/12=0.004).
Figure 1. Associations between adult outcomes and childhood diagnostic groups.
Legend: Figure 1A shows the likelihood of having either any outcome or more than one outcome based upon childhood psychiatric status. Figure 1b looks at all those with a key outcome and what portion is accounted for by each diagnostic group. Figure 2c looks at the all those with more than one outcome and what portion is accounted for by each diagnostic group.
All models were retested accounting for sex, race, low SES, family dysfunction, family instability, maltreatment, adult psychiatric status, and adult subthreshold status. Table 3 shows the associations in these adjusted models. Both psychiatric and subthreshold cases continued to predict greater risk for having an adult outcome or having 2 or more such outcomes in models adjusted for other psychosocial risk factors. Low childhood SES, adult psychiatric functioning and adult symptomatic impairment were significant covariates in each of these models.
Table 3.
Adjusted associations between childhood diagnostic groups and young adult outcomes.
| Cases vs. Noncases | Impair. only vs. Noncases | Cases vs. Impair. only | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p value | Sig. Covariates |
OR | 95% CI | p value | Sig. Covariates |
OR | 95% CI | p value | Sig. Covariates |
|
| Any outcome | 3.1 | 1.7–5.5 | <0.001 | 2,6,7 | 1.9 | 1.1–3.3 | 0.03 | 2,6,7 | 1.6 | 0.9–2.6 | 0.09 | 2,5,6,7 |
| Multiple outcomes | 3.8 | 1.8–8.2 | <0.001 | 2, 5,6,7 | 3.2 | 1.5–6.9 | 0.003 | 2,5,6,7 | 1.2 | 0.7–2.1 | 0.56 | 2,5,6,7 |
| Health | ||||||||||||
| Multiple psychiatric* | 3.3 | 1.1–10.1 | 0.04 | 1,4,7 | 0.5 | 0.1–3.2 | 0.45 | 1,4,7 | 6.0 | 1.7–20.9 | 0.006 | 4,7 |
| Multiple addictions | 5.1 | 1.3–19.7 | 0.02 | 1,6,7 | 2.7 | 0.7–11.1 | 0.17 | 1,6,7 | 1.8 | 0.7–15.4 | 0.21 | 1,6,7 |
| Suicidality | 1.8 | 0.6–5.4 | 0.27 | 6 | 1.2– | 0.4–3.3 | 0.76 | 6 | 1.4 | 0.5–4.0 | 0.48 | 6 |
| Serious physical event | 2.1 | 0.6–6.9 | 0.22 | 6 | 0.3 | 0.1–1.1 | 0.08 | 6 | 8.2 | 3.4–19.8 | <0.001 | 2,6 |
| Legal | ||||||||||||
| Serious criminality | 2.4 | 0.9–6.5 | 0.09 | 1,2 | 2.4 | 0.8–7.0 | 0.11 | 1,2 | 0.9 | 0.5–1.9 | 0.86 | 1,2 |
| Incarceration | 4.7 | 1.4–16.2 | 0.01 | 1,2 | 6.2 | 2.2–17.2 | <0.001 | 1,2 | 0.8 | 0.3–2.0 | 0.58 | 1,2 |
| Financial | ||||||||||||
| High School dropout | 2.1 | 0.8–5.2 | 0.13 | 1,2,3,5 | 3.6 | 1.5–8.9 | 0.005 | 1,2,3,5 | 0.6 | 0.3–1.0 | 0.07 | 1,2,5 |
| Unable to keep job | 4.2 | 1.3–13.7 | 0.02 | 7 | 3.7 | 1.1–12.7 | 0.04 | 7 | 1.1 | 0.5–2.5 | 0.82 | 7 |
| Residential instability | 10.0 | 2.8–35.5 | <0.001 | 3.8 | 1.0–14.8 | 0.05 | 2.6 | 1.1–6.5 | 0.04 | |||
| Social | ||||||||||||
| Early parenthood | 3.4 | 0.8–14.8 | 0.09 | 1,5 | 3.0 | 0.7–14.0 | 0.16 | 1,5 | 1.2 | 0.5–3.1 | 0.65 | 1 |
| No social support | 3.3 | 0.8–13.6 | 0.10 | 4,7 | 1.1 | 0.2–5.0 | 0.95 | 4,7 | 2.8 | 0.9–8.8 | 0.07 | 4,7 |
| Relational instability | 2.0 | 0.7–5.7 | 0.18 | 1 | 0.9 | 0.3–2.5 | 0.79 | 1 | 2.2 | 0.9–5.6 | 0.09 | 1,6 |
Adjusted analysis controlled for all covariates except adult psychiatric status. Bolded values are significant at p<0.05 and met the Bonferroni adjusted alpha levels in unadjusted associations. Covariates: 1=Sex; 2 = Low SES; 3 = Family instability; 4 = Family dysfunction; 5 = Maltreatment; 6 = adult psychiatric problem; 7 = adult subthreshold problems.
Specificity and cumulative burden
Adult outcomes may be accounted for by specific childhood disorders or one’s cumulative psychiatric burden. Supplemental table 3 shows associations between specific childhood disorders and having an adverse outcome. In adjusted models, childhood depression and conduct disorder were associated with a higher likelihood of having an adverse outcome, and only conduct disorder predicted having 2 or more adverse outcomes.
Of the total 527 childhood psychiatric cases followed into adulthood, 268 had only one childhood/adolescent disorder, 135 had 2 childhood diagnoses and 125 had 3 or more childhood diagnoses. Supplemental figure 1 shows the likelihood of having an adult outcome based upon the total number of childhood diagnoses. This linear cumulative burden variable predicted having any adult outcome (OR= 1.5, 95%CI 1.3–1.9, p<0.001) and having 2 or more such outcomes (OR= 1.5, 95%CI 1.2–1.8, p<0.001) in models adjusted for other childhood adversities. In a final model, which included both the individual psychiatric disorders as well as the cumulative burden variable, only the cumulative burden variable predicted having an outcome (OR= 1.8, 95%CI 1.1–3.0, p=0.01) or having more than one outcome (OR= 2.2, 95%CI 1.3–3.8, p=0.005).
Discussion
The adult outcomes examined here – educational failure, criminality, addiction, suicidality, teenage parenthood, mental and physical health problems, untimely death, and social isolation – are the focus of considerable public policy efforts. Only about 1 in 5 individuals without a history of childhood psychiatric problems reported such an adverse outcome. This rate increased to 6 in 10, however, for those that met criteria for a common childhood psychiatric disorder. This risk persisted when accounting for childhood psychosocial adversities such as maltreatment that have long been linked with both childhood psychiatric disorder and disrupted development (e.g.,29). Most importantly, this risk was evident even after accounting for adult psychiatric diagnostic and subthreshold problems suggesting that there are long-term effects of childhood problems that are independent of current psychiatric status..
It is not surprising that those with a history of childhood psychiatric problems continue to display continued impairment into adulthood8–11, particularly given what is known about the continuity of psychiatric problems across development2, 4, 6. What is surprising and novel is that these long-term effects are evident even after statistically controlling for childhood adversities and adult psychiatric functioning. Additional strengths of the current study include the following features: it followed children prospectively and assessed a broad range of childhood psychiatric problems; it included subthreshold cases that made up 31% of the population and are typically ignored in the diagnostic literature; the prospective design controlled for a range of early adversities that have strong associations with childhood and adult psychiatric functioning, so the effects identified here are independent of such preexisting factors; and it focused on a limited set of serious functional outcomes.
The adverse long-term outcomes were not limited to those meeting full criteria for a childhood diagnosis. Subthreshold cases had 3 times higher odds of having an adult outcome and 5 time higher odds of 2 or more such outcomes as compared to those with no psychiatric history. We have previously argued that our diagnostic system needs to find a means to accommodate such individuals as they make up a significant proportion of children seeking treatment14, 15. Such efforts need not require diluting the threshold for mental health problems or mislabeling normal distress30Moderately-impairing physical health concerns often require clinical attention, and psychiatric problems are no different. This study suggests that recognizing subthreshold cases needs to be a public health priority and that intervention with these individuals may forestall future impairments, distress, and societal costs12.
Specific individual disorders did not predict adverse adult outcomes after accounting for cumulative psychiatric dose or burden. The initial specificity analysis identified a pattern of associations that were largely consistent with existing long-term outcomes studies of depression31, 32 and conduct disorder33, 34. These specific effects of depression and conduct disorder, however, were attenuated in models accounting for cumulative exposure. This cumulative burden variable may indicate comorbidity, severity of psychiatric problems, persistence of psychiatric disorders or all three35. For the purpose of estimating adult functioning a single dimension of overall childhood psychiatric risk may be more useful than the less parsimonious DSM approach16, 36.
Caveats
The Great Smoky Mountains study has many strengths but it is not representative of the U.S. population. Childhood cases may have been missed if participants met criteria prior to study involvement, between assessments, or after their last assessment. If this is the case, these analyses may underestimate the number of children affected by psychiatric illness and the adult burden of childhood psychiatric illness. Similarly, adult functioning was only assessed 3 times between ages 19 and 26. Adverse physical health effects may not be evident until later in life. The study design does not allow for definite conclusions about causal effects as unmeasured factors may account for observed associations. Many adult outcomes studied are related to individual symptoms of antisocial personality disorder, although associations persisted in analyses accounting for adult psychiatric status including antisocial personality disorder. Finally, while the CAPA interview has been the subject of extensive validity analyses24, 25, the upward extension has not been studied independently.
Common childhood psychiatric disorders are costly37, impairing38, and often a source of great distress for the child and burden to others. Over the course of childhood many if not most will experience impairing psychiatric problems3. These common early disorders are often associated with a disrupted transition to adulthood even if the psychiatric problems do not persist into adulthood and even if the problems do not meet full criteria for a psychiatric disorder. And, with each additional exposure to childhood psychiatric problems, the prognosis becomes more dire. If the goal of public health efforts is to increase opportunity and optimal outcomes, and to reduce distress, then there may be no better target than the reduction of childhood psychiatric distress – including both at the clinical and subthreshold levels.
Supplementary Material
Acknowledgements
The work presented here was supported by the National Institute of Mental Health (MH080230, MH63970, MH63671, MH48085, MH075766, MH094605), the National Institute on Drug Abuse (DA/MH11301, DA011301, DA016977, DA011301, DA036523), NARSAD (Early Career Award to WEC), and the William T Grant Foundation.
None of the funding organizations had any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. Dr. Copeland had full access to all the data in the study, performed all statistical analyses, and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Financial Disclosures
None of the authors has biomedical financial interests or potential conflicts of interest.
Contributor Information
William E. Copeland, Department of Psychiatry and Behavioral Sciences at Duke University Medical Center.
Dieter Wolke, Email: D.Wolke@warwick.ac.uk, Department of Psychology and Division of Mental Health and Wellbeing at the University of Warwick.
Lilly Shanahan, Email: lilly_shanahan@unc.edu, Department of Psychology at the University of North Carolina, Chapel Hill.
E. Jane Costello, Email: elizabeth.costello@duke.edu, Department of Psychiatry and Behavioral Sciences at Duke University Medical Center.
References
- 1.Harhay MO, King CH. Global burden of disease in young people aged 10–24 years. The Lancet. 2012;379(9810):27–28. doi: 10.1016/S0140-6736(12)60019-1. [DOI] [PubMed] [Google Scholar]
- 2.Kim-Cohen J, Caspi A, Moffitt T, Harrington H, Milne B, Poulton R. Prior juvenile diagnoses in adults with mental disorder: Developmental follow-back of a prospective-longitudinal cohort. Archives of General Psychiatry. 2003;60:709–717. doi: 10.1001/archpsyc.60.7.709. [DOI] [PubMed] [Google Scholar]
- 3.Copeland W, Shanahan L, Costello EJ, Angold A. Cumulative Prevalence of Psychiatric Disorders by Young Adulthood: A Prospective Cohort Analysis From the Great Smoky Mountains Study. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50(3):252–261. doi: 10.1016/j.jaac.2010.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005 Jun 1;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. 2005. [DOI] [PubMed] [Google Scholar]
- 5.Costello EJ, Angold A, Keeler GP. Adolescent outcomes of childhood disorders: The consequences of severity and impairment. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:121–128. doi: 10.1097/00004583-199902000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Copeland WE, Shanahan L, Costello EJ, Angold A. Childhood and Adolescent Psychiatric Disorders as Predictors of Young Adult Disorders. Arch Gen Psychiatry. 2009;66(7):764–772. doi: 10.1001/archgenpsychiatry.2009.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roisman GI, Masten AS, Coatsworth JD, Tellegen A. Salient and emerging developmental tasks in the transition to adulthood. Child Dev. 2004 Jan-Feb;75(1):123–133. doi: 10.1111/j.1467-8624.2004.00658.x. [DOI] [PubMed] [Google Scholar]
- 8.Goodman A, Joyce R, Smith JP. The long shadow cast by childhood physical and mental problems on adult life. Proceedings of the National Academy of Sciences. 2011;108(15):6032–6037. doi: 10.1073/pnas.1016970108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fergusson DM, John Horwood L, Ridder EM. Show me the child at seven: the consequences of conduct problems in childhood for psychosocial functioning in adulthood. Journal of Child Psychology and Psychiatry. 2005;46(8):837–849. doi: 10.1111/j.1469-7610.2004.00387.x. [DOI] [PubMed] [Google Scholar]
- 10.Copeland WE, Angold A, Shanahan L, Costello EJ. Longitudinal Patterns of Anxiety From Childhood to Adulthood: The Great Smoky Mountains Study. Journal of the American Academy of Child & Adolescent Psychiatry. 2013 doi: 10.1016/j.jaac.2013.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mannuzza S, Klein RG. Long-term prognosis in attention-deficit/hyperactivity disorder. 2000;9(3):711–726. 2000/07// [PubMed] [Google Scholar]
- 12.Angold A, Costello EJ, Farmer EMZ, Burns BJ, Erkanli A. Impaired but undiagnosed. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:129–137. doi: 10.1097/00004583-199902000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Lewinsohn PM, Shankman SA, Gau JM, Klein DN. The prevalence of comorbidity of subthreshold psychiatric conditions. Psychological Medicine. 2004;34:613–622. doi: 10.1017/S0033291703001466. [DOI] [PubMed] [Google Scholar]
- 14.Costello EJ, Shugart MA. Above and below the threshold: Severity of psychiatric symptoms and functional impairment in a pediatric sample. Pediatrics. 1992 Sep 3;90:359–368. [PubMed] [Google Scholar]
- 15.Angold A, Erkanli A, Farmer E, et al. Psychiatric disorder, impairment, and service use in rural African American and White youth. Archives of General Psychiatry. 2002;59:893–901. doi: 10.1001/archpsyc.59.10.893. [DOI] [PubMed] [Google Scholar]
- 16.Caspi A, Houts RM, Belsky DW, et al. The p Factor: One General Psychopathology Factor in the Structure of Psychiatric Disorders? Clinical Psychological Science. 2013 Aug 14; doi: 10.1177/2167702613497473. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lahey BB, Rathouz PJ, Hulle C, et al. Testing Structural Models of DSM-IV Symptoms of Common Forms of Child and Adolescent Psychopathology. Journal of Abnormal Child Psychology. 2008;36(2):187–206. doi: 10.1007/s10802-007-9169-5. [DOI] [PubMed] [Google Scholar]
- 18.Sterba S, Copeland W, Egger H, Costello E, Erkanli A, Angold A. Longitudinal dimensionality of adolescent psychopathology: Testing the differentiation hypothesis. Journal of Child Psychology and Psychiatry. 2010;51(8):871–884. doi: 10.1111/j.1469-7610.2010.02234.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krueger R, Caspi A, Moffitt T, Silva P. The structure and stability of common mental disorders (DSM-III-R): A longitudinal--epidemiological study. Journal of Abnormal Psychology. 1998 May;107(2):216–227. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- 20.Kendler KS, Walters EE, Neale MC, Kessler RC, Heath AC, Eaves LJ. The structure of the genetic and environmental risk factors for six major psychiatric disorders in women. Phobia, generalized anxiety disorder, panic disorder, bulimia, major depression, and alcoholism. Archives of General Psychiatry. 1995;52(2):374–383. doi: 10.1001/archpsyc.1995.03950170048007. [DOI] [PubMed] [Google Scholar]
- 21.Kendler KS, Davis CG, Kessler RC. The familial aggregation of common psychiatric and substance use disorders in the National Comorbidity Survey: a family history study. British Journal of Psychiatry. 1997;170:541–548. doi: 10.1192/bjp.170.6.541. [DOI] [PubMed] [Google Scholar]
- 22.Copeland WE, Adair CE, Smetanin P, et al. Diagnostic transitions from childhood to adolescence to early adulthood. Journal of Child Psychology and Psychiatry. 2013 doi: 10.1111/jcpp.12062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- 24.Angold A, Costello EJ. The Child and Adolescent Psychiatric Assessment (CAPA) Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:39–48. doi: 10.1097/00004583-200001000-00015. [DOI] [PubMed] [Google Scholar]
- 25.Angold A, Costello EJ. A test-retest reliability study of child-reported psychiatric symptoms and diagnoses using the Child and Adolescent Psychiatric Assessment (CAPA-C) Psychological Medicine. 1995;25:755–762. doi: 10.1017/s0033291700034991. [DOI] [PubMed] [Google Scholar]
- 26.Angold A, Prendergast M, Cox A, Harrington R, Simonoff E, Rutter M. The Child and Adolescent Psychiatric Assessment (CAPA) Psychological Medicine. 1995;25:739–753. doi: 10.1017/s003329170003498x. [DOI] [PubMed] [Google Scholar]
- 27.Copeland W, Wolke D, Angold A, Costello E. Adult psychiatric outcomes of bullying and being bullied by peers in childhood and adolescence. JAMA Psychiatry. 2013:1–8. doi: 10.1001/jamapsychiatry.2013.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Angold A, Cox A, Prendergast M, et al. The Young Adult Psychiatric Assessment (YAPA) Durham, NC: Duke University Medical Center; 1999. [Google Scholar]
- 29.Herrenkohl EC, Herrenkohl RC, Rupert LJ, Egolf BP, Gary LJ. Risk factors for behavioral dysfunction: The relative impact of maltreatment, SES, physical health problems, cognitive ability, and quality of parent-child interaction. Child Abuse and Neglect. 1995;19(2):191–203. doi: 10.1016/0145-2134(94)00116-c. [DOI] [PubMed] [Google Scholar]
- 30.Parker G. Is depression overdiagnosed? Yes. BMJ. 2007 Aug 18;335(7615):328. doi: 10.1136/bmj.39268.475799.AD. 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fergusson DM, Woodward LJ. Mental health, educational, and social role outcomes of adolescents with depression. Archives of General Psychiatry. 2002;59:225–231. doi: 10.1001/archpsyc.59.3.225. [DOI] [PubMed] [Google Scholar]
- 32.Colman I, Wadsworth MEJ, Croudace TJ, Jones PB. Forty-Year Psychiatric Outcomes Following Assessment for Internalizing Disorder in Adolescence. Am J Psychiatry. 2007 Jan 1;164(1):126–133. doi: 10.1176/ajp.2007.164.1.126. 2007. [DOI] [PubMed] [Google Scholar]
- 33.Fergusson D, Woodward L. Educational, psychosocial, and sexual outcomes of girls with conduct problems in early adolescence. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2000;41(6):779–792. [PubMed] [Google Scholar]
- 34.Fergusson D, Lynskey M. Conduct problems in childhood and psychosocial outcomes in young adulthood: A Prospective Study. Journal of Emotional and Behavioral Disorders. 1998;6(1):2–18. [Google Scholar]
- 35.Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40:57–87. [PubMed] [Google Scholar]
- 36.Association AP. Diagnostic and statistical manual of mental disorders fifth edition (DSM-5) American Psychiatric Association, Arlington. 2013 [Google Scholar]
- 37.Costello EJ, Copeland W, Cowell A, Keeler G. Service Costs of Caring for Adolescents With Mental Illness in a Rural Community, 1993–2000. American Journal of Psychiatry. 2007;164(1):36. doi: 10.1176/appi.ajp.2007.164.9.A36. [DOI] [PubMed] [Google Scholar]
- 38.Costello EJ, Angold A, Burns BJ, Erkanli A, Stangl DK, Tweed DL. The Great Smoky Mountains Study of Youth: Functional impairment and severe emotional disturbance. Archives of General Psychiatry. 1996;53(12):1137–1143. doi: 10.1001/archpsyc.1996.01830120077013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.