Abstract
Paradoxical manifestation is worsening of pre-existing tuberculous lesion or appearance of new lesions in patients whose condition initially improved with antituberculous treatment. Our hypothesis was that paradoxical manifestation in non-HIV tuberculous meningitis (TBM) patients was underestimated and this could contribute to patients’ prognosis. This was the first systemic study of paradoxical manifestation in HIV-negative TBM patients.
Between 2009 and 2014, TBM patients were studied prospectively in 2 hospitals. Clinical features, cerebrospinal fluid, and radiological findings were monitored. Paradoxical manifestation was divided into definite (4 weeks or more) and probable (between 14 and 27 d) after commencement of antituberculous treatment.
Forty-one non-HIV TBM patients were recruited. Definite paradoxical manifestation occurred in 23/41 (56%) of the patients. Time to onset of paradoxical manifestation was between 28 days and 9 months, and majority was between 28 and 50 days.
Neuroimaging manifestation in the brain (22/41 patients, 54%) and clinical manifestation (22/41 patients, 54%) were most commonly seen, followed by cerebrospinal fluid manifestation (7/41 patients, 17%). Neuroimaging changes most commonly seen were worsening of leptomeningeal enhancement, new infarcts, new tuberculomas, and enlargement of tuberculoma. Initial Computed Tomography Angiography/magnetic resonance angiography brain showed vasculitis in 14 patients, with 2 (12.5%) showing paradoxical vasculitis during follow-up.
Recurrence of the paradoxical manifestation was seen in 7/23 (30%) of the patients. More than half (14/23, 61%) of the patients improved, 6 (26%) patients died, and 3 (13%) patients had persistent neurological deficit.
Paradoxical manifestation was very common in non-HIV TBM patients. Neuroimaging paradoxical manifestation of 2-4 weeks may not be paradoxical manifestation but could be delayed treatment response.
INTRODUCTION
Tuberculosis (TB) results in serious morbidity and mortality.1 Among the patients with tuberculosis, 4% have tuberculous meningitis (TBM).2 Despite treatment with antituberculous drugs, TBM patients can have worsening of condition.3 This phenomenon is described as paradoxical manifestation.3
The paradoxical manifestation is described as the worsening of pre-existing tuberculous lesions or the appearance of new tuberculous lesions in patients whose clinical symptoms initially improved with antituberculosis treatment in HIV-negative patients.3 There are limited reports of large series of non-HIV paradoxical reaction in TBM in the literature, the only one being that of Sütlas et al,4 involving 61 patients from Turkey.
Our hypothesis was that the frequency of worsening of clinical condition of HIV-negative patients with TBM after commencement of treatment of the disease (paradoxical manifestation) was underestimated. We also hypothesized that this delayed worsening is important and can also contribute to patients’ prognosis.
METHODOLOGY
This was a cohort follow-up study on patients with TBM, with prospective follow-up and prospective inclusion of new cases.
Patient Selection
Between 2009 and 2014, we prospectively recruited TBM patients at the University Malaya Medical Centre (UMMC) and Kuala Lumpur General Hospital, Kuala Lumpur, Malaysia—2 large public hospitals in central peninsular Malaysia.
The study was approved by the Institutional Ethics Committee of UMMC and Ministry of Health in Malaysia. All patients or their legally acceptable representatives provided informed consent for the study.
One TBM patient with multidrug resistance and 2 patients who were not compliant to antituberculous therapy were excluded from the study. Noncompliant patients were those who did not adhere to antituberculous treatment prescribed by doctors. These patients did not take anti-TB medications daily and regularly.
We collected information on demographic characteristics, clinical features on admission to hospital, radiological results, treatment, clinical course, and outcome.
Tuberculous meningitis was classified as “definite” if cerebrospinal fluid (CSF) acid-fast bacilli (AFB) direct smear, or mycobacterial culture or polymerase chain reaction (PCR) for mycobacteria tuberculosis, or histopathological findings were positive. TBM was termed as “probable” when patients had one or more of the following features: suspected active pulmonary tuberculosis (PTB) on chest X-ray, AFB in body specimens (apart from CSF), and other extrapulmonary TB.5
Tuberculous meningitis was classified as “possible” in patients with ≥4 of the following features: duration of illness for >5 days, raised CSF white cell count, CSF lymphocyte predominance, CSF glucose/plasma glucose ratio of <0.5, turbid CSF, absence of Cryptococcus in CSF, altered consciousness, focal neurological deficit, or response to antituberculous therapy.5
We graded the severity of meningitis at the time of admission to hospital. Patients in stage 1 were fully conscious and rational, with meningeal signs, but no focal neurologic deficits. Patients in stage 2 had altered mentation or focal neurologic deficits. Patients in stage 3 had either deep stupor or delirium or complete hemiplegia or paraplegia.6
All the TBM patients recruited received adequate treatment with first-line antituberculous medications comprising of intensive phase (ethambutol, isoniazid, rifampicin, and pyrazinamide) for 2 months followed by maintenance phase (isoniazid, rifampicin). The total duration of antituberculous therapy was 12 to 18 months. The treatment regimen was based on British Infection Society guidelines.7 All the patients had supervised therapy during hospitalization. They received the antituberculous drugs under intermittent directly supervised therapy (DOTS) while on outpatients’ follow-up.8 They were all compliant to treatment.
Methods
The radiological information on admission was recorded. The magnetic resonance imaging (MRI) of the brain was performed with 3.0-Tesla Signa HDx MR system (GE Healthcare). T1-weighted image (T1W), T2-weighted image (T2W), T2 fluid-attenuated inversion recovery (T2 FLAIR), and diffusion-weighted image (DWI), apparent diffusion (ADC), and magnetic resonance angiography (MRA) sequences were obtained. MRI T1 with gadolinium contrast was performed. Serial computed tomography (CT) brain and MRI brain was done. Follow-up MRI was done 1 to 2 months after initiation of antituberculous treatment and also during the time of clinical deterioration.
Paradoxical manifestation was divided into “definite,” where the onset of deterioration was 4 weeks and more after commencement of antituberculous treatment; and “probable,” where the onset of deterioration was between 14 and 27 days after commencement of antituberculous treatment. Paradoxical manifestation was divided into definite and probable paradoxical manifestation according to the definition by Carvalho et al.9 According to Carvalho et al, paradoxical manifestation was defined as clinical/radiological worsening of previous tuberculous lesions or development of new lesions after at least 1 month of antituberculous treatment in patients who initially responded to anti-TB therapy.9 In addition, most patients who deteriorated at 2 to 4 weeks were likely due to delayed treatment response.
The presence of paradoxical manifestation was divided into paradoxical clinical manifestation, paradoxical CSF manifestation, and paradoxical neuroimaging changes. In terms of paradoxical clinical manifestation, clinical deterioration was evaluated. Follow-up clinical changes were recorded for all the patients from time of admission to 2014.
Paradoxical CSF abnormalities were categorized as increased CSF pleocytosis, shift towards polymorphonuclear pleocytosis, reduced CSF glucose, and increased CSF protein.
In addition, the presence of paradoxical neuroimaging features such as worsening hydrocephalus, worsening leptomeningeal enhancement, new/enlarging tuberculoma, new infarcts, and worsening paradoxical angiographic abnormalities were recorded. Worsening hydrocephalus was defined as progression of mild hydrocephalus to moderate/severe hydrocephalus. Worsening leptomeningeal enhancement was defined as leptomeningeal enhancement that became thicker and more dense. In addition, worsening leptomeningeal enhancement included formation of new leptomeningeal enhancement at other areas of the brain.
New tuberculoma was defined as formation of new cerebral tuberculous lesion or lesions (tuberculoma). Enlarging tuberculoma was defined as increase in size of pre-existing tuberculoma. Presence of new infarct was defined as presence of new stroke (cerebral infarction) at a particular part of the brain, not present in previous brain scan/imaging. Angiographic abnormalities consist of vasculitis and vasospasm. Worsening paradoxical angiographic abnormalities was defined as worsening of pre-existing vasculitis/vasospasm or presence of new vasculitis/vasospasm.
Recurrence of paradoxical manifestation was defined as occurrence of new clinical or radiological manifestation a month or longer after the previous paradoxical event. The time to development of each paradoxical manifestation was documented. Treatment with dexamethasone was also recorded.
The patients were monitored at regular intervals by clinical, CSF parameters, and serial neuroimaging results. In addition to similar follow-up, they had lumbar puncture and MRI/CT brain done at regular intervals. Repeat CSF analysis was planned 1 month after initiation of antituberculous treatment and also during the time of clinical deterioration. Corticosteroid (dexamethasone) was administered to TBM patients who had severe TBM.
Statistical Analysis
All descriptive statistics were done using Statistical Package for Social Sciences, SPSS (Version 18.0, SPSS Inc., Chicago, IL). Chi-square test (or Fisher exact test) was used to analyze categorical data. Continuous variables were expressed as means and analyzed with Student t test. A P value of <0.05 (2-tailed P value) was considered as statistical significance.
RESULTS
Demography Characteristics of TBM Patients
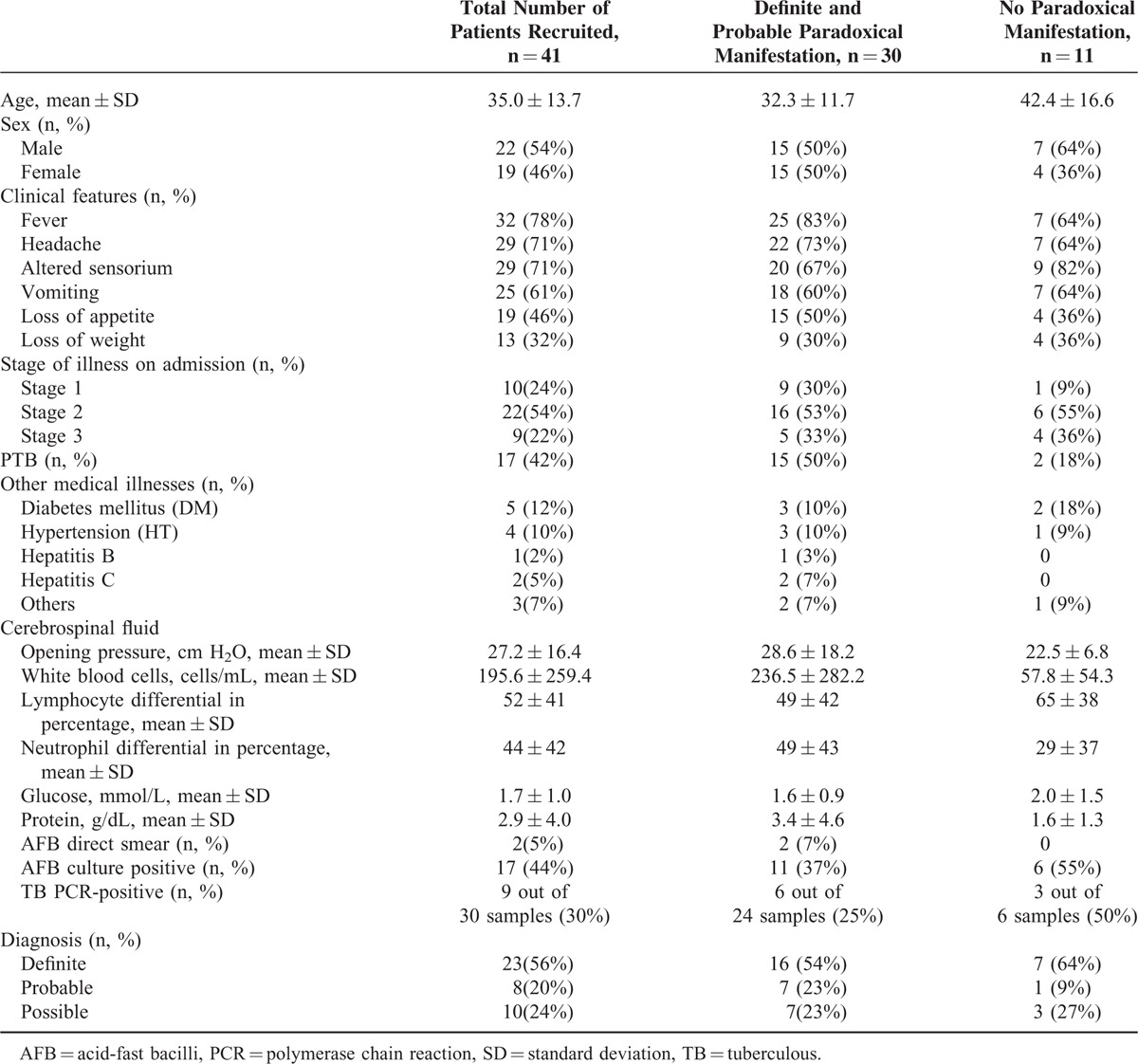
Forty-one patients with TBM admitted to UMMC and Hospital Kuala Lumpur from 2009 to 2015 were recruited (Table 1). CT scan of the brain was done for all the patients and MRI of the brain was done for 38 TBM patients (92.7%).
TABLE 1.
Baseline Characteristics and Cerebrospinal Fluid (CSF) Results of Tuberculous Meningitis Patients
Definite Paradoxical Manifestation of TBM Patients
Table 2 is the summary of the findings of the definite paradoxical manifestations, and Table 3 lists the details of these patients.
TABLE 2.
Summary of the Changes in the 23 Patients With Definite Paradoxical Manifestation
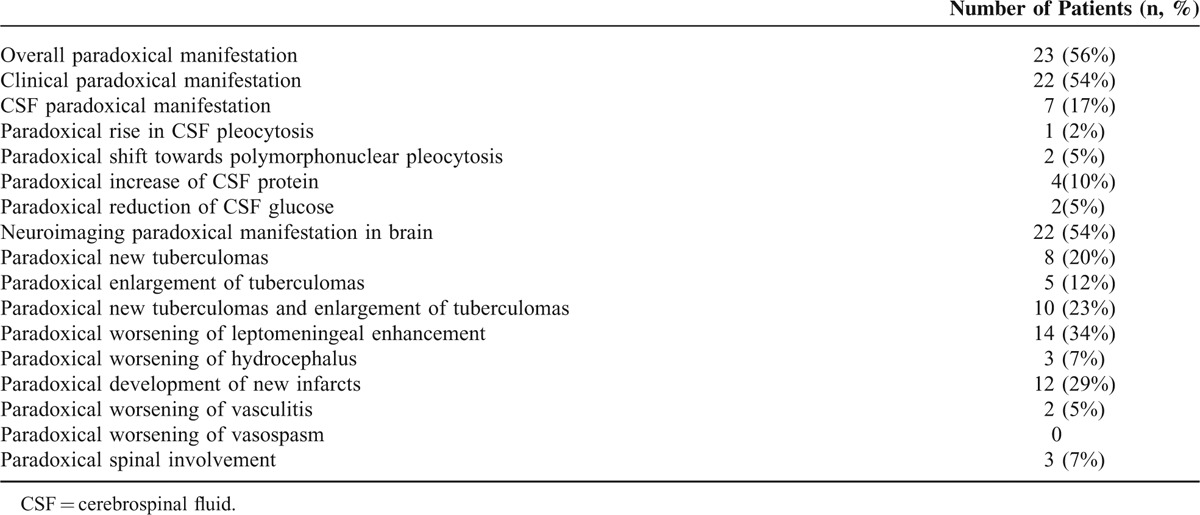
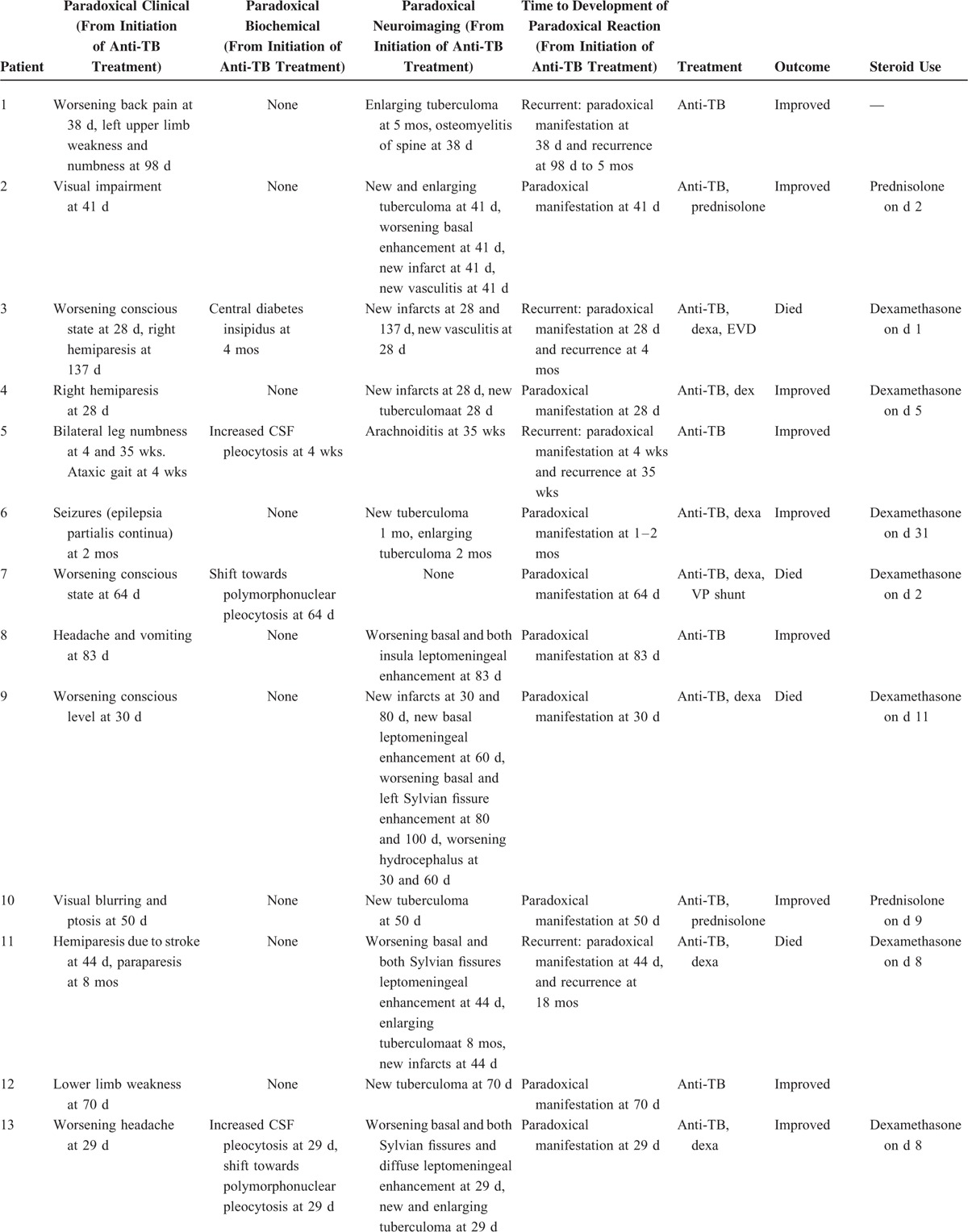
TABLE 3.
Clinical, CSF, and Imaging Details of the 23 Patients With Definite Paradoxical Manifestation in Study TBM Patients
As shown, paradoxical manifestation occurred in 23 (56%) TBM patients. Neuroimaging paradoxical manifestation in the brain and clinical paradoxical manifestation were more commonly seen compared with CSF paradoxical manifestation.
Neuroimaging changes most commonly seen were as follows: worsening leptomeningeal enhancement, new infarcts, new tuberculomas, and enlargement of tuberculoma. In terms of neuroimaging features, 22 patients (54%) had neuroimaging paradoxical manifestation in the brain. Worsening leptomeningeal enhancement while on antituberculous medication was observed in 14 patients (34%). One patient in our cohort had paradoxical manifestation of leptomeningeal enhancement at the optic chiasm.
Twelve patients (29%) had paradoxical development of new infarcts. The number of new infarcts in each patient varied from 1 to 3 infarcts. The time to development of new infarcts ranged from 28 days to 5 months.
Eight patients (20%) developed paradoxical new tuberculomas, and 5 patients (12%) had enlargement of tuberculoma during course of therapy. The appearance of new tuberculoma/s in our patients varied from 28 days to 5 months and the time to tuberculoma enlargement ranged from 28 days to 8 months. Three patients (7%) developed paradoxical worsening of hydrocephalus. The time to development of worsening of hydrocephalus ranged from 28 days to 5 months.
In our patients, MRA/Computed Tomography Angiography (CTA) was performed in 31 patients with TBM, with a follow-up angiography in 16 patients. Initial angiography revealed abnormalities in 17 (54.8%) patients (14 vasculitis, 3 vasospasm). Thus, 2/16 (12.5%) patients had paradoxical vasculitis and no patient had paradoxical vasospasm.
Paradoxical clinical manifestation was observed in 22 patients (54%). There were 5 patients (22%) with worsening conscious level, 5 patients (22%) with seizures, 4 patients (18%) with hemiparesis, 3 patients (13%) with headache, 2 patients (9%) with visual impairment, 2 patients (9%) with third cranial nerve palsy, and 1 patient (4%) each with back pain, sixth cranial nerve palsy, and ataxic gait.
The CSF paradoxical manifestation was observed in 7 patients (17%). The time to paradoxical increase of CSF protein and reduction of CSF glucose was 28 days to 7 months. Time to paradoxical shift towards polymorphonuclear pleocytosis was 28 to 64 days. Time to paradoxical rise in CSF pleocytosis was 28 to 29 days.
Paradoxical spinal involvement was observed in 3 patients (7%). There were 2 patients (5%) with leptomeningeal enhancement at spine, 1 patient (2%) with TB myelitis with spinal cord edema, and 1 patient (2%) with osteomyelitis of the spine. Time to paradoxical spinal involvement was 28 days to 35 weeks.
Seven out of 23 patients (30%) with paradoxical manifestation had recurrent paradoxical manifestation (Table 3 ).
Fourteen out of 23 patients (61%) with paradoxical manifestation improved, whereas 6 patients (26%) died and 3 patients (13%) had persistent neurological deficit. There was no significant difference in the outcome of 23 patients with definite paradoxical manifestation as compared with the other 18 patients. Neither was there significant difference in the severity of disease during presentation between the 2 groups.
Out of the 23 TBM patients with paradoxical manifestation, 17 patients (74%) were given corticosteroids. Among them, 8 (47%) improved clinically. However, 6 patients (35%) died and 3 patients (18%) had persistent neurological deficit.
Probable Paradoxical Reaction
Probable paradoxical manifestation occurred in 7 (17%) of the TBM patients. Paradoxical CSF changes were associated with worsening leptomeningeal enhancement in 3 patients (7%), worsening hydrocephalus in 2 patients (5%), and new infarcts, new vasculitis, worsening vasospasm, and pachygyri enhancement in 1 patient (2%) each.
There was a paradoxical development of tuberculoma at the optic chiasm in 1 patient, resulting in vision defect and impairment.
Out of the 7 TBM patients with probable paradoxical manifestation, 5 patients (71%) were given corticosteroids. Among them, 2 (40%) improved clinically and the other 3 patients (60%) died.
Differences Between TBM Patients who Have Definite Paradoxical Manifestation, Probable, and no Paradoxical Manifestation
There was statistical significance (Table 4) when comparing between TBM patients with definite, probable, and no paradoxical manifestation for clinical paradoxical manifestation (P < 0.0001), CSF paradoxical manifestation (P = 0.012), and neuroimaging paradoxical manifestation in the brain (P < 0.0001). The most obvious differences in the neuroimaging paradoxical manifestation in the brain were the more common worsening of leptomeningeal enhancement (P = 0.003), new infarcts (P = 0.006), and new tuberculoma (P = 0.037) in the definite cases.
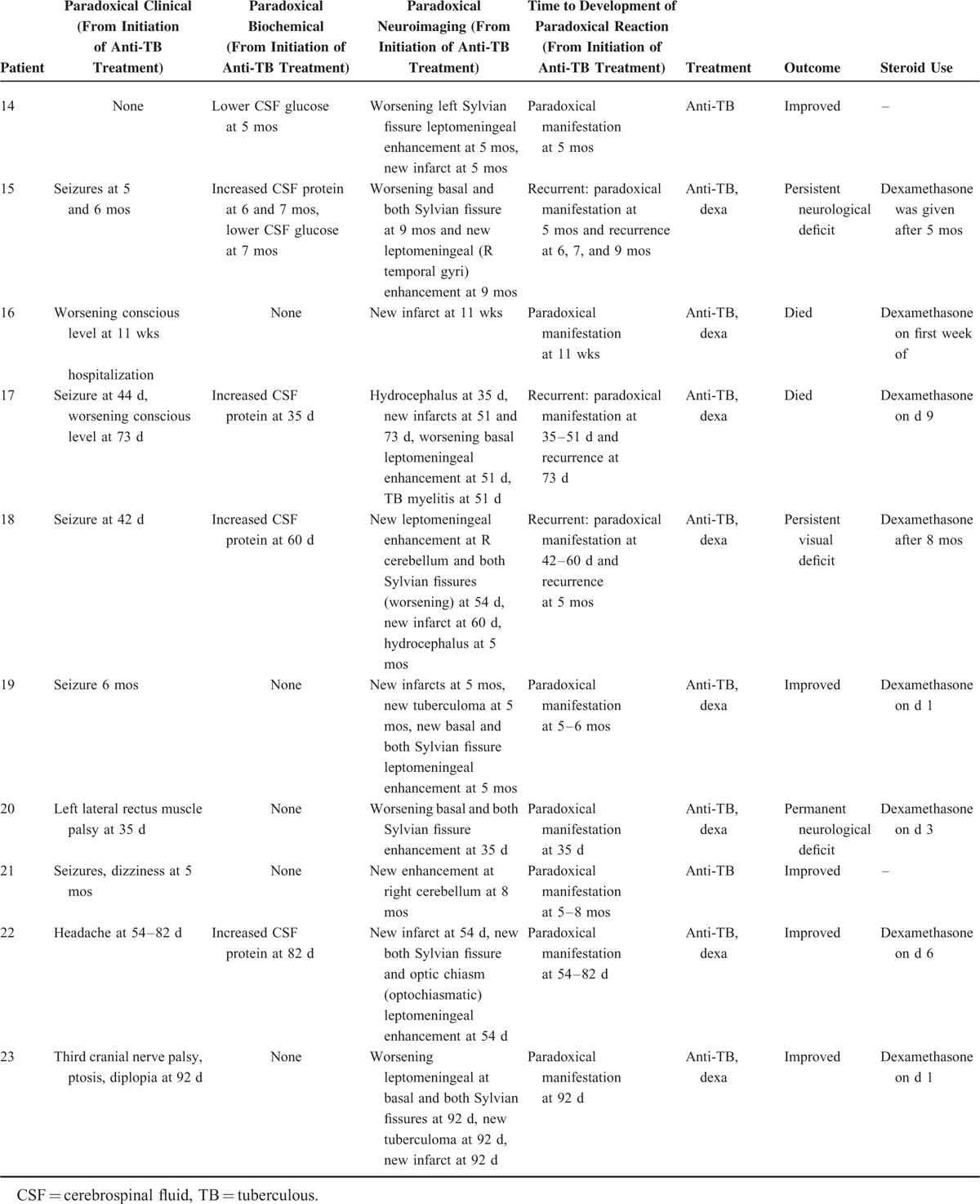
TABLE 3 (Continued).
Clinical, CSF, and Imaging Details of the 23 Patients With Definite Paradoxical Manifestation in Study TBM Patients
In our study, 14 patients (61%) with definite paradoxical manifestation improved, whereas 6 patients (55%) with no paradoxical manifestation improved.
In terms of management of paradoxical manifestation, antituberculous therapy was continued for a longer duration (18 months). Dexamethasone was given to TBM patients who had severe definite paradoxical manifestation. In patients who had worsening hydrocephalus resulting in severe hydrocephalus, they were referred to the neurosurgeon for insertion of extraventricular drainage (EVD).
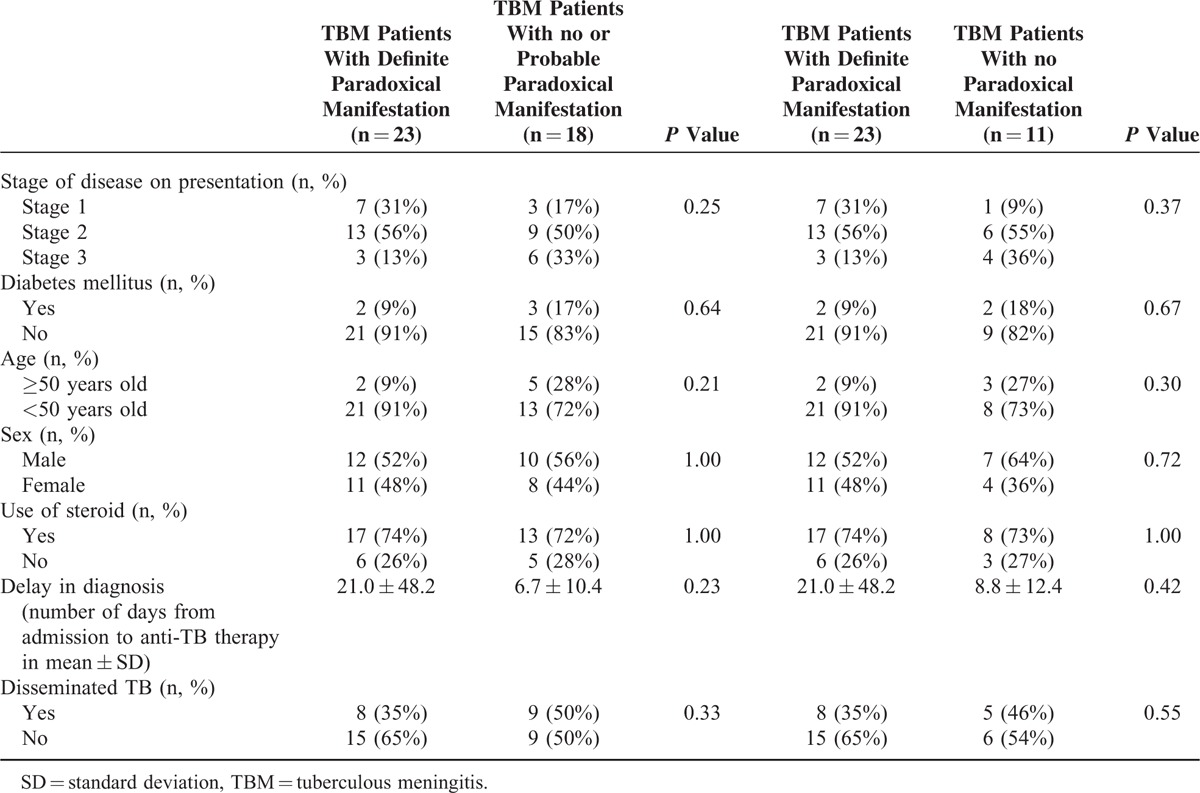
Determinants of Paradoxical Manifestation
Table 5 showed univariate analysis of determinants of paradoxical manifestations. However, there was no statistical significance with univariate analysis. Therefore, statistical analysis with multilogistic regression was not performed.
TABLE 4.
Differences Between TBM Patients With Definite Paradoxical Manifestation, Probable and no Paradoxical Manifestation
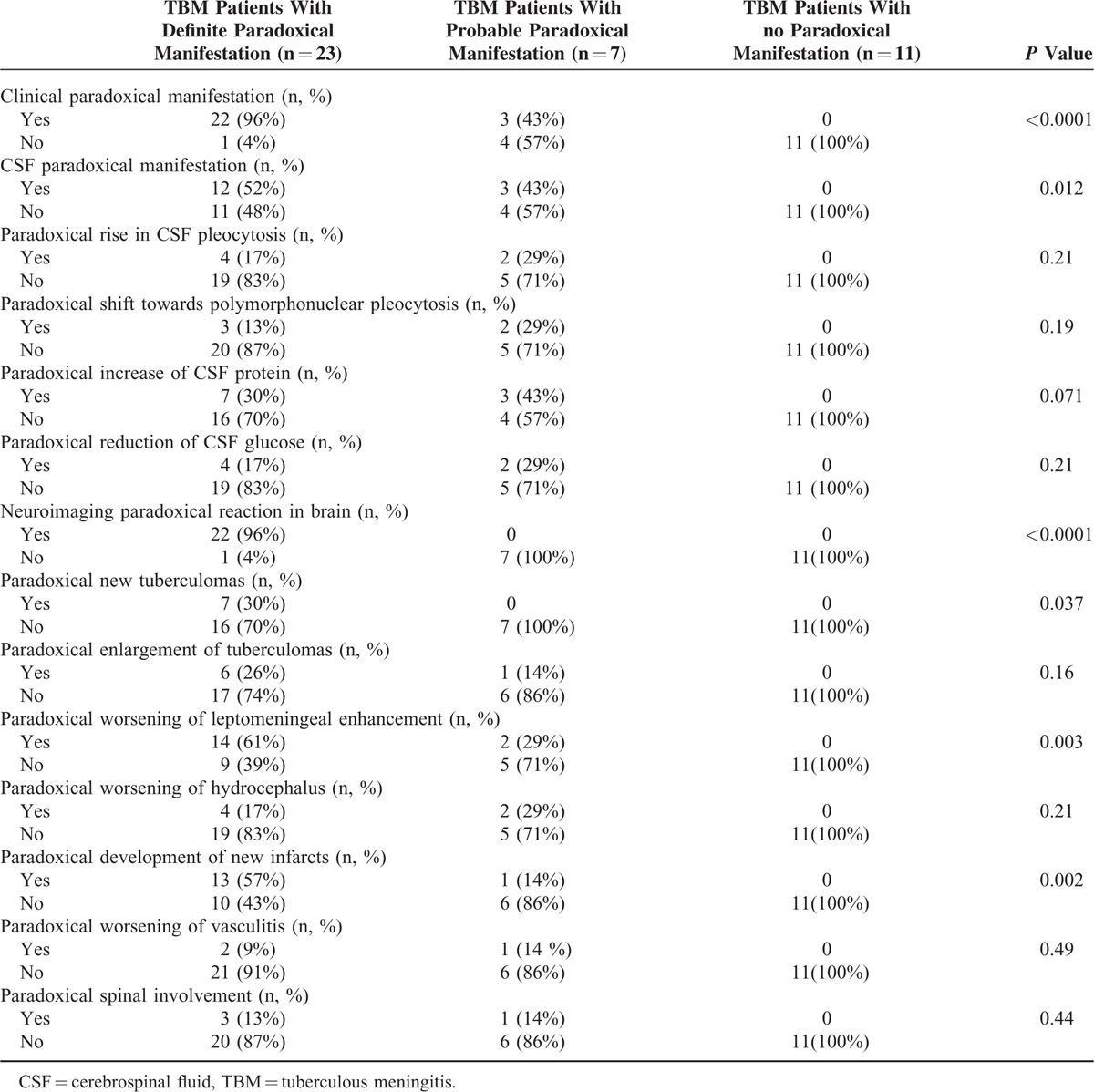
TABLE 5.
Determinants for Development of Definite Paradoxical Manifestation
Time to Onset of 26 Patients With Definite Paradoxical Manifestation
Time to onset of paradoxical manifestation in our TBM patients was between 28 days and 9 months. Most of the patients had onset of paradoxical manifestation at 28 to 50 days. Majority of the TBM patients presented with the onset of neuroimaging of the brain paradoxical manifestation at 50 to 100 days, clinical paradoxical manifestation at 28 to 44 days, and CSF paradoxical manifestation at 29 to 35 days and at 60 to 64 days (Figure 1A–D).
FIGURE 1.
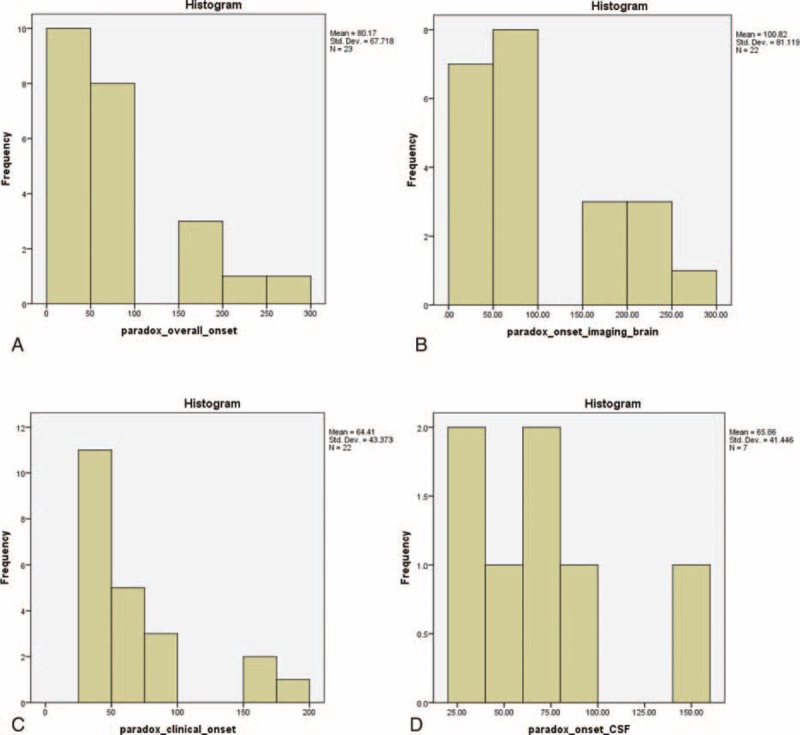
A, Onset of 23 patients with definite paradoxical manifestation (in d). B, Onset of neuroimaging of brain paradoxical manifestation (in d). C, Onset of clinical paradoxical manifestation (in d). D, Onset of CSF paradoxical manifestation (in d). CSF = cerebrospinal fluid.
The longest latency till onset of paradoxical manifestation was 9 months for onset of paradoxical neuroimaging of the brain, 6 months for clinical paradoxical manifestation, and 5 months for CSF paradoxical manifestation.
Figure 2A–C showed the MRI brain of a patient with definite paradoxical manifestation.
FIGURE 2.
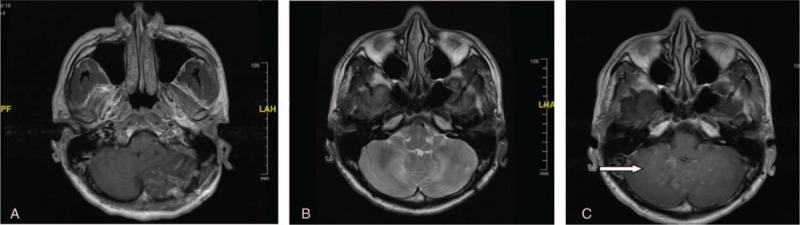
A, T1 with contrast axial view showed leptomeningeal enhancement. B, MRI brain T2W axial showed the disappearance of previously seen hyperintense lesion at left cerebellum during paradoxical manifestation. C, T1 with contrast axial view showed new enhancement of right cerebellum (arrow) with residual enhancement at left cerebellum. MRI = magnetic resonance imaging.
DISCUSSION
This was the first prospective and comprehensive study of paradoxical reaction in non-HIV TBM patients. The most important finding in this study was that paradoxical manifestation was common. Paradoxical manifestation occurred in 56% of our TBM patients, higher than the reported rates in the literature.9 In literature, paradoxical manifestation has been said to occur in 25% of extrapulmonary, and <1% of pulmonary TB patients.3,10–12
The second important finding in this study was that the patients with onset of deterioration at 2 to 4 weeks (defined as probable paradoxical manifestation in this study) manifested differently from those with onset >4 weeks. There were significant differences in the neuroimaging, clinical, and CSF manifestations between these 2 groups of patients. The most obvious differences in the neuroimaging deterioration were the more common worsening of leptomeningeal enhancement, and development of new infarcts and new tuberculoma in the definite cases. The differentiation between those with onset less than or more than 4 weeks is important, as the only previous systemic study on paradoxical manifestation by Sütlas et al4 included patients with onset <4 weeks.
Neuroimaging changes in the brain and clinical paradoxical manifestation were the commonest paradoxical manifestations in our patients followed by CSF manifestation. The changes seen in our patients were also largely similar to the previous studies, but occurred more frequently. In our patients, worsening/new leptomeningeal enhancement was the most common neuroimaging paradoxical manifestation observed in 34% of the patients. The previously reported leptomeningeal enhancement was in 19.7% of the patients.4
Development of new infarct was the second most common brain neuroimaging paradoxical manifestation in our study seen in 29% of our patients. This is higher than the 3% reported by Anuradha et al.13 In our study, 23% of the patients developed new tuberculoma or enlargement of tuberculoma, again higher than the previously reported 6.4%.3,14 Close to a tenth (12.5%) of our patients with repeat angiography showed paradoxical angiographic abnormalities (vasculitis with no vasospasm), higher than the 7.7% incidence previously reported.15 There is only 1 previous report of vasospasm as a feature of paradoxical manifestation.15
Paradoxical clinical manifestation, one of the commonest paradoxical manifestation, was observed in 54% of our patients. Hemiparesis has been reported to be associated with the development of new infarcts, and cranial nerve palsy with the worsening of the leptomeningeal inflammation.3,16
Cerebrospinal fluid manifestation was seen in nearly a third of our patients with paradoxical manifestation. Paradoxical CSF manifestation usually occurs several weeks after the initiation of antituberculous therapy.3 In our patients, CSF paradoxical manifestation most commonly occurs at 29 to 35 days and at 60 to 64 days.
The time to onset of paradoxical reaction in our patients ranged from 28 days to 9 months. This is within the latency previously reported in the literature. It has been said that the latency of paradoxical manifestation tends to be longer for extrapulmonary as compared with PTB.9,11
In our patients, the appearance of new tuberculomas varied from 4 weeks to 5 months. It was reported to vary from 4 weeks to 18 months (median 4 months) in the literature.17,18 The time to tuberculoma enlargement was between 4 weeks and 8 months in our patients. It was mostly reported to be within 6 weeks in the literature.17,18 The latest onset of paradoxical CSF abnormalities in our patient cohort was 150 days, later than the 108 days in the study by Teoh et al.14
A large proportion (30%) of our patients has recurrent manifestation. Recurrent paradoxical manifestation has not been described previously in the literature.3,4,10–12 The phenomenon of paradoxical manifestation is said to be due to interaction between the host's exaggerated immune response and the direct effects of mycobacterial antigen.3,19 Kim and Kim20 described the term “immunologic paradox” as a therapy-induced increase in the Mycobacterium tuberculosis (MTB)-specific Th1-cell reaction in the CSF or peripheral blood after 2 and 4 weeks, respectively, despite clinical improvement.21 The humoral and cell-mediated immune reactions are both excessively stimulated by antigens released from the killed bacteria.20 The recurrent parodoxical manifestation is consistent with a hypothesis from immune response to local antigen release.
The parodoxical manifestation that occurs even after prolonged therapy suggests that the antigenic stimulus may be poorly cleared from disease sites.22M. tuberculosis has a number of insoluble lipid-rich antigens in its cell wall that potently stimulate the response of mononuclear phagocytes.22
The release of mycobacterial cell wall components, including lipoarabinomannan (LAM), and the 30-kDa antigen during mycobacterial destruction by antibiotics may be responsible for an inflammatory host response and production of tumor necrosis factor-alpha (TNF-α) leading to this paradoxical manifestation.21 An increase in plasma TNF-α level may be associated with transient clinical deterioration observed early in the treatment of severe TB.22 In addition, regulatory T-cell dysfunction, at a later stage of TB infection, can result in paradoxical manifestation.23
We also postulate that longer duration of antituberculous therapy and the fact that TBM is a more severe disease compared with PTB7,12,24 as other contributory factors that determine the higher percentage of paradoxical manifestation in patients with TBM in comparison with PTB.
In our study cohort, there was little difference in the outcome between the patients with definite and absent paradoxical manifestation. Reported outcomes are generally favorable in a majority of patients with paradoxical reactions during treatment for TBM.12,14
Many studies have indicated that addition of corticosteroids to antituberculosis regimen helps in early resolution of paradoxical reaction, although there are no controlled trials.3 The limitation of the study was that not all the study patients had CTA/MRA and CSF TB PCR.
In conclusion, this is the presentation of a comprehensive study on paradoxical manifestation with largest number of non-HIV TBM patients. We have demonstrated that paradoxical manifestation is common in the non-HIV TBM. Imaging and clinical were the most common manifestation. In close to one-third of those with paradoxical manifestation was recurrent.
ACKNOWLEDGMENTS
Authors’ contribution: M-LST made substantial contributions to conception and design, acquisition of data, and analysis and interpretation of data. She also was involved in drafting the manuscript or revising it critically for important intellectual content. HMN, SV, and KGO made contributions to acquisition of data. KR, HMN, KAAK, and NRMZ made contributions to analysis of data. MHR gave final approval of the version to be published. CTT revised the manuscript critically for important intellectual content and gave final approval of the version to be published.
Footnotes
Abbreviations: ADC = apparent diffusion coefficient, AFB = acid-fast bacilli, CSF = cerebrospinal fluid, CT = computed tomography, DWI = diffusion weighted image, MRA = magnetic resonance angiography, MRI = magnetic resonance imaging, MRS = modified Rankin scale, PCR = polymerase chain reaction, T1W = T1-weighted image, T2 FLAIR = T2 fluid-attenuated inversion recovery, T2W = T2-weighted image, TBM = tuberculous meningitis.
Funding: Supported by High Impact Research grant UM.C/625/1/HIR/MOE/MED/08/07 H-20001-00-E000035 and UMRG Grant RG390-11HTM.
Conflicts of interest: The study sponsor did not have involvement in the study design; in the collection, analysis and interpretation of the data; in the writing of the report; and in the decision to submit the paper for publication.
REFERENCES
- 1.Misra UK, Kalita J, Maurya PK. Stroke in tuberculous meningitis. J Neurol Sci 2011; 303:22–30. [DOI] [PubMed] [Google Scholar]
- 2.de Castro CC, de Barros NG, Campos ZM, et al. CT scans of cranial tuberculosis. Radiol Clin North Am 1995; 33:753–769. [PubMed] [Google Scholar]
- 3.Ravindra Kumar Garg, Hardeep Singh Malhotra, Neeraj Kumar. Paradoxical reaction in HIV negative tuberculous meningitis. J Neurol Sci 2014; 340:26–36. [DOI] [PubMed] [Google Scholar]
- 4.Sütlas PN, Unal A, Forta H, et al. Tuberculous meningitis in adults: review of 61 cases. Infection 2003; 31:387–391. [DOI] [PubMed] [Google Scholar]
- 5.Thwaites GE, Nguyen DB, Nguyen HD, et al. Dexamethasone for the treatment of tuberculous meningitis in adolescents and adults. N Engl J Med 2004; 351:1741–1751. [DOI] [PubMed] [Google Scholar]
- 6.Raut T, Garg RK, Jain A, et al. Hydrocephalus in tuberculous meningitis: incidence, its predictive factors and impact on the prognosis. J Infect 2013; 66:330–337. [DOI] [PubMed] [Google Scholar]
- 7.Thwaites G, Fisher M, Hemingway C, et al. British Infection Society guidelines for the diagnosis and treatment of tuberculosis of the central nervous system in adults and children. J Infect 2009; 59:167–187. [DOI] [PubMed] [Google Scholar]
- 8.Treatment of tuberculosis:guidelines-Index of-World Health Organisation. Fourth Edition. http://apps.who.int/iris/bitstream/10665/44165/1/9789241547833_eng.pdf. [Google Scholar]
- 9.Carvalho AC, De Iaco G, Saleri N, et al. Paradoxical reaction during tuberculosis treatment in HIV-seronegative patients. Clin Infect Dis 2006; 42:893–895. [DOI] [PubMed] [Google Scholar]
- 10.Lorent N, Sebatunzi O, Mukeshimana G, et al. Incidence and risk factors of serious adverse events during antituberculous treatment in Rwanda: a prospective cohort study. PLoS One 2011; 6:e19566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheng VC, Yam WC, Woo PC, et al. Risk factors for development of paradoxical response during antituberculosis therapy in HIV-negative patients. Eur J Clin Microbiol Infect Dis 2003; 22:597–602. [DOI] [PubMed] [Google Scholar]
- 12.Geri G, Passeron A, Heym B, et al. Paradoxical reactions during treatment of tuberculosis with extrapulmonary manifestations in HIV negative patients. Infection 2013; 41:537–543. [DOI] [PubMed] [Google Scholar]
- 13.Anuradha HK, Garg RK, Agarwal A, Sinha MK, Verma R, Singh MK, et al. Predictors of stroke in patients with tuberculous meningitis and its effect on the outcome. Q J Med 2010; 103:671–678. [DOI] [PubMed] [Google Scholar]
- 14.Teoh R, O’Mahony G, Yeung VT. Polymorphonuclear pleocytosis in the cerebrospinal fluid during chemotherapy for tuberculous meningitis. J Neurol 1986; 233:237–241. [DOI] [PubMed] [Google Scholar]
- 15.Singh B, Garg RK, Singh MK, et al. Computed tomography angiography in patients with tuberculous meningitis. J Infect 2012; 64:565–572. [DOI] [PubMed] [Google Scholar]
- 16.Schoeman JF, Donald PR. Tuberculous meningitis. Handb Clin Neurol 2013; 112:1135–1138. [DOI] [PubMed] [Google Scholar]
- 17.Coulter JB, Baretto RL, Mallucci CL, et al. Interferon gamma. Lancet Infect Dis 2007; 7:225–232. [DOI] [PubMed] [Google Scholar]
- 18.Unal A, Suflas PN. Clinical and radiological features of symptomatic central nervous system tuberculomas. Eur J Neurol 2005; 12:797–804. [DOI] [PubMed] [Google Scholar]
- 19.Afghani B, Lieberman JM. Paradoxical enlargement or development of intracranial tuberculomas during therapy: case report and review. Clin Infect Dis 1994; 19:1092–1099. [DOI] [PubMed] [Google Scholar]
- 20.Kim SH, Kim YS. Immunologic paradox in the diagnosis of tuberculous meningitis. Clin Vaccine Immunol 2009; 16:1847–1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sáenz B, Hernandez-Pando R, Fragoso G, et al. The dual face of central nervous system tuberculosis: a new Janus Bifrons? Tuberculosis (Edinb) 2013; 93:130–135. [DOI] [PubMed] [Google Scholar]
- 22.Hawkey CR, Yap T, Pereira J, et al. Characterization and management of paradoxical upgrading reactions in HIV-uninfected patients with lymph node tuberculosis. Clin Infect Dis 2005; 40:1368–1371. [DOI] [PubMed] [Google Scholar]
- 23.Bekker LG, Maartens G, Steyn L, et al. Selective increase in plasma tumour necrosis factor-alpha and concomitant clinical deterioration after initiating therapy in patients with severe tuberculosis. J Infect Dis 1998; 178:580–584. [DOI] [PubMed] [Google Scholar]


