Abstract
Clinically significant pain (CSP) is one of the most common complaints among cancer patients during repeated hospitalizations, and the prevalence ranges from 24% to 86%. This study aimed to characterize the trends in CSP among cancer patients and examine the differences in the prevalence of CSP across repeated hospitalizations.
A hospital-based, retrospective cohort study was conducted at an academic hospital. Patient-reported pain intensity was assessed and recorded in a nursing information system. We examined the differences in the prevalence of worst pain intensity (WPI) and last evaluated pain intensity (LPI) of ≥4 or ≥7 points among cancer inpatients from the 1st to the 18th hospitalization. Linear mixed models were used to determine the significant difference in the WPI and LPI (≥4 or ≥7 points) at each hospitalization.
We examined 88,133 pain scores from the 1st to the 18th hospitalization among cancer patients. The prevalence of the 4 CSP types showed a trend toward a reduction from the 1st to the 18th hospitalization. There was a robust reduction in the CSP prevalence from the 1st to the 5th hospitalization, except in the case of LPI ≥ 7 points. The prevalence of a WPI ≥ 4 points was significantly higher (0.240-fold increase) during the 1st hospitalization than during the 5th hospitalization. For the 2nd, 3rd, and 4th hospitalizations, there was a significantly higher prevalence of a WPI ≥ 4 points compared with the 5th hospitalization. We also observed significant reductions in the prevalence of a WPI ≥ 7 points during the 1st to the 4th hospitalizations, an LPI ≥ 4 points during the 1st to the 3rd hospitalizations, and an LPI ≥ 7 points during the 1st to the 2nd hospitalization.
Although the prevalence of the 4 CSP types decreased gradually, it is impossible to state the causative factors on the basis of this observational and descriptive study. The next step will examine the factors that determine the CSP prevalence among cancer patients. However, based on these positive findings, we can provide feedback to nurses, physicians, and pharmacists to empower them to be more committed to pain management.
INTRODUCTION
Pain is one of the most feared and burdensome symptoms experienced during repeated hospitalizations among cancer patients.1,2 Cancer patients repeatedly require hospitalization to receive professional care, and cancer-related care services are usually performed in 3 stages. Patients undergo surgery, chemotherapy, and/or radiation therapy after the cancer diagnosis (the initial stage), and continue receiving chemotherapy and other treatments after this initial stage (the continuing stage). Eventually, palliative and/or hospice care are provided to cancer patients to minimize their pain before death (the final stage).3 However, the prevalence of pain among cancer patients ranges from 24% to 86%,1,4 and more than one-third of patients with pain grade their pain as moderate or severe. Despite clear World Health Organization (WHO) recommendations, pain still is a major problem experienced by cancer patients.1
When attempting to calculate pain prevalence in the hospital setting, simply asking a patient whether they are experiencing pain is not adequate because the severity of pain is not determined.1 Patient-reported pain intensity can be assessed using a 0 to 10 numerical rating scale (NRS); the Faces Pain Scale (FPS); the Faces, Legs, Activity, Cry, and Consolability (FLACC) Behavioral Tool; or a visual analogue scale (VAS), which are important tools that quantify a patient's perception of pain.4–9 “Clinically significant pain” (CSP) is defined as patient-reported pain intensity >4 points.10 In particular, pain intensity ≥7 points is defined as severe pain.4,11,12 To clearly document patient-reported pain intensity and to make the data available in real time, an electronic nursing information system (NIS) must be established to record and collect pain intensity, rather than relying on traditional manual chart documentation.
Although previous studies have used pain prevalence as an important indicator of pain in patients,4,13 no data are currently available regarding CSP prevalence, which can be examined among cancer patients according to the worst pain intensity (WPI) and the last evaluated pain intensity (LPI) before discharge for each hospitalization. Moreover, the literature on pain assessment and management among hospitalized cancer patients remains limited.2 In addition, traditional manual chart reviews and interviews are still the most common methods for data collection.4,13 Therefore, if we want to conduct time-series-based and hospital-based outcome analyses among patients, an electronic NIS is superior to the traditional methods of data collection. In terms of the cutoff points of 4 and 7, we divided CSP into 4 types: moderate-to-severe pain with a WPI ≥ 4 points; moderate-to-severe pain with an LPI ≥ 4 points; severe pain with a WPI ≥ 7 points; and severe pain with an LPI ≥ 7 points. Thus, the purposes of this study were to characterize trends in the prevalence of the 4 types of CSP among cancer patients during each hospitalization and to examine differences in the CSP prevalence across repeated hospitalizations based on an electronic NIS.
MATERIALS AND METHODS
Design
This study was a single-center, hospital-based, retrospective cohort study conducted at a national academic hospital in Taiwan. All cancer inpatients admitted between January 1, 2011 and December 31, 2013 were included in this analysis. According to the International Classification of Diseases, 9th Revision, the codes 140–209 and 230–239 were used to identify cancer patients.
For each patient during each hospitalization, we selected only one pain score, which included 2 types: WPI and LPI before discharge. Patient-reported pain intensity scores >4 points were defined as CSP. In particular, a pain intensity ≥ 7 points was defined as severe pain.4,11,12 Considering the cutoff points of 4 and 7, the prevalence of CSP or severe pain among the cancer patients was examined via the WPI and LPI during each hospitalization. CSP during each hospitalization included 4 types: moderate-to-severe pain with a WPI ≥ 4 points; moderate-to-severe pain with an LPI ≥ 4 points; severe pain with a WPI ≥ 7 points; and severe pain with an LPI ≥ 7 points. The formula for calculating the CSP prevalence was as follows: CSP prevalence at each hospitalization = number of patients with WPI (LPI) scores ≥ 4 (moderate-to-severe pain) or ≥ 7 points (severe pain)/total number of inpatients for this hospitalization.
Setting
The hospital has 2747 inpatient beds and approximately 2700 nursing staff members who provide health care services. This hospital manages approximately 97,000 hospitalizations per year. An electronic NIS is used for the routine documentation and charting of vital signs, including pain intensity scores; information is recorded at bedside using hand-held devices. During each observation, the nurses immediately (at the patient's bedside) recorded the patient-reported pain intensity in the NIS. This immediate data entry ensured the accuracy of the recorded pain intensities. This NIS was introduced at the academic hospital in 2011 and has been used hospital-wide for all inpatients since then. Before 2011, all nurses participated in an educational program on proper pain assessment and pain documentation via an NIS. The training program was the cornerstone of quality pain assessment and pain documentation.
Chen14 analyzed the integrity of the NIS records of cancer inpatient pain intensities from January 1 to December 31, 2012. The study used 4 levels of analysis (the number of assessments per person, the number of days of hospitalization per person, the number of hospitalizations per person, and the number of people assessed). The analysis revealed high integrity (97.3%–99.9%) for the database. Therefore, the integrity of the pain assessment database could be ensured by integrating pain assessment sources.
Data Collection
Patient-reported pain intensity was evaluated with an NRS and the FPS in alert and cooperative patients and with the FLACC Behavioral Tool in unconscious or uncooperative patients.6–8 These 3 pain scales, which have good reliability and validity, are all 11-point pain scales where 0 points indicates no pain at all and 10 points indicates the worst possible pain.7,8 All patients were assessed systematically at least once per day by the nurses. Specifically, the pain assessment was performed once each day when no pain at all was present or when the pain intensity was <4 and tolerable, thrice per day when the pain intensity was ≥4 or <4 and intolerable, and as needed when painkiller therapy implementation was indicated.
Ethical Considerations
This study was conducted with the approval of the Institutional Review Board of Taipei Veterans General Hospital. The research was supported by the chief executive officer, medical director and nursing officer of the study hospital.
Analytic Approach
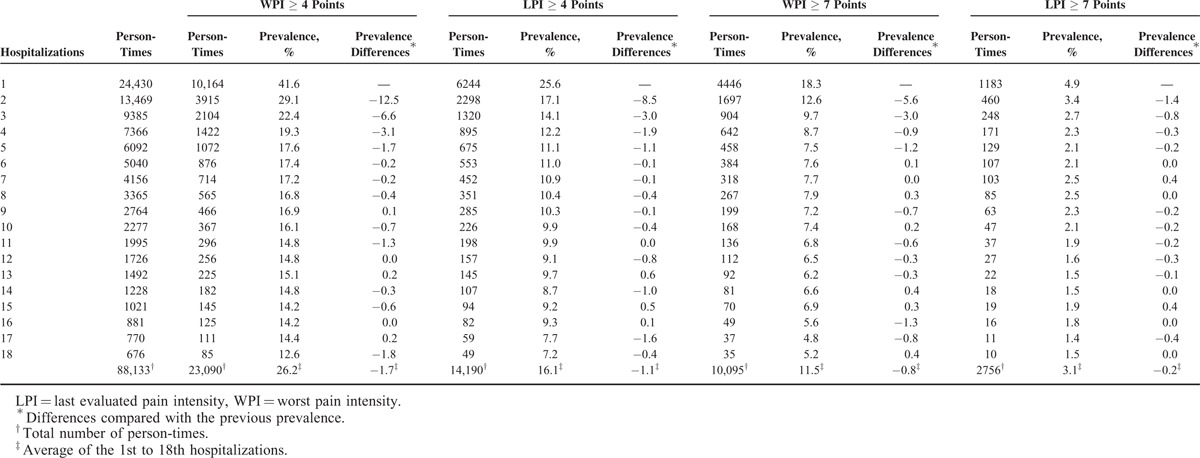
Descriptive statistics were generated for CSP prevalence from the 1st to the 18th hospitalization, and the prevalence of the 4 CSP types is shown in Table 1. From the 1st to 5th hospitalizations, the prevalence of the 4 CSP types sharply decreased, and the absolute differences compared with the previous prevalence was greater than or equal to the average absolute prevalence differences during the 1st to 18th hospitalizations. Therefore, we selected the 5th hospitalization as the reference point for determining the differences in the prevalence of WPI and LPI (≥ 4 or ≥ 7 points) at each hospitalization using linear mixed models for inferential statistics. A P value <0.05 was considered significant. Statistical analyses were performed with the Statistical Package for the Social Sciences (SPSS) version 21.0 for Windows (SPSS Inc, Chicago, IL).
TABLE 1.
The Prevalence of Clinically Significant Pain Among Cancer Inpatients During Each Hospitalization
RESULTS
A total of 1,356,042 pain scores were collected over the 3-year time period. After we reconfirmed the data based on the chart number and admission date, the number of pain scores was reduced to 94,037. We determined the CSP prevalence during each hospitalization, and the number of hospitalizations per patient at this hospital ranged from 1 to 18. In total, 88,133 pain scores were studied. The process of retrieving CSP information from the NIS database is shown in Figure 1.
FIGURE 1.
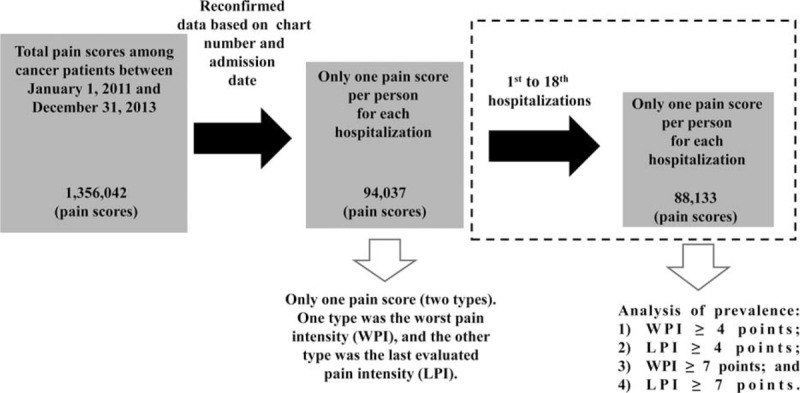
Retrieval of clinically significant pain scores from the NIS database. NIS = nursing information system.
Demographic Characteristics of the Inpatients With Cancer
We examined 88,133 pain scores from the 1st to the 18th hospitalization of patients with cancer. The inpatient age ranged from 0.3 to 101.6 years with a mean of 59.3 ± 17.1 years. Among the inpatients, 47,773 (54.2%) were males and 40,360 (45.8%) were females.
Trends in CSP Prevalence
As the number of hospitalizations increased, the prevalence of a WPI ≥ 4 points decreased from 41.6% to 12.6%, and the prevalence of a WPI ≥ 7 points decreased from 18.3% to 5.2%. Regarding LPI, we also observed downward trends in pain prevalence. With increasing hospitalizations, the prevalence of an LPI ≥ 4 points decreased from 25.6% to 7.2%, and the prevalence of an LPI ≥ 7 points decreased from 4.9% to 1.5%. There was a robust reduction in the CSP prevalence from the 1st to the 5th hospitalization, except for an LPI ≥ 7 points (Table 1).
Differences in CSP Prevalence During Each Hospitalization
The prevalence of a WPI ≥ 4 points during the 1st hospitalization was significantly higher (0.240-fold increase) than the 5th hospitalization. For the 2nd, 3rd and 4th hospitalizations, there was a significantly higher prevalence of a WPI ≥ 4 points compared with the 5th hospitalization. After the 11th hospitalization, the prevalence of a WPI ≥ 4 points was significantly lower than the prevalence for the 5th hospitalization. In addition, the prevalence of an LPI ≥ 4 points was significantly higher during the 1st (0.145-fold increase), 2nd (0.060-fold increase), and 3rd (0.030-fold increase) hospitalizations (Table 2). Table 2 also shows the prevalence of a WPI or LPI ≥ 7 points. To evaluate the CSP prevalence from the 1st to the 5th hospitalization, we characterized the trends in the prevalence of the 4 CSP types (Fig. 2).
TABLE 2.
Differences in the Clinically Significant Pain Prevalence Among Cancer Inpatients During Each Hospitalization
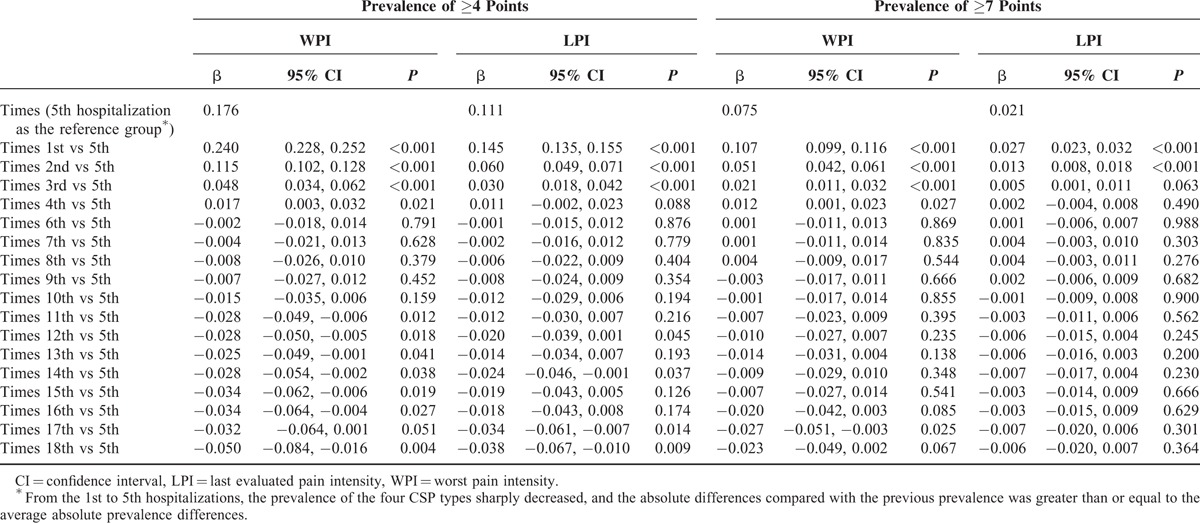
FIGURE 2.
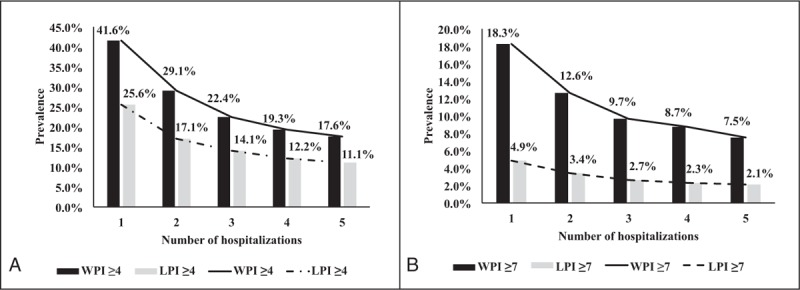
Trends in the CSP prevalence from the 1st to the 5th hospitalization. The 5th hospitalization was viewed as a reference group to determine the CSP differences for WPI and LPI of (A) ≥4 or (B) ≥7 points using linear mixed models. (A) For WPI ≥ 4, 1st versus 5th times (P < 0.001); 2nd versus 5th times (P < 0.001); 3rd versus 5th times (P < 0.001); and 4th versus 5th times (P = 0.021). For LPI ≥ 4, 1st versus 5th times (P < 0.001); 2nd versus 5th times (P < 0.001); 3rd versus 5th times (P < 0.001); and 4th versus 5th times (P = 0.088). (B) For WPI ≥ 7, 1st versus 5th times (P < 0.001); 2nd versus 5th times (P < 0.001); 3rd versus 5th times (P < 0.001); and 4th versus 5th times (P = 0.027). For LPI ≥ 7, 1st versus 5th times (P < 0.001); 2nd versus 5th times (P < 0.001); 3rd versus 5th times (P = 0.063); and 4th versus 5th times (P = 0.490). CSP = clinically significant pain, LPI = last evaluated pain intensity, WPI = worst pain intensity.
DISCUSSION
In this study, we examined the CSP prevalence during each hospitalization among cancer patients who were repeatedly hospitalized over time. Importantly, we found that the prevalence of the 4 CSP types decreased from the 1st to the 18th hospitalization. Specifically, the prevalence of a WPI ≥ 4 or 7 points was significantly reduced from the 1st to the 4th hospitalization. The prevalence of an LPI ≥ 4 points was significantly reduced from the 1st to the 3rd hospitalization, and the prevalence of an LPI ≥ 7 points was significantly reduced from the 1st to the 2nd hospitalization.
In the present study, the prevalence of a WPI ≥ 4 points ranged from 12.6% to 41.6%, and the prevalence of a WPI ≥ 7 points ranged from 5.2% to 18.3%. These values are similar to other studies 4,7 and lower than the values published in a systematic review of cases over the past 40 years.1 However, the previous studies focused on pain prevalence during a single hospitalization. Because cancer patients often require repeated hospitalizations, examining pain prevalence during one hospitalization is insufficient for these inpatients. Therefore, a long-term analysis of pain during the repetitive hospitalizations of each patient should be performed.
In addition, we assessed LPI before discharge and demonstrated that the prevalence of an LPI ≥ 4 or 7 points was lower than the prevalence of a WPI ≥ 4 or 7 points for each hospitalization. The CSP prevalence tended to decrease before discharge for each hospitalization. At our institution, after each pain assessment, the nurses used proper painkiller therapy to prevent the severity of the pain from worsening; however, to date, there is still a gap between pain assessment and the implementation of pain treatment strategies. To reduce the clinical divide, high-quality pain documentation is useful because the assessment and documentation of pain are viewed as the cornerstones of effective pain management.10 Standard-setting agencies, such as the Joint Commission, rely on documentation in the patient care record to assess the quality of pain management.15,16 However, over one-third of the information recorded is not in accord with the patient's report, and the nurses’ documentation regarding pain may be incomplete in the nursing records.11 Therefore, we used systematic pain assessments and regularly documented pain intensity by direct entry into an NIS database in our hospital. Nurses specifically recorded the pain score in the NIS, so that the pain intensity and effectiveness of the chosen pain management therapy could be rapidly determined by nurses, physicians, and pharmacists.17 Through systematic pain assessment and documentation in an NIS, nurses are more attentive to pain symptoms among cancer patients and can immediately notify the physician in charge to improve pain. At our institution, pain assessment and management are addressed through a multidisciplinary approach. Nurses, physicians, and pharmacists all facilitate pain management; importantly, the nurses are the gatekeepers in pain assessment and management.
All cancer patients will experience pain during repeated hospitalizations.10 Carr et al10 noted that the recurrence of moderate or severe pain during repeated hospitalizations reflects a lack of continuous and effective pain management strategies. In our hospital, the prevalence of a WPI ≥ 4 and 7 points was significantly reduced from the 1st to the 4th hospitalization. The prevalence of an LPI ≥ 4 points was significantly reduced from the 1st to the 3rd hospitalization, and the prevalence of an LPI ≥ 7 points was significantly reduced from the 1st to the 2nd hospitalization. This observation affirmed the significantly decreased CSP prevalence during repeated hospitalizations, which could be the long-term outcome of the nurses’ role as gatekeepers in pain assessment and management for cancer inpatients.
Our study had 2 methodological strengths. First, we used an NRS, the FPS, or the FLACC Behavioral Tool to measure an individual's pain intensity, which is also known as a patient-reported outcome. Patient-reported outcomes are important measurements that have been incorporated into ongoing clinical care.18,19 This implies that during daily practice, simply asking “the pain question” (without the use of extensive and time-consuming questionnaires) can detect patients who are experiencing pain. Based on the patient-reported pain intensity, we could characterize the trends in CSP prevalence during repeated hospitalizations. Using the same scoring method at different time points to measure pain allows clinicians to observe variation in pain over time.5,19 However, cancer pain is a complex and multidimensional symptom that is affected by psychological and social variables and the disease process itself.20 Although the distinction between the presence or absence of CSP among cancer patients will enable the calculation CSP prevalence, this distinction does not provide information about the severity of pain or the degree of pain reduction between the WPI and LPI for each hospitalization. To facilitate the comparison of studies and to coordinate the planning of pain services, multidimensional tools, such as the absolute difference in pain intensity or the percentage difference in pain intensity, may be used in future research.
The second strength of this study was the use of an electronic data capture system for outcome studies that integrated data collection into the ongoing process of patient care to conduct a hospital-based study. In general, there is still a lack of information about pain assessment and scoring on a hospital-wide basis.10 This gap presents a challenge, and it can be difficult to integrate the collection of valid outcome measures into a busy clinical practice in which time and cost-containment pressures already exist. The real-time availability of data essentially requires electronic data capture followed by automatic reporting. The burden of providing the data on either the patient or the physician must be minimized to make data collection as brief as possible to facilitate meaningful results. Therefore, the development and implementation of patient-reported outcome data collection systems for a large number of pain programs and integration into electronic health records are critical steps.18 Then, patient-reported pain intensity can be clearly documented, eliminating transcription error, facilitating the subsequent retrieval and analysis of data, and allowing tracking over time by clinicians to guide patient care.10
Our study evaluated the CSP prevalence in an entire population of cancer inpatients during each hospitalization in an academic hospital, thereby addressing the weaknesses of the previous study,7 which evaluated the pain intensity of first-time medical oncology unit inpatients. In addition, most studies related to pain prevalence have relied on interviews, manual documentation of pain assessment, and retrospective chart reviews.21–24 In our study, the CSP prevalence was similar to or lower than the prevalence reported in other studies. This result may be due to the electronic NIS instead of the traditional data collection method. The most common electronic NIS functionalities or components are records of patient pain intensity and clinical notes.25 The NIS enables the integration of pain intensity data collection into the ongoing process of pain measurement, and provides comprehensive information about pain assessment.18 The electronic NIS is increasingly viewed as an essential tool for quality assurance and improvement in a variety of care settings.25 Further research regarding pain documentation using electronic medical records is needed.
This study also had 2 limitations. One limitation is that this study was conducted in a cancer inpatient cohort that was heterogeneous regarding clinical stage. This study was conducted at a single academic hospital. Thus, the second limitation is that the generalizability of the findings may be limited. However, our study design can be replicated at other institutions to validate these results.
CONCLUSION
In conclusion, this report represents the first hospital-based study that used an electronic database to analyze CSP prevalence among cancer inpatients in Taiwan. The trend curves for the prevalence of the 4 CSP types indicated a reduction from the 1st to the 18th hospitalization. In particular, the prevalence of a WPI ≥ 4 and 7 points was significantly reduced from the 1st to the 4th hospitalization. Although the prevalence of the 4 CSP types decreased gradually, it is impossible to state the causative factors on the basis of this observational and descriptive study. The next step will examine the factors that determine the CSP prevalence among cancer patients. However, based on these positive findings, we can provide feedback to nurses, physicians, and pharmacists to empower them to be more committed to pain management.
Acknowledgments
The authors thank the contributions made by Yi-Syuan Wu (biostatistician) during the statistical analysis of the data.
Footnotes
Abbreviations: CSP = clinically significant pain, FLACC = Faces, Legs, Activity, Cry, and Consolability, FPS = Faces Pain Scale, LPI = last evaluated pain intensity, NIS = nursing information system, NRS = numerical rating scale, VAS = visual analogue scale, WPI = worst pain intensity.
K-YW and C-YL contributed equally to this work.
This study was financially supported by grants from the Taipei Veterans General Hospital (V104C-024).
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.van den Beuken-van Everdingen MHJ, de Rijke JM, Kessels AG, et al. Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol 2007; 18:1437–1449. [DOI] [PubMed] [Google Scholar]
- 2.Mearis M, Shega JW, Knoebel RW. Does adherence to National Comprehensive Cancer Network guidelines improve pain-related outcomes? An evaluation of inpatient cancer pain management at an academic medical center. J Pain Symptom Manage 2014; 48:451–458. [DOI] [PubMed] [Google Scholar]
- 3.Li TY, Hsieh JS, Lee KT, et al. Cost trend analysis of initial cancer treatment in Taiwan. PLOS One 2014; 9:e108432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Melotti RM, Samolsky-Dekel BG, Ricchi E, et al. Pain prevalence and predictors among inpatients in a major Italian teaching hospital. A baseline survey towards a pain free hospital. Eur J Pain 2005; 9:485–495. [DOI] [PubMed] [Google Scholar]
- 5.Farrar JT. Advances in clinical research methodology for pain clinical trials. Nat Med 2010; 16:1284–1293. [DOI] [PubMed] [Google Scholar]
- 6.Paice JA, Cohen FL. Validity of a verbally administered numeric rating scale to measure cancer pain intensity. Cancer Nurs 1997; 20:88–93. [DOI] [PubMed] [Google Scholar]
- 7.Martoni AA, Esposti CD, Cricca A, et al. Twice-daily pain monitoring as standard clinical practice for inpatients at a medical oncology unit: a descriptive study. Ann Oncol 2007; 18:158–162. [DOI] [PubMed] [Google Scholar]
- 8.Voepel-Lewis T, Zanotti J, Dammeyer JA, et al. Reliability and validity of the face, legs, activity, cry, consolability behavioral tool in assessing acute pain in critically ill patients. Am J Crit Care 2010; 19:55–62. [DOI] [PubMed] [Google Scholar]
- 9.Alghadir A, Anwer S, Anwar D, et al. The development and validation of Hundred Paisa Pain Scale for measuring musculoskeletal pain: a prospective observational study. Medicine (Baltimore) 2015; 94:e1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carr ECJ, Meredith P, Chumbley G, et al. Pain: a quality of care issue during patients’ admission to hospital. J Adv Nurs 2014; 70:1391–1404. [DOI] [PubMed] [Google Scholar]
- 11.de Rond ME, de Wit R, van Dam FS, et al. A pain monitoring program for nurses: effect on communication, assessment and documentation of patients’ pain. J Pain Symptom Manage 2000; 20:424–439. [DOI] [PubMed] [Google Scholar]
- 12.Wang K, Chen Z, Meng Z, et al. Analgesic effect of high intensity focused ultrasound therapy for unresectable pancreatic cancer. Int J Hyperthermia 2011; 27:101–107. [DOI] [PubMed] [Google Scholar]
- 13.Visentin M. Towards a pain-free hospital: a project to improve the approach to the patient in pain. J Headache Pain 2002; 3:59–61. [Google Scholar]
- 14.Chen YF. The integrity and appropriateness of cancer pain assessment data in a medical center to promote pain-free hospital. [National Digital Library of Theses and Dissertations in Taiwan]. October 23, 2013. Available at: http://handle.ncl.edu.tw/11296/ndltd/67278617764982538647 Assessed May 23, 2014. [Google Scholar]
- 15.Samuels JG, Fetzer S. Pain management documentation quality as a reflection of nurse's clinical judgment. J Nurs Care Qual 2009; 24:223–231. [DOI] [PubMed] [Google Scholar]
- 16.Joint Commission Accreditation of Healthcare Organizations. Comprehensive Accreditation Manual for Hospital: The Official Handbook. Joint Commission Resources, Inc; USA 2006. [Google Scholar]
- 17.de Rond ME, de Wit R, van Dam FS, et al. A pain monitoring program for nurses: effect on the administration of analgesics. Pain 2000; 89:25–38. [DOI] [PubMed] [Google Scholar]
- 18.Witkin LR, Farrar JT, Ashburn MA. Can assessing chronic pain outcomes data improve outcomes? Pain Med 2013; 14:779–791. [DOI] [PubMed] [Google Scholar]
- 19.Farrar JT, Polomano RC, Berlin JA, et al. A comparison of change in the 0-10 numeric rating scale to a pain relief scale and global medication performance scale in a short-term clinical trial of breakthrough pain intensity. Anesthesiology 2010; 112:1464–1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Luckett T, Davidson PM, Green A, et al. Assessment and management of adult cancer pain: a systematic review and synthesis of recent qualitative studies aimed at developing insights for managing barriers and optimizing facilitators within a comprehensive framework of patient care. J Pain Symptom Manage 2013; 46:229–253. [DOI] [PubMed] [Google Scholar]
- 21.de Remer CE, Fleming VH, Brown S, et al. Evaluation of pain management documentation. South Med J 2011; 104:629–633. [DOI] [PubMed] [Google Scholar]
- 22.Lucenteforte E, Collini F, Simonetti M, et al. Assessing pain in hospital in-patients: a cross-sectional study in Tuscany, Italy. Intern Emerg Med 2012; 7:477–482. [DOI] [PubMed] [Google Scholar]
- 23.Hanley MA, Jensen MP, Ehde DM, et al. Clinically significant change in pain intensity ratings in persons with spinal cord injury or amputation. Clin J Pain 2006; 22:25–31. [DOI] [PubMed] [Google Scholar]
- 24.Gerbershagen K, Gerbershagen HJ, Lutz J, et al. Pain prevalence and risk distribution among inpatients in a German teaching hospital. Clin J Pain 2009; 25:431–437. [DOI] [PubMed] [Google Scholar]
- 25.Zheng NT, Rokoske FS, Kirk MA, et al. Hospices’ use of electronic medical records for quality assessment and performance improvement programs. J Pain Symptom Manage 2014; 48:582–589. [DOI] [PubMed] [Google Scholar]


