Abstract
This article presents the results of a process evaluation of the Alaska Native (AN) Colorectal Cancer (CRC) Family Outreach Program, which encourages CRC screening among AN first-degree relatives (i.e., parents, siblings, adult children; hereafter referred to as relatives) of CRC patients. Among AN people incidence and death rates from CRC are the highest of any ethnic/racial group in the United States. Relatives of CRC patients are at increased risk; however, CRC can be prevented and detected early through screening. The evaluation included key informant interviews (August to November 2012) with AN and non-AN stakeholders and program document review. Five key process evaluation components were identified: program formation, evolution, outreach responses, strengths, and barriers and challenges. Key themes included an incremental approach that led to a fully formed program and the need for dedicated, culturally competent patient navigation. Challenges included differing relatives’ responses to screening outreach, health system data access and coordination, and the program impact of reliance on grant funding. This program evaluation indicated a need for more research into motivating patient screening behaviors, electronic medical records systems quality improvement projects, improved data-sharing protocols, and program sustainability planning to continue the dedicated efforts to promote screening in this increased risk population.
Keywords: Alaska Native people, colorectal cancer prevention, colorectal cancer screening, data-sharing protocols, family history, patient navigators, program sustainability
Background
Colorectal Cancer Prevention and First-Degree Relatives
Colorectal cancer (CRC) is the second leading cause of cancer mortality and new cases of cancer among Alaska Native (AN) people, who experience twice the incidence and mortality due to this disease as do Whites in the United States (Kelly, Alberts, Sacco, & Lanier, 2012). CRC can be successfully treated if detected early or prevented by removal of precancerous (adenomatous) polyps. People with a family history of CRC or adenomatous polyps in one or more first-degree relatives (i.e., parents, siblings, or children) are almost twice as likely as the person with average risk to experience CRC themselves, especially if their family member was affected before age 45 (Fuchs et al., 1994; Slattery & Kerber, 1994; St John et al., 1993). Screening strategies targeting relatives of CRC patients could contribute to the prevention or early detection of 15% to 20% of CRC cases (Boutron, Faivre, Quipourt, Senesse, & Michiels, 1995; Pariente, Milan, Lafon, & Faivre, 1998). Therefore, AN relatives are an increased risk population, within a larger AN population that experiences a significant health disparity due to CRC.
Cancer was once considered a rare disease in the AN population. The growing burden of cancer has led to an increased focus on cancer prevention and early detection by tribal leaders from around the state, as well as by tribal and clinical leadership within the Alaska Tribal Health System (ATHS). The Alaska Native Medical Center (ANMC) CRC Screening Guidelines (2013) are based on guidelines from several national organizations (Allison & Potter, 2009; Levin et al., 2008; Winawer et al., 2003) and recommend that AN relatives receive a colonoscopy every 5 years beginning at age 40 or 10 years before the earliest age at which a relative was diagnosed, whichever was earlier.
Program Overview
The ATHS is made up of regional tribal health organizations (THOs) that provide health care and services to AN people living in their geographic area. In many parts of Alaska, the regional THO is the only health care provider available for both Native and non-Native residents. The ATHS provides cradle-to-grave comprehensive care for approximately 143,000 tribal members. The ATHS is a huband-spoke network of small village-based clinics, subregional clinics, and regional hospitals. There is only one AN tertiary care hospital (ANMC) located in Anchorage, Alaska. The goal of the AN CRC Family Outreach Program is to encourage first-degree relatives of CRC patients (hereafter referred to as “AN relatives”) seen at ANMC to obtain CRC screening. CRC patients at ANMC are asked for a contact list of their relatives while still in the hospital for cancer treatment or when returning for follow-up appointments; alternately, a form with a business reply envelope is mailed, to be filled out at home. The contact information given by the CRC patient is entered into a database. This information is then used by patient navigators to provide direct outreach to AN relatives using telephoned and mailed reminders, encouraging them to get screened for CRC, scheduling them into the screening clinic, and guiding them through the cancer screening process.
Method
A process evaluation was conducted to better understand key components of the AN CRC Family Outreach Program. Key informant semistructured interviews formed a central line of evidence in this evaluation, along with program document review, including review of grant progress reports, written and electronic mail correspondence, and meeting minutes. Key informants were selected to ensure that former and current AN and non-AN program staff and managers, as well as key stakeholders involved in the creation of the program, were represented. A snowball sampling technique (Goodman, 1961; Patton, 1990) was used to identify informants until all identified key informants had either participated or declined to participate. The interview guide was developed by the evaluator in consultation with the program director and included 21 semistructured open-ended questions. Coding of the questionnaire used directed content analysis wherein broad categories were initially developed based on question topics and further coding of content resulted in new codes and categories (Hsieh & Shannon, 2005). All interviews were conducted in person. The interviews were audiotaped, and transcribed verbatim, and the transcripts coded by one coder using established qualitative software (QSR International NVivo Version 10, Burlington, MA).
The Alaska Area Institutional Review Board (IRB), the University of Alaska Fairbanks IRB, and the Alaska Native Tribal Health Consortium and Southcentral Foundation research and ethics committees and privacy officers reviewed and approved the study protocol.
Results
Between July 30, 2012, and September 5, 2012, a total of eight interviews with key informants were conducted including hospital administrators (1 interview), patient navigators (2), program managers (1), data analysts (1), and clinicians (3). Those who declined (n = 5; data analyst [1], clinician [2], program managers [2]) self-reported that nonparticipation was due to insufficient knowledge of the program. Of the AN relatives listed in the database as being due for screening, 44% have been screened. This is lower than the AN general population average screening rate of 58.5% (Indian Health Service, 2012). The findings of the key informant interviews were delineated into five main components of the process evaluation. These components included program formation, evolution, outreach responses, strengths, and barriers and challenges (see Table 1).
Table 1.
Key Themes of the Alaska Native Colorectal Cancer Family Outreach Program Process Evaluation, 2012.
| Key component | Themes |
|---|---|
| Program formation | • Incremental approach to program development |
| Program evolution | • Additional funding used to hire dedicated outreach staff (patient navigators) |
| • Improved outreach tracking system and patient materials | |
| • Improved endoscopic access for patients | |
| Outreach responses | • Increased awareness of colorectal cancer and the need for screening among population served |
| • Fear of finding cancer | |
| • Wanting to prevent cancer by getting screened | |
| • Needing help navigating the system to get screened | |
| • Familial support for screening | |
| Strengths | • Geographically and ethnically defined patient population |
| • Screening costs covered by Alaska Tribal Health System | |
| • Support by hospital leadership (Chief of Surgery) | |
| • Only program collecting this information and using it for outreach among Alaska Native people | |
| • Dedicated staff time | |
| • Alaska Native patient navigators who receive intensive training in motivational interviewing and patient outreach techniques | |
| Barriers and challenges | • Culturally heterogeneous population from across state |
| • More patients still due for screening | |
| • Need for more education on benefits of screening (patients) | |
| • Reliance on grant funding for program operations | |
| • Need for improved data sharing and reporting in Alaska Tribal Health System |
Program Formation
The Alaska Native Tumor Registry, which monitors cancer among AN people, has documented a rise in both CRC incidence and mortality among AN people. Those data, coupled with the literature showing that compared with nonrelatives, relatives have a higher prevalence of CRC, and ANMC clinical observations of CRC in multiple family members, sparked interest in the late 1990s of the ANMC Chief of Surgery in collecting family information from AN CRC patients.
The AN CRC Family Outreach Program began as a spreadsheet in the late 1990s of ~200 newly diagnosed AN CRC patients. In early 2001, an ANMC nurse practitioner was assigned to communicate with CRC patients seen at the hospital to request voluntary contact information for their AN relatives. CRC patients were approached either in person or by mailed letter. The hospital's risk management and legal departments reviewed the project activities and the outreach letter. Because the nurse practitioner was primarily providing screening endoscopy procedures, she was limited in her capacity to dedicate sufficient time to contacting the AN relatives identified. However, a registered nurse assisted temporarily in sending some outreach letters to AN relatives. At that time, no attempt was made to keep track of how many AN relatives were contacted or obtained CRC screening.
Originally kept as a hand-written ledger, the AN relatives’ contact information was transcribed into a Microsoft Access database in 2002. Although beneficial in that the database could be used immediately and contained the exact variables required, it was not linked to the hospital's medical record system. Keeping AN relatives’ screening information current was difficult and required significant staff time.
A medical records system CRC tracking package was created in 2003 and used briefly to keep track of patients due for screening. This package could leverage patient registration and previous screening information from the electronic medical record. However, there were drawbacks to using the tracking package. All information had to be hand-entered (similar to the database), it did not offer as many useful fields, and it was difficult for staff to navigate or pull aggregated reports.
The freestanding Microsoft Access database is still the primary data management tool used for the program. The database can be used by multiple staff members conducting outreach simultaneously. All contact information is kept on a secure server, and access to the server is password-protected. In 2008, a programmer/analyst worked to increase the capacity of the database, most notably by adding fields on AN relatives’ screening dates and results, a tracking log to record and display outreach activities and patient notes, and report functions for those activities (number of phone calls made, number of letters sent, appointments kept, etc.). That was the first point at which outcomes of the program could be tracked and evaluated.
Program Evolution
In April 2007, a program assistant was hired using grant funding to identify AN relatives, maintain the database, and provide outreach to relatives to encourage them to get screened (using phone contacts and mailed letters). Despite the program assistant's limited experience in patient outreach and knowledge in motivating AN relatives to complete screening, and competing clinical job responsibilities, relatives’ screening rates increased from about 25 relatives screened per year in the early 2000s to 90 screened in 2008. Public education efforts were also increasing throughout the late 2000s so increases in screening were likely not solely due to the program activities. Also, in October 2009, the program assistant's job title was changed to patient navigator to better reflect the job duties.
In 2009, the screening endoscopist started allowing direct referrals whereby low-risk patients did not have to go through a primary care provider to schedule a colonoscopy. The program also notified providers when the AN relatives in their care were due for screening by letter, fax, telephone calls, or electronic messages within the electronic medical system. The outreach letter text was also simplified and a picture of the screening staff added so that patients would feel more comfortable when the patient navigator contacted them by phone or they came in for screening.
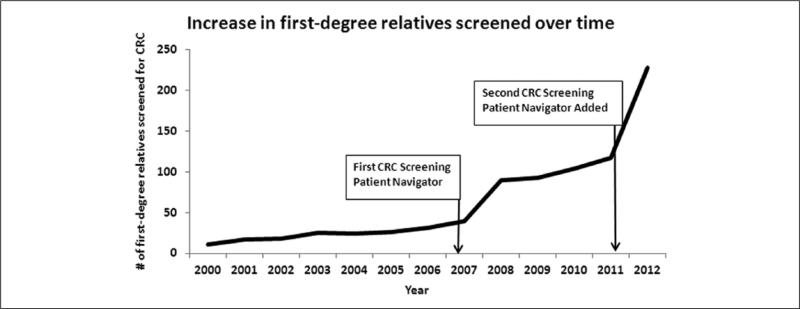
In 2012, a second patient navigator was hired using research grant funding. The additional staff capacity almost doubled the number of AN relatives screened to 228, from 117 in 2011 (see Figure 1). At the same time, there was also a shift in the location and staffing of the CRC screening clinic. This shift brought additional case manager assistants, who were able to take over the clinical duties the patient navigator had been performing previously and so enabled more time for outreach activities.
Figure 1.
First-degree relatives screened from the Alaska Native Colorectal Cancer Family Outreach Program, 2000-2012.
Outreach Responses
The original goal for the outreach program was to reduce CRC on a population level, working systematically from a list of individuals at increased risk due to family history. The program has found that the most effective way to obtain family history lists from CRC patients is during a face-to-face interaction. This can be especially difficult for cancer patients who may be feeling sick, are just learning of their diagnosis and treatment plan, or are working through the effects of treatment. However, during that personal interaction, it is possible to sit with the cancer patient and explain that the information collected will be used to help their family members. Oftentimes, AN relatives are at the hospital (helping care for the CRC patient), and they can be approached directly to be scheduled for screening.
Several key informants pointed out that over the past 15 to 20 years there has been an enhanced awareness about CRC in the AN population, due to increased education throughout the state and wider availability of screening services (Cueva, Dignan, & Kuhnley, 2012; Cueva et al., 2013; Kuhnley & Cueva, 2011). Many of the informants felt that the Native population as a whole has become much more aware of family history as a risk factor, and the need for CRC screening.
Similar to other populations, for AN relatives, there are an additional set of issues that play into screening adherence. AN relatives experience conflicting emotions, including fear or anger about getting cancer, especially if the relative is the primary caretaker for the cancer patient. They see what the patient is experiencing, including if the treatment is unsuccessful. Sometimes the AN relatives do not want to complete the screening procedure for fear that they will find out that they also have cancer. At times, AN relatives simply do not believe that they are at risk themselves.
One patient navigator reported:
I've had people who were just absolutely upset that I called. I told them, “Your family member had colon—.” They're like, “Who?” “Oh, yeah, I guess she did.” And I say, “Well, you are more likely to develop these precancerous polyps.” And they say, “Oh, bunch of baloney!” (Patient Navigator)
For some other AN relatives, if they see a loved one delay seeking care for symptoms, they feel a very strong impetus to be screened, themselves. For others, seeing CRC caught early in a family member, and that person is alive and disease-free, can also be a cue to get screened. Some interview participants described occasions when the CRC patient told their family members that they (i.e., the family members) are at higher risk, and encouraged them to get screened; sometimes, two AN relatives provide support and encouragement to one another.
Often we'll see somebody who has cancer, and when one of the siblings get screened and they kind of push the others to get screened. So I think there's family pressure which works to help, and that makes a difference. I think that the more people that are screened, the more likely any given patient who hasn't been screened will be able to talk to somebody who's actually gone through it. (Hospital Administrator)
Successful Components and Strengths of the Program
All key informants reported that the most critical and also successful components of the program are the staff and other related resources dedicated to actively obtaining information on AN relatives and providing outreach to those relatives, including multiple telephone calls, to schedule them for screening. Key informants highlighted that if the program did not collect the AN relatives’ information from CRC patients, then there would be no way for clinicians to know which patients need earlier CRC screening, and at what age. For relatives as well, without the program's efforts, many would neither know they need to be screened, nor how to obtain screening.
I don't know of any other program around the country that is actually dedicating resources to going out and finding people that are at risk this way. Most of them are leaving it up to families and people to show up rather than to actually have people dedicated to gathering that information. (Program Manager)
A further strength is that patient navigators (one male, one female) are ANs themselves, and contribute their cultural competence toward motivating relatives to obtain screening. One patient navigator commented:
I think of Native people as a whole family, in a way, whether they're close together or far apart. So that's what kind of drives me to call people and be passionate about talking to people because I think of them as family members. (Patient Navigator)
Staff providing outreach have received training in motivational interviewing, social marketing, and patient navigation to help increase their ability to promote screening completion among relatives. Finding a leader and champion at the highest level of administration—the ANMC Chief of Surgery, who provided staff resources toward the program—has also played a key role in the ongoing vitality of the program.
Another element that benefits the program is that the AN population is a racial subgroup that is geographically defined and a patient population that is well defined, unlike other health care systems in the United States. Additionally, because CRC screening occurs within the ATHS, all AN relatives have access to screening regardless of financial status. By removing the financial burden, a major barrier to screening experienced by other U.S. populations is reduced.
Program Barriers and Challenges
The CRC Outreach Program was described as being very staff intensive, especially in terms of maintaining the program database and providing outreach to relatives. At various points in the implementation of the program, the staff responsible for outreach have been required to take on additional clinical duties. As a result, they have not always been able to devote adequate time and attention to outreach activities. While the program has been successful at increasing outreach to relatives, there are still many who are not screened.
One key informant stated:
The biggest challenge now is getting us up the next 20 percent. And that's going to take different approaches, whether that's different techniques of screening or making better use of the navigator program to do outreach [ . . . ]. Unless we do something different, we're going to stay where we are. (Hospital Administrator)
A major challenge for the program mentioned by all key informants is the continued reliance on grant and research money and the resulting impact on program sustainability.
I've seen this many, many times in the Indian Health Service and now in the Alaska Native Health System is that when the grant for a program starts to shrink, the program also begins to shrink. And when the grant goes away, the program goes away and it has nothing to do with how important that program is to the health of the population or how successful the program is. (Clinician)
Another challenging issue identified is the complexity of implementing a coordinated statewide focus, in the context of minimal data sharing and reporting ability throughout the ATHS. Although the ATHS serves AN people, there is limited infrastructure to support communication and record sharing between medical record systems. The medical record information for relatives who have completed screening at one of the regional facilities is not regularly transmitted to ANMC and vice versa. As such, a primary care provider at the regional facility might recommend screening, not knowing that the patient was screened elsewhere, or the AN CRC Family Outreach Program database may show relatives are due who have already been screened.
Within the electronic medical record system, a mechanism is lacking that could alert providers at regional facilities about relatives living in their region who are in need of screening. With such knowledge, these relatives could be screened more conveniently at their regional facility. Currently, this information is only available through out-reach lists that are compiled and distributed periodically to regional facilities by the AN CRC Family Outreach Program. These findings point to the need for more coordinated data management and system efficiencies to improve the overall outreach to AN relatives at risk for CRC.
In addition to reporting mechanisms, there is also the need for enhanced coordination and education for tribal providers and case managers to ensure that they are knowledgeable about the importance of CRC screening for their patients at increased risk and the appropriate age to refer relatives for screening. Additionally, providers need training based in health behavior change models and theory, and which provide them with tools to motivate patients to achieve healthier behaviors (Kiviniemi, Bennett, Zaiter, & Marshall, 2011; Wahab, Menon, & Szalacha, 2008). Primary care providers may develop positive and trusting relationships with their patients, and so their recommendations could help improve screening adherence in this population (Codori, Petersen, Miglioretti, & Boyd, 2001; Griffith, Passmore, Smith, & Wenzel, 2012; Madlensky, Esplen, Gallinger, McLaughlin, & Goel, 2003; Rawl et al., 2005; Zlot, Cox, Silvey, & Leman, 2012; Zlot, Silvey, Newell, Coates, & Leman, 2012).
Conclusions
To the best of our knowledge, the AN CRC Family Outreach Program is unique in the United States in its sustained and concerted efforts to gather information and provide outreach to relatives of CRC patients, and is the first and only program of its kind for AN or American Indian people. There has also been an increased focus in the United States on CRC screening in the general population, most notably through the 25 state and 4 tribal CRC Control Programs funded by the Centers for Disease Control and Prevention (Joseph, DeGroff, Hayes, Wong, & Plescia, 2011). However, the CRC Control Programs primarily target individuals at average risk for CRC. We are not aware of programs that utilize systematic outreach to individuals with an increased risk due to family history or personal history of CRC.
This qualitative study was undertaken to explore some of the initial factors that gave rise to the AN CRC Family Outreach Program, key elements of program success, and challenges to the continued growth and sustainability of the program. Representation from multiple groups of stakeholders, including clinical staff, program staff, and hospital leadership, made this process evaluation a strong and valuable source of information. Five key components were identified. Within the program formation and evolution components, it was notable that an incremental approach, whereby the CRC outreach activities were initially fragmented and somewhat disjointed, continual reflection toward improvement resulted in a well-developed program of service. Within the outreach responses component, key themes include the increasing trend in CRC screening awareness among the AN population and the increasing number of AN relatives screened for CRC. However, many relatives report a range of responses to the outreach they receive, which affect their participation in screening efforts. Within the successes and strengths component, a key theme was that dedicated patient navigators were vital for increasing screening in this population. Woven through the strengths and successes component was the support for program activities exhibited by key leadership within the organization, which was critical to the expansion of the program, along with successful attainment of program funding. However, within the barriers and challenges component, notable themes were the reliance on grant funding for program continuation, the continued need for dedicated staff time, and health system data access and coordination issues.
Implications for Policy and Practice
This study has important implications for policy and practice. The first is that even though the program began modestly, the focus on screening and the increasing use of data systems for measuring the impact of the program allowed it over the years to progressively grow and thrive. Other programs might consider building data tracking in the initial phases of the program design, as well as flexibility so that activities can be added incrementally as funding allows. Additionally, the use of dedicated patient navigators, especially staff who were themselves AN, and so could provide outreach that was culturally congruent to the relatives that they served, was essential to the success of the program. It is important that any program seeking to use patient navigators for outreach make sure that they have dedicated time to do the work, and a clearly defined role within the medical care setting so that they are able to carry out those activities (DeGroff, Coa, Morrissey, Rohan, & Slotman, 2013). Last, leadership support was cited as a key factor in the longevity of this program, despite concerns over reliance on grant funding for carrying out program activities. Selecting the right environmental supports and continuously working to engage leadership may help increase the sustainability capacity of other grant-funded programs seeking to do similar work (Luke, Calhoun, Robichaux, Elliott, & Moreland-Russell, 2014).
Several limitations of this study should be noted. Although the key findings can be used by other health organizations seeking to improve CRC screening outreach, especially for relatives of CRC patients, we were unable to compare and contrast the unique activities and process of the AN CRC Family Outreach Program with another program. Furthermore, the characteristics of the ATHS tend to limit the generalizability of these findings to other health care delivery systems. Last, although all interviews were audio recorded and two key informants provided additional information to confirm key points made during the interview, key components and themes were determined by one coder.
Overall, this process evaluation provided a rich source of information on the development, successful components and strengths, and barriers and challenges of a program to increase CRC screening among AN relatives of CRC patients. These findings have relevance for other programs and organizations working to systematically increase health seeking behaviors among populations experiencing significant health disparities.
Acknowledgments
We acknowledge the contributions and support of the Indian Health Service and the Alaska Native Tribal Health Consortium Board of Directors.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding for this study was provided by the Centers for Disease Control and Prevention, Division of Cancer Prevention and Control.
Footnotes
Authors’ Note
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Allison JE, Potter MB. New screening guidelines for colorectal cancer: A practical guide for the primary care physician. Primary Care. 2009;36:575–602. doi: 10.1016/j.pop.2009.04.009. doi:10.1016/j. pop.2009.04.009. [DOI] [PubMed] [Google Scholar]
- Boutron MC, Faivre J, Quipourt V, Senesse P, Michiels C. Family history of colorectal tumours and implications for the adenoma-carcinoma sequence: A case control study. Gut. 1995;37:830–834. doi: 10.1136/gut.37.6.830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Codori AM, Petersen GM, Miglioretti DL, Boyd P. Health beliefs and endoscopic screening for colorectal cancer: Potential for cancer prevention. Preventive Medicine. 2001;33(2 Pt 1):128–136. doi: 10.1006/pmed.2001.0862. doi:10.1006/pmed.2001.0862. [DOI] [PubMed] [Google Scholar]
- Cueva M, Dignan M, Kuhnley R. Readers’ Theatre: A communication tool for colorectal cancer screening. Journal of Cancer Education. 2012;27:281–286. doi: 10.1007/s13187-011-0295-y. doi:10.1007/s13187-011-0295-y. [DOI] [PubMed] [Google Scholar]
- Cueva M, Kuhnley R, Slatton J, Dignan M, Underwood E, Landis K. Telenovela: An innovative colorectal cancer screening health messaging tool. International Journal of Circumpolar Health. 2013;72:21301. doi: 10.3402/ijch.v72i0.21301. doi:10.3402/ijch.v72i0.21301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeGroff A, Coa K, Morrissey KG, Rohan E, Slotman B. Key considerations in designing a patient navigation program for colorectal cancer screening. Health Promotion Practice. 2013;15:483–495. doi: 10.1177/1524839913513587. doi:10.1177/1524839913513587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuchs CS, Giovannucci EL, Colditz GA, Hunter DJ, Speizer FE, Willett WC. A prospective study of family history and the risk of colorectal cancer. New England Journal of Medicine. 1994;331:1669–1674. doi: 10.1056/NEJM199412223312501. doi:10.1056/NEJM199412223312501. [DOI] [PubMed] [Google Scholar]
- Goodman L. Snowball sampling. Annals of Mathematical Statistics. 1961;32:148–170. [Google Scholar]
- Griffith KA, Passmore SR, Smith D, Wenzel J. African Americans with a family history of colorectal cancer: Barriers and facilitators to screening. Oncology Nursing Forum. 2012;39:299–306. doi: 10.1188/12.ONF.299-306. doi:10.1188/12.ONF.299-306. [DOI] [PubMed] [Google Scholar]
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qualitative Health Research. 2005;15:1277–1288. doi: 10.1177/1049732305276687. doi:10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- Indian Health Service . Alaska area aggregate GPRA [Government Performance and Results Act of 1993] clinical performance report, CRS [Clinical Reporting System] (Version 10.0) Alaska Area Native Health Service; Anchorage: 2012. [Google Scholar]
- Joseph DA, DeGroff AS, Hayes NS, Wong FL, Plescia M. The Colorectal Cancer Control Program: Partnering to increase population level screening. Gastrointestinal Endoscopy. 2011;73:429–434. doi: 10.1016/j.gie.2010.12.027. doi:10.1016/j.gie.2010.12.027. [DOI] [PubMed] [Google Scholar]
- Kelly JJ, Alberts SR, Sacco F, Lanier AP. Colorectal cancer in Alaska Native people, 2005-2009. Gastrointestinal Cancer Research. 2012;5:149–154. [PMC free article] [PubMed] [Google Scholar]
- Kiviniemi MT, Bennett A, Zaiter M, Marshall JR. Individual-level factors in colorectal cancer screening: A review of the literature on the relation of individual-level health behavior constructs and screening behavior. Psycho-Oncology. 2011;20:1023–1033. doi: 10.1002/pon.1865. doi:10.1002/pon.1865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhnley R, Cueva M. Learning about cancer has brightened my light: Cancer education for Alaska community health aides and community health practitioners (CHA/Ps). Journal of Cancer Education. 2011;26:522–529. doi: 10.1007/s13187-011-0207-1. doi:10.1007/s13187-011-0207-1. [DOI] [PubMed] [Google Scholar]
- Levin B, Lieberman DA, McFarland B, Andrews KS, Brooks D, Bond J, Winawer SJ. Screening and surveil-lance for the early detection of colorectal cancer and adenomatous polyps, 2008: A joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology. 2008;134:1570–1595. doi: 10.1053/j.gastro.2008.02.002. doi:10.3322/CA.2007.0018. [DOI] [PubMed] [Google Scholar]
- Luke DA, Calhoun A, Robichaux CB, Elliott MB, Moreland-Russell S. The Program Sustainability Assessment Tool: A new instrument for public health programs. Preventing Chronic Disease. 2014;11:130184. doi: 10.5888/pcd11.130184. doi:10.5888/pcd11.130184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madlensky L, Esplen MJ, Gallinger S, McLaughlin JR, Goel V. Relatives of colorectal cancer patients: Factors associated with screening behavior. American Journal of Preventive Medicine. 2003;25:187–194. doi: 10.1016/s0749-3797(03)00202-2. [DOI] [PubMed] [Google Scholar]
- Pariente A, Milan C, Lafon J, Faivre J. Colonoscopic screening in first-degree relatives of patients with “sporadic” colorectal cancer: A case-control study. The Association Nationale des Gastroenterologues des Hopitaux and Registre Bourguignon des Cancers Digestifs (INSERM CRI 9505). Gastroenterology. 1998;115:7–12. doi: 10.1016/s0016-5085(98)70358-0. [DOI] [PubMed] [Google Scholar]
- Patton M. Qualitative evaluation and research methods. Sage; Newbury Park, CA: 1990. [Google Scholar]
- Rawl SM, Menon U, Champion VL, May FE, Loehrer P, Sr., Hunter C, Skinner CS. Do benefits and barriers differ by stage of adoption for colorectal cancer screening? Health Education Research. 2005;20:137–148. doi: 10.1093/her/cyg110. doi:10.1093/her/cyg110. [DOI] [PubMed] [Google Scholar]
- Slattery ML, Kerber RA. Family history of cancer and colon cancer risk: The Utah Population Database. Journal of the National Cancer Institute. 1994;86:1618–1626. doi: 10.1093/jnci/86.21.1618. [DOI] [PubMed] [Google Scholar]
- St John DJ, McDermott FT, Hopper JL, Debney EA, Johnson WR, Hughes ES. Cancer risk in relatives of patients with common colorectal cancer. Annals of Internal Medicine. 1993;118:785–790. doi: 10.7326/0003-4819-118-10-199305150-00005. [DOI] [PubMed] [Google Scholar]
- Wahab S, Menon U, Szalacha L. Motivational interviewing and colorectal cancer screening: A peek from the inside out. Patient Education & Counseling. 2008;72:210–217. doi: 10.1016/j.pec.2008.03.023. doi:10.1016/j.pec.2008.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winawer S, Fletcher R, Rex D, Bond J, Burt R, Ferrucci J, Simmang C. Colorectal cancer screening and surveillance: Clinical guidelines and rationale—Update based on new evidence. Gastroenterology. 2003;124:544–560. doi: 10.1053/gast.2003.50044. doi:10.1053/gast.2003.50044. [DOI] [PubMed] [Google Scholar]
- Zlot AI, Cox SL, Silvey K, Leman R. The effect of chronic disease family history on healthcare provider practice and patient behavior among Oregonians. Public Health Genomics. 2012;15:189–200. doi: 10.1159/000335555. doi:10.1159/000335555. [DOI] [PubMed] [Google Scholar]
- Zlot AI, Silvey K, Newell N, Coates RJ, Leman R. Family history of colorectal cancer: Clinicians’ preventive recommendations and patient behavior. Preventing Chronic Disease. 2012;9:E21. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3277407/ [PMC free article] [PubMed] [Google Scholar]