Abstract
A zygomycetous fungus was observed in a biopsy of a 9-year-old male. The patient was presented with severe cutaneous lesions subsequent to a traumatic car accident. Following fungal detection, antifungal treatment was prescribed but condition deteriorated rapidly and above knee amputation was done as lifesaving and to control fungal infection. Analysis of the 28 S rRNA gene (accession KT149770) aligned the isolate with members of the genus Apophysomyces and the pathogen was identified as Apophysomces variabilis.
Keywords: Zygomycetes, Apophysomyces, Amputation, 28S rRNA gene, Aseer region
1. Introduction
Zygomycosis (mucormycosis) is a rare but often fatal infection caused by fungi in the class Zygomycetes. It usually affects persons with underling factors such as diabetes mellitus, metabolic acidosis, or immunodeficiency states [1], [2]. Zygomycetes are saprophytic fungi that are ubiquitous in soil or decaying organic material. The clinical manifestations of zygomycosis mainly are rhinocerebral, pulmonary, cutaneous, gastrointestinal, cardiac and cerebral disease [1]. The most common agent of zygomycosis is Rhizopus species, but other species in the order Mucorales such as Absidia, Mucor, Rhizomucor are also frequently seen, whereas Saksenaea vasiformis and Apophysomyces elegans are considered rare pathogens [2]. Many infections caused by Apophysomyces spp. have been reported including fatal necrotizing fasciitis in immunocompetent patients [3], [4]. Apophysomyces variabilis is considered an emerging species which is able to inflict significant diseases even among immunocompetent patients [5], [6]. We describe a case of cutaneous zygomycosis caused by a zygomycete in an immunocompetent 9-year-old child who had a trauma from a car accident.
2. Case
A 9 year old previously healthy child admitted to Aseer Central hospital, southern region of Saudi Arabia in January 3rd, 2014, with complaint of fever and swelling of the left leg of two weeks duration, following road traffic accident. The patient sustained condylar fracture of the left femur and lacerated wound of medial aspect of the left leg, initially seen in a peripheral hospital where he was given antibiotics and wound care, but fever continued and swelling progressed over several days.
The patient was admitted to Aseer Central Hospital after two weeks in the peripheral hospital in January 2014. On the first day of admission to Aseer Hospital, initial microbiology report stated the detection of Pseudomonas aeruginosa. Accordingly, the patient started on broad spectrum antibiotics that included intravenous vancomycin (Gulf Pharmaceutical Industries, UAE) at a dose of 10 mg/kg every six hours and intravenous meropenem (Astra Zeneca UK Limited) at dose of 20 mg/kg every eight hours, as well as debridement of the wound several times. No response to these measures was observed and the patient condition worsened with progression of wide spread necrosis of skin and soft tissue that extended from mid-thigh down to the left ankle (Fig. 1).
Fig. 1.
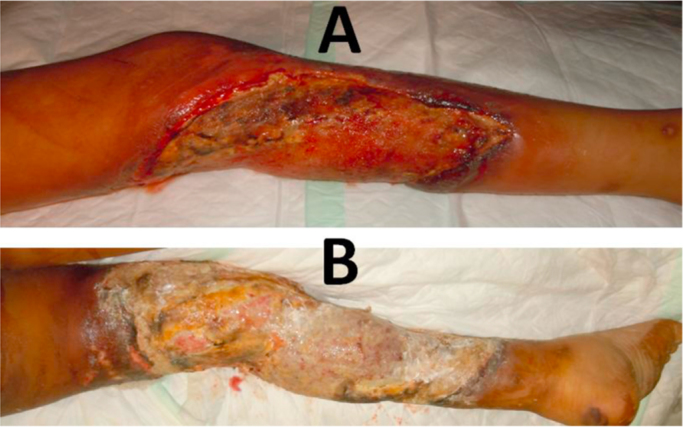
Massive ulcerated cutaneous zygomycosis lesions on the left leg of the 9 years old patient. Lesions seen after two weeks (A) and wide spread necrosis of skin and soft tissue that extended from mid-thigh down to the left ankle seen just prior to amputation (B).
On day three of hospital admission debrided tissues specimens were submitted to both histopathology and microbiology laboratories. Direct microscopy of smears from debrided tissues showed broad hyaline multinucleated asptate hyphae suggestive of a zygomycetous fungus (Fig. 2). Histopathology specimen from the debrided tissues showed aseptated broad hyaline hyphae.
Fig. 2.
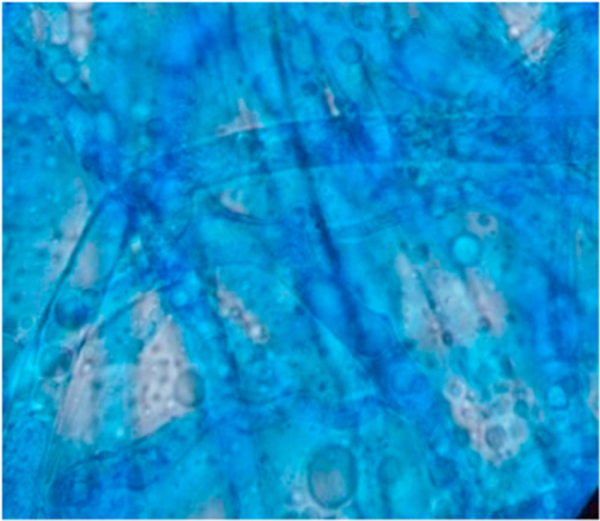
A direct microscopy micrograph of smear from debrided tissues obtained from the 9 year old male patient suffering from a subcutaneous wound infection. Note the broad hyaline multinucleated aseptate hyphae suggestive of a zygomycetous fungus.
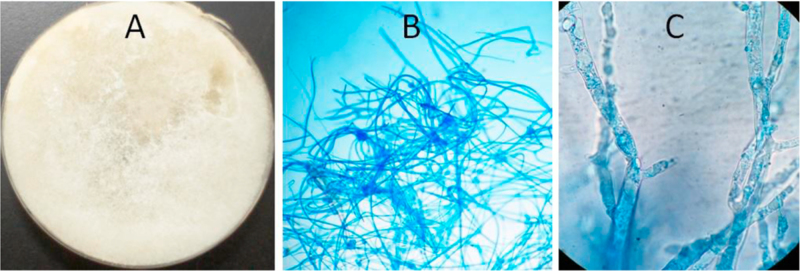
Culture was performed on Sabouraud dextrose agar (SDA) plates. Identification of the mold was done on the basis of colony morphology appeared on SDA and on microscopic features following recommended guiding principles [7]. Heavy mold growth on SDA from the purulent material was obtained after 3 days incubation at 30 °C (Fig. 3A). Under the microscope the mold shows broad aseptate hyaline hyphae which showed a unique type of sporangium (Fig. 3B and C).
Fig. 3.
Growth of the zygomatous fungus (AB7-1) on Sabouraud dextrose agar (A) showing heavy white mold. Under the microscope the mold shows broad hyaline aseptate hyphae (B, C).
On day three and following a positive mycological report, a combination of intravenous voriconazole and amphotericin B was started. Voriconazole (Pfizer Inc.) was given at a dose of 6 mg/kg each 12 h for the first 24 hours, then 4 mg/kg after; and amphotericin B (Gilead Science, Paris, France) at dose of 1 mg/ kg taken once daily for two weeks. This combination was launched trying to control the infection. But condition deteriorated more and fever continued, limb became non-viable and the patient admitted to pediatric intensive care unit with signs of septic shock. Above knee amputation was done as lifesaving and to control fungal infection. After amputation patient improved and discharged in good condition after one month of stay in hospital on oral itraconazole (SPIMACO) at 150 mg taken daily for one month to be followed up in OPD.
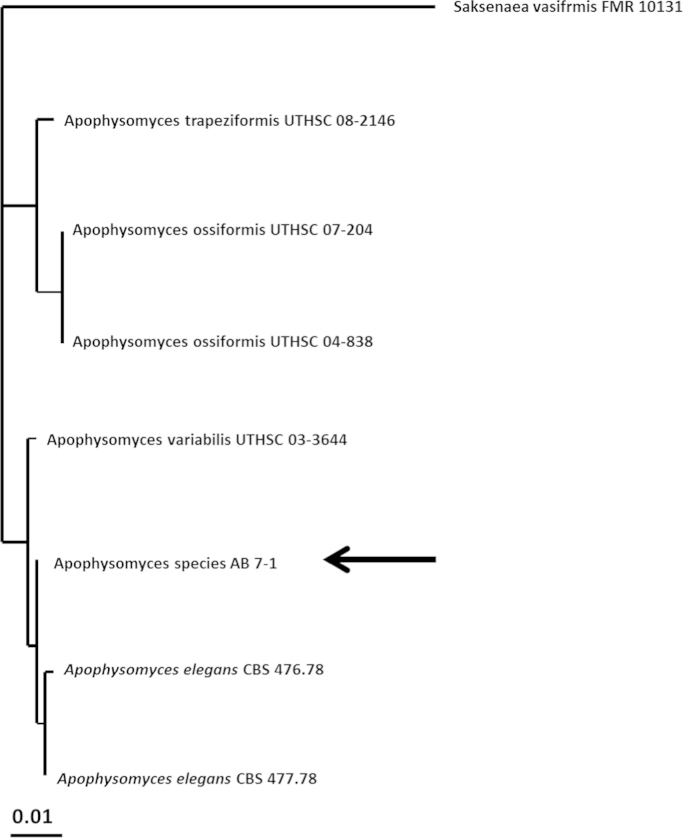
PCR amplification of the D1/D2 domains of the ribosomal large subunit (LSU) was performed [8]. Obtained nucleotide sequences (bp 709; Genebank accession number KT149770) were tested on the BLAST electronic system (http://blast.ncbi.nlm.nih.gov/Blast.cgi). Then sequences were analyzed using PHYDIT for Windows (Version 3.1., J. Chun) and in comparison to all known sequences of zygomycetes found in GenBank database. A phylogenetic tree was made using the neighbor-joining algorithm. Sequence analysis of domains D1 and D2 of the 28 S rRNA gene showed that the isolate belonged to members of the genus Apophysomyces and the pathogen was identified as Apophysomces variabilis (Fig. 4).
Fig. 4.
Estimate of Apophysomces phylogeny based on sequence analysis of domains D1 and D2 of the 28 S rRNA gene (accession KT149770) showing the taxonomic position of the strain AB7-1 (arrow) within members of the genus Apophysomces. The analysis shows that the strain is placed within a clade encompassing A. elegans and A. variabilis.
3. Discussion
Primary cutaneous zygomycosis is characterized by necrotic lesions and the fungus is usually inoculated by trauma [9]. We report a rare case of zygomycosis in a child. This infection might have been caused by an implantation of the fungus from soil via the traumatic car accident to the same degree as cutaneous zygomycosis generally [9], [10]. The present case is considered a primary cutaneous zygomycosis given the fact that the patient had undergone a traumatic injuries followed by soil contamination. This type of infections was described to occur rapidly and become invasive in up to 50% of cases involved in extensive soil contamination [11]. Similar cases have been described in the literature. Kordy et al. [12] reported a posttraumatic necrotizing fasciitis caused by Apophysomyces elegans in a child and many cases with various outcomes have been reviewed [13].
The case presented in this report was unfortunate to have gone through such a dreadful consequence. Initial assumption of a bacterial infection (two weeks in peripheral hospital and 2 days on central hospital) has worsened the condition of the child and obviously the fungus propagated heavily. If diagnosed early, a zygomycosis case is generally has a good prognosis [9]. In this study, the case was treated with a combination of amphotericin B and voriconazole. Studies have shown that only amphotericin B had good fungistatic activity against zygomycete fungi; whereas voriconazole has shown MICs ranged from 2 to>32 µg/ ml [14]. It is obvious that the use of amphotericin B rather than voriconazole had managed the infection. Few cases of cutaneous zygomycosis have been described in Saudi Arabia. A case was described in a 65-year-old Saudi immunocompetent male with no significant past medical history but the patient told he had a palm tree thorn prick [15]. A primary cutaneous zygomycosis that resembles necrotizing fasciitis in a young healthy Saudi male patient with a polytrauma was reported [16]. Their case had similar epidemiological and clinical pictures but this team has succeeded in achieving a complete recovery. They indicate early diagnosis by tissue culture and histopathology study as a prerequisite to successfully treatment [16].
Conflict of Interest
There are none.
References
- 1.Ribes J.A., Vanover-Sams C.L., Baker D.J. Zygomycetes in human disease. Clin. Microbiol. Rev. 2000;13:236–301. doi: 10.1128/cmr.13.2.236-301.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Linder N., Keller N., Huri C., Kuint J., Goldshmidt-Reuven A., Barzilai A. Primary cutaneous mucormycosis in a premature infant: case report and review of the literature. Am. J. Perinatol. 1998;15:35–38. doi: 10.1055/s-2007-993895. [DOI] [PubMed] [Google Scholar]
- 3.Ruiz C.E., Arango M., Correa A.L., Lopez L.S., Restrepo A. [Necrotizing fasciitis in an immunocompetent patient caused by Apophysomyces elegans] Biomedica. 2004;24:239–251. [PubMed] [Google Scholar]
- 4.Weddle G., Gandy K., Bratcher D., Pahud B., Jackson M.A. Apophysomyces trapeziformis infection associated with a tornado-related injury. Pediatr. Infect. Dis. J. 2012;31:640–642. doi: 10.1097/INF.0b013e31824bcc36. [DOI] [PubMed] [Google Scholar]
- 5.dela Cruz W.P., Calvano T.P., Griffith M.E., White C.E., Kim S.H., Sutton D.A., Thompson E.H., Fu J. Invasive Apophysomyces variabilis infection in a burn patient. J. Clin. Microbiol. 2012;50:2814–2817. doi: 10.1128/JCM.00671-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guarro J., Chander J., Alvarez E., Stchigel A.M., Robin K., Dalal U., Rani H., Punia R.S. Apophysomyces variabilis infections in humans. Emerg. Infect. Dis. 2011;17:134–135. doi: 10.3201/eid1701.101139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.D. Ellis. Mycology Online. Identification of Medically Important Fungi,. School of Molecular & Biomedical Science, The University of Adelaide, Australia 5005, 2014. http://www.mycology.adelaide.edu.au Accessed March 2014
- 8.Fliegerova K., Mrazek J., Voigt K. Differentiation of anaerobic polycentric fungi by rDNA PCR-RFLP. Folia Microbiol. (Praha) 2006;51:273–277. doi: 10.1007/BF02931811. [DOI] [PubMed] [Google Scholar]
- 9.Bonifaz A., Vazquez-Gonzalez D., Tirado-Sanchez A., Ponce-Olivera R.M. Cutaneous zygomycosis. Clin. Dermatol. 2012;30:413–419. doi: 10.1016/j.clindermatol.2011.09.013. [DOI] [PubMed] [Google Scholar]
- 10.Ajello L., Dean D.F., Irwin. R.S. The zygomycete Saksenaea vasiformis as a pathogen of humans with a critical rewiew of the etiology of zygomycosis. Mycologia. 1976;68:52–62. [PubMed] [Google Scholar]
- 11.Snell B.J., Tavakoli K. Necrotizing fasciitis caused by Apophysomyces elegans complicating soft-tissue and pelvic injuries in a tsunami survivor from Thailand. Plast. Reconstr. Surg. 2007;119:448–449. doi: 10.1097/01.prs.0000233624.34950.f8. [DOI] [PubMed] [Google Scholar]
- 12.Kordy F.N., Al-Mohsen I.Z., Hashem F., Almodovar E., Al Hajjar S., Walsh T.J. Successful treatment of a child with posttraumatic necrotizing fasciitis caused by Apophysomyces elegans: case report and review of literature. Pediatr. Infect. Dis. J. 2004;23:877–879. doi: 10.1097/01.inf.0000136870.17071.fd. [DOI] [PubMed] [Google Scholar]
- 13.Edlich R.F., Winters K.L., Woodard C.R., Britt L.D., Long W.B. 3rd. Massive soft tissue infections: necrotizing fasciitis and purpura fulminans. J. Long. Term. Eff. Med. Implant. 2005;15:57–65. doi: 10.1615/jlongtermeffmedimplants.v15.i1.70. [DOI] [PubMed] [Google Scholar]
- 14.Espinel-Ingroff A., Boyle K., Sheehan D.J. In vitro antifungal activities of voriconazole and reference agents as determined by NCCLS methods: review of the literature. Mycopathologia. 2001;150:101–115. doi: 10.1023/a:1010954803886. [DOI] [PubMed] [Google Scholar]
- 15.Al-Hedaithy M. Cutaneous zygomycosis due to Saksenaea vasiformis: Case report and literature review. Ann. Saudi Med. 1998;18:428–431. doi: 10.5144/0256-4947.1998.428. [DOI] [PubMed] [Google Scholar]
- 16.Al Barrag M.K., Al Zobydi A.H., Al Hazmi M.M., N.T M., Bakrain M.Y., Alsiddiky A.M. Post-traumatic Lethal Form of Primary Cutaneous Zygomycosis in a Healthy Young Patient and Review of the Literature. J. Taibah Univ. Med. Sci. 2009;4:162–169. [Google Scholar]