Abstract
Bioweapons are most often designed for delivery to the lung, although this route is not the usual portal of entry for many of the pathogens in the natural environment. Vaccines and therapeutics that are efficacious for natural routes of infection may not be effective against the pulmonary route. Pulmonary models are needed to investigate the importance of specific bacterial genes in virulence, to identify components of the host immune system that are important in providing innate and acquired protection, and for testing diagnostic and therapeutic strategies. This report describes the characteristics of host and Bacillus anthracis interactions in a murine pulmonary-infection model. The infective dose varied depending on the route and method of inoculation. The germination process in the lung began within 1 h of inoculation into the lung, although growth within the lung was limited. B. anthracis was found in the lung-associated lymph nodes ∼5 h after infection. Minimal pneumonitis was associated with the lung infection, but significant systemic pathology was noted after dissemination. Infected mice typically succumbed to infection ∼3 to 4 days after inoculation. The 50% lethal doses differed among inbred strains of mice, but within a given mouse strain, neither the age nor the sex of the mice influenced susceptibility to B. anthracis.
Bacillus anthracis is a gram-positive, spore-forming, rod-shaped bacterium that causes the disease anthrax (21). Anthrax is predominantly a disease of herbivores, and humans usually become infected through incidental exposure during animal handling. B. anthracis resides in the soil as a spore, and the spores typically enter the herbivore through ingestion and germinate into a vegetative state in tissues. The signals for germination include amino acids, nucleosides, and glucose (2, 30, 31). Once in the vegetative state, the organism multiplies rapidly and produces two important toxins that contribute to the pathology of the infection. Pathogenesis is thought to be due to the effects of toxins and to the high number of organisms that reach critical target organs (3, 19, 35, 41).
Anthrax in humans may take three forms, i.e., cutaneous, gastrointestinal, and pneumonic. The most common form of human anthrax is cutaneous anthrax, typically caused by the inoculation of spores into open wounds on the extremities of animal handlers, e.g., wool sorter's disease (28, 37). Cutaneous anthrax is a disease with a mortality approaching 20% in the untreated. Naturally acquired pulmonary anthrax is very unusual, occurring about 1/20 as often as cutaneous anthrax. However, when respiratory anthrax occurs, it has a mortality approaching 100% if not treated early (21).
The United States has been aware of the potential use of B. anthracis spores as inhaled weapons of bioterrorism for many years and was exploring its use as a bioweapon until offensive bioweapons work was terminated in 1969 and 1970 (8). Awareness of this threat was heightened following the use of the U.S. mail system to disseminate a weaponized form of B. anthracis spores and to induce pulmonary disease in those receiving and handling contaminated mail in the fall of 2001 (11).
The pathogenesis of anthrax, particularly inhalational anthrax, is complex, and most studies have examined in vitro cell culture models in an attempt to understand the early stage of infection. B. anthracis spores that are dispersed into 1- to 5-μm-diameter particles are likely inhaled into the alveolar spaces of the lung (6). The spores are presumed to be phagocytosed by alveolar macrophages (20). The phagosomes fuse with lysosomes to produce phagolysosomes. Many spores may be killed in the phagolysosomes, but surviving spores may remain in the lung, or those escaping phagocytosis may drain via lymphatics into the mediastinum, where they may exist as spores for an undetermined length of time. Once spores are inside macrophages, the surviving spores can undergo germination to a vegetative state (13), although whether macrophages are absolutely required for germination in vivo is unclear. After germination, the symptoms of infection follow as a result of the rapid replication of the organisms and the release of toxins. The toxins of B. anthracis consist of combinations of two different proteins: either protective antigen (PA) plus lethal factor or PA plus edema factor (5, 25, 29). An additional known virulence factor is the capsule of the vegetative form. The genes for the three protein components of the toxins are carried on the plasmid pXO1, and the capsule is encoded by the plasmid pXO2 (24). PA is a receptor-binding protein that facilitates the transport of edema factor and lethal factor into target cells. The toxins act to inhibit an effective immune response against B. anthracis and directly damage cells (7, 25, 29). The role of the capsule has not been extensively studied, but experiments using an acapsular Sterne B. anthracis strain that lacks the plasmid pXO2 showed that the capsule has antiphagocytic properties that facilitate the infectious process (40). Host-related signals that affect the transcription of the toxin and capsule genes include temperature and the bicarbonate-CO2 balance. Additional genes that may play roles in B. anthracis virulence include a germination operon, gerX, and a stress transcription factor gene (24).
The development of well-characterized models of pneumonic anthrax is essential in order to understand its pathogenesis, as well as to discover new, more effective vaccines and microbicidal agents. The majority of animal models for anthrax were used to test the efficacy of vaccines against anthrax, and little immunopathology was described. Mice, in particular, were used extensively for testing vaccines (4, 7, 10, 23, 33). Most murine studies used a subcutaneous (s.c.) infection route, but one study described the use of an intratracheal (i.t.) infection model to examine the role of irradiation in pulmonary anthrax infection (14). For virulent B. anthracis, the s.c. 50% lethal dose (LD50) was reported to be 6 to 25 spores (40). The present report compares the intranasal (i.n.) and i.t. routes for modeling inhalation anthrax in mice with the Ames strain of B. anthracis spores and describes the rate of germination, kinetics of dissemination, and histopathology. Finally, the model was used to test the hypothesis that genetics and age are determinants of susceptibility to B. anthracis.
MATERIALS AND METHODS
B. anthracis spore preparation.
The original B. anthracis (Ames strain) spore stock (BA-O) was obtained from the U.S. Army Medical Research Institute of Infectious Diseases, Frederick, Md. To provide a new working stock (BA-NS-1), a sample of the original strain was streaked onto a blood agar plate (Remel, Lenexa, Kans.) and incubated overnight at 37°C. Prewarmed 2× SG medium (24a) was then inoculated with one colony from the overnight plate culture and incubated at 37°C on a shaker. A sample from this preculture (1.25 ml) was added to 50 ml of 2× SG medium (prewarmed) in a 500-ml filter-top plastic flask and shaken for 24 h. At the end of the 24-h period, 200 ml of sterile double-distilled H2O was added to the culture, and incubation was continued with shaking for 40 more hours. After the 40-h incubation, the sporulation of the culture was evaluated, and no vegetative cells were observed by phase-contrast microscopy. The culture was then transferred to a sterile Oakridge tube and spun in a Sorvall Superspeed centrifuge using an SS-34 rotor at 4,000 rpm and 4 to 10°C for 20 min, washed one time with sterile phosphate-buffered saline (PBS), and resuspended in 50 ml of sterile PBS. The culture was heated to 68°C for 40 min prior to further preparation to remove potentially contaminating vegetative cells. Aliquots of the final solution were transferred into vials and frozen at −80°C. The titer of the new stock was determined by plating serial dilutions onto blood agar plates using a spiral plater (Spiral Biotech, Bethesda, Md.).
Inoculum.
An aliquot of the BA-NS-1 working stock was removed from the freezer and thawed to room temperature in a biohazard hood. The stock was then diluted in serial dilutions with sterile PBS to a desired concentration.
Animals.
Mice were purchased and maintained as specific pathogen free. For most studies, female BALB/c mice were obtained from Harlan (Madison, Wis.) and were between 6 and 8 weeks of age. For analysis of strain sensitivity, mice were obtained from Harlan or Jackson Laboratories (Bar Harbor, Maine), depending on availability, and were between 6 and 10 weeks of age. Both male and female mice were tested. For the experiments evaluating differences among inbred strains of mice, all mice in the experiment were age and sex matched. The mice were housed five per cage in the vivarium located at the University of New Mexico in autoclaved, individually ventilated (HEPA-filtered) cages (Tecniplast, Phoenixville, Pa.) with autoclaved Tek-Fresh (Harlan) bedding. The mice had access to irradiated food (Harlan) and autoclaved water ad libitum. The animals were allowed to acclimate for at least 7 days prior to being used in experimental studies. All protocols were approved by the University of New Mexico Institutional Animal Care and Use Committee.
Animal inoculations.
All mice were inoculated and kept in an animal biosafety level 3 containment area. For i.n. inoculations, mice were lightly anesthetized with isoflurane, and a 50-μl inoculum was placed on the nares for inhalation into the lungs. For i.t. inoculations, mice were anesthetized with avertin and restrained on a small board, a small incision was made through the skin over the trachea, and the underlying tissue was separated. A bent 30-gauge needle attached by sterile polypropylene tubing to a tuberculin syringe was used; the needle was inserted into and parallel with the trachea, and a 50-μl inoculum was delivered into the lung. Thirty minutes after i.n. or i.t. inoculations, lungs from three random mice were harvested and homogenized, and dilutions were plated on sheep blood agar plates to determine the number of organisms deposited into the lung. For s.c. inoculation, doses of spores were delivered in a total volume of 200 μl of PBS using a 29-gauge needle attached to an insulin syringe.
LD50 and mean time to death (MTD).
For determination of LD50s, 10 mice per group per dose of B. anthracis were used. The LD50 was calculated according to the method of Reed and Muench (34). The MTD was calculated by averaging the time of death for all individuals that died within a group.
Determination of organ CFU.
Lungs were removed after euthanasia by opening the chest cavity and cutting the trachea at the bifurcation. Lung CFU were determined by homogenizing the entire lung in 1 ml of sterile PBS in tubes using a bead beater. The homogenates were serially diluted and plated on sheep blood agar plates using a spiral plating system. Colony counts were determined using an automated counter scanner system (Spiral Biotek). For some studies, half of the homogenate was heated (40 min at 68°C) prior to plating. Viability after heat treatment was taken as a measure of the population of dormant spores. To control for the potential of cross-contamination during the harvesting and plating procedures in the lung-associated lymph node (LALN) harvest, naïve uninfected mice were randomly harvested along with infected mice, and their LALNs were plated as well. All uninfected mice had zero colonies in their LALNs (data not shown).
Histopathology.
Each mouse received 10,000 spores i.t., and groups of three mice were euthanized at selected intervals with an overdose of avertin. The lungs were inflated with ∼1 ml of 10% buffered formalin prior to being removed from the chest cavity. The lungs and other organs were then placed in 10% formalin for >24 h prior to being processed. Sectioned tissues were stained with hematoxylin and eosin prior to evaluation. A minimum of three mice were evaluated at each time point by a board-certified veterinary pathologist (J.H.).
Statistical analysis.
Comparisons among multiple groups of nonparametric data were statistically evaluated by Kaplan-Meier and Logrank (Mantel-Cox) analyses using the StatView statistical program (version 5.0.1; SAS Institute, Cary, N.C.). Differences were considered significant at P values of <0.05.
RESULTS
Determination of LD50s for i.n. versus i.t. delivery methods.
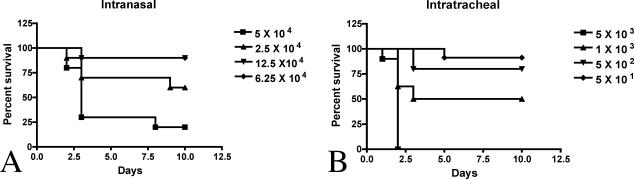
Previous studies had reported that the LD50 for spores delivered s.c. was 6 to 25 spores (40). Our results support this finding (Table 1). We next compared two different methods for lung delivery and determined the LD50 for each. BALB/c mice were challenged either i.n. or i.t. with a range of doses of B. anthracis spores, and survival was monitored (Fig. 1). The efficiency of establishing an infection varied significantly between the two methods. The LD50 for BALB/c mice was found to be ∼37,000 spores using the i.n. method and ∼1,000 spores using the i.t. method (Table 1); 100,000 spores were commonly required for 80 to 90% mortality via an i.n. inoculation, while only 5,000 spores were needed for 100% mortality when given i.t. In addition, the MTD was slightly increased for the i.n. route compared to the i.t. route.
TABLE 1.
LD50s for B. anthracis delivered i.n., i.t., or s.c.a
| Route of inoculum | LD50 (no. of spores) | MTD (days) |
|---|---|---|
| i.n. | 37,000 | 3.1 |
| i.t. | 870 | 2 |
| s.c. | 19 | 3.6 |
Groups of female BALB/c mice were challenged with four different doses (10 mice/dose) of B. anthracis spores either i.n., i.t., or s.c., and survival was monitored. Two different experiments were performed for each route. Calculations were based on the inoculum lung depositions recorded for each of the four doses.
FIG. 1.
Survival curves for mice infected i.n. (A) versus i.t. (B) with different doses of B. anthracis Ames strain spores. Groups of female mice (10/group) were infected i.n. or i.t. (as described in Materials and Methods) with the doses shown. Lung depositions were determined in three random mice from each group to assess the actual dose that was delivered to the lung.
Efficiency of spore germination induction between the two routes of inoculation.
We hypothesized that one of the reasons for the difference between the LD50s for the i.n. and i.t. inoculation methods was that the i.t. method delivered a higher number of spores deeper in the lung, where the environment may be optimal for rapid germination. To test this hypothesis, we examined the efficiencies of germination for the two inoculation methods. We took advantage of the fact that spores are resistant to heating at 68°C for 40 min, while spores that have started the germination process are sensitive to this heating process. Lungs were harvested in two different ways to assess whether significant numbers of spores remained in the trachea and large bronchi after delivery by the two different methods: (i) individual lobes were removed from the bronchial tree as close to the lung parenchyma as possible, and (ii) whole-lung homogenates were collected by cutting across the bronchi at the bifurcation of the trachea. No significant difference was observed between the numbers of CFU recovered by the two methods, indicating that both methods delivered similar numbers of spores into the lung airways. Lung tissues were subsequently homogenized at different time points after i.n. or i.t. inoculation, and half of the sample was heated, while the remaining sample was not. Both samples were plated, and the numbers of CFU were determined. The germination efficiency was defined as follows: number of CFU recovered from the unheated sample − number of CFU recovered from the heated sample/number of CFU recovered from the unheated samples × 100. Within 1 h postinoculation, the germination efficiencies were ∼90% for the i.n. route and 97% for the i.t. route. These kinetic data were comparable to the heat sensitivity of spores in in vitro experiments where spores were exposed to germinants (22).
Pathology associated with i.t. and i.n. spore administration.
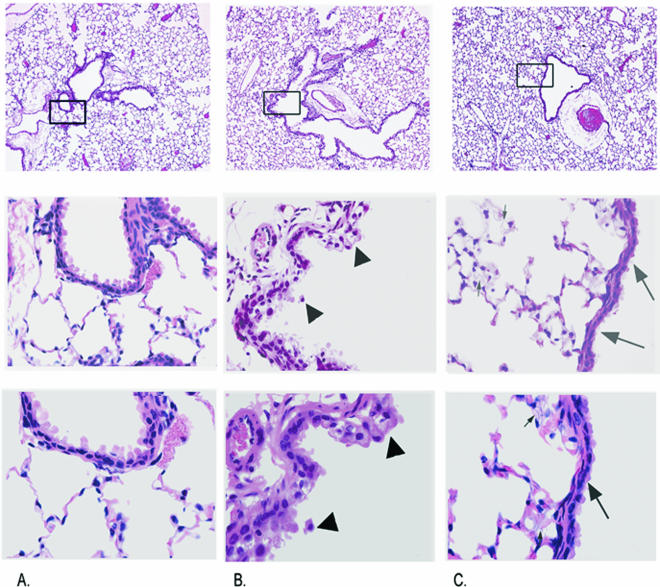
The pulmonary and extrapulmonary lesions that developed following either an i.t. or an i.n. inoculation of B. anthracis were similar. Figures 2 and 3 demonstrate the typical histologic lesions of anthrax in the lung and spleen, respectively, from BALB/c mice exposed to B. anthracis by the i.t. route. At 3 to 5 h postexposure, there were no significant lesions detected in the lungs (data not shown). After 24 h, there was acute, mild, widespread swelling and vacuolar degeneration with occasional sloughing and necrosis of conducting airway epithelial cells (compare Fig. 2A and B). Multifocal, mild attenuation of conducting airway epithelium, interpreted as epithelial sliding to cover defects left by sloughed and dead epithelial cells, was also evident. Infrequently, small foci of minimal fibrinosuppurative to histiocytic alveolitis were evident in random alveoli. In the spleen at 24 h, a mild increase in intravascular neutrophils was evident, along with infrequent to occasional foci, consistent with lymphocyte apoptosis, i.e., nuclear fragmentation without necrosis (data not shown).
FIG. 2.
Anthrax-induced lung pathology in BALB/c mice. The top image in each panel is a low-magnification view showing the area of focus for the high magnifications below. (A) Uninfected control mice. (B) Twenty-four hours postexposure. (C) Forty-eight hours postexposure. Note the vacuolar degeneration and sloughing of bronchiolar epithelium at 24 h (arrowheads). At 48 h, the epithelium is attenuated (large arrows). Myriads of vegetative B. anthracis bacilli are present within alveolar capillaries (small arrows). Magnifications, ×40 (top), ×220 (middle), ×400 (bottom).
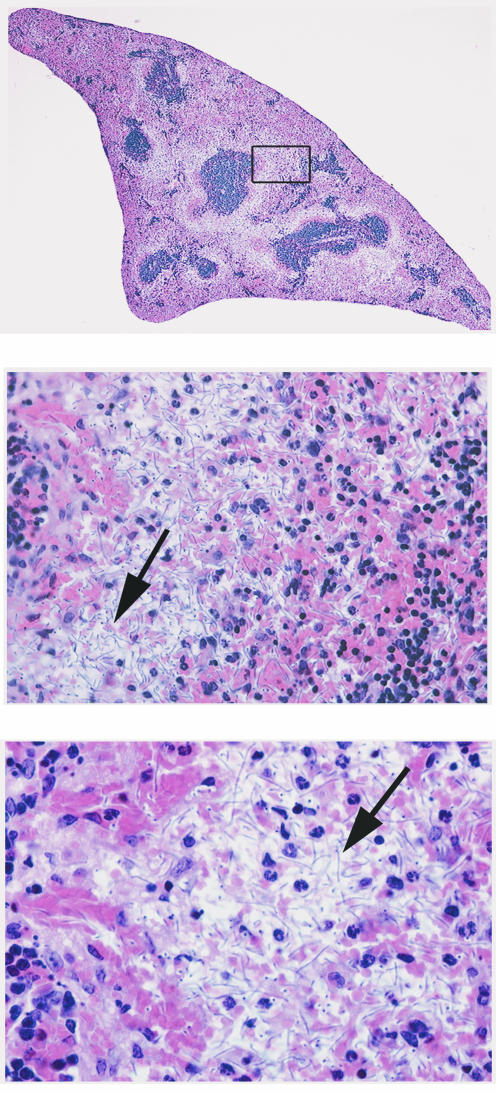
FIG. 3.
Anthrax-induced spleen pathology in BALB/c mice 48 h postexposure. There are necrosis of the red pulp with hemorrhage, neutrophilic inflammation, fibrin exudation, and myriads of bacilli (large arrow). Magnifications, ×50 (top), ×280 (middle), ×500 (bottom).
After 48 h, mild, widespread attenuation of the conducting airway epithelium was still evident in the lungs, although the vacuolar degeneration and death of epithelial cells were substantially reduced (compare Fig. 2B and C). Most mice had many bacterial rods diffusely distributed within the alveolar capillaries and, to a lesser extent, within the larger pulmonary vessels (Fig. 2C). Alveolar inflammation was typically infrequent to nonexistent (Fig. 2C). Occasionally, there were minimal to mild fibrinosuppurative and histiocytic infiltrates in the adventitia of large pulmonary veins late in the infection. Finding bacilli in alveolar capillaries correlated with massive numbers of bacilli in the spleen as well. These mice had massive necrotizing splenitis (red pulp) with variable congestion, hemorrhage, and fibrin deposition and aggregates of cells with nuclear fragmentation consistent with apoptotic lymphocytes (Fig. 3). Occasionally, the only splenic lesion after 48 h was a slight increase in intravascular neutrophils and minimal to mild lymphocyte apoptosis, with only small numbers of intrasinusoidal bacterial rods. The lungs of these same mice typically had only rare bacilli or no evidence of bacilli within alveolar septae, suggesting that the dissemination phase in these mice was in its early phase.
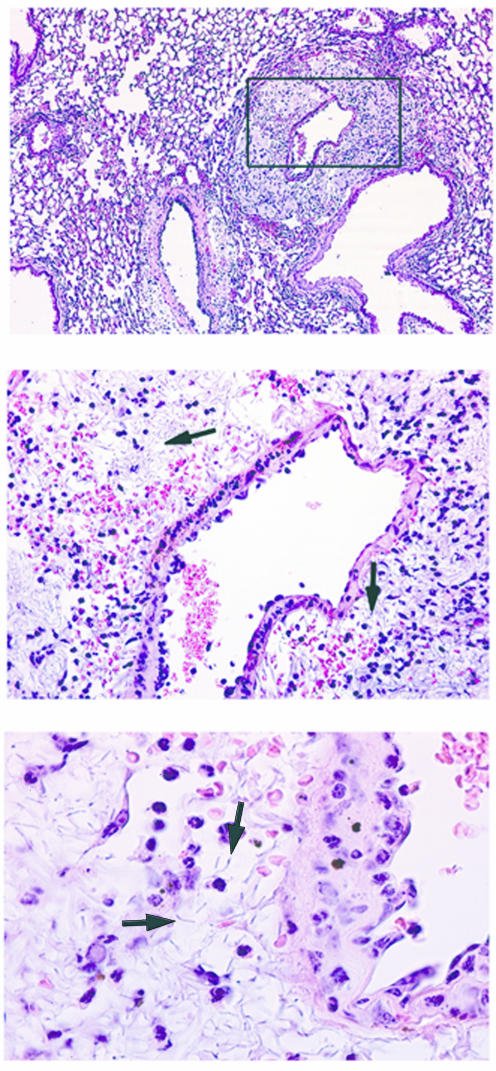
On rare occasions, the lungs showed evidence of vasculitis and perivasculitis with bacilli in the absence of systemic dissemination (Fig. 4). In these mice, the growth of bacilli in the adventitia of large vessels suggested the possibility of local spread of bacilli to or from the mediastinum.
FIG. 4.
Pulmonary blood vessel pathology in anthrax-infected mice. Focal vasculitis with abundant perivascular bacilli (arrows) was observed, although rarely, in the lungs after 24 to 48 h, without evidence of dissemination. Magnifications, ×50 (top), ×280 (middle), ×500 (bottom).
Tissues other than spleen and lung were examined histologically in a subset of mice. In mice with disseminated B. anthracis, nuclear fragmentation was consistently observed in several lymph node groups, whether or not bacteria were evident. Abundant bacteria were also evident in the kidneys of mice with disseminated B. anthracis, especially in the glomeruli, but inflammatory changes were consistently absent. Other lesions occasionally observed in mice with disseminated anthrax included nuclear fragmentation within endothelial cells lining the hepatic and adrenal sinusoids, with a few bacterial rods occasionally observed in the sinusoids. In addition, there were several small intracerebral vessels in one mouse that had intravascular fibrin thrombi with fibrinoid necrosis of the vessel wall. Rare intravascular bacteria were evident within vessels in this mouse when gram-stained sections were examined. The brains of other mice were without detectable bacteria or lesions.
Kinetics of dissemination following pulmonary spore administration.
B. anthracis extrapulmonary spread is likely a multistep process requiring germination, establishment of local infection, and then dissemination. Previous studies by Ross in a guinea pig model demonstrated that B. anthracis organisms reached the draining lymph nodes of the lung between 4 and 5 h after i.t. inoculation of 50,000 spores (35). We determined whether this timing was similar in the murine i.t. model. We inoculated mice with two different dosages of B. anthracis (5,000 and 50,000 spores), and the LALNs were harvested 5 h later. Two out of five mice receiving 5,000 spores had detectable bacteria (1 to 2 CFU) in their LALNs, while five out of five mice that received 50,000 spores had detectable colonies (range, 5 to 387 CFU) in their LALNs. No LALNs were detected on the second day of infection, suggesting that they had undergone complete cytolysis. This is consistent with reports of severe lymphocytolysis that occurs during human inhalational anthrax (18).
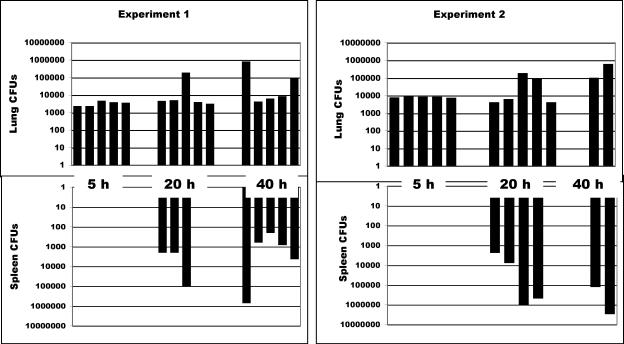
We also examined the kinetics of extrapulmonary dissemination in the murine model. BALB/c mice were challenged i.t., and lungs and spleens were harvested at different time intervals after inoculation. Figure 5 shows that dissemination occurred between days 1 and 2, which was consistent with the onset of severe clinical symptoms usually observed on day 2 or 3, followed by death 4 to 8 h later. The number of CFU recovered from the lungs remained constant and did not increase prior to detection of CFU in the spleen. We speculate that the significant increase in lung-associated CFU noted on days 2 and 3 was likely due to organisms trapped in the pulmonary capillaries following systemic dissemination, as observed in the histological specimens.
FIG. 5.
Increases in numbers of lung CFU following i.t. inoculation of B. anthracis occurs coincident with colonization of the spleen. Mice were inoculated i.t. with ∼5,000 spores of B. anthracis. The data represent two separate experiments. Mice (five per group) were euthanized at 5, 20, and 40 h postinoculation, and the numbers of CFU in the lung and the spleen were determined. In experiment 2, only two mice were alive at the 40-h time point. The upper graphs show numbers of lung CFU at the three time points, and the lower graphs show numbers of splenic CFU. Each lane in the upper graphs represents a single mouse, and the lower bars show the corresponding splenic CFU.
LD50 differences among different mouse strains.
Previous work on the genetic differences in anthrax susceptibility among inbred mouse strains concentrated on the s.c. route of infection (39, 40). Very little information is available about whether the infective dose varies among different strains of mice when delivered into the lung. We challenged mice of different genetic backgrounds with B. anthracis spores by the s.c., i.n., or i.t. route and compared the LD50s (Table 2). The s.c. route showed the lowest LD50, but no significant difference was observed among the tested mouse strains. In contrast, significant LD50 differences were noted among different strains of mice after pulmonary challenge. BALB/c mice were the most resistant, whereas DBA/2, C3H, and A/J mice were the most sensitive. The pattern of sensitivity was identical for the i.n. and i.t. routes, although as previously shown (Table 1), more organisms were consistently required for a productive infection via the i.n. route. Separate studies were conducted in male and female mice. No difference in susceptibility was observed between males and females in any mouse strain (data not shown).
TABLE 2.
LD50s for different mouse strains challenged by different routes of infectiona
| Route | LD50 (no. of spores)
|
|||||
|---|---|---|---|---|---|---|
| BALB/c | DBA/2 | C3H | 129X1/SVJ | C57BL/6J | A/J | |
| s.c. | 19 | 5 | 5 | 5 | 19 | 5 |
| i.n. | 37,000 | <6,250 | 6,250 | 25,000 | 12,500 | 6,250 |
| i.t. | 870 | 35 | 24 | ND | 500 | ND |
Mice were infected with four different doses (10 mice/dose) of B. anthracis spores by either an s.c., i.n., or i.t. inoculation, and the LD50 was determined. Different mouse strains were analyzed in parallel for each infection route. For the s.c. and i.n. routes one experiment was performed with all male mice (40 mice/strain) and one experiment was performed with all female mice (40 mice/strain, except no female A/J mice were used). All female mice were used in the i.t. experiment (40 mice/strain). ND, not done.
Effect of age on pulmonary infection.
A potential influence of age on susceptibility to aerosol anthrax was investigated, due to the high incidence of lethal anthrax cases that developed in middle-aged humans exposed to anthrax during the 1979 accident at Sverdlosk or in the 2001 post office exposures in the United States (16, 17, 26). Previous studies analyzing a variety of immune parameters have suggested that both mice and humans develop immune defects with increasing age (9, 32). Therefore, 3- and 22-month-old C57BL/6 mice purchased from the National Institute on Aging were challenged with four different doses of B. anthracis spores, as shown in Fig. 1, and the LD50s were determined. The LD50 of 22-month-old mice was 12,500 spores, and that for the 3-month-old mice was 15,800 spores.
DISCUSSION
We compared two pulmonary routes of infection for B. anthracis, and described the rates of germination, extrapulmonary spread, and histopathology with the goal of establishing a well-characterized model for understanding the pathobiology of pulmonary anthrax. We also showed that there is genetic variability in susceptibility to anthrax. However, no difference was observed between the sexes, and the data from one mouse strain suggest that age is not a factor.
Pulmonary models of infectious agents have typically utilized one of three strategies to deliver organisms into the lung, i.e., aerosolization, i.n. inoculation, or i.t. inoculation. Each of these methods has advantages and disadvantages. Nose-only aerosolization has the advantage of delivering the bacteria in a manner most similar to a bioweapon and, if performed correctly, will deliver organisms to the deep lung. The disadvantages include the technical challenge of delivering identical doses reproducibly, the safety hazards associated with aerosolization of biothreats, and the fact that the delivery of particles to the alveolar region is very inefficient in rodents (36). Mice often swallow the majority of inhaled particles rather than depositing them in the lung. Thus, the exposure to the gut during an aerosol exposure is great and may influence the infectious process. The i.n. method requires manipulations and the ability to get the mouse to breathe at an appropriate rate to inhale the majority of inoculum. Depending on the characteristics of the bacteria and vehicle, some bacteria are delivered to the upper airways as well as the lower airways. There is a small amount of liquid that accompanies the inoculum that may also be swallowed by the mouse. The primary advantage is that the technique is easily transferred from laboratory to laboratory, and the doses delivered are reproducible once the technique is mastered. The i.t. route is also technically challenging and invasive but delivers reproducible numbers of CFU to the lung while minimizing delivery to the upper airways or gut. Still, we recognize that some of the i.t. bolus may be exhaled and then swallowed. For this reason we use the absolute deposition dose in the lungs from random mice, rather than the inoculum, to describe i.t. or i.n. doses. For this report, we chose to compare the i.n. and i.t. routes of infection primarily because they deliver a more accurate and reproducible dose to the lungs than aerosol delivery and are less hazardous.
The pathogeneses of pulmonary anthrax were similar following either the i.n. or i.t. route of infection. The primary differences between the two models were the lower LD50 associated with the i.t. route of delivery and, in our hands, the improved efficiency of establishing an infection with the i.t. method. The difference in LD50 may be due to the mechanics of delivery. The i.t. method likely delivers a more reproducible dose of organisms to the deeper lung than the i.n. route, although increasing the i.n. dose appears to overcome this problem. While fewer mice were reproducibly infected by the i.n. route than by the i.t. route, the kinetics of morbidity and mortality were similar for the mice that did become infected. Mice inoculated by either route died ∼48 to 96 h postinoculation, although in general, mice that received an i.t. dose died closer to the 48-h time point and mice inoculated i.n. died closer to the 72-h time point.
For purposes of studying host-pathogen interactions, the optimal model would be one in which the paces of infection in each organ and tissue compartment are nearly synchronized in all groups of infected mice following inoculation. Unfortunately, the pulmonary-anthrax model demonstrates variability even among members of a single inbred mouse strain inoculated at the same time. This variability should probably be expected because of the complicated pathway B. anthracis requires for dissemination (i.e., germination, virulence factor production, and lung penetration). The best representation of the lack of synchrony in the infection was the variability in the number of organisms that had disseminated to the LALN 5 h after an i.t. delivery of 50,000 spores to the lung. Because the bacteria grow exponentially postdissemination, differences are likely amplified over the course of infection, as demonstrated by the splenic CFU data and the differences in the times to death within a single inoculum dose.
The pulmonary and splenic lesions observed in BALB/c mice after i.t. inoculation with B. anthracis spores were qualitatively similar to the lesions observed after i.n. inoculation. Most mice showed evidence of disseminated anthrax infection by 48 h. Differences between mice in the timing of lesion development and the overall severity of lesions were probably the result of variations in the rate of dissemination. The most consistently identified pathological lesions of disseminated anthrax appeared in the spleen. After 48 h, these lesions ranged in severity from mild lymphoid necrosis with few or no detectable bacilli to the more common lesion of severe necrotizing and hemorrhagic splenitis with many bacilli. Pulmonary changes at 48 h consisted primarily of diffuse distention of septal capillaries with bacilli, with minimal to no parenchymal inflammation. In a few cases, there was mild, acute, perivascular fibrinosuppurative and histiocytic inflammation involving the hilar aspects of large pulmonary vessels. Those mice with mild splenic lesions and few splenic bacilli often were without bacilli in the pulmonary septal capillaries, and those mice with severe splenic lesions and many splenic bacilli always had many bacilli in the pulmonary septal capillaries. None of the mice had diffuse septal bacilli without detectable bacilli in the spleen. The tight correlation between the presence of splenic bacilli and lung bacilli and the diffuse nature of the intraseptal distribution of lung bacilli are consistent with hematogenous spread of the bacilli back to the lungs after systemic dissemination.
Focal pulmonary vasculitis and perivasculitis with abundant perivascular bacilli occurred, but without the presence of diffuse pulmonary septal bacilli or splenic bacilli. We interpreted these cases as representing local proliferation of bacilli within the lungs without systemic distribution. Alternatively, this focal finding might indicate local spread from the mediastinum to the lungs via the connective tissue associated with the major pulmonary vasculature.
The splenic and pulmonary lesions described in humans or nonhuman primates that died following inhalation exposure to B. anthracis spores are very similar to those observed in mice after i.t. inoculation (1, 12, 15, 38). Splenic lesions are characterized by splenomegaly, with congestion, hemorrhage, necrosis, and many intrasinusoidal bacilli. Lung changes are characterized by pulmonary septal bacilli with minimal to no inflammation in most humans and primates with disseminated anthrax. In addition to the splenic and pulmonary changes, humans and primates with disseminated anthrax also demonstrate hemorrhagic mediastinal lymphadenitis, mediastinal edema and hemorrhage, hemorrhagic meningitis, and gastrointestinal submucosal hemorrhages. Scattered foci of necrotizing vasculitis have been identified in multiple organs in more severe cases.
Recently, the pathological effects of B. anthracis lethal toxin exposure were explored in BALB/c mice (27). Major lesions were identified in the spleen, bone marrow, and liver. Prominent hepatocellular centrilobular necrosis was attributed to lethal toxin-mediated liver hypoxia, with subsequent hypoalbuminemia leading to pleural effusion. The prominent hepatocellular necrosis observed with lethal toxin exposure in mice is in contrast with our results using spores inoculated i.t. We noted minimal pathological changes other than infrequent sinusoidal endothelial necrosis. The differences are likely due to the presence of other B. anthracis virulence factors in the spore inoculation model that contribute to host pathology and death before lethal toxin production reaches high enough levels to cause significant liver pathology. Future studies are planned to quantitate the toxin levels following infection with live spores.
The consequences of B. anthracis delivery via the pulmonary route have been examined histologically in different animal models and following two different human population exposure events. Information from these studies suggests that spores introduced into the lung are phagocytosed by alveolar macrophages and taken to lymph nodes, where germination and replication occur. Our studies are compatible with these earlier histological findings and provide a model for addressing host-pathogen interactions using molecular and immunological tools.
As an example of how the pulmonary-infection model might be used to explore host susceptibility factors, we examined whether the mouse strain and age might affect the ability of the host to resist pulmonary-anthrax infection. No difference in LD50 was detected between male and female mice or among the different age groups of C57BL/6 mice. However, significant differences were observed among different inbred mouse strains in susceptibility to pulmonary infection with the Ames strain of B. anthracis. DBA/2 and C3HeB/FeJ or C3H/HeN mice were consistently more susceptible to i.t. and i.n. inoculation of B. anthracis. A/J and C57BL/6 mice were moderately susceptible, while BALB/c and 129X1/SVJ mice were the most resistant. DBA/2 and A/J mice were also previously shown to be more susceptible to the avirulent Sterne strain (40). Both of these mouse strains are C5 deficient, and replenishing C5 in A/J mice produced A/J mice with a Sterne-resistant phenotype (39). In our model, C3HeB/FeJ mice, which are not C5 deficient, are as sensitive as DBA/2 mice. Therefore, genetic factors, in addition to C5 deficiency, must play a role in establishing a resistant phenotype. The strain differences in susceptibility to the virulent Ames strain may provide a model for determining what genetic factors are important for producing a more resistant lung environment against B. anthracis.
The generalized public fear that resulted from the identification of anthrax infections caused by contamination of the U.S. mail resulted in mass disruption of normal daily life. Whether B. anthracis spores are capable of being an agent for mass destruction of human life is unclear. However, one important lesson from the human immunodeficiency virus epidemic is that the early, nearly paralyzing fear of this fatal disease in the 1980s lessened once the public understood the cause of infection and how its spread might be prevented. Furthermore, understanding the molecular mechanisms of productive infection helped in the identification of therapeutic targets. Crucial to developing control measures for B. anthracis is the recognition that the organism will be introduced through the lungs as a bioweapon. Therefore, murine lung models of anthrax that can be used to explore pathogenic and resistance mechanisms are essential. Our studies show that while the dosage that induces disease when spores are delivered to the lung may differ depending on whether an i.t. or i.n. route is used, the outcomes and general host responses appear to be very comparable.
Acknowledgments
This work was funded by the Department of Research Advanced Projects Agency of the Department of Defense (N00178-01-C-3069 to C.R.L.) and the National Institutes of Health (NIAID 1U54 AI057156-01 and NHLBI RO1 HL64548 to C.R.L. and NHLBI P50 HL 56384 to M.F.L.).
Editor: J. D. Clements
REFERENCES
- 1.Abramova, F. A., L. M. Grinberg, O. V. Yampolskaya, and D. H. Walker. 1993. Pathology of inhalational anthrax in 42 cases from the Sverdlovsk outbreak of 1979. Proc. Natl. Acad. Sci. USA 90:2291-2294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barlass, P. J., C. W. Houston, M. O. Clements, and A. Moir. 2002. Germination of Bacillus cereus spores in response to l-alanine and to inosine: the roles of gerL and gerQ operons. Microbiology 148:2089-2095. [DOI] [PubMed] [Google Scholar]
- 3.Barnes, J. 1947. The development of anthrax following administration of spores by inhalation. Br. J. Exp. Pathol. 28:385-394. [Google Scholar]
- 4.Beedham, R. J., P. C. Turnbull, and E. D. Williamson. 2001. Passive transfer of protection against Bacillus anthracis infection in a murine model. Vaccine 19:4409-4416. [DOI] [PubMed] [Google Scholar]
- 5.Bhatnagar, R., and S. Batra. 2001. Anthrax toxin. Crit. Rev. Microbiol. 27:167-200. [DOI] [PubMed] [Google Scholar]
- 6.Brand, P., K. Haussinger, T. Meyer, G. Scheuch, H. Schulz, T. Selzer, and J. Heyder. 1999. Intrapulmonary distribution of deposited particles. J. Aerosol Med. 12:275-284. [DOI] [PubMed] [Google Scholar]
- 7.Brossier, F., M. Levy, and M. Mock. 2002. Anthrax spores make an essential contribution to vaccine efficacy. Infect. Immun. 70:661-664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Christopher, G. W., T. J. Cieslak, J. A. Pavlin, and E. M. Eitzen, Jr. 1997. Biological warfare. A historical perspective. JAMA 278:412-417. [PubMed] [Google Scholar]
- 9.Corberand, J., F. Ngyen, P. Laharrague, A. M. Fontanilles, B. Gleyzes, E. Gyrard, and C. Senegas. 1981. Polymorphonuclear functions and aging in humans. J. Am. Geriatr. Soc. 29:391-397. [DOI] [PubMed] [Google Scholar]
- 10.Coulson, N. M., M. Fulop, and R. W. Titball. 1994. Bacillus anthracis protective antigen, expressed in Salmonella typhimurium SL 3261, affords protection against anthrax spore challenge. Vaccine 12:1395-1401. [DOI] [PubMed] [Google Scholar]
- 11.Cullamar, E. K., and L. I. Lutwick. 2002. Inhalational anthrax. Curr. Infect. Dis. Rep. 4:238-243. [DOI] [PubMed] [Google Scholar]
- 12.Dalldorf, F. G., A. F. Kaufmann, and P. S. Brachman. 1971. Woolsorters' disease. An experimental model. Arch. Pathol. 92:418-426. [PubMed] [Google Scholar]
- 13.Dixon, T. C., A. A. Fadl, T. M. Koehler, J. A. Swanson, and P. C. Hanna. 2000. Early Bacillus anthracis-macrophage interactions: intracellular survival and escape. Cell Microbiol. 2:453-463. [DOI] [PubMed] [Google Scholar]
- 14.Elliott, T. B., I. Brook, R. A. Harding, S. S. Bouhaouala, S. J. Peacock, and G. B. Knudson. 2002. Bacillus anthracis infection in irradiated mice: susceptibility, protection, and therapy. Mil. Med. 167:103-104. [PubMed] [Google Scholar]
- 15.Fritz, D. L., N. K. Jaax, W. B. Lawrence, K. J. Davis, M. L. Pitt, J. W. Ezzell, and A. M. Friedlander. 1995. Pathology of experimental inhalation anthrax in the rhesus monkey. Lab. Investig. 73:691-702. [PubMed] [Google Scholar]
- 16.Ginaldi, L., M. De Martinis, A. D'Ostilio, L. Marini, M. F. Loreto, V. Martorelli, and D. Quaglino. 1999. The immune system in the elderly. II. Specific cellular immunity. Immunol. Res. 20:109-115. [DOI] [PubMed] [Google Scholar]
- 17.Greene, C. M., J. Reefhuis, C. Tan, A. E. Fiore, S. Goldstein, M. J. Beach, S. C. Redd, D. Valiante, G. Burr, J. Buehler, R. W. Pinner, E. Bresnitz, and B. P. Bell. 2002. Epidemiologic investigations of bioterrorism-related anthrax, New Jersey, 2001. Emerg. Infect. Dis. 8:1048-1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grinberg, L. M., F. A. Abramova, O. V. Yampolskaya, D. H. Walker, and J. H. Smith. 2001. Quantitative pathology of inhalational anthrax. I. quantitative microscopic findings. Mod. Pathol. 14:482-495. [DOI] [PubMed] [Google Scholar]
- 19.Guarner, J., J. A. Jernigan, W. J. Shieh, K. Tatti, L. M. Flannagan, D. S. Stephens, T. Popovic, D. A. Ashford, B. A. Perkins, and S. R. Zaki. 2003. Pathology and pathogenesis of bioterrorism-related inhalational anthrax. Am. J. Pathol. 163:701-709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guidi-Rontani, C., M. Weber-Levy, E. Labruyere, and M. Mock. 1999. Germination of Bacillus anthracis spores within alveolar macrophages. Mol. Microbiol. 31:9-17. [DOI] [PubMed] [Google Scholar]
- 21.Inglesby, T. V., T. O'Toole, D. A. Henderson, J. G. Bartlett, M. S. Ascher, E. Eitzen, A. M. Friedlander, J. Gerberding, J. Hauer, J. Hughes, J. McDade, M. T. Osterholm, G. Parker, T. M. Perl, P. K. Russell, and K. Tonat. 2002. Anthrax as a biological weapon, 2002: updated recommendations for management. JAMA 287:2236-2252. [DOI] [PubMed] [Google Scholar]
- 22.Ireland, J. A., and P. C. Hanna. 2002. Amino acid- and purine ribonucleoside-induced germination of Bacillus anthracis DeltaSterne endospores: gerS mediates responses to aromatic ring structures. J. Bacteriol. 184:1296-1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ivins, B. E., S. L. Welkos, G. B. Knudson, and S. F. Little. 1990. Immunization against anthrax with aromatic compound-dependent (Aro-) mutants of Bacillus anthracis and with recombinant strains of Bacillus subtilis that produce anthrax protective antigen. Infect. Immun. 58:303-308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Koehler, T. M. 2002. Bacillus anthracis genetics and virulence gene regulation. Curr. Top. Microbiol. Immunol. 271:143-164. [DOI] [PubMed] [Google Scholar]
- 24a.Leighton, T. J., and R. H. Doi. 1971. The stability of messenger ribonucleic acid during sporulation in Bacillus anthracis. J. Biol. Chem. 246:3189-3195. [PubMed] [Google Scholar]
- 25.Little, S. F., and B. E. Ivins. 1999. Molecular pathogenesis of Bacillus anthracis infection. Microbes Infect. 1:131-139. [DOI] [PubMed] [Google Scholar]
- 26.Meselson, M., J. Guillemin, M. Hugh-Jones, A. Langmuir, I. Popova, A. Shelokov, and O. Yampolskaya. 1994. The Sverdlovsk anthrax outbreak of 1979. Science 266:1202-1208. [DOI] [PubMed] [Google Scholar]
- 27.Moayeri, M., D. Haines, H. A. Young, and S. H. Leppla. 2003. Bacillus anthracis lethal toxin induces TNF-alpha-independent hypoxia-mediated toxicity in mice. J. Clin. Investig. 112:670-682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mock, M., and A. Fouet. 2001. Anthrax. Annu. Rev. Microbiol. 55:647-671. [DOI] [PubMed] [Google Scholar]
- 29.Mock, M., and T. Mignot. 2003. Anthrax toxins and the host: a story of intimacy. Cell Microbiol. 5:15-23. [DOI] [PubMed] [Google Scholar]
- 30.Moir, A. 2003. Bacterial spore germination and protein mobility. Trends Microbiol. 11:452-454. [DOI] [PubMed] [Google Scholar]
- 31.Moir, A., B. M. Corfe, and J. Behravan. 2002. Spore germination. Cell. Mol. Life Sci. 59:403-409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Orme, I. M. 1987. Aging and immunity to tuberculosis: increased susceptibility of old mice reflects a decreased capacity to generate mediator T lymphocytes. J. Immunol. 138:4414-4418. [PubMed] [Google Scholar]
- 33.Pezard, C., M. Weber, J. C. Sirard, P. Berche, and M. Mock. 1995. Protective immunity induced by Bacillus anthracis toxin-deficient strains. Infect. Immun. 63:1369-1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reed, L., and H. Muench. 1938. A simple method of estimating fifty per cent endpoints. Am. J. Hyg. 27:493-497. [Google Scholar]
- 35.Ross, J. 1957. The pathogenesis of anthrax following administration of spores by the respiratory route. J. Pathol. Bacteriol. 73:485-494. [Google Scholar]
- 36.Schlessinger, R. 1995. Deposition and clearance for inhaled particles, p. 191-224. In R. O. McClellan and R. F. Henderson (ed.), Concepts in inhalation toxicology. Taylor and Francis, Washington, D.C.
- 37.Spencer, R. C. 2003. Bacillus anthracis. J. Clin. Pathol. 56:182-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vasconcelos, D., R. Barnewall, M. Babin, R. Hunt, J. Estep, C. Nielsen, R. Carnes, and J. Carney. 2003. Pathology of inhalation anthrax in cynomolgus monkeys (Macaca fascicularis). Lab. Investig. 83:1201-1209. [DOI] [PubMed] [Google Scholar]
- 39.Welkos, S. L., and A. M. Friedlander. 1988. Pathogenesis and genetic control of resistance to the Sterne strain of Bacillus anthracis. Microb. Pathog. 4:53-69. [DOI] [PubMed] [Google Scholar]
- 40.Welkos, S. L., T. J. Keener, and P. H. Gibbs. 1986. Differences in susceptibility of inbred mice to Bacillus anthracis. Infect. Immun. 51:795-800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Young, G., M. Zelle, and R. Lincoln. 1946. Respiratory pathogenicity of Bacillus anthracis spores. J. Infect. Dis. 79:2333-2346. [DOI] [PubMed] [Google Scholar]